Abstract
Objective
This randomized, cross-over trial was designed to investigate the metabolic and appetitive responses to skipping breakfast in overweight women who were habitual breakfast Eaters or Skippers.
Design and Methods
Nine Eaters and nine Skippers were studied on two separate days during which subjects ate breakfast (B), or had no breakfast (NB), followed by a standard lunch meal 4 hours later. Blood sampling for hormones and metabolites was performed after lunch and appetite was rated throughout the day.
Results
Interactions between day and habitual breakfast pattern were seen for Area Under the Curve (AUC) for insulin and free fatty acids (FFA). Both insulin (p=0.020) and FFA (p=0.023) AUC were higher on the NB day for Eaters, but similar on both days for Skippers. Eaters had higher pre-lunch hunger AUC on the NB day (p=0.015) as well as lower pre-lunch satiety AUC under both conditions (p=0.019).
Conclusion
Overall, this study showed that the adverse effects of skipping breakfast (higher insulin and FFA responses to lunch, increased hunger and decreased satiety) were found primarily in habitual breakfast eaters. This suggests that meal skipping may have enhanced effects in habitual Eaters due to entrainment of metabolic and appetitive regulatory systems.
Keywords: Breakfast skipping, eating behaviors, women, glucose metabolism, insulin, appetite
Introduction
Obesity is a serious public health problem in the United States, with a majority of Americans now being either overweight or obese (1). Though many factors contribute to the obesity epidemic, it is possible that breakfast skipping is one such factor. Epidemiological studies have shown that breakfast skipping is associated with higher BMI in children, adolescents and adults (2, 3, 4, 5, 6, 7, 8, 9, 10, 11), and most longitudinal studies have shown breakfast skipping to be associated with greater weight gain (4, 12). Prospective studies have shown that skipping breakfast is associated with dyslipidemia (13, 14), increased blood pressure (14, 15), higher risk of type 2 diabetes and metabolic syndrome (12, 15), and increased risk of coronary heart disease (16).
However, a causal relationship between breakfast skipping and weight gain has not been established. The fact that breakfast skippers have a higher risk of type 2 diabetes mellitus suggests that skipping breakfast might lead to changes in glucose metabolism. Several small studies have investigated the metabolic response to food after eating or omitting breakfast. These studies have shown breakfast skipping to be associated with impairment of insulin sensitivity (17, 18), decreased fullness and decreased levels of hormones related to satiety (19), and deterioration of lipid profiles (17, 20).
However, none of these studies evaluated obese adults or assessed the effects of habitual breakfast pattern. Thus, in order to investigate the metabolic, hormonal, and appetitive responses to skipping breakfast, we carried out a randomized, cross-over trial of overweight and obese women who were habitual breakfast eaters or breakfast skippers. The primary hypothesis was that skipping breakfast would lead to an increased insulin response following lunch, and that this effect would be more pronounced in habitual breakfast skippers. Secondary outcomes included response of additional hormones and metabolites, appetitive response, energy intake, energy expenditure, substrate oxidation, and differences between breakfast eaters and skippers.
Methods
Ethics Statement
This study was conducted according to the principles expressed in the Declaration of Helsinki. The study was approved by the Colorado Multiple Institutional Review Board. All patients provided written informed consent for the collection of samples and subsequent analysis.
Subjects
Healthy women of all ethnic groups, ages 25-40, with BMI 27-35 kg/m2, without eating disorders, and who were either habitual breakfast eaters (Eaters) or breakfast skippers (Skippers) were recruited. Subjects were asked to identify themselves as Eaters or Skippers by answering the question: “How many days per week do you eat breakfast?” Eaters reported eating breakfast ≥ 5 days per week and Skippers reported eating breakfast ≤2 days per week. Women without menses were excluded, and all women reported no active dieting or intensive exercise training. Additionally, subjects were excluded if they were identified as having night eating syndrome (at least 25% of food intake is consumed after the evening meal and/or at least two episodes of nocturnal eating per week) (21).
Pre-study Procedures
Pre-study procedures included measurement of height, weight, vital signs, and resting metabolic rate (RMR). After 30 minutes of quiet rest, RMR was measured using standard indirect calorimetry with the ventilated hood technique (Parvo Medics Truemax 2400, Salt Lake City, UT). Subjects remained awake, supine, lightly clothed in a thermoneutral (68-74 °F) quiet room. The following equation was used to estimate total energy expenditure (TEE): TEE = measured RMR (kcals) x activity factor. A standard activity factor of 1.4 was used for all subjects. Prior to the first study visit day, all subjects completed a 3 day diet diary in order to obtain usual dietary intake patterns and confirm reported breakfast eating pattern (Eater or Skipper).
Study Visits
Each subject underwent 2 study conditions (Breakfast – B and No Breakfast – NB) with the order of study conditions determined using a computer-generated randomization table. Four Skippers and three Eaters underwent the NB condition first, and six Eaters and five Skippers underwent B first. Subjects were not aware of the order of study visits until the first study day. The study visits were timed to occur during the follicular phase of the menstrual cycle with one month between visits (22). Subjects were asked not to do purposeful exercise in the 48 hours prior to each study day. Each subject's total daily energy intake (EI) for study visits was estimated based upon TEE as described above. Subjects were provided with a standard dinner meal (35% of daily EI; 15% protein, 30% fat, 55% carbohydrate) to be eaten the night before each test day between 6 and 8 PM and were asked not to eat anything after 8 PM. On the morning of the test day, subjects presented for baseline measurements at 7:00 AM. Their height, weight and vital signs were measured and then they were asked to lie quietly for 30 minutes. Subsequently, RMR was measured at baseline, as described above, and subjects were then asked to rate hunger and satiety using visual analog scales (VAS). Hunger was rated on a 100-mm line preceded by the question, “How hungry do you feel right now?” and anchored by “not at all hungry” on the left and “extremely hungry” on the right. Satiety was rated by VAS with the question, “How full do you feel right now?” with the anchors “not at all” and “extremely (23). When the appetite ratings were complete, an intravenous catheter was inserted into an antecubital vein and blood was drawn for fasting glucose, insulin, free fatty acids (FFA), ghrelin, PYY (peptide YY), GLP-1 (glucagon-like peptide 1), and triglycerides (TG). When all baseline measurements were complete, subjects were provided with breakfast along with 250mL water on the B test day, or 250mL water alone on the NB test day. The breakfast meal contained 25% of total daily EI (15% protein, 30% fat, 55% carbohydrate). The content of the breakfast was wheat flakes plus milk, scrambled eggs, and orange juice. Time zero was the time that the subject began eating (or drinking) and subjects were asked to consume the breakfast (or water) within 20 minutes. Blood sampling was performed prior to and every 30 minutes after the lunch meal for 3 hours. Subjects rated hunger and satiety using VAS hourly prior to lunch, every 30 minutes for 3 hours following lunch, and hourly until the end of the study day. Indirect calorimetry was performed hourly throughout each testing day (Figure 1).
