Abstract
A missing or deficient buccal alveolar bone plate is often an important limiting factor for immediate implant placement. Titanium dental implants enhanced with porous, tantalum-based trabecular metal material (PTTM) are designed for osseoincorporation, a combination of vascularized bone ingrowth and osseointegration (bone on-growth). Demineralized bone matrix (DBM) contains growth factors with good handling characteristics. However, the combination of these 2 materials in facial alveolar bone regeneration associated with immediate implant therapy has not been reported. A 65-year-old Asian woman presented with a failing central incisor. Most of the buccal alveolar bone plate of the socket was missing. A PTTM enhanced implant was immediately placed with DBM. Cone beam CT scans 12 months after the insertion of the definitive restoration showed regeneration of buccal alveolar bone. A combination of a PTTM enhanced implant, DBM, and a custom healing abutment may have an advantage in retaining biologically active molecules and form a scaffold for neovascularization and osteogenesis. This treatment protocol may be a viable option for immediate implant therapy in a failed tooth with deficient buccal alveolar bone.
INTRODUCTION
Immediate placement of an endosseous implant into a fresh extraction socket has been demonstrated to be an effective and successful treatment comparable to an implant placed in a healed site.1–9 Advancements in cone beam computed tomography (CBCT) have allowed the accurate placement of implants with a flapless surgical protocol,10–13 shown to maintain periimplant soft tissue and hard tissue and to minimize postsurgical complications,14 perhaps through preserving periosteum that supplies blood to the buccal tissue.15 Improving the implant surface roughness has proved to be better than machined surface implants in terms of improving bone on-growth or osseointegration.16,17 However, the modifications for the most part only improve the surface roughness in 2 dimension.18 Recently, a modification of the surface with porous tantalum trabecular metal (PTTM) was introduced.16,18,19 PTTM material is 80% porous with bone-like microstructures and a modulus of elasticity similar to bone.20 PTTM-enhanced Ti dental implants increase the implant surface area by nearly 70%. The PTTM portion allows both bone on-growth and in-growth, known as osseoincorporation.18 Autografts or autogenous grafts are the gold standard for all graft materials. Unfortunately harvesting autogenous grafts is not always possible.21 Allografts have proven to be a clinically acceptable