Abstract
Introduction
Cardiovascular prevention is more effective if started early in life, but available interventions to promote healthy lifestyle habits among youth have been ineffective. Impulsivity in particular has proven to be an important barrier to the adoption of healthy behaviors in youth. Observational evidence suggests that mindfulness interventions may reduce impulsivity and improve diet and physical activity. We hypothesize that mindfulness training in adjunct to traditional health education will improve dietary habits and physical activity among teenagers by reducing impulsive behavior and improving planning skills.
Methods/Design
The Commit to Get Fit study is a pilot cluster randomized controlled trial examining the feasibility, acceptability and preliminary efficacy of school-based mindfulness training in adjunct to traditional health education for promotion of a healthy diet and physical activity among adolescents. Two schools in central Massachusetts (30 students per school) will be randomized to receive mindfulness training plus standard health education (HE-M) or an attention-control intervention plus standard health education (HE-AC). Assessments will be conducted at baseline, intervention completion (2 months), and 8 months. Primary outcomes are feasibility and acceptability. Secondary outcomes include physical activity, diet, impulsivity, mood, body mass index, and quality of life.
Conclusions
This study will provide important information about feasibility and preliminary estimates of efficacy of a school-delivered mindfulness and health education intervention to promote healthy dietary and physical activity behaviors among adolescents. Our findings will provide important insights about the possible mechanisms by which mindfulness training may contribute to behavioral change and inform future research in this important area.
Keywords: Mindfulness, diet, physical activity, school-based interventions, adolescents
1. INTRODUCTION
Unhealthy dietary habits and physical inactivity are important modifiable risk factors for the development of cardiovascular disease, the leading cause of death in the United States and worldwide. (1) Both habits are often established during adolescence and are highly prevalent among teenagers. (2) There is mounting evidence that poor diet and sedentary lifestyle early in life lead to the premature development of the metabolic syndrome (3) and contribute to the early development of atherosclerosis. (4, 5) Conversely, the establishment of healthy dietary and physical activity habits in youth leads to significant health benefits in adulthood, thus highlighting the need to develop programs aimed at improving dietary and physical activity habits early in life. (6) Such programs, however, have had modest effects, and there is limited knowledge on how to maintain positive changes over time. (7–9) A possible reason is that adolescents underestimate the long-term consequences of unhealthy behaviors (10) and are thus not motivated to adopt a healthy lifestyle. In addition, adolescence is a time of expanding freedom and boundaries testing, often resulting in impulsive behaviors that undermine efforts at engaging in health-supporting behaviors. Unhealthy behaviors (including poor diet and lack of exercise) in adolescents have been in fact associated with impulsivity and poor planning skills. (11, 12)
Mindfulness training is a behavioral intervention aimed at developing an increased awareness of the moment-to-moment experience of mental events and physical sensations. (13) There is preliminary evidence suggesting a role of mindfulness training in promoting healthy behaviors in youth, possibly through a reduction in impulsiveness. Observational studies conducted among college students have linked higher mindfulness levels with healthier dietary and exercise behaviors (14, 15) and with lower impulsiveness. (16, 17) The role of mindfulness training in promoting healthy behaviors among younger teens, however, has been so far fairly unexplored.
This pilot study proposes to evaluate the feasibility, acceptability, and preliminary efficacy of a novel approach using mindfulness training to promote and maintain healthy dietary and physical activity behaviors among adolescents. The primary outcomes of this study are feasibility and acceptability. We hypothesize that 1) we will be able to meet our recruitment goals within the specified time frame, 2) no more than 20% of participants will drop out of the study, and 3) at least 80% of participants will indicate high acceptability ratings in program evaluations. Secondary aims include preliminary assessments of efficacy on physical activity, dietary behaviors, impulsivity, mood, sedentary behaviors and quality of life. We posit that the addition of mindfulness training to a health education program, compared to a health education program alone, will improve diet and physical activity, and these changes will be maintained over time. In addition, we expect to observe a decrease in impulsivity, indicating impulsivity may serve as a potential mediator of the effect of the intervention on diet and physical activity.
2. MATERIALS AND METHODS
2.1. Study design
The “Commit to Get Fit” study (Clinicaltrials.gov NCT01975896) is a pilot cluster randomized clinical trial designed to evaluate the feasibility, acceptability, and preliminary estimates of efficacy of health education plus mindfulness training compared to health education plus attention control for the promotion of physical activity and healthy dietary behavior among adolescents.
2.2. Setting
The study will be conducted at two high schools located in central Massachusetts that offer health education classes as part of their 9th grade school curriculum. We selected schools with similar key characteristics, i.e. socioeconomic level and ethnic diversity of their student body (more than 40% of students belong to non-white minorities). We chose a school setting for a number of reasons. First, the majority of adolescents (over 95%) attend school, (18) making a school-based program easily accessible to adolescents. Second, health education classes are taught in 9th grade in more than 60% of schools in Massachusetts and throughout the US, thus providing a natural venue for delivering information regarding healthy diet and physical activity and providing training in mindfulness. (19) Third, a program conducted within the school setting and integrated with the academic curriculum does not place additional time or transportation burdens on the students and their families. Developing and testing mindfulness training within existing health education programs in schools provides a model with high dissemination potential.
2.3. Population
We will recruit a convenience sample of 9th grade students (n = 30 per school) from health education classes. We chose this particular age group because this is an emerging adult population, transitioning from the parental control typical of childhood to a phase in which teens begin to make their own independent choices, including dietary and physical activity choices. (20) Another reason for targeting adolescents is that unhealthy dietary and physical activity habits are often established during adolescence. (2) Currently available educational programs have had only modest effects on dietary and physical activity behaviors, and mixed results on weight and body-mass index. (7–9) The combination of the increasing prevalence of unhealthy dietary and physical activity behaviors and the limitations of currently available interventions suggest a critical need for interventions targeting these unhealthy behaviors in this population.