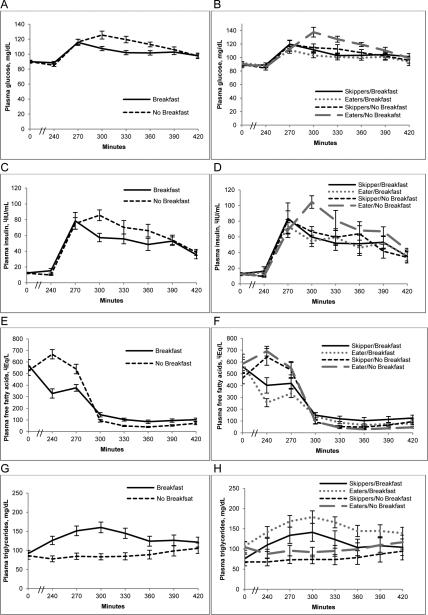
Figure 1.
Overview of study day. Study procedures are shown by time (minutes). IC – Indirect calorimetry; VAS – Visual Analog Scales for appetite ratings; Labs – glucose, insulin, free fatty acids, triglycerides, leptin, GLP-1, PYY, ghrelin.
At 240 minutes, subjects were provided with a standard lunch containing 35% of daily EI (15% protein, 30% fat, 55% carbohydrate). The lunch meal was comprised of the same foods in the same amounts on both test days, and was made up of a sandwich, chips, and fruit. Subjects were asked to consume all contents of the lunch meal within 20 minutes.
At 540 minutes, subjects were provided with an ad libitum dinner meal and told to eat as much or as little as they needed to feel full. The dinner meal was comprised of pepperoni pizza, fettucine alfredo, vanilla yogurt and chocolate pudding and provided a total of 2600 kcal (15% protein, 30% fat, 55% carbohydrate). After the meal was finished the subjects were allowed to leave. They were provided with a box of snack foods to take home and were told that if they wanted to eat anything that evening, they should eat only items contained in the box (and no items from their home). The box contained soda (diet and regular), grapes, plain M&M's, cashews, vanilla ice cream, pretzels, and potato chips. They returned the uneaten portion of snacks the following day, and the amount eaten both at dinner and from snack foods was determined by weigh-back methods.
Laboratory Analyses
Blood samples were collected in EDTA-containing tubes, centrifuged, placed in aliquot tubes and stored at −70 to −80° C until analysis. All assays were run after both study days were complete for each subject. For GLP-1, 30ɥl of dipeptidyl peptidase IV inhibitor was added to the 4ml EDTA tube prior to collection. GLP-1 assays were performed with Alpco Diagnostics ELISA (43-GPTHU-E01). Insulin concentrations were measured using competitive radioimmunoassay (Millipore). Radioimmunoassay was used to analyze serum leptin (Millipore), serum PYY concentrations (Millipore Cat. #PYYT-66HK) and total serum ghrelin concentrations (Millipore Cat. #GHRT-89HK). All radioimmunoassays were performed with a Perkin Elmer Wallac Gamma counter using Maciel RIA-AID data reduction software. Assays for glucose, TG and FFA were performed on the Olympus AU400e Chemistry Analyzer (Beckman). Reagents were purchased from Beckman Coulter for glucose and TG and from WACO for FFA.
Statistical Analysis
Sample size calculations were performed using SigmaPlot version 12 (San Jose, CA). Sample size was determined with the use of glucose and insulin data from a study of over- and underfeeding done by our group (24). Power was estimated for a range of possible differences for a paired t-test at the 0.05 level. A sample of 18 subjects would give us 80% power to detect a difference in insulin AUC of 3000 μIU/mL x 180 min. Assuming a 25% dropout rate, a sample size of 24 women enrolled would provide about 18 subjects for analysis. Baseline characteristics of the two groups (Skippers vs. Eaters) and EI were analyzed with the use of Wilcoxon rank sum tests. Area Under the Curve (AUC) was calculated for all outcomes with the exception of energy intake (laboratory values, appetite ratings, energy expenditure and respiratory quotient [RQ]) using the trapezoid method (25). For laboratory values, AUC for the 3-hour period following lunch was used. For appetite ratings, energy expenditure and RQ, AUC was calculated for the pre-lunch period (time zero through 240 min) and post-lunch period (270 through 540 min). Energy intake (dinner, evening snack and total EI) and all AUC outcomes were modeled using mixed-model linear regression (SAS 9.3, SAS Institute, Cary, NC). Day, skipper/eater, and order were included as predictors in every model. The day by skipper/eater interaction was tested in every model. The interaction term was left in the final model in models where it was significant at the 0.05 alpha-level, but was removed from the final model if not significant. All models included random intercepts for subjects to account for the repeated measures on subjects. All data for all 18 subjects were included in analyses, with the exception of EI data for one subject in the Skipper group (due to failure to follow protocol in returning the snack box items) and glucose data for one subject in the Eater group (due to missing data).
Results
Subjects and baseline characteristics
A total of 24 women were enrolled in the study. Two subjects completed one study day and then dropped out of the study due to scheduling conflicts, and 4 other subjects dropped out prior to the first study day, also due to scheduling conflicts. A total of 18 women completed the study, 9 Skippers and 9 Eaters. Subjects were 72% Caucasian, 22% African American, and 6% Asian. They were 88% Non-Hispanic and 22% Hispanic. There was no difference among groups in race or ethnicity, and no difference in age, BMI or RMR (Table 1).