alternative to autografts without complications from a donor site.21 Demineralized bone allografts retain the organic portions of the allografts, including growth factors such as bone morphogenic proteins (BMPs). With immediate implant placement, usually, if intact facial and lingual plates are present and if the gap between the implant and the socket is within 3 to 4 mm, no grafting is necessary.22,23 In practice, the facial plate is often missing, and, instead of placing an immediate implant, clinicians often choose to graft the socket or preserve the site. The integrity of the facial plate is viewed as one of the most important factors in determining whether immediate implant placement is appropriate.23–30 This clinical report demonstrates a protocol for immediately placing dental implants in sockets with compromised facial plates and for regenerating the facial bone with minimal surgical intervention.
CLINICAL REPORT
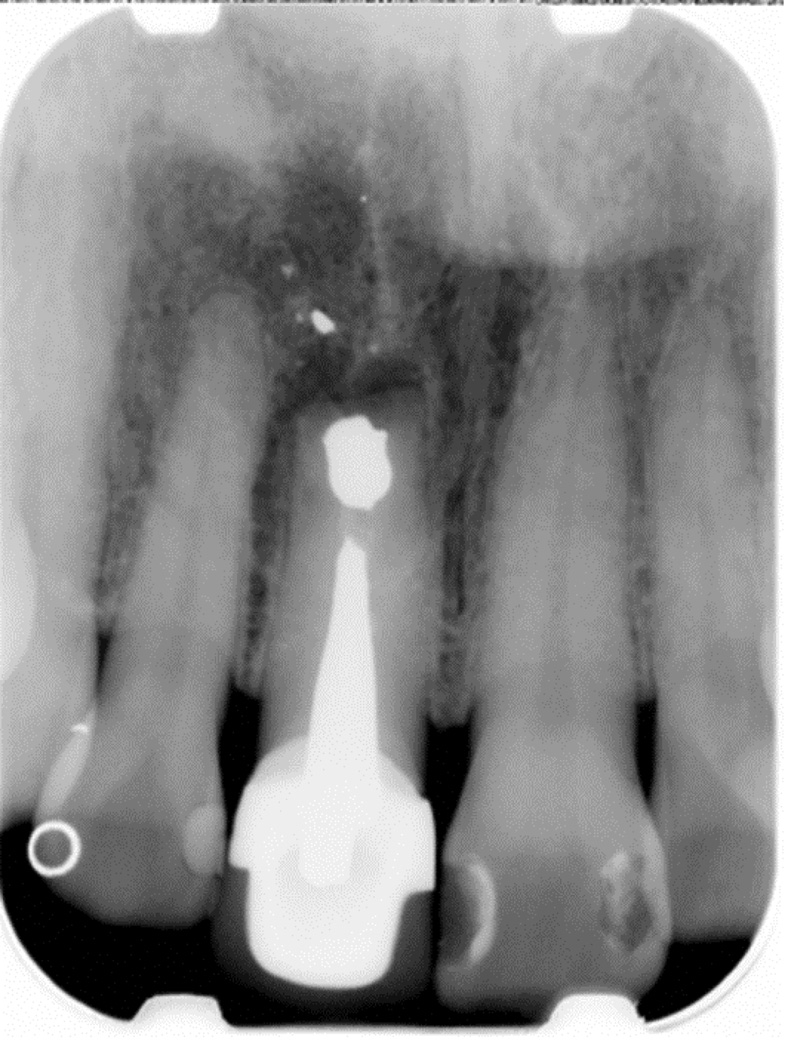
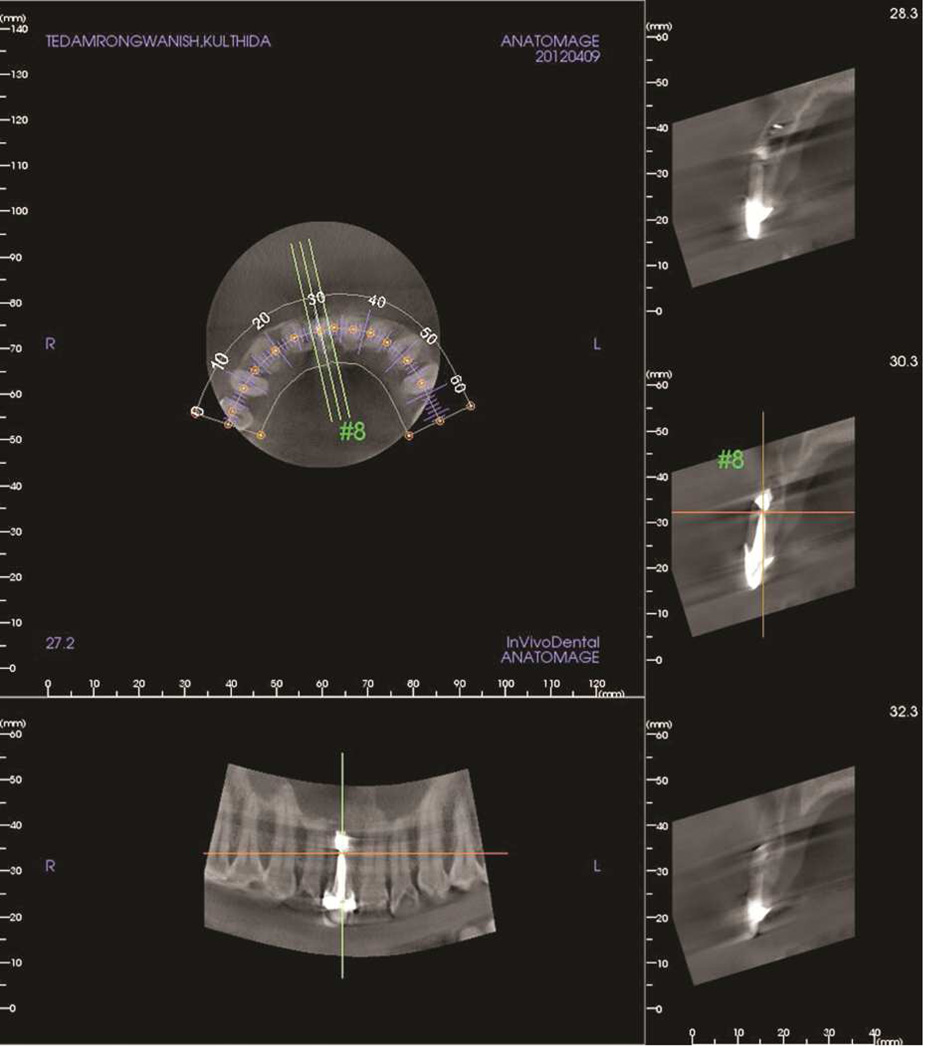
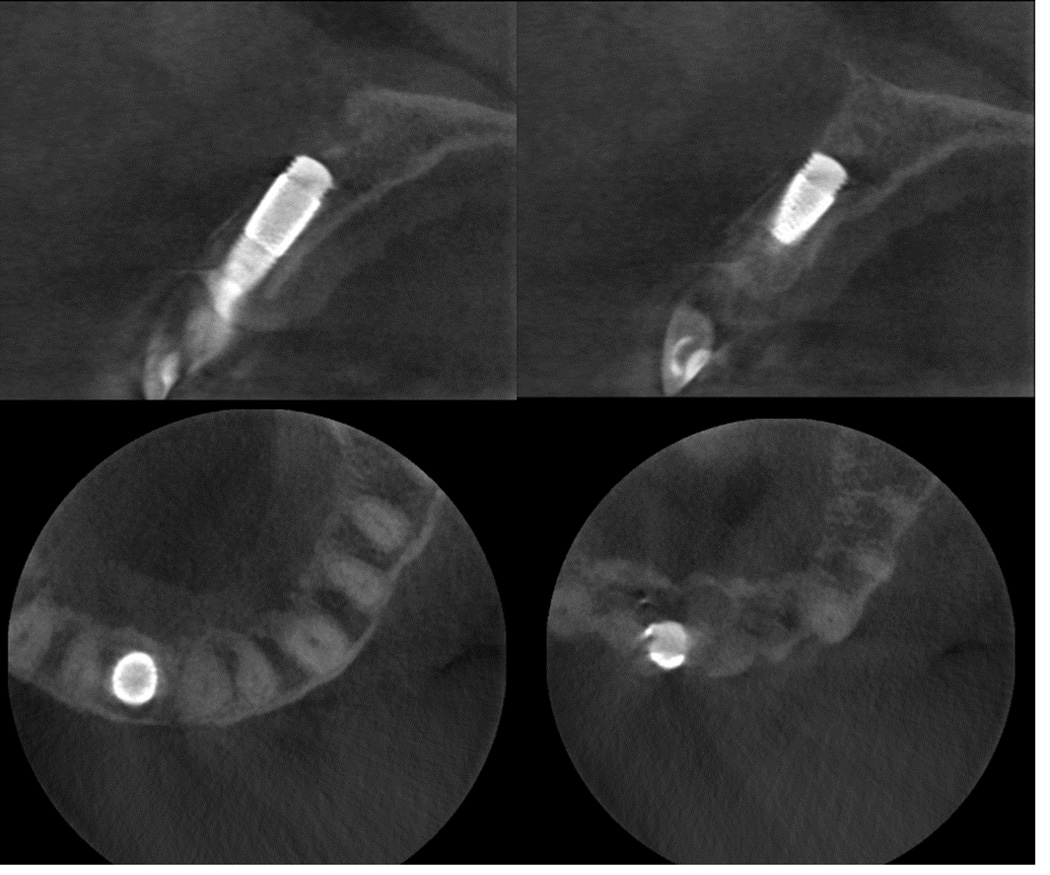
A 65-year-old Asian woman presented to the University of North Carolina at Chapel Hill Dental Faculty Practice with her chief complaint being, “One of my front teeth is black. Sometimes I feel pus coming out of the gum.” The maxillary right central incisor had a history of conventional endodontic treatment and later endodontic surgery. The patient had been periodically taking antibiotics, but the fistula tract had never resolved. The patient was in good general health, with no contraindications for implant therapy. The clinical examination showed that the tooth had a facial pocket of approximately 8 mm; however, a thick facial keratinized tissue was noted. The facial tissue of the tooth appeared enlarged and dark, with a fistula tract in the apical area. The tooth had been restored with a metal ceramic crown that was asymptomatic (Fig. 1A-C). A periapical radiograph revealed the tooth had a metal post and core, gutta percha endodontic obturation, and an amalgam apical restoration. CBCT scans were made (Kodak 9000 CBCT scanner; Kodak Dental Systems, Carestream Health). The CBCT scans showed that the apical lesion connected to the labial fistula tract and no intact facial plate as noted for the majority of the facial root surface (Fig. 1D). A diagnosis of chronic apical periodontitis of an unrestorable tooth was made. Different treatment options were discussed along with the risks and benefits of each procedure. The patient elected the option of extraction, immediate implant placement, grafting, and delayed implant restoration.