The study sample will likely reflect the gender and ethnicity distribution of students at the selected high schools, where minorities are well represented (40% of students). Students will be considered eligible for the study under the following conditions: 1) Enrolled in 9th grade; 2) No prior mindfulness training; and 3) English speaking with at least one English speaking parent/guardian. Students will be excluded if any of the following conditions is present: 1) Planning to move out of the area within the next 8 months; 2) Unable or unwilling to provide informed assent (adolescent) and consent (parent); 3) A diagnosis of a serious psychiatric illness during the past 5 years; and 4) Developmental delay that would prevent study participation.
2.4. Recruitment
Schools will serve as the primary vehicle for reaching parents or guardians of potentially eligible students. A letter will be sent to school principals and health education teachers explaining the purpose and benefits of the project, and requirements for student participation. Investigators and research staff will meet with the school principals and health education teachers to explain the purpose and significance of the study. Recruitment packets containing an informational brochure, eligibility criteria, and parental informed consent and adolescent assent forms will be mailed to parents or given to students to take home. For logistical reasons and to avoid singling out students participating in the study, all students will receive the study interventions as part of their health education curriculum, while only those consenting/assenting will complete study assessments and receive study stipends. Enrollment in the study will be on a “first come, first served” basis; namely, students returning consent/assent forms first will be enrolled until we reach our planned sample size.
2.5. Screening and consent/assent procedures
Interested students who returned a signed parental consent form will be invited to a screening visit with the Project Director in the school nurse’s office, similar to the approach successfully used by the investigators in prior school-based trials. (21, 22) Assent will be explained such that students understand they have a right to refuse to participate and that their school evaluations will not be affected by whether or not they decide to enroll in the study. The informed consent and assent process will not identify the condition in which the students will be enrolled so that students will not have prior knowledge of which condition they may be assigned, thereby reducing the potential for selection bias. The proposed study will be explained in detail, along with the participant’s role in it and the confidentiality of all collected information, including the digital recording of the intervention sessions for treatment fidelity assessments. The Project Director will be responsible for obtaining assent and consent and will address any question the adolescent may have. Assent and consent will be requested from and signed by the adolescent and parent. Once student assent and parental consent are obtained and eligibility is confirmed, the student will be enrolled in the study and follow the protocol for their school condition.
2.6. Randomization
To avoid intra-school contamination between the two interventions, we will use a cluster design where each school is the unit of randomization, rather than randomizing individual students. Schools will be randomized to one of two conditions: Health Education plus Attention Control (HE-AC) or Health Education plus Mindfulness training (HE-M).
2.7. Retention plan
We will collect address, phone, and email information from participants as well as from three contacts to ensure we will be able to reach participants for follow-up study assessments at the end of intervention (2 months post-baseline) and at 8 months follow-up (end of academic year). Tracking procedures will be implemented for those not attending a scheduled study visit or not accessible by phone or e-mail. In addition, students will receive a $20 incentive at each data collection completion and an additional $20 for their participation in the final focus group. The Committee for the Protection of Human Subjects at the University of Massachusetts Medical School approved the study protocol and all study materials (Docket H-00002904).
2.8. Study interventions
Both interventions will be delivered during the time allocated for health education classes at each school. This choice has the advantage of integrating the interventions into the students’ regular school day. Furthermore, health education classes are taught in 9th grade in more than 60% of schools in Massachusetts and throughout the US, (19) thus providing a wide platform for dissemination should efficacy be demonstrated in a future phase III efficacy trial.
Students in both conditions will receive the same dose and content of health education (one session each week for 8 weeks). In addition to health education classes, students in the school allocated to the HE-M condition will receive one 35-minute session of mindfulness training per week for 8 weeks, while students in the school allocated to the HE-AC condition will receive one 35-minute “attention control” session for 8 weeks, with no active component delivered.
Health Education
The health education intervention will be delivered by existing health education teachers, one at each school (total of 2 teachers). Prior to the start of the health education classes we will hold regular meetings with the two health education teachers to produce a manualized version of the intervention. The health education curriculum will be informed by materials developed as part of a previous study conducted by our group to improve diet and physical activity among adolescents. The curriculum will be based on the Diabetes Prevention Program (DPP) lifestyle intervention (22, 23) as well as on standard curricula for school-based health education programs with particular attention to the unique needs of adolescents. (24) (25) Topics will include increasing the intake of fruits and vegetables, reducing sugar sweetened drinks, and decreasing the intake of foods high in fat, unhealthy carbohydrates, and calories. Additional topics will include managing hunger and appetite, structuring meals to include a healthy breakfast, portion sizes, and eating out in a healthy way. The physical activity curriculum will be based on current recommendations about physical activity in youth (26), such as engaging in at least 1 hour of moderate-to-vigorous physical activity most days of the week, importance of building physical activity into the teen’s lifestyle, (27) and reducing sedentary behavior. Prior to the beginning of the study, the health education intervention will be standardized and manualized in collaboration with the health education teachers at both schools. The health education curriculum and materials will include a detailed, standardized lesson plan as well as a student booklet.
Mindfulness Training
The mindfulness instructor will be a graduate of the Center for Mindfulness professional training program with significant experience in teaching mindfulness among teenagers as well as with a current personal mindfulness practice. Only one instructor will deliver the mindfulness intervention for the HE-M condition throughout the study. The instructor will receive three hours of training including review and discussion of the intervention script and of treatment fidelity procedures.