Table 1.
| All subjects, n=18 | Breakfast Eaters, n=9 | Breakfast Skippers, n=9 | |
|---|---|---|---|
| Age, years | 29 (27, 32) | 29 (27.5, 31.5) | 28 (26.5, 34) |
| BMI, kg/m2 | 30.2 (28.6, 33.7) | 30.2 (29.2, 32.7) | 30 (27.8, 34.3) |
| Breakfast normally consumed, d/wk | 3.5 (1, 6) | 6 (5.5, 7) | 1 (1, 2)* |
| RMR, kcal/day | 1549 (1463, 1688) | 1563 (1465, 1755) | 1536 (1460, 1594) |
Values are medians (interquartile range)
Different from Breakfast Eaters, p<0.001
BMI, Body Mass Index; RMR, Resting Metabolic Rate
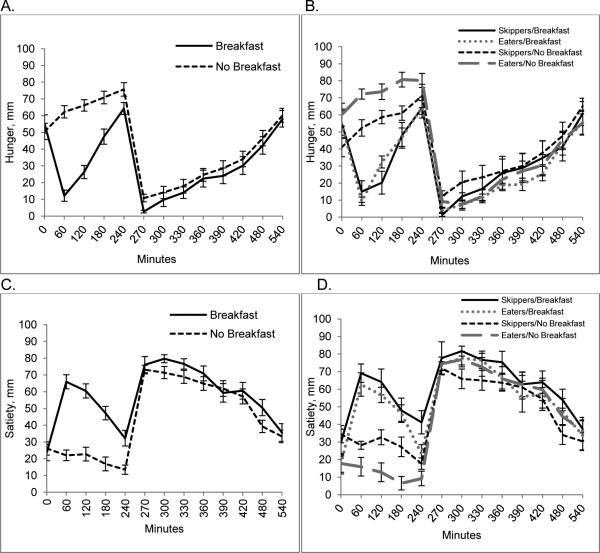
Laboratory Measures
There were significant interactions between day and breakfast pattern (Skipper/Eater) for insulin and FFA AUC, such that values were higher on the NB day for Eaters but similar on both days for Skippers (Figure 2 and Table 2). The AUC's for TG, GLP-1 and PYY were higher on the B day, whereas AUC was lower on the B day for glucose. Order effect was evaluated and was not found to be significant.
Figure 2.
Metabolic response to breakfast skipping in habitual breakfast eaters and skippers. Glucose (A), insulin (C), free fatty acids (E) and triglycerides (G) are shown at 0 minutes, 240 minutes (prior to lunch meal) and every 30 minutes for 180 minutes following the lunch meal on the Breakfast and No Breakfast days in all subjects combined. Values are means ± SEM, n=18. Also shown are differences between the response in breakfast Eaters vs. Skippers for glucose (B), insulin (D), free fatty acids (F) and triglycerides (H). Values are means ± SEM, n=18 (9 Skippers; 9 Eaters).
Table 2.
Post-lunch AUC for hormones and metabolites on breakfast and no breakfast days for breakfast skippers and eaters1,2
| Outcome | Effect | Category | Estimate | 95% CI | p-value |
|---|---|---|---|---|---|
| Skipper/Eater | 0.45 | (−8.87, 9.78) | 0.919 | ||
| Day × Skipper/Eater | −9.66 | (−17.8, −1.52) | 0.023 | ||
| Breakfast/Eater | 25.7 | (18.8, 32.5) | |||
| Breakfast/Skipper | 34.9 | (28.5, 41.3) | |||
| No Breakfast/Eater | 35.1 | (28.2, 41.9) | |||
| No Breakfast/Skipper | 34.6 | (28.2, 41.0) | |||
| GLP-1 AUC, pM × 180 min | Breakfast/No Breakfast | 321 | (177, 464) | <0.001 | |
| Breakfast | 1198 | (876, 1520) | |||
| No Breakfast | 877 | (555, 1200) | |||
| Skipper/Eater | −138 | (−757, 480) | 0.642 | ||
| Eater | 969 | (513, 1420) | |||
| Skipper | 1100 | (682, 1530) | |||
| Ghrelin AUC, ng/L × 180 min | Breakfast/No Breakfast | −2.67 | (−13.2, 7.91) | 0.600 | |
| Breakfast | 13.0 | (11.1, 14.9) | |||
| No Breakfast | 13.3 | (11.4, 15.1) | |||
| Skipper/Eater | −5.47 | (−41.2, 30.2) | 0.750 | ||
| Eater | 12.9 | (10.2, 15.5) | |||
| Skipper | 13.4 | (10.9, 15.8) | |||
| Glucose AUC, g/L × 180 min | Breakfast/No Breakfast | −14.6 | (−24.7, −4.59) | 0.007 | |
| Breakfast | 187 | (179, 195) | |||
| No-Breakfast | 201 | (193, 209) | |||
| Skipper/Eater | 331 | (−922, 158) | 0.582 | ||
| Eater | 196 | (186, 205) | |||
| Skipper | 192 | (184, 201) | |||
| Insulin AUC, IU/L × 180 min | Breakfast/No Breakfast | −0.31 | (−1.97, 1.35) | 0.698 | |
| Skipper/Eater | 2.49 | (−8.96, 5.87) | 0.138 | ||
| Day × Skipper/Eater | −2.95 | (−5.37, −0.53) | 0.020 | ||
| Breakfast /Eater | 9.26 | (6.77, 11.7) | |||
| Breakfast /Skipper | 9.72 | (7.40, 12.0) | |||
| No Breakfast/Eater | 12.5 | (10.0, 15.0) | |||
| No Breakfast/Skipper | 10.0 | (7.71, 12.4) | |||
| PYY AUC, ng/L × 180 min | Breakfast/No Breakfast | 2.25 | (0.65, 3.86) | 0.008 | |
| Breakfast | 19.6 | (18.1, 21.1) | |||
| No Breakfast | 17.4 | (15.9, 18.8) | |||
| Skipper/Eater | −0.37 | (−2.82, 2.07) | 0.750 | ||
| Eater | 18.3 | (16.5, 20.1) | |||
| Skipper | 18.7 | (17.0, 20.4) | |||
| TG AUC, g/L × 180 min | Breakfast/No Breakfast | 88.6 | (447, 133) | <0.001 | |
| Breakfast | 241 | (196, 285) | |||
| No Breakfast | 152 | (107, 196) | |||
| Skipper/Eater | 40.1 | (−36.2, 116) | 0.281 | ||
| Eater | 216 | (160, 273) | |||
| Skipper | 176 | (124, 229) | |||
Values are mean AUC (95% CI), n=18. For outcomes that do not include interactions, estimates, CI's, and p-values are given for each predictor, and least-squares means and CI's are given for each predictor group. For outcomes that do include interactions, least-squares means are given for each day by skipper/eater combination rather than for day groups and skipper/eater groups separately.