Fig. 1.
Preoperative photographs and radiographs. A, Maxillary right central incisor with facial fistula tract. B, Palatal view. C, Periapical radiograph. D, CBCT scans showing no radiographic sign of buccal alveolar bone.
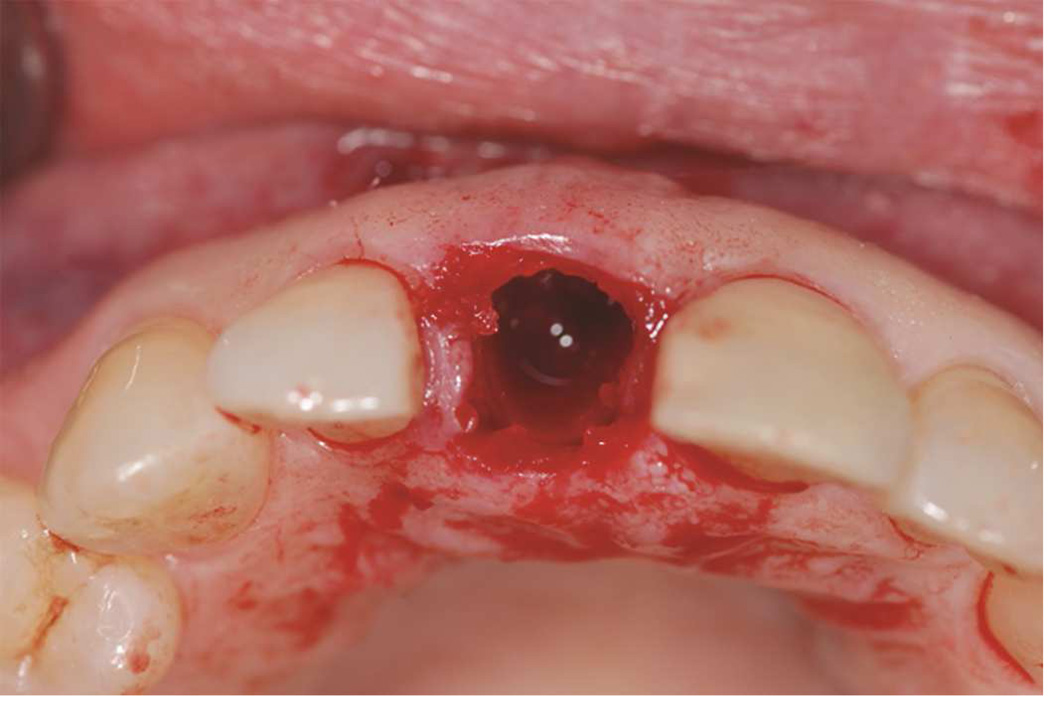
The tooth was extracted with minimal trauma. The buccal socket defect depth was about 13 mm midbuccal measured from the top of the midbuccal gingival margin, 10 mm mesially and 8 mm distally, measured from the mesial and distal interdental papillae. The palatal plate and proximal bone, however, were mostly intact (Fig. 2). Implant placement consisted of a single drill approach.30 The final drill (4.4mm/3.8 mm in diameter) was positioned against the palatal wall of the socket without contacting the facial tissue, and the osteotomy was prepared to the appropriate length, 13 mm from the top of the palatal bone. The osteotomy site was tapped with the implant bone tapper (4.7 mmD Bone Tap; Zimmer Dental Inc) to create the implant threading in the palatal bone. This ensured the implant position palatal to the buccal defect and left sufficient buccal room for grafting material. Demineralized bone matrix putty with cortical and cancellous bone chips (Puros Demineralized Bone Matrix Putty; Zimmer Dental Inc) was placed in the socket. A PTTM-enhanced titanium (Ti) implant (Zimmer Dental Inc) was threaded into the socket by engaging only the palatal wall of the prepared osteotomy (Fig. 3). Despite the facial plate defect, the implant had good primary stability with insertion torque of approximately 50 Ncm. A custom healing abutment was fabricated from an interim abutment (Zimmer Dental Inc) and bis-acryl resin (Integrity; Dentsply Caulk). The custom healing abutment was fabricated to fit inside the socket with a smooth polished surface and slightly concave emergence profile. A maxillary interim partial removable dental prosthesis was delivered after adjusting the cervical portion of the denture tooth to fit the custom abutment (Fig. 4). The patient was advised to wear the interim prosthesis overnight but, after the first night, to wear it only during the day.
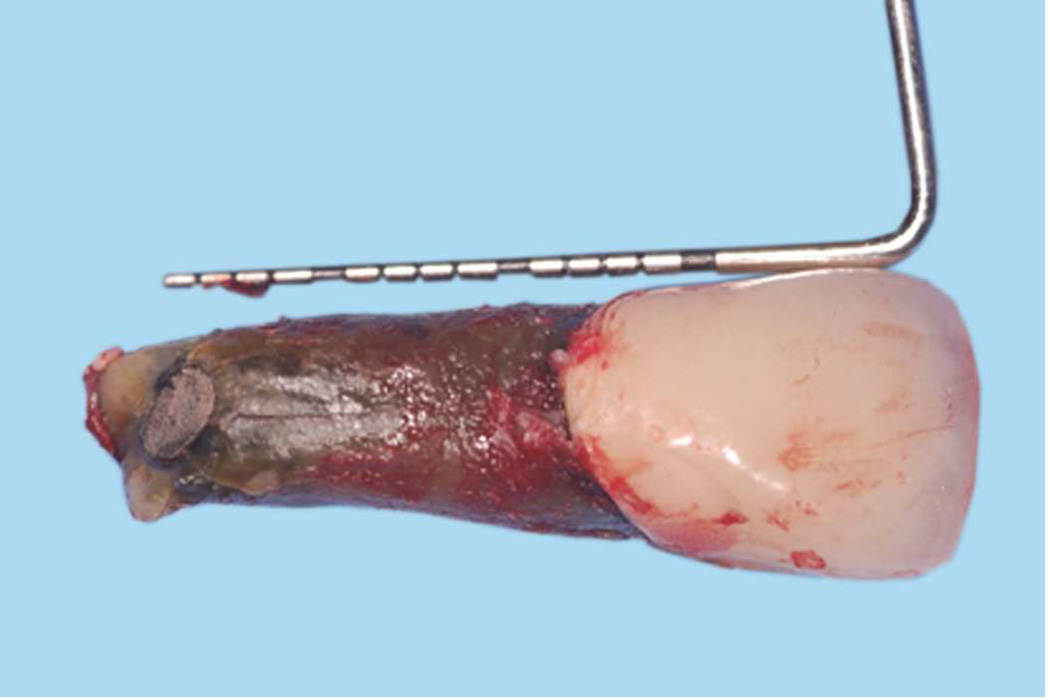
Fig. 2.