The mindfulness intervention is aimed at developing and increasing mindfulness skills among teenagers. The curriculum of the intervention is based on an adaptation of the traditional Mindfulness Based Stress Reduction Program (13) to a school setting and to an in-class delivery format. The intervention will focus on two main practices:
Practice of attention focusing techniques such as the awareness of breath exercise and body scan exercise. To avoid jargon, these techniques will be called “awareness of breath” (AOB) and “awareness of sensations” (AOS) exercises. These exercises will be the focus of the first 1–4 sessions/weeks of training;
Practice of techniques aiming at widening the focus of attention from one single object of attention (the breath or physical sensations in the body) to different objects. This will be the focus of the second part of the training (session/weeks 5–8). Whenever possible, practical and every day life examples will be used to illustrate and clarify a particular technique within a context that is meaningful for teen-agers.
Briefly, the mindfulness intervention’s curriculum will include the following components: 1) the AOS exercise, a technique based on the cultivation of attention to bodily sensations that normally go unnoticed; 2) training in the awareness of the sensations of breathing; 3) training in directing the attention to simple activities of daily life: sounds, visual objects, thoughts and emotions, and in recognizing when the attention is no longer focused on that specific object of attention; 4) practice of ‘open awareness’ in which students will be instructed to just notice which events (physical sensation, sound, visual object, thought) their attention is spontaneously drawn to from moment to moment; and 5) mindful movement (standing and walking exercises).
An outline of the mindfulness intervention with a description of the content of each session is provided in Table 1. The instructor will follow the intervention outline in regard to topics introduced at each session as well as their sequence. Q&A sessions are deliberately left open.
Table 1.
Mindfulness intervention outline
|
Session 1: Introduction to mindfulness training - Awareness of Breath (AOB)
| |
| TOPIC | DURATION (minutes) |
| Instructor to start by introducing herself | |
| • Why are we doing this? Introduction and discussion | 10 |
| • Awareness of Breath (AOB) exercise | 5 |
| • Q&A | 10 |
| • AOB (let’s do it again) | 5 |
| • Give MP3s/CDs to students | |
| • Set up for home practice: How do you do it? How do you set up for success? When is the best time of the day for you? | 5 |
| • Students encouraged to practice AOB exercise during the following week with aid of digital recording - track 1 once a day | |
Teaching tip: The following points can be used to initiate/sustain discussion:
| |
|
| |
|
Session 2: AOB/daily experience
| |
| • Q&A related to practice in previous week | 10 |
| • Awareness of daily experience: exercise of paying attention to everyday activity (raisin exercise). This exercise subtly hints at “dietary habits” and connects students to pay attention to what they “take in” | 5 |
| • Q&A/introduce informal practice | 10 |
| • AOB exercise | 10 |
| • Students encouraged to practice AOB exercise during the following week with aid of digital recording - track 1 once a day | |
|
| |
|
Session 3: Awareness of Sensations (AOS)
| |
| • Q&A related to practice in previous week | 10 |
| • AOS: Students instructed to move awareness to different parts of the body in a systematic way, beginning with the toes and progressing to the top of the head, noticing whatever sensations happen to be present in that part of the body at that moment. Do both sides of the body at once – and do not focus on individual digits. End with short AOB exercise. | 15 |
| Teaching tip: A flashlight with a beam may be a good way to introduce AOS practice. First shifting the light in the room. The beam can be directed to different parts of the body to show shift of attention. | |
| • Q&A | 10 |
| • Students encouraged to practice AOS exercise during the following week with aid of digital recording - track 2 once a day | |
|
| |
|
Session 4: Introducing Everyday Practice/Awareness of Body Movement (ABM)
| |
| • Q&A related to practice in previous week | 10 |
| • Glass of water or other non-alcoholic drink – exercise of mindful drinking (This exercise subtly hints at “dietary habits” and connects students to pay attention to what they “take in”) | |
| Teaching tip: Point out to students that we are learning to become aware of activities that occur daily, but are not noticed. For example, when we are very thirsty, we are totally aware of the experience of drinking water. Now, we are learning to pay attention to the entire process of “drinking” …picking up the glass, the first sip, etc. | 5 |
| • Q&A | 10 |
| • AOB exercise, short AOS exercise - introduce ABM through guided standing or walking practice | 10 |
| • Students encouraged to practice AOS exercise during the following week with aid of digital recording - track 2 once a day | |
|
| |
|
Session 5: AOB/AOS/ABM/Awareness of Sounds
| |
| • Q&A related to practice in previous week | 10 |
| • Short AOB, short AOS + ABM, followed by awareness of sounds exercise | 15 |
| Teaching tip: Possible to introduce awareness of sounds with a few musical instruments, then open to ambient sounds. Explain what observing means: the sound itself (qualities like loud, soft, sudden…); the “naming”; the reaction to the sound (memories, associations, emotions…) | |
| • Q&A | 10 |
| • Students instructed to practice this way of relating to their experience throughout the day and particularly to their experience of sounds. Students encouraged to practice with aid of digital –recording – track 3 once a day. | |
| Teaching tip: Give examples. They can do this by stopping and listening, and opening to the sounds that are present in the environment at a given moment. They can try listening to a whole song this way. | |
|
| |
|
Session 6: AOB/AOS/Awareness of Emotions
| |
| • Q&A related to practice in previous week | 10 |
| • Short AOB, short AOS, followed by awareness of emotions exercise (observing the physical sensations, memories… associated with the emotion) | 15 |
| • Q&A | |
| Teaching tip: A range of emotions needs to be included here. Those that are easy, those that are difficult. Familiar emotions, and the possibility of exploring a wider range of emotions that you have, but don’t notice. | 10 |