AUC – Area Under Curve; FFA – free fatty acids; GLP-1 – glucagon-like peptide 1; PYY – peptide YY; TG – triglycerides
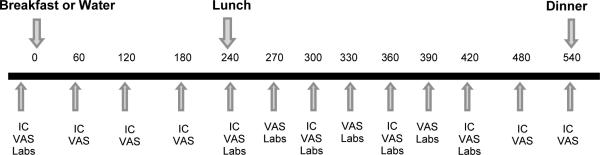
Appetite ratings
There were significant interactions between condition and breakfast pattern for pre-lunch hunger AUC and post-lunch satiety AUC (Figure 3 and Table 3). Pre-lunch hunger AUC was higher on the NB day for Eaters as compared to Skippers. Overall pre-lunch hunger under both the B and NB conditions was higher in Eaters. Pre-lunch satiety under both conditions was lower in Eaters as compared to Skippers. Post-lunch satiety AUC was similar on both days for Eaters, whereas it was higher on the B day for Skippers. There was no significant order effect.
Figure 3.
Appetitive response to breakfast skipping in habitual breakfast eaters and skippers. Eaters. Hunger (A) and satiety (C) at 0 minutes and every hour prior to the lunch meal, every 30 minutes for 180 minutes following lunch, and hourly until end of study day are shown on the breakfast and no breakfast day for all subjects. Values are means ± SEM, n=18. Hunger (B) and satiety (D) in breakfast Eaters vs. Skippers at 0 minutes and every hour prior to the lunch meal, every 30 minutes for 180 minutes following lunch, and hourly until end of study day are shown on the breakfast and no breakfast day. Values are means ± SEM, n=18 (9 Skippers, 9 Eaters).
Table 3.
Pre- and post-lunch AUC for hunger and satiety on breakfast and no breakfast days for breakfast skippers and eaters1,2
| Outcome | Effect | Category | Estimate | 95% CI | p-value |
|---|---|---|---|---|---|
| Pre-lunch hunger AUC, cm × 240 min | Breakfast/No Breakfast | −51.1 | (−72.1, −30.1) | <.0001 | |
| Skipper/Eater | 42.0 | (15.8, 68.2) | 0.003 | ||
| Day × Skipper/Eater | −38.0 | (−67.7, −8.33) | 0.015 | ||
| Breakfast/Eater | 90.1 | (71.3, 109) | |||
| Breakfast/Skipper | 86.2 | (67.7, 105) | |||
| No Breakfast/Eater | 179 | (160, 198) | |||
| No Breakfast/Skipper | 137 | (119, 156) | |||
| Post-lunch hunger AUC, cm × 270 min | Breakfast/No Breakfast | −10.7 | (−24.4, 2.93) | 0.116 | |
| Breakfast | 76.5 | (54.9, 98.1) | |||
| No-Breakfast | 87.3 | (65.7, 109) | |||
| Skipper/Eater | −16.3 | (−56.5, 23.9) | 0.405 | ||
| Eater | 73.8 | (44.7, 102.8) | |||
| Skipper | 90.0 | (61.7, 118) | |||
| Pre-lunch satiety AUC, cm × 240 min | Breakfast/No Breakfast | 72.1 | (54.1, 90.1) | <.0001 | |
| Breakfast | 121 | (106, 136) | |||
| No-Breakfast | 49.1 | (34.2, 64.0) | |||
| Skipper/Eater | −28.4 | (−51.7, −5.21) | 0.019 | ||
| Eater | 70.9 | (54.1, 87.7) | |||
| Skipper | 99.4 | (83.0, 116) | |||
| Post-lunch satiety AUC, cm × 270 min | Breakfast/No Breakfast | 31.5 | (11.2, 51.8) | 0.005 | |
| Day × Skipper/Eater | −32.5 | (−61.2, −3.83) | 0.029 | ||
| Breakfast/Eater | 162 | (136, 189) | |||
| Breakfast/Skipper | 174 | (148, 201) | |||
| No Breakfast/Eater | 163 | (137, 190) | |||
| No Breakfast/Skipper | 143 | (117, 169) | |||
Values are mean AUC (95% CI), n=18. For outcomes that do not include interactions, estimates, CI's, and p-values are given for each predictor, and least-squares means and CI's are given for each predictor group. For outcomes that do include interactions, least-squares means are given for each day by skipper/eater combination rather than for day groups and skipper/eater groups separately.
AUC – Area Under Curve
Energy intake
EI for breakfast and lunch did not differ by day, per study design (Table 4). Dinner, snack and total EI, as well as macronutrient composition, were examined with the use of the mixed model, and there were no interactions, differences between Eaters and Skippers, or order effect, so data presented are for the difference between B and NB only. Dinner, snack and total EI did not differ by day. Protein, carbohydrate and fiber intake were higher on the B day.