Extraction and socket examination. A, Extracted tooth. B, Facial view with buccal alveolar bone missing (note tissue displacement when pushing with Perioprobe. C, Occlusal view. D, Measurement of palatal bone height, about 3–4 mm from palatal gingival margin.
Fig. 3.
Socket grafting and implant placement procedure. A, With final drill for osteotomy preparation, socket was prepared to about 13 mm from most cervical part of palatal bone (approximately 16 mm from palatal gingival margin). B, DBM material was placed into socket. C, Implant in place with implant insertion device (Fixture mount). D, Final implant position.
Fig. 4.
Interim abutment and prosthesis. A, Custom healing abutment in place. B, Interim partial removable dental prosthesis. D, Facial and palatal view of interim prosthesis in place.
Chlorhexidine mouth rinse (twice a day for 2 weeks) and Amoxicillin (500 mg 4 times a day for 7 days) were prescribed. The patient was also advised to use acetaminophen or ibuprofen as needed for pain. No narcotics were prescribed. In addition, a soft diet and cold temperature food were prescribed for the 48 hours after the surgery. The patient was scheduled for monitoring at 1 week (Fig. 5), and 1 month after the surgery. Definitive impressions were made at 2 months after the surgery. Three months after the surgery (Fig. 6), a definitive custom computer-aided design and computer-aided manufacturing (CAD/CAM) zirconia abutment (Atlantis; Astratech/Dentsply) was delivered and tightened to 25 Ncm. A definitive ceramic CAD/CAM lithium disilicate crown (IPS e.max; Ivoclar Vivadent) was luted onto the abutment with resin cement (RelyX Unicem; 3M ESPE). Periapical