| • Students instructed to practice this mindful way of relating to their experience throughout the day and particularly to their experience of emotions. Students encouraged to practice with aid of study CD – track 3 once a day. | |
|
| |
|
Session 7: AOB/AOS/Thoughts
| |
| • Q&A related to practice in previous week | 10 |
| • Short AOB, short AOS, followed by awareness of thoughts exercise (observing the physical sensations, memories, emotions… associated with the thought) | |
| Teaching tip: Offering the power of different thoughts— The thoughts of not being good enough, popular, or thoughts of being a caring, kind person. How do thoughts affect you? Get to know them more closely. They are not all true, but beginning to become familiar with them, is a source of great power in your life. You can see more clearly that you are more than your thoughts! | 15 |
| • Q&A | 10 |
| • Students instructed to practice this mindful way of relating to their experience throughout the day and particularly to their experience of thoughts. Students encouraged to practice with aid of study CD– track 3 once a day. | |
|
| |
|
Session 8: Open Awareness
|
|
| • Q&A related to practice in previous week | 10 |
| • Short AOB, short AOS, sounds, emotions, thoughts, open awareness. Students instructed to notice where the attention goes when it is not directed with open awareness. | |
| Teaching tip: Metaphor of ocean and waves may be helpful. Like the ocean -- knowing the waves of sensation, thoughts, emotions, but also being the large, deep water. Allowing yourself to be still and know yourself despite all the coming and going, wanting and being satisfied…despite all the changes, we have the ability to attend, to know what is happening as it is happening. | 15 |
| • Q&A | 10 |
| • Students asked to practice this mindful way of relating to their experience during the day, and to bring this resource to all their experiences (pleasant and unpleasant ones). Instruct student to keep practicing with or without recording once a day. | |
In addition to the weekly training session with the mindfulness instructor, students will practice mindfulness with the guidance of a 15 minute digitally recorded guided mindfulness practice CD or MP3, consistent with the techniques learned during each session with the instructor. Students will practice daily in class for 15 minutes and will be instructed to practice for an additional 15 minutes at home.
Attention Control
The attention control intervention (HE-AC condition) is designed to control for the non-specific components associated with the mindfulness intervention (i.e., attention received by the instructor, additional time spent in discussion and interaction with classmates). The attention control intervention will match the mindfulness intervention for duration and frequency. Its content will not include any active component of either health education (i.e., diet and physical activity) or mindfulness training and will include topics chosen by the health educators as feasible for the health education classroom setting. These include discussions and classroom activities regarding the 5 components of wellness (mental, spiritual, physical, emotional, energetic), health risk factors identified by the CDC, strategies for increasing one’s health literacy, improving one’s self-confidence, self-esteem, and resiliency, and mental and emotional health.
A summary of all study–related activities, including schedule for intervention delivery in each school is shown in Table 2.
Table 2.
Study-related activities
| Baseline | Weekly (week 1–8) | Week 9 | 6 months of follow-up | |
|---|---|---|---|---|
| Study Interventions | ||||
| 45 minute Health Education (both HE-M and HE-AC) | x | |||
| 35 minute mindfulness session in class (HE-M only) | x | |||
| Listening to mindfulness recording in class (HE-M only) | x | |||
| Listening to mindfulness recording at home (HE-M only) | x | |||
| 35 minute AC intervention (HE-AC only) | x | |||
| Feasibility and Acceptability (primary outcome) | ||||
| Recruitment metrics | x | |||
| Retention | x | x | ||
| Session attendance | x | |||
| Mindfulness practice logs | x | |||
| Program satisfaction scale | x | |||
| Focus groups (students) | x | |||
| Debriefing session (HE teachers) | x | |||
| Secondary Outcomes | ||||
| 24 hours dietary recalls | x | x | x | |
| Accelerometry | x | x | x | |
| 7-Days PAR | x | x | x | |
| Weight, height, BMI | x | x | x | |
| Quality of life | x | x | x | |
| Sedentary behaviors | x | x | x | |
| Mediators | ||||
| Impulsivity | x | x | x | |
| Mindfulness | x | x | x | |
| Knowledge | x | x | x | |
| Self-efficacy | x | x | x | |
| Stress | x | x | x | |
| Mood & anxiety | x | x | x | |
| Covariates/Moderators | ||||
| Socio-demographics | x | |||
| Medical history | x | |||
| Parental control on dietary and exercise choices | x | |||
| Quality Control | ||||
| Audit of 10% tapes of mindfulness training (HE-M only) | x | |||
| Health education checklist (HE-M and HE-AC) | x | |||
2. 9. Safety considerations
While we do not anticipate serious adverse events or side effects given the educational nature of the health education curriculum, the behavioral nature of the mindfulness intervention and the lack of report of severe side effects with mindfulness training, we will actively monitor the possible occurrence of adverse events. Potential untoward events include muscle soreness, pain, and musculoskeletal injuries as a result of the mindful movement practiced during sessions and emotional discomfort during mindfulness practice. Mindful movement includes simple stretching exercises and walking meditation that are safely practiced by older age groups with minimal risk. Students will be instructed to wear comfortable clothes and shoes during classes; and the mindfulness instructor will actively supervise the students during these exercises. Psychological distress during mindfulness practice rarely occurs in the absence of ongoing serious psychiatric conditions. The mindfulness instructor will actively inquire at the beginning and during each class about psychological side effects, and the students will be instructed to inform the mindfulness instructor should any discomfort arise during the training. Mindfulness instructors are experienced and trained on how to help individuals presenting with such issues. If a student presents signs of psychological discomfort during or between sessions, the student will be excused from participating in the mindfulness component of the health education class.