Table 4.
| Energy, kcal | Protein, g | Fat, g | Carbohydrate, g | Fiber, g | ||
|---|---|---|---|---|---|---|
| Breakfast | Breakfast | 497 (463, 529) | 20 (19, 22) | 18 (16, 19) | 75 (70, 80) | 8 (8, 9) |
| No Breakfast | N/A | N/A | N/A | N/A | N/A | |
| Lunch | Breakfast | 713 (691, 782) | 29 (27, 30) | 25 (23, 27) | 103 (98, 110) | 6 (5, 7) |
| No Breakfast | 713 (691, 782) | 29 (27, 30) | 25 (23, 27) | 103 (98, 110) | 6 (5, 7) | |
| Dinner | Breakfast | 815 (550, 1072) | 33 (22, 42) | 27 (18, 36) | 112 (75, 148) | 4 (3, 5) |
| No Breakfast | 837 (594, 972) | 33 (25, 39) | 28 (19, 32) | 116 (82, 134) | 4 (3, 5) | |
| Snack | Breakfast | 701 (177, 1023) | 8 (3, 12) | 24 (10, 48) | 110 (33, 140) | 3 (1, 7) |
| No Breakfast | 716 (360, 1197) | 10 (4, 18) | 37 (12, 58) | 101 (49, 121) | 4 (1, 6) | |
| Total | Breakfast | 2516 (2363, 3324) | 85 (77, 103) | 98 (76, 120) | 380 (328, 459) | 23 (19, 28) |
| No Breakfast | 2344 (1913, 2777) | 75 (64, 86)* | 94 (64, 127) | 318 (262, 368)* | 15 (12, 19)** |
Values are medians (interquartile range), n=17 (9 Eaters, 8 Skippers)
Different from Breakfast, p<0.05
Different from Breakfast, p<0.05
Different from Breakfast, p<0.001
g, grams; kcal, kilocalorie
Energy expenditure
The pre-lunch EE AUC was higher on the B as compared to NB day (Table 5). Post-lunch EE AUC showed a trend toward being higher on the B day, but did not reach significance (p=0.051). There were no group differences, interactions, or order effect for EE.
Table 5.
Pre- and post-lunch AUC for energy expenditure and respiratory quotient on breakfast and no breakfast days for breakfast skippers and eaters1,2
| Outcome | Effect | Category | Estimate | 95% CI | p-value |
|---|---|---|---|---|---|
| Pre-lunch EE AUC, Mcal/day × 240 min | Breakfast/No Breakfast | 459 | (372, 545) | <.0001 | |
| Breakfast | 411 | (388, 434) | |||
| No Breakfast | 365 | (342, 388) | |||
| Skipper/Eater | 177 | (−271, 626) | 0.415 | ||
| Eater | 397 | (364, 429) | |||
| Skipper | 379 | (347, 411) | |||
| Post-lunch EE AUC, Mcal/day × 270 min | Breakfast/No Breakfast | 11.7 | (−90.8, 234) | 0.051 | |
| Breakfast | 430 | (404, 456) | |||
| No Breakfast | 418 | (392, 444) | |||
| Skipper/Eater | 28.3 | (−21.5, 78.2) | 0.247 | ||
| Eater | 438 | (402, 474) | |||
| Skipper | 410 | (375, 445) | |||
| Pre-lunch RQ AUC, RQ × 240 min | Breakfast/No Breakfast | 14.1 | (8.59, 19.6) | <.0001 | |
| Skipper/Eater | −3.39 | (−11.36, 4.59) | 0.381 | ||
| Day × Skipper/Eater | 8.71 | (0.92, 16.5) | 0.031 | ||
| Breakfast/Eater | 206 | (200, 212) | |||
| Breakfast/Skipper | 201 | (195, 206) | |||
| No Breakfast/Eater | 184 | (177, 189) | |||
| No Breakfast/Skipper | 186 | (181, 192) | |||
| Order | −7.39 | (−14.5, −0.25) | 0.043 | ||
| Breakfast First | 190 | (186, 195) | |||
| No Breakfast First | 198 | (192, 203) | |||
| Post-lunch RQ AUC, RQ × 270 min | Breakfast/No Breakfast | 3.46 | (−0.68, 7.59) | 0.096 | |
| Breakfast | 204 | (201, 207) | |||
| No-Breakfast | 201 | (198, 204) | |||
| Skipper/Eater | 8.15 | (4.00, 12.3) | 0.001 | ||
| Eater | 206 | (203, 209) | |||
| Skipper | 198 | (195, 201) | |||
| Order | −7.25 | (−11.5, −2.99) | 0.002 | ||
| Breakfast First | 199 | (196, 201) | |||
| No Breakfast First | 206 | (203, 209) | |||
Carbohydrate and fat oxidation
There was an interaction between pre-lunch RQ AUC and habitual breakfast pattern, such that the AUC was lower on the B day for Skippers as compared to Eaters (Table 5). Pre-lunch RQ AUC was higher overall on the B as compared to NB day. Post-lunch RQ AUC was lower in Skippers as compared to Eaters under both conditions. There was a significant order effect for both pre-lunch and post-lunch RQ AUC, with higher values for both if the NB day was first.
Discussion
This randomized, cross-over trial was designed to investigate the hormonal, metabolic, and appetitive effects of breakfast skipping in overweight women, and to identify potential differences between habitual breakfast skippers and breakfast eaters. Our primary findings suggest that the effects of breakfast skipping differ depending on habitual breakfast pattern. Eaters demonstrated greater insulin and FFA responses to lunch after skipping breakfast, reported greater hunger before lunch, and had lower rates of fat oxidation after lunch on both days.
While the glucose response was higher after skipping breakfast for both Eaters and Skippers, the insulin and FFA responses were higher only in Eaters. Two other studies done in breakfast eaters have shown that skipping breakfast for one day (18) or fourteen days (17) resulted in an increased glucose and insulin response to a test meal. One of these studies also measured FFA and found an increased FFA response, similar to our finding of increased FFA in Eaters on the NB day (18). The higher FFA levels prior to lunch on the NB day were expected as subjects were fasting and were therefore undergoing lipolysis. FFA are widely believed to be involved in the causal association between obesity and insulin resistance, though the mechanisms have not been fully elucidated (26, 27). The “second meal phenomenon,” or the observation that the rise in blood glucose is less after the second of two similar meals (in both diabetics and nondiabetics), has been previously studied and found to be associated with enhanced muscle glycogen storage and appears to be determined by suppression of plasma FFA's (28). However, the lack of increased insulin and FFA response after breakfast skipping in habitual breakfast skippers is a novel finding. As the B day represents the typical diet pattern for Eaters, it is possible that the NB condition causes a greater increase in lipolysis and subsequent FFA levels, thus leading to higher insulin levels following lunch. In contrast, the NB day for Skippers represents their typical pattern, so they do not exhibit the same changes in glucose metabolism.