radiographs were made at the surgery visit, 3-month recall/definitive impression visit, and after delivery of the definitive restoration (Fig. 7 A-C). Follow-up CBCT scans was made at 6 months after the delivery of the definitive restoration (Fig. 7D) to evaluate the regenerated facial plate. The implant restoration maintained optimal soft tissue contour and esthetics (Fig. 7E). No clinical mobility of the implant was detected with minimal probing depth (approximately 0.5 to 2 mm).
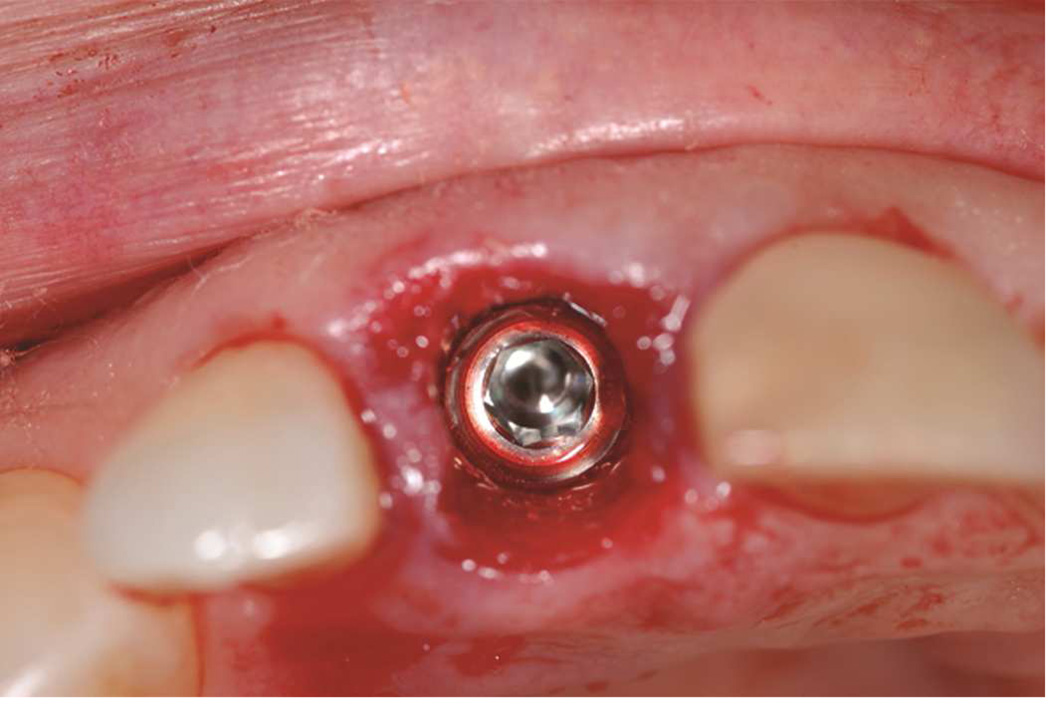
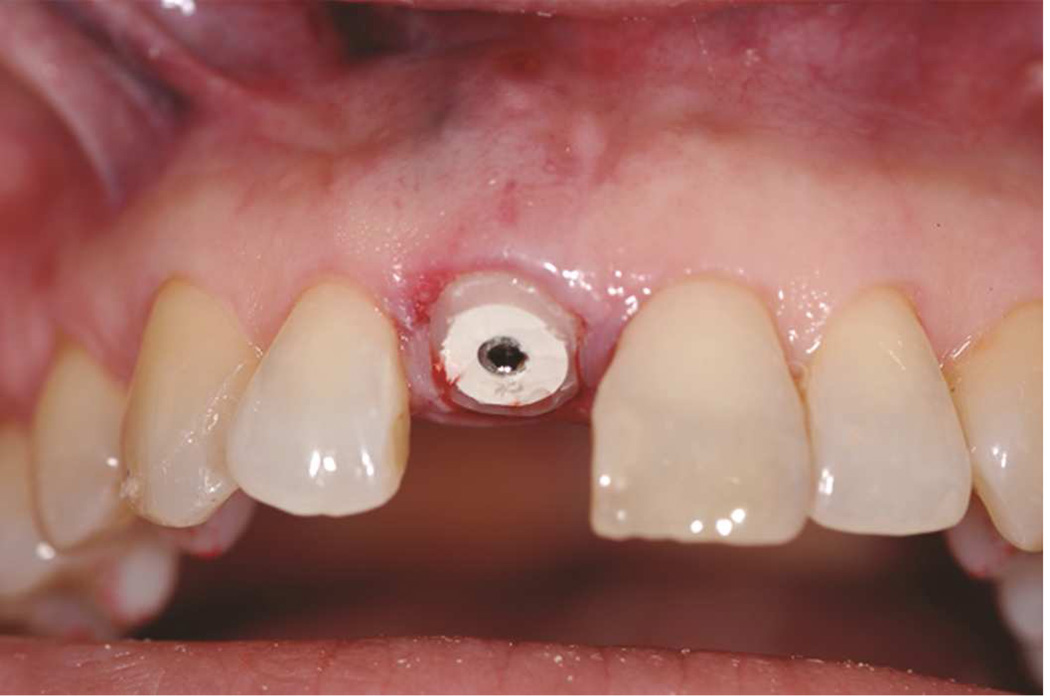
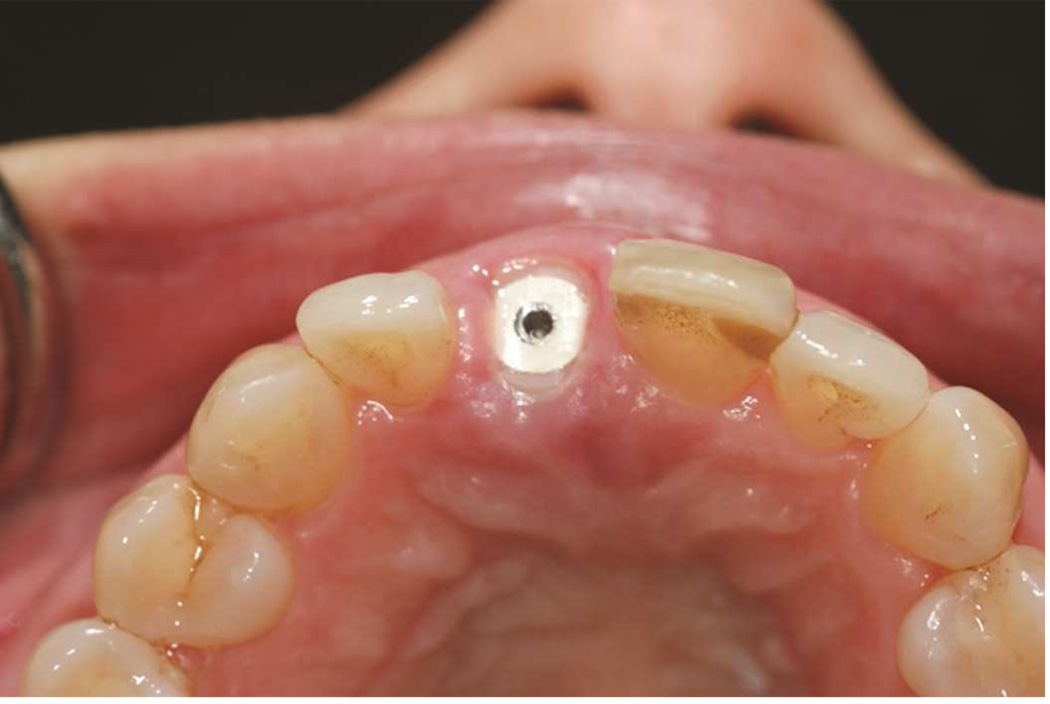
Fig. 5.
One week after surgery. A, Frontal view. Healing of fistula tract and maintenance of soft tissue were noted. B, C, Facial and palatal views of soft tissue around custom healing abutment. D, Close-up view of soft tissue esthetics.
Fig. 6.
Definitive prosthesis. A, CAD/CAM zirconia custom abutment in place with polyvinyl siloxane placed in the abutment screw access. B, C, Facial and palatal views of luted definitive ceramic crown. D, Frontal view of smile.
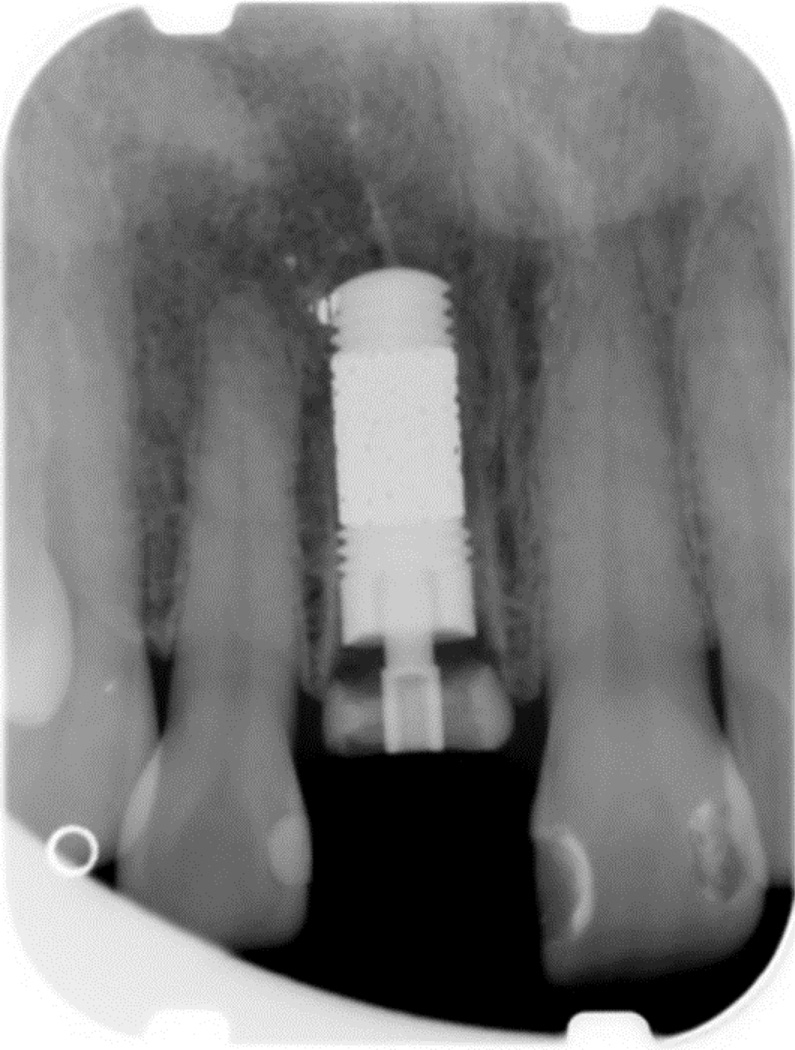
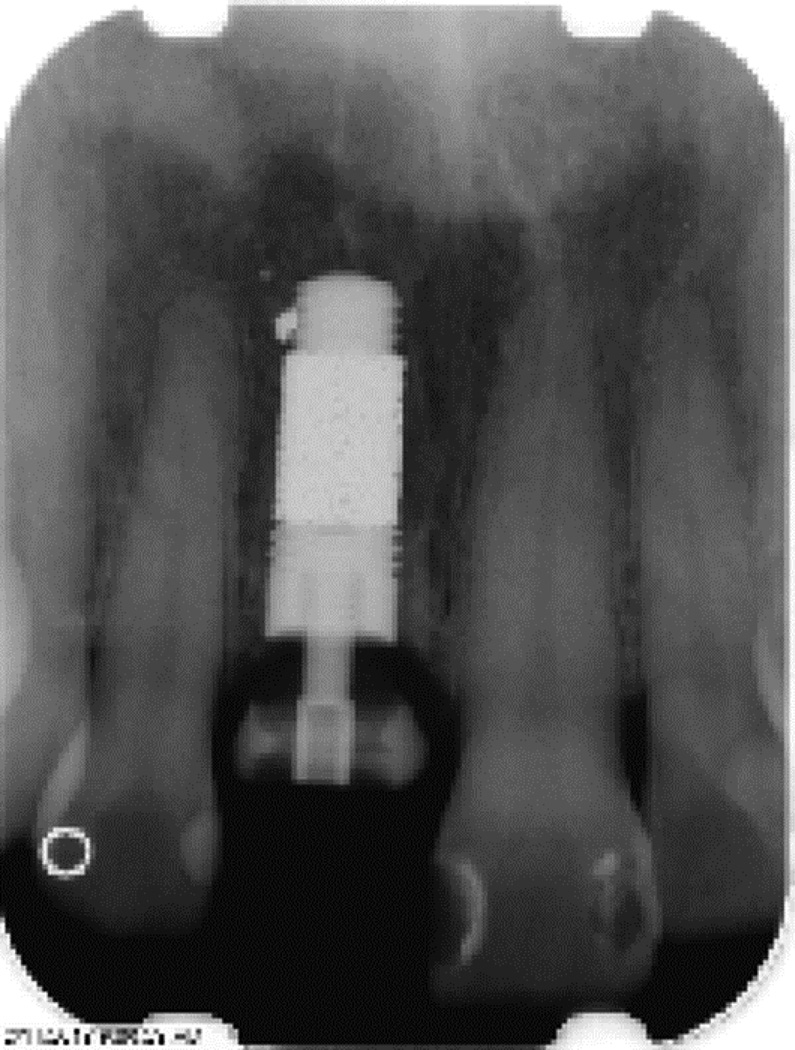
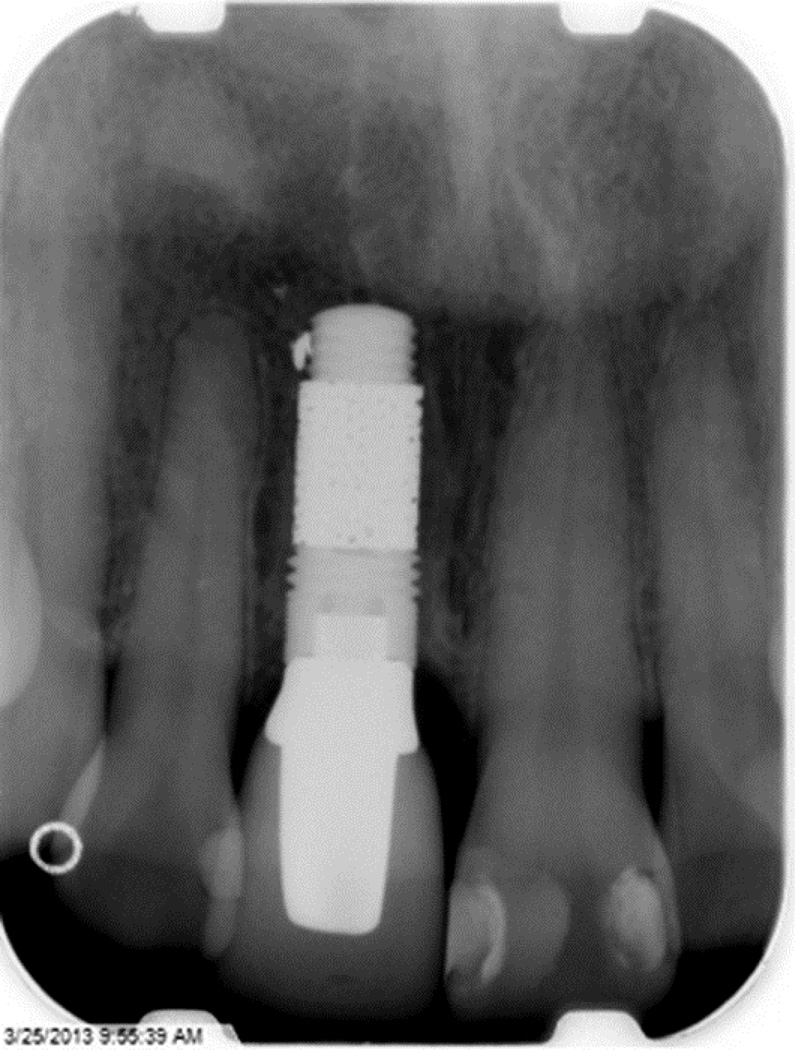
Fig. 7.
Postoperative radiographs. A, Immediately after surgery. B, 3 months after surgery. C, At insertion of definitive crown. D, Facial view of definitive restoration at 6-month-recall visit. E, CBCT scans approximately 6 months after definitive crown insertion.
DISCUSSION