2.10. Primary outcomes
All assessments will be performed at baseline, at the end of the intervention (2 months post-baseline), and at 8 months of follow-up (6 months after intervention completion and also the end of the academic year). A chart of the study assessments is presented in Table 2.
Feasibility
We will measure recruitment rates, retention rates, and intervention adherence. Recruitment metrics will include number of screened and eligible participants, number of eligible students who refused to participate, and reasons for refusal. Retention measures will be the number of subjects who dropped out or were lost to follow-up and reason(s) for dropping out. As for adherence, we will collect information on class attendance and on the number of times the adolescent listened to the study MP3 recording on their own by means of a self-reported mindfulness log that students will receive at enrollment and which will be collected by the health education teacher each week.
Acceptability
At the end of the intervention we will conduct a focus group with participants in the HE-M condition to obtain feedback on the interventions and on their participation in the study. Topics will include the students’ opinions regarding the health education and mindfulness training sessions and materials; instructor-led mindfulness sessions and individual and in-class mindfulness practice; the effectiveness of the mindfulness instructor and health education teachers; perceived barriers to participating in the in-class mindfulness sessions on and individual mindfulness practice; and feedback and recommendations for study recruitment strategies. On a survey following the intervention, each teen will also complete a form rating the overall satisfaction with the program on a scale ranging from 1 (not at all) to 5 (very much). A debriefing session will be conducted with the two heath education teachers to assess the teachers’ overall opinion about the study and obtain feedback about recruitment strategies, study assessments, the health education curriculum, barriers to implementation, and incentives recommended for the involvement of health education teachers in a future larger study.
2.11. Secondary outcomes
Physical activity
Physical activity will be measured using accelerometry (Actigraph, LLC, Fort Walton Beach, FL) Model GT1M(28). Accelerometry has been recommended for the assessment of physical activity among teens and children, (28) has high reliability, (29) and has shown good correlations with measured oxygen uptake (30, 31). Students will receive an accelerometer at each study visit and will be instructed to wear the accelerometer for the next 7 days, and then to return it to the health education teacher for study staff to collect. For adolescents, wearing an accelerometer for longer periods of time is problematic, as we repeatedly experienced in our previous studies involving teenagers. We thus decided to compromise on a 7-day period. There is very limited information on accelerometer reactivity effects among children and adolescents, with a recent manuscript reporting higher activity on the first day the accelerometer is worn. (32) The extent of reactivity, however, was much larger in younger (pre-school) children than that in adolescents (such as those enrolled in our study). (32) Furthermore, since both HE and M-HE students will wear accelerometers in our study, we expect reactivity effects to be similar in both groups. The following metrics will be considered: number of valid days, wearing time, average counts/min, average counts/day, average minutes of moderate-to-vigorous physical activity /day, and average minutes of moderate-to-vigorous physical activity bouts per day. The Physical Activity Recall Questionnaire (33) will also be collected and used as a backup for accelerometer failure or missing data.
Diet
We will use 24-hour dietary recalls (validated with adolescents and children) to assess total calorie intake, saturated fat, and fruit/vegetables intake. The prevalence of teens meeting current recommendations (34) for diet and physical activity will also be assessed.
2.12. Other secondary outcomes of interest
Body mass index (BMI)
Trained research staff will collect measures of height and weight to calculate BMI using standard methodology. Weight measurements will be taken on digital scales and measured to the nearest 2/10th of a pound. Heights will be measured to the nearest 1/8th of an inch using portable stadiometers, without shoes. Measures will be converted to the metric scale. BMI will be calculated from weight (kg)/height squared (in meters) and BMI-z score for age/sex determined using CDC growth charts.
Quality of life will be measured using the Pediatric Quality of Life Inventory. (35)
Sedentary behaviors will include self-reported assessments of the average number of hours the teen spent watching TV, at the computer or playing non-active video games.
2.13. Mediators
Impulsivity will be measured using the Barratt impulsivity scale, (36) modified to exclude items not applicable to adolescents (e.g., “I plan for job security”, “I change jobs”) and to adapt some items to make them more relevant for teens (e.g., “I am restless at the theater or lectures” changed to “I am restless at the movie theatre or in class”).
Mindfulness will be evaluated using the Mindful Attention Awareness Scale, (37, 38) an instrument that has been validated in healthy teens. One item that does not apply to this specific age group (“I drive places on ‘automatic pilot’ and then wonder why I went there”) has been deleted.
Knowledge will be assessed through an ad-hoc survey containing specific questions on dietary recommendations, physical activity, and sedentary behavior.
Diet and exercise self-efficacy will be measured using a one-item questionnaire adapted from the Go Girls study (39).
Stress will be evaluated using the Perceived Stress Scale, 4-items measuring the teen’s stress level over the past month. (40)
Depression will be measured by the Children’s Depression Inventory, a 6-item measure that screens for depressive symptoms, assessed over the past month. (41)
Anxiety will be assessed using the State-Trait Anxiety Inventory for Children. (42)
2.14. Covariates
We will collect socio-demographic information (age, gender, ethnicity, socio-economic status), medical history (previous medical and psychiatric health conditions, current medications, smoking); and information about the youth’s perception of the level of parental control on dietary habits, healthy food availability, and exercise choices (modified questionnaire based on Parental Control Index). (43, 44)
2.15. Process measures
The protocols and materials for each intervention will be refined and manualized in order to ensure that the delivery of the interventions is consistent across mindfulness instructors and health education teachers.