Skipping breakfast was also found in this study to result in changes in appetite and appetite-related hormones. Both groups reported greater hunger on the NB day, but Eaters reported greater hunger and less satiety as compared to Skippers. Both groups were found to have reduced PYY and GLP-1 responses to lunch after skipping breakfast. Since both hormones are thought to induce satiety (29), it could be hypothesized that the lower levels after lunch on the NB day would lead to decreased satiety and increased food consumption later in the day. However, our results showed that the calories consumed at breakfast were compensated for over the course of the day, resulting in similar EI on both days. It is possible that this finding is a product of the study design, as subjects were required to consume the same lunch meal in the same amounts on both study days. Since the greatest difference in appetite occurred at the pre-lunch time point, it is likely that any potential change in EI would have occurred at the lunch meal if subjects had been allowed ad libitum food intake.
Our study also examined the effects of breakfast skipping on EE and measures of carbohydrate and fat oxidation. Skipping breakfast was found to result in lower EE overall, with the difference being driven mainly by the pre-lunch values. The higher pre-lunch EE on the B day is attributable to the thermic effect of food (TEF) after breakfast, because other variables are kept constant on the two testing days, and TEF has been shown to last up to 6 hours (30). Post-lunch EE was also slightly increased on the B day, suggesting possible continued effects on post-lunch TEF related to breakfast consumption (although this difference was small). Skipping breakfast was found to result in a lower RQ, with the difference driven by pre-lunch values. This suggests greater fat oxidation on the NB day, likely due to ongoing lipolysis. Of interest, we found that Skippers had a lower pre-lunch RQ on the B day and lower post-lunch RQ on both days, suggesting greater fat oxidation, consistent with the slightly higher FFA in Skippers on B days. We did find evidence of an order effect, such that both pre- and post-lunch RQ were lower if the B day was first. It is possible that the combination of new experimental procedures (eating breakfast in an experimental setting, along with the first experience of repeated indirect calorimetry measurements) caused greater anxiety and release of catecholamines, leading to lipolysis and lower RQ, as it has been shown that anxiety affects measurements using indirect calorimetry (31)
Perhaps the most novel finding of the present study is that the adverse effects of breakfast skipping were seen only in habitual breakfast eaters. This suggests a ‘metabolic and behavioral memory’ for usual eating patterns. It has been shown that circadian rhythms and eating patterns are related, but it has not been demonstrated whether eating patterns drive circadian rhythms or whether the reverse occurs (32, 33). Similar to our findings, patterns of increased insulin and FFA have been seen in studies of circadian disruption (34, 35). Thus, it is possible that breakfast skipping represents a disruption to usual patterns in the Eaters, thus resulting in changes in glucose metabolism, but that habitual Skippers have adapted to this pattern and therefore do not show such changes. It is interesting to note that Skippers did not react adversely to eating breakfast, even though this would also represent a disruption to their usual eating pattern, and this may represent an area of future study.
There are several limitations to this study that should be acknowledged. First, we have studied only a small group of overweight women, so findings may not be applicable to men or individuals of normal weight. However, since the majority of Americans are now overweight, it could be argued that our findings apply to a clinically more relevant population. We did not include a true “run-in diet” period prior to the study days, although we did provide a dinner meal prior to each study day to ensure that the energy intake at dinner was the same prior to both study days. Therefore, our findings relate to the acute effects of skipping breakfast, and did not address possible longer-term adaptations. Given our findings in Skippers, it is possible that the metabolic effects seen in Eaters would disappear after a period of adaptation to skipping breakfast. Lastly, qualitative data regarding reasons for diet pattern choice (Eater vs. Skipper) were not collected in this study. It is possible that such factors might affect outcomes, and should be addressed in future studies.
Further studies are needed to confirm these results in a larger population and to assess longer-term effects of breakfast skipping. Additional studies would also be of benefit from a clinical standpoint. Current recommendations from health care providers and US dietary guidelines advocate for breakfast consumption (36). However, several recent studies have questioned the benefit of breakfast consumption (37, 38, 39, 40). The present study shows that the adverse effects of skipping breakfast occur only in breakfast eaters, suggesting that there is some adaptation to breakfast skipping. As it is not known whether the beneficial effects of eating breakfast would occur after a longer period of time, it is not certain whether a public health campaign to increase breakfast consumption would be of benefit to breakfast skippers.
In conclusion, the present study found that in overweight women, the adverse effects of one day of breakfast skipping (increased insulin and FFA response, increased hunger and decreased satiety) were found primarily in the breakfast eaters. These results suggest that habitual food intake patterns entrain metabolic systems in overweight breakfast Eaters such that skipping breakfast results in adverse metabolic consequences.
What is already known about this subject:
Breakfast skipping is associated with higher BMI and weight gain
Breakfast skipping is associated with higher risk for type 2 diabetes mellitus, dyslipidemia, high blood pressure, and higher cardiovascular risk
Small studies have shown skipping breakfast to be associated with impairment of insulin sensitivity
What this study adds:
The adverse effects of skipping breakfast were seen primarily in habitual breakfast eaters
Breakfast eaters had increased insulin and FFA responses to a lunch meal, and reported higher hunger and lower satiety as compared to breakfast skippers
These findings suggest that meal skipping may have enhanced effects in habitual breakfast eaters due to entrainment of metabolic and appetitive regulatory systems.
Values are mean AUC (95% CI), n=18. For outcomes that do not include interactions, estimates, CI's, and p-values are given for each predictor, and least-squares means and CI's are given for each predictor group. For outcomes that do include interactions, least-squares means are given for each day by skipper/eater combination rather than for day groups and skipper/eater groups separately.
Acknowledgements
We would like to acknowledge and thank the University of Colorado Clinical and Translational Science Institute (CCTSI) as well as the CCTSI Metabolic Kitchen for their support of this study. We would also like to thank the study participants for their time.