This clinical report may be the first to demonstrate the regeneration of the facial plate after extraction and immediate implant placement with DBM and a PTTM-enhanced Ti dental implant. The key to success in this patient might be attributed to a combination of factors, including the flapless surgical procedure, DBM graft material, PTTM-enhanced Ti implant, and the custom healing abutment. First, the flapless procedure has been documented to provide a better blood supply to the implant site especially when it is used in conjunction with extraction and immediate implant placement.10,15 Second, the demineralized bone matrix (DBM) has been shown to have both osteoinduction and vascular induction through BMPs, the vascularized growth factor (VEGF), and other growth factors, such as fibroblast growth factor, insulin-like growth factor, platelet-derived growth factor, and TGF-β.21,31–37 DBM is easy to handle when used with immediate implant placement. The material flows into the gap between the implant fixture and the socket. Third, PTTM provides an excellent environment for first clot formation, neovascularization18 and later a scaffold for bone regeneration in a 3-dimensional manner through osseoincorporation.18 Finally, the clots, grafting, and implant were protected with the custom healing abutment and the interim partial removable dental prosthesis. Note that the apical portion of the implant appears to have a fenestration. This may be the result of the positioning of the implant fixture or the large defect from endodontic surgery that may need more time to mature and mineralize. This protocol provides optimal protection for the clot formation, minimizes the irritation from the oral environment, and protects the implant from excessive occlusal loading. Waiting for 3 months before loading the implant also allows completion of bone regeneration.