Fidelity assessments will be conducted following the guidelines developed by the Treatment Fidelity Workgroup. (45) For the mindfulness curriculum, the mindfulness instructor will digitally record each session and complete the auditor checklist corresponding to that class at the end of each session. A random selection of 10% of all recordings will be reviewed after each weekly session and feedback provided to the instructor before the next scheduled session. Optimal treatment fidelity would be evidenced by 100% of objectives met. If less than 85% of objectives are met, the auditor will provide remediation as needed. For the health education curriculum delivered in both study conditions, clear lesson plans were developed to standardize delivery of the curriculum to the students. To assess fidelity to delivery of the health education intervention, the health education teachers will complete a structured form to record whether or not the planned topics were discussed during each health education session.
2.16. Data collection
Measurements of weight and height and accelerometer fitting will be performed in the school nurse’s office; dietary recalls will be conducted over the phone while the student is at home. Study surveys will be completed at school and will be pre-tested to ensure the time burden does not exceed 45 minutes. Research Electronic Data capture (REDCap) technology will be used for direct data entry from study participants during the interviews. (46) REDCap employs automatic checks for values that are out of range or represent errors of logic. Outliers will be corrected with verification from participants.
Data management
We will program the system with validation rules at the time of entry and develop programs to perform comprehensive edits after the data have been submitted to the main database. These edits will check for validity, consistency, and normal range values both within and between forms. Edit queries will be generated and resolved with corrections posted to the database through the REDCap system, which enforces an audit trail for all changes. For analysis, data will be exported from the REDCap system as SAS© data sets and merged within SAS© to create the official analysis files for the study using SAS© statistical software version 9.2. (47). All data analysis personnel will be blinded to group assignment.
2.17. Statistical analyses
All analyses will be performed according to the intention to treat approach. (48)
Feasibility
Separately for each treatment group (school), we will estimate rates of retention, adherence, and acceptability scores (dichotomized at 80+%) at 2 and 8 months, accounting for within-class clustering and dependence over time using generalized estimating equation (GEE) logistic regression. (49) Correlates will be identified by including candidate predictors in the logistic regression models. For qualitative analyses we will use NVivo© qualitative data analysis software, QSR International Pty Ltd. Version 9, 2010 to import transcribed data, conduct thematic analyses, identify common themes in participants’ responses, sort responses according to themes and summarize findings. (50, 51)
Diet and physical activity
We expect that the HE-M group, compared to HE-AC, will have greater changes since baseline in healthy diet indicators (total calorie, saturated fat and fruit/vegetable intake), and in physical activity (accelerometer counts) at the end of the intervention; these changes will be maintained over time (at 8 months follow-up). To obtain preliminary estimates of efficacy at key time points HE-M versus HE-AC differences will be estimated for change since baseline diet and using linear mixed models (52) with a random effect for class to account for clustering, with fixed effects treatment group, time point (categorized as 2 and 8 months), and their interaction, adjusting for baseline outcome values to account for possible regression to the mean. (53) Baseline variables predictive of the outcome being modeled will be included as covariates. (54, 55) Similar models will be estimated for the other secondary outcomes (continuous variables).
Exploratory analyses
Mediators
We posit that the HE-M intervention, compared to HE-AC, will increase mindfulness skills; changes in mindfulness skills will be associated with a decrease in impulsivity; and a decrease in impulsivity will be positively associated with changes in diet and physical activity. We will use linear mixed modeling (to incorporate clustering within class) to examine the mediation hypothesized above.
Moderators
We will explore whether the effect of the intervention differs by gender, baseline levels of physical activity and dietary intake of certain nutrients, baseline BMI (under-normal weight, overweight, obese), and categorized levels of perceived parental control on dietary and physical activity choices. Interactions of these characteristics with treatment group will be added one at a time to models for Aim 2.
Sample size considerations
Since pilot studies do not provide meaningful estimates of effect sizes for planning subsequent large randomized controlled trials due to the imprecision inherent in data from small samples, (56, 57) our proposed sample size of 30 students per condition/school was based on practical consideration (costs and duration of funding). Estimates of intra-class correlation from our prior studies of mindfulness interventions for hot flashes (58) range from 0.0105 for within-mindfulness class to 0.027 for within-school (change in BMI from our previous study of obese adolescents)(22); taking a conservative approach and using the 0.027 multiplied by 50% to account for possibly higher intra-class correlation in a class than in an entire school, the resulting design effect is 1+[0.027 × 1.5 × (20−1)] = 1.77, (59) giving an effective sample size of 40/1.77 = 23 per condition/school. Based on our prior studies with adolescents in school settings, we anticipate at least 80% retention. Thus, a conservatively wide 95% confidence interval for retention rate per condition is 80% ± 15.7%, equal 64.4%, 95.7%. 3.