Funding Sources: This study was supported by the following grants: NIH grant 5 T32 DK007446-30; Endocrine Fellows Foundation grant: Fellows Development Research Grant Program in Diabetes, Obesity and Fat Cell Biology; Nutrition Obesity Research Center (NORC) Grant 5P30DK048520; NIH/NCATS Colorado CTSI Grant Number UL1 TR001082.
Glossary
- AUC
Area Under Curve
- EE
energy expenditure
- RQ
respiratory quotient
Footnotes
Author contributions: EAT, MAC, and JH designed research; EAT conducted research; BM and EAT performed statistical analyses; EAT, MAC, JH and DHB wrote the manuscript; all authors approved the final manuscript.
Conflict of interest:
All authors declare no conflict of interest.
References
- 1.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA : the journal of the American Medical Association. 2012;307:491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 2.Cho S, Dietrich M, Brown CJ, Clark CA, Block G. The effect of breakfast type on total daily energy intake and body mass index: results from the Third National Health and Nutrition Examination Survey (NHANES III). Journal of the American College of Nutrition. 2003;22:296–302. doi: 10.1080/07315724.2003.10719307. [DOI] [PubMed] [Google Scholar]
- 3.Albertson AM, Anderson GH, Crockett SJ, Goebel MT. Ready-to-eat cereal consumption: its relationship with BMI and nutrient intake of children aged 4 to 12 years. Journal of the American Dietetic Association. 2003;103:1613–1619. doi: 10.1016/j.jada.2003.09.020. [DOI] [PubMed] [Google Scholar]
- 4.Berkey CS, Rockett HR, Gillman MW, Field AE, Colditz GA. Longitudinal study of skipping breakfast and weight change in adolescents. Int J Obes Relat Metab Disord. 2003;27:1258–1266. doi: 10.1038/sj.ijo.0802402. [DOI] [PubMed] [Google Scholar]
- 5.Song WO, Chun OK, Obayashi S, Cho S, Chung CE. Is consumption of breakfast associated with body mass index in US adults? Journal of the American Dietetic Association. 2005;105:1373–1382. doi: 10.1016/j.jada.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 6.Fabry P, Hejl Z, Fodor J, Braun T, Zvolankova K. The Frequency of Meals. Its Relation to Overweight, Hypercholesterolaemia, and Decreased Glucose-Tolerance. Lancet. 1964;2:614–615. doi: 10.1016/s0140-6736(64)90510-0. [DOI] [PubMed] [Google Scholar]
- 7.Deshmukh-Taskar PR, Nicklas TA, O'Neil CE, Keast DR, Radcliffe JD, Cho S. The relationship of breakfast skipping and type of breakfast consumption with nutrient intake and weight status in children and adolescents: the National Health and Nutrition Examination Survey 1999-2006. Journal of the American Dietetic Association. 2010;110:869–878. doi: 10.1016/j.jada.2010.03.023. [DOI] [PubMed] [Google Scholar]
- 8.Gibson SA, O'Sullivan KR. Breakfast cereal consumption patterns and nutrient intakes of British schoolchildren. Journal of the Royal Society of Health. 1995;115:366–370. doi: 10.1177/146642409511500608. [DOI] [PubMed] [Google Scholar]
- 9.Timlin MT, Pereira MA. Breakfast frequency and quality in the etiology of adult obesity and chronic diseases. Nutrition reviews. 2007;65:268–281. doi: 10.1301/nr.2007.jun.268-281. [DOI] [PubMed] [Google Scholar]
- 10.Timlin MT, Pereira MA, Story M, Neumark-Sztainer D. Breakfast eating and weight change in a 5-year prospective analysis of adolescents: Project EAT (Eating Among Teens). Pediatrics. 2008;121:e638–645. doi: 10.1542/peds.2007-1035. [DOI] [PubMed] [Google Scholar]
- 11.Deshmukh-Taskar P, Nicklas TA, Radcliffe JD, O'Neil CE, Liu Y. The relationship of breakfast skipping and type of breakfast consumed with overweight/obesity, abdominal obesity, other cardiometabolic risk factors and the metabolic syndrome in young adults. The National Health and Nutrition Examination Survey (NHANES): 1999-2006. Public health nutrition. 2013;16:2073–2082. doi: 10.1017/S1368980012004296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mekary RA, Giovannucci E, Willett WC, van Dam RM, Hu FB. Eating patterns and type 2 diabetes risk in men: breakfast omission, eating frequency, and snacking. Am J Clin Nutr. 2012;95:1182–1189. doi: 10.3945/ajcn.111.028209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith KJ, Gall SL, McNaughton SA, Blizzard L, Dwyer T, Venn AJ. Skipping breakfast: longitudinal associations with cardiometabolic risk factors in the Childhood Determinants of Adult Health Study. Am J Clin Nutr. 2010;92:1316–1325. doi: 10.3945/ajcn.2010.30101. [DOI] [PubMed] [Google Scholar]
- 14.Stote KS, Baer DJ, Spears K, Paul DR, Harris GK, Rumpler WV, et al. A controlled trial of reduced meal frequency without caloric restriction in healthy, normal-weight, middle-aged adults. Am J Clin Nutr. 2007;85:981–988. doi: 10.1093/ajcn/85.4.981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Odegaard AO, Jacobs DR, Jr., Steffen LM, Van Horn L, Ludwig DS, Pereira MA. Breakfast frequency and development of metabolic risk. Diabetes care. 2013;36:3100–3106. doi: 10.2337/dc13-0316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cahill LE, Chiuve SE, Mekary RA, Jensen MK, Flint AJ, Hu FB, et al. Prospective Study of Breakfast Eating and Incident Coronary Heart Disease in a Cohort of Male US Health Professionals. Circulation. 2013;128:337–343. doi: 10.1161/CIRCULATIONAHA.113.001474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Farshchi HR, Taylor MA, Macdonald IA. Deleterious effects of omitting breakfast on insulin sensitivity and fasting lipid profiles in healthy lean women. Am J Clin Nutr. 2005;81:388–396. doi: 10.1093/ajcn.81.2.388. [DOI] [PubMed] [Google Scholar]
- 18.Astbury NM, Taylor MA, Macdonald IA. Breakfast consumption affects appetite, energy intake, and the metabolic and endocrine responses to foods consumed later in the day in male habitual breakfast eaters. The Journal of nutrition. 2011;141:1381–1389. doi: 10.3945/jn.110.128645. [DOI] [PubMed] [Google Scholar]