CONCLUSION
This review and clinical report proposes a hypothesis that extraction and immediate implant placement can be successfully performed even when buccal alveolar bone is missing. A combination of DBM, a PTTM-enhanced Ti implant, custom healing abutment, and interim partial removable dental prosthesis may have provided an optimal environment for buccal alveolar bone regeneration and osseoincorporation, preserved the buccal blood supply, enhanced neovascularization, and controlled occlusal loading. This protocol should be used with caution in selected patients. A future longitudinal study is needed to confirm whether this protocol can be applied to the general population.
Acknowledgement
The authors thank the members of the University of North Carolina at Chapel Hill Dental Faculty Practice where clinical work was done. The work of author SB was partly supported by the American Academy of Implant Dentistry Foundation, the American College of Prosthodontists Educational Fund, the the National Institutes of Health (NIH) grant HL092338, and the University of North Carolina at Chapel Hill Junior Faculty Award. The Matthew Wood Prosthodontics Award supported author WCB.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Statement of conflicts of Interests
There was no direct compensation for this review and Zimmer Dental Inc has no role in the writing and publication of this manuscript. However, author SB is a Zimmer Institute lecturer. In addition, Zimmer Dental Inc does not directly support salary for any authors; however, Zimmer Dental Inc was supporting the work of author SB through unrestricted research and educational grants.
REFERENCES
- 1.Chen ST, Wilson TG, Jr, Hammerle CH. Immediate or early placement of implants following tooth extraction: review of biologic basis, clinical procedures, and outcomes. Int J Oral Maxillofac Implants. 2004;19(Suppl):12–25. [PubMed] [Google Scholar]
- 2.Amler MH. The time sequence of tissue regeneration in human extraction wounds. Oral Surg Oral Med Oral Pathol. 1969;27:309–318. doi: 10.1016/0030-4220(69)90357-0. [DOI] [PubMed] [Google Scholar]
- 3.Boyne PJ. Osseous repair of the postextraction alveolus in man. Oral Surg Oral Med Oral Pathol. 1966;21:805–813. doi: 10.1016/0030-4220(66)90104-6. [DOI] [PubMed] [Google Scholar]
- 4.Evian CI, Rosenberg ES, Coslet JG, Corn H. The osteogenic activity of bone removed from healing extraction sockets in humans. J Periodontol. 1982;53:81–85. doi: 10.1902/jop.1982.53.2.81. [DOI] [PubMed] [Google Scholar]
- 5.Lekovic V, Kenney EB, Weinlaender M, Han T, Klokkevold P, Nedic M, et al. A bone regenerative approach to alveolar ridge maintenance following tooth extraction. Report of 10 cases. J Periodontol. 1997;68:563–570. doi: 10.1902/jop.1997.68.6.563. [DOI] [PubMed] [Google Scholar]
- 6.Lekovic V, Camargo PM, Klokkevold PR, Weinlaender M, Kenney EB, Dimitrijevic B, et al. Preservation of alveolar bone in extraction sockets using bioabsorbable membranes. J Periodontol. 1998;69:1044–1049. doi: 10.1902/jop.1998.69.9.1044. [DOI] [PubMed] [Google Scholar]
- 7.Camargo PM, Lekovic V, Weinlaender M, Nedic M, Vasilic N, Wolinsky LE, et al. A controlled re-entry study on the effectiveness of bovine porous bone mineral used in combination with a collagen membrane of porcine origin in the treatment of intrabony defects in humans. J Clin Periodontol. 2000;27:889–896. doi: 10.1034/j.1600-051x.2000.027012889.x. [DOI] [PubMed] [Google Scholar]
- 8.Iasella JM, Greenwell H, Miller RL, Hill M, Drisko C, Bohra AA, et al. Ridge preservation with freeze-dried bone allograft and a collagen membrane compared to extraction alone for implant site development: a clinical and histologic study in humans. J Periodontol. 2003;74:990. doi: 10.1902/jop.2003.74.7.990. [DOI] [PubMed] [Google Scholar]
- 9.Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent. 2003;23:313–323. [PubMed] [Google Scholar]
- 10.Givens E, Bencharit S, Byrd WC, Hosseini B, Phillips C, Tyndall D. Immediate placement and provisionalization of implants into sites with periradicular infection with and without antibiotics: An exploratory study. J Oral Implantol. 2013 doi: 10.1563/AAID-JOI-D-13-00002. in press. [DOI] [PubMed] [Google Scholar]
- 11.Chen ST, Buser D. Clinical and esthetic outcomes of implants placed in postextraction sites. Int J Oral Maxillofac Implants. 2009;24(Suppl):186–217. [PubMed] [Google Scholar]
- 12.Del Fabbro M, Ceresoli V, Taschieri S, Ceci C, Testori T. Immediate loading of postextraction implants in the esthetic area: systematic review of the literature. Clin Implant Dent Relat Res. 2013 doi: 10.1111/cid.12074. in press. [DOI] [PubMed] [Google Scholar]
- 13.Marcelis K, Vercruyssen M, Naert I, Teughels W, Quirynen M. Model-based guided implant insertion for solitary tooth replacement: a pilot study. Clin Oral Implants Res. 2012;23:999–1003. doi: 10.1111/j.1600-0501.2011.02242.x. [DOI] [PubMed] [Google Scholar]
- 14.Noelken R, Neffe BA, Kunkel M, Wagner W. Maintenance of marginal bone support and soft tissue esthetics at immediately provisionalized OsseoSpeed implants placed into extraction sites: 2-year results. Clin Oral Implants Res. 2013 doi: 10.1111/clr.12069. in press. [DOI] [PubMed] [Google Scholar]
- 15.Kim JI, Choi BH, Li J, Xuan F, Jeong SM. Blood vessels of the peri-implant mucosa: a comparison between flap and flapless procedures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:508–512. doi: 10.1016/j.tripleo.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 16.Kim DG, Huja SS, Tee BC, et al. Bone ingrowth and initial stability of titanium and porous tantalum dental implants: a pilot canine study. Implant Dent. 2013;22:399–405. doi: 10.1097/ID.0b013e31829b17b5. [DOI] [PubMed] [Google Scholar]