DISCUSSION
Mindfulness has been defined as the act of “paying attention to the present moment’s experience in an intentional and non-judgmental way”. (60) Studies have shown that mindfulness skills can be improved and refined with training and dedicated practice and such increases in mindfulness in turn result in a variety of beneficial effects on psychological distress, pain, and other important health outcomes. (61, 62)
An area of inquiry that has received limited attention is the possible effect of mindfulness training on health behaviors. In adults, mindfulness training may promote healthier eating habits by increasing awareness of eating and satiety cues. (63) Preliminary studies, however, have shown that overall, mindfulness interventions alone have a modest (64) or null effect on the dietary intake of several nutrients. (65, 66) In contrast, composite interventions including mindfulness training and a dietary intervention increased vegetable protein and fiber intake and decreased total energy and saturated fat intake. (67, 68) Likewise, mindfulness training delivered together with an exercise and dietary intervention has been shown to significantly increase activity levels. (67)
The literature is likewise relatively silent regarding the possible effect of mindfulness training on health habits among younger populations. Preliminary evidence based on observational studies suggests that mindfulness training may play a role in promoting behavioral change in adolescents. For example, higher dispositional mindfulness (i.e., the capacity that individuals have to be mindful prior to training)(69, 70) has been associated with increased physical activity, reduced binge eating episodes and better sleep quality (14) as well as with healthier dietary habits and greater diet self-efficacy. (15)
There are a number of reasons why mindfulness training could have an effect on promoting healthy behaviors in youth. In this age group, unhealthy behaviors such as poor diet quality, sedentariness, and low physical activity levels appear strongly associated with poor self-regulation and high impulsivity. (11, 12, 71, 72) In addition, high impulsivity has been associated with overweight and obesity and with measures of abdominal adiposity. (12) Mindfulness training typically emphasizes the development of a particular type of attention, namely the intentional and non-judgmental acceptance of thoughts, feelings, and sensations arising in the field of consciousness at any given moment. This particular way of paying attention is the very opposite of impulsivity and in fact, dispositional mindfulness has been associated with lower impulsivity and better self-control in youth (16), which are both important determinants of healthy behaviors in younger populations. (11, 12, 71)
The objective of the present study is to explore whether mindfulness may play a role in promoting behavioral change. Specifically, “Commit To Get Fit” seeks to study the role of mindfulness training in promoting healthy diet and physical activity among adolescents. Our working hypothesis is that mindfulness training will increase mindfulness levels, which in turn will be associated with lower impulsivity, and that improvement in impulsivity will be associated with positive changes in dietary and physical activity habits (Figure 1).
Figure 1.
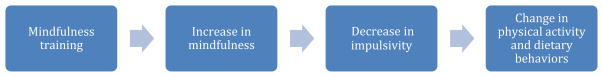
Conceptual model
We considered other models to guide the design of this study, for example, the transactional model of stress, which is typically used in mindfulness interventions in adults. (73, 74) While this model may apply to the smaller subgroup of adolescents with high perceived stress (75, 76) and psychiatric disorders (77–79) it is unlikely that it will be relevant for the majority of adolescents, who have no anxiety and normal levels of stress. We will however collect information about these important outcomes and explore effect modification by stress and anxiety/depression levels.
In conclusion, this is the first experimental study to explore the role of mindfulness training in the promotion and maintenance of healthy physical activity and dietary habits among adolescents. An additional innovation of the study is the delivery of mindfulness training in the context of existing health education classes in the school setting. This is a notable strength of this study, because it ensures the scalability of the intervention to other high schools if a future phase III efficacy RCT yields positive results. If this preliminary study is feasible and gives us preliminary indications that the HE-M intervention is effective, our next step will be to conduct a large, cluster, 2 × 2 factorial RCT that will rigorously evaluate whether mindfulness plus health education, or either alone, compared to an attention control group, can improve diet and physical activity in adolescents. This future study will also have statistical power to include a full mediation analysis to assess the role of change in mindfulness and impulsivity on maintenance of healthy dietary and exercise habits. We will also consider including a functional magnetic resonance component to test possible neuro-physiological mechanisms underlying the effect of the mindfulness intervention.
Acknowledgments
This project was funded by a grant from the National Institutes of Health (R21 HL119665) to Drs. Pbert and Salmoirago-Blotcher. The funding agency had no involvement in the study design; in the collection, analysis and interpretation of data; in the writing of this report; and in the decision to submit this article for publication.
Footnotes
Conflicts of interest
None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, et al. Executive summary: heart disease and stroke statistics--2013 update: a report from the American Heart Association. Circulation. 2013;127(1):143–52. doi: 10.1161/CIR.0b013e318282ab8f. [DOI] [PubMed] [Google Scholar]
- 2.Wardle J, Jarvis MJ, Steggles N, Sutton S, Williamson S, Farrimond H, et al. Socioeconomic disparities in cancer-risk behaviors in adolescence: baseline results from the Health and Behaviour in Teenagers Study (HABITS) Prev Med. 2003;36(6):721–30. doi: 10.1016/s0091-7435(03)00047-1. Epub 2003/05/15. eng. [DOI] [PubMed] [Google Scholar]