- 19.Leidy HJ, Racki EM. The addition of a protein-rich breakfast and its effects on acute appetite control and food intake in 'breakfast-skipping' adolescents. International journal of obesity. 2010;34:1125–1133. doi: 10.1038/ijo.2010.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Farshchi HR, Taylor MA, Macdonald IA. Regular meal frequency creates more appropriate insulin sensitivity and lipid profiles compared with irregular meal frequency in healthy lean women. European journal of clinical nutrition. 2004;58:1071–1077. doi: 10.1038/sj.ejcn.1601935. [DOI] [PubMed] [Google Scholar]
- 21.Allison KC, Engel SG, Crosby RD, de Zwaan M, O'Reardon JP, Wonderlich SA, et al. Evaluation of diagnostic criteria for night eating syndrome using item response theory analysis. Eating behaviors. 2008;9:398–407. doi: 10.1016/j.eatbeh.2008.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brennan IM, Feltrin KL, Nair NS, Hausken T, Little TJ, Gentilcore D, et al. Effects of the phases of the menstrual cycle on gastric emptying, glycemia, plasma GLP-1 and insulin, and energy intake in healthy lean women. American journal of physiology Gastrointestinal and liver physiology. 2009;297:G602–610. doi: 10.1152/ajpgi.00051.2009. [DOI] [PubMed] [Google Scholar]
- 23.Cornier MA, Grunwald GK, Johnson SL, Bessesen DH. Effects of short-term overfeeding on hunger, satiety, and energy intake in thin and reduced-obese individuals. Appetite. 2004;43:253–259. doi: 10.1016/j.appet.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 24.Thomas EA, Bechtell JL, Vestal BE, Johnson SL, Bessesen DH, Tregellas JR, et al. Eating-related behaviors and appetite during energy imbalance in obese-prone and obese-resistant individuals. Appetite. 2013;65C:96–102. doi: 10.1016/j.appet.2013.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Allison DB, Paultre F, Maggio C, Mezzitis N, Pi-Sunyer FX. The use of areas under curves in diabetes research. Diabetes care. 1995;18:245–250. doi: 10.2337/diacare.18.2.245. [DOI] [PubMed] [Google Scholar]
- 26.Boden G. Interaction between free fatty acids and glucose metabolism. Current opinion in clinical nutrition and metabolic care. 2002;5:545–549. doi: 10.1097/00075197-200209000-00014. [DOI] [PubMed] [Google Scholar]
- 27.Boden G. Fatty acid-induced inflammation and insulin resistance in skeletal muscle and liver. Current diabetes reports. 2006;6:177–181. doi: 10.1007/s11892-006-0031-x. [DOI] [PubMed] [Google Scholar]
- 28.Jovanovic A, Leverton E, Solanky B, Ravikumar B, Snaar JE, Morris PG, et al. The second-meal phenomenon is associated with enhanced muscle glycogen storage in humans. Clinical science. 2009;117:119–127. doi: 10.1042/CS20080542. [DOI] [PubMed] [Google Scholar]
- 29.Suzuki K, Jayasena CN, Bloom SR. The gut hormones in appetite regulation. Journal of obesity. 2011;2011:528401. doi: 10.1155/2011/528401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reed GW, Hill JO. Measuring the thermic effect of food. Am J Clin Nutr. 1996;63:164–169. doi: 10.1093/ajcn/63.2.164. [DOI] [PubMed] [Google Scholar]
- 31.Scott CB. Resting metabolic rate variability as influenced by mouthpiece and noseclip practice procedures. The Journal of burn care & rehabilitation. 1993;14:573–577. [PubMed] [Google Scholar]
- 32.Baron KG, Reid KJ, Kern AS, Zee PC. Role of sleep timing in caloric intake and BMI. Obesity (Silver Spring) 2011;19:1374–1381. doi: 10.1038/oby.2011.100. [DOI] [PubMed] [Google Scholar]
- 33.Depner CM, Stothard ER, Wright KP., Jr Metabolic consequences of sleep and circadian disorders. Current diabetes reports. 2014;14:507. doi: 10.1007/s11892-014-0507-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Buxton OM, Cain SW, O'Connor SP, Porter JH, Duffy JF, Wang W, et al. Adverse metabolic consequences in humans of prolonged sleep restriction combined with circadian disruption. Science translational medicine. 2012;4:129ra143. doi: 10.1126/scitranslmed.3003200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Scheer FA, Hilton MF, Mantzoros CS, Shea SA. Adverse metabolic and cardiovascular consequences of circadian misalignment. Proceedings of the National Academy of Sciences of the United States of America. 2009;106:4453–4458. doi: 10.1073/pnas.0808180106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.U.S. Department of Agriculture and U.S. Department of Health and Human Services . Dietary Guidelines for Americans. 7th ed. US Government Printing Office; Washington, DC: Dec, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dhurandhar EJ, Dawson J, Alcorn A, Larsen LH, Thomas EA, Cardel M, et al. The effectiveness of breakfast recommendations on weight loss: a randomized controlled trial. Am J Clin Nutr. 2014 doi: 10.3945/ajcn.114.089573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Betts JA, Richardson JD, Chowdhury EA, Holman GD, Tsintzas K, Thompson D. The causal role of breakfast in energy balance and health: a randomized controlled trial in lean adults. Am J Clin Nutr. 2014 doi: 10.3945/ajcn.114.083402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brown AW, Bohan Brown MM, Allison DB. Belief beyond the evidence: using the proposed effect of breakfast on obesity to show 2 practices that distort scientific evidence. Am J Clin Nutr. 2013 doi: 10.3945/ajcn.113.064410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Casazza K, Fontaine KR, Astrup A, Birch LL, Brown AW, Bohan Brown MM, et al. Myths, presumptions, and facts about obesity. The New England journal of medicine. 2013;368:446–454. doi: 10.1056/NEJMsa1208051. [DOI] [PMC free article] [PubMed] [Google Scholar]