- 17.Trisi P, Marcato C, Todisco M. Bone-to-implant apposition with machined and MTX microtextured implant surfaces in human sinus grafts. Int J Periodontics Restorative Dent. 2003;23:427–437. [PubMed] [Google Scholar]
- 18.Bencharit S, Byrd WC, Altarawneh S, et al. Development and Applications of Porous Tantalum Trabecular Metal-Enhanced Titanium Dental Implants. Clin Implant Dent Relat Res. 2013 doi: 10.1111/cid.12059. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schlee M, van der Schoor WP, van der Schoor AR. Immediate Loading of Trabecular Metal-Enhanced Titanium Dental Implants: Interim Results from an International Proof-of-Principle Study. Clin Implant Dent Relat Res. 2013 doi: 10.1111/cid.12127. in press. [DOI] [PubMed] [Google Scholar]
- 20.Lakstein D, Backstein D, Safir O, Kosashvili Y, Gross AE. Trabecular Metal cups for acetabular defects with 50% or less host bone contact. Clin Orthop Relat Res. 2009;467:2318–2324. doi: 10.1007/s11999-009-0772-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Giannoudis PV, Dinopoulos H, Tsiridis E. Bone substitutes: an update. Injury. 2005;36(Suppl 3):S20–S27. doi: 10.1016/j.injury.2005.07.029. [DOI] [PubMed] [Google Scholar]
- 22.Tarnow DP, Chu SJ. Human histologic verification of osseointegration of an immediate implant placed into a fresh extraction socket with excessive gap distance without primary flap closure, graft, or membrane: a case report. Int J Periodontics Restorative Dent. 2011;31:515–521. [PubMed] [Google Scholar]
- 23.Becker W, Becker BE, Hujoel P. Retrospective case series analysis of the factors determining immediate implant placement. Compend Contin Educ Dent Oct. 2000;21:805–808. 810-801, 814 passim; quiz 820. [PubMed] [Google Scholar]
- 24.Lang NP, Pun L, Lau KY, Li KY, Wong MC. A systematic review on survival and success rates of implants placed immediately into fresh extraction sockets after at least 1 year. Clin Oral Implants Res. 2012;23(Suppl 5):39–66. doi: 10.1111/j.1600-0501.2011.02372.x. [DOI] [PubMed] [Google Scholar]
- 25.Covani U, Chiappe G, Bosco M, Orlando B, Quaranta A, Barone A. A 10-year evaluation of implants placed in fresh extraction sockets: a prospective cohort study. J Periodontol. 2012;83:1226–1234. doi: 10.1902/jop.2012.110583. [DOI] [PubMed] [Google Scholar]
- 26.Waasdorp JA, Evian CI, Mandracchia M. Immediate placement of implants into infected sites: a systematic review of the literature. J Periodontol. 2010;81:801–808. doi: 10.1902/jop.2010.090706. [DOI] [PubMed] [Google Scholar]
- 27.Javed F, Romanos GE. The role of primary stability for successful immediate loading of dental implants. A literature review. J Dent. 2010;38:612–620. doi: 10.1016/j.jdent.2010.05.013. [DOI] [PubMed] [Google Scholar]
- 28.Juodzbalys G, Sakavicius D, Wang HL. Classification of extraction sockets based upon soft and hard tissue components. J Periodontol. 2008;79:413–424. doi: 10.1902/jop.2008.070397. [DOI] [PubMed] [Google Scholar]
- 29.Vignoletti F, Matesanz P, Rodrigo D, Figuero E, Martin C, Sanz M. Surgical protocols for ridge preservation after tooth extraction. A systematic review. Clin Oral Implants Res. 2012;23(Suppl 5):22–38. doi: 10.1111/j.1600-0501.2011.02331.x. [DOI] [PubMed] [Google Scholar]
- 30.Hosseini B, Byrd W, Preisser JS, Khan A, Duggan D, Bencharit S. Effects of Antibiotics on Bone and Soft Tissue Healing Following Immediate Single-tooth Implant Placement into Sites with Apical Pathology. J Oral Implantol. 2014 doi: 10.1563/aaid-joi-D-14-00075. in press. [DOI] [PubMed] [Google Scholar]
- 31.Emad B, Sherif el M, Basma GM, Wong RW, Bendeus M, Rabie AB. Vascular endothelial growth factor augments the healing of demineralized bone matrix grafts. Int J Surg. 2006;4:160–166. doi: 10.1016/j.ijsu.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 32.Moore ST, Katz JM, Zhukauskas RM, Hernandez RM, Lewis CS, Supronowicz PR, et al. Osteoconductivity and osteoinductivity of Puros(R) DBM putty. J Biomater Appl. 2011;26:151–171. doi: 10.1177/0885328210366061. [DOI] [PubMed] [Google Scholar]
- 33.Toolan BC. Current concepts review: orthobiologics. Foot Ankle Int. 2006;27:561–566. doi: 10.1177/107110070602700715. [DOI] [PubMed] [Google Scholar]
- 34.De Long WG, Jr, Einhorn TA, Koval K, McKee M, Smith W, Sanders R, et al. Bone grafts and bone graft substitutes in orthopaedic trauma surgery. A critical analysis. J Bone Joint Surg Am. 2007;89:649–658. doi: 10.2106/JBJS.F.00465. [DOI] [PubMed] [Google Scholar]
- 35.El-Chaar ES. Demineralized bone matrix in extraction sockets: a clinical and histologic case series. Implant Dent. 2013;22:120–126. doi: 10.1097/ID.0b013e3182859869. [DOI] [PubMed] [Google Scholar]
- 36.Gruskin E, Doll BA, Futrell FW, Schmitz JP, Hollinger JO. Demineralized bone matrix in bone repair: history and use. Adv Drug Deliv Rev. 2012;64:1063–1077. doi: 10.1016/j.addr.2012.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chen B, Lin H, Zhao Y, Wang B, Zhao Y, Liu Y, et al. Activation of demineralized bone matrix by genetically engineered human bone morphogenetic protein-2 with a collagen binding domain derived from von Willebrand factor propolypeptide. J Biomed Mater Res A. 2007;80:428–434. doi: 10.1002/jbm.a.30900. [DOI] [PubMed] [Google Scholar]