- 3.Ferreira I, Twisk JW, van Mechelen W, Kemper HC, Stehouwer CD. Development of fatness, fitness, and lifestyle from adolescence to the age of 36 years: Determinants of the metabolic syndrome in young adults: the amsterdam growth and health longitudinal study. Arch Intern Med. 2005;165(1):42–8. doi: 10.1001/archinte.165.1.42. [DOI] [PubMed] [Google Scholar]
- 4.Berenson GS, Srinivasan SR, Bao W, Newman WP, 3rd, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med. 1998;338(23):1650–6. doi: 10.1056/NEJM199806043382302. Epub 1998/06/06. eng. [DOI] [PubMed] [Google Scholar]
- 5.Raitakari O, Juonala M, Khn M, et al. Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: The cardiovascular risk in young finns study. JAMA. 2003;290(17):2277–83. doi: 10.1001/jama.290.17.2277. [DOI] [PubMed] [Google Scholar]
- 6.Daniels SR, Pratt CA, Hayman LL. Reduction of risk for cardiovascular disease in children and adolescents. Circulation. 2011;124(15):1673–86. doi: 10.1161/CIRCULATIONAHA.110.016170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gonzalez-Suarez C, Worley A, Grimmer-Somers K, Dones V. School-based interventions on childhood obesity: a meta-analysis. Am J Prev Med. 2009;37(5):418–27. doi: 10.1016/j.amepre.2009.07.012. Epub 2009/10/21. eng. [DOI] [PubMed] [Google Scholar]
- 8.Kropski JA, Keckley PH, Jensen GL. School-based obesity prevention programs: an evidence-based review. Obesity (Silver Spring) 2008;16(5):1009–18. doi: 10.1038/oby.2008.29. eng. [DOI] [PubMed] [Google Scholar]
- 9.Sharma M. School-based interventions for childhood and adolescent obesity. Obes Rev. 2006;7(3):261–9. doi: 10.1111/j.1467-789X.2006.00227.x. Epub 2006/07/27. eng. [DOI] [PubMed] [Google Scholar]
- 10.Whalen CK, Henker B, O’Neil R, Hollingshead J, Holman A, Moore B. Optimism in children’s judgments of health and environmental risks. Health Psychol. 1994;13(4):319–25. doi: 10.1037//0278-6133.13.4.319. Epub 1994/07/01. eng. [DOI] [PubMed] [Google Scholar]
- 11.Wills TA, Isasi CR, Mendoza D, Ainette MG. Self-control constructs related to measures of dietary intake and physical activity in adolescents. J Adolesc Health. 2007;41(6):551–8. doi: 10.1016/j.jadohealth.2007.06.013. Epub 2007/11/21. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Terracciano A, Sutin AR, McCrae RR, Deiana B, Ferrucci L, Schlessinger D, et al. Facets of personality linked to underweight and overweight. Psychosom Med. 2009;71(6):682–9. doi: 10.1097/PSY.0b013e3181a2925b. Epub 2009/05/06. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kabat-Zinn J. Full catastrophe living: using the wisdom of your body and mind to face stress, pain, and illness. New York: Dell Publishing; 1990. [Google Scholar]
- 14.Roberts KC, Danoff-Burg S. Mindfulness and health behaviors: is paying attention good for you? J Am Coll Health. 2011;59(3):165–73. doi: 10.1080/07448481.2010.484452. Epub 2010/12/28. eng. [DOI] [PubMed] [Google Scholar]
- 15.Gilbert D, Waltz J. Mindfulness and Health Behaviors. Mindfulness. 2010;1(4):227–34. [Google Scholar]
- 16.Peters J, Erisman S, Upton B, Baer R, Roemer L. A Preliminary investigation of the relationships between dispositional mindfulness and impulsivity. Mindfulness. 2012;2(4):228–35. [Google Scholar]
- 17.Murphy C, MacKillop J. Living in the here and now: interrelationships between impulsivity, mindfulness, and alcohol misuse. Psychopharmacology. 2012;219(2):527–36. doi: 10.1007/s00213-011-2573-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.U.S. Department of Commerce. Historical statistics of the United States Colonial Times to 1970; Current population reports, Serios P-20, various years; and current population survey, October, 1970 through 2007. 2007. [Google Scholar]
- 19.Brener N, Demissie Z, Foti K, McManus T, Shanklin S, Hawkins J, et al. School Health Profiles 2010: Characteristics of Health Programs Among Secondary Schools. Atlanta: Centers for Disease Control and Prevention; 2011. [Google Scholar]
- 20.Larson RW, Verma S. How children and adolescents spend time across the world: work, play, and developmental opportunities. Psychol Bull. 1999;125(6):701–36. doi: 10.1037/0033-2909.125.6.701. Epub 1999/12/10. eng. [DOI] [PubMed] [Google Scholar]
- 21.Pbert L, Druker S, DiFranza JR, Gorak D, Reed G, Magner R, et al. Effectiveness of a school nurse-delivered smoking-cessation intervention for adolescents. Pediatrics. 2011;128(5):926–36. doi: 10.1542/peds.2011-0520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pbert L, Druker S, Gapinski MA, Gellar L, Magner R, Reed G, et al. A school nurse-delivered intervention for overweight and obese adolescents. J Sch Health. 2013;83(3):182–93. doi: 10.1111/josh.12014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.BMI Percentile Calculator for Child and Teen - English Version 2012 [10-2-2012] Available from: http://apps.nccd.cdc.gov/dnpabmi/Calculator.aspx.
- 25.Neinstein LS, editor. Adolescent Health Care: A Practical Guide. 4. Philadelphia, PA: Lippincott Williams and Wilkins; 2002. [Google Scholar]
- 26.Carrel AL, Bernhardt DT. Exercise prescription for the prevention of obesity in adolescents. Curr Sports Med Rep. 2004;3(6):330–6. doi: 10.1007/s11932-996-0008-1. [DOI] [PubMed] [Google Scholar]
- 27.Rowlands AV, Eston RG, Ingledew DK. Measurement of physical activity in children with particular reference to the use of heart rate and pedometry. Sports Med. 1997;24(4):258–72. doi: 10.2165/00007256-199724040-00004. [DOI] [PubMed] [Google Scholar]
- 28.Trost SG, McIver KL, Pate RR. Conducting accelerometer-based activity assessments in field-based research. Med Sci Sports Exerc. 2005;37:S531–43. doi: 10.1249/01.mss.0000185657.86065.98. eng. [DOI] [PubMed] [Google Scholar]
- 29.Welk GJ, Schaben JA, Morrow JR., Jr Reliability of accelerometry-based activity monitors: A generalizability study. Med Sci Sports Exerc. 2004;36(9):1637–45. [PubMed] [Google Scholar]
- 30.Brage S, Wedderkopp N, Franks PW, Andersen LB, Froberg K. Reexamination of validity and reliability of the CSA monitor in walking and running. Med Sci Sports Exerc. 2003;35(8):1447–54. doi: 10.1249/01.MSS.0000079078.62035.EC. [DOI] [PubMed] [Google Scholar]
- 31.Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. Accelerometer Med Sci Sports Exerc. 1998;30(5):777–81. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- 32.Dössegger A, Ruch N, Jimmy G, Braun-Fahrländer C, Mäder U, Hänggi J, Bringolf-Isler B. Reactivity to Accelerometer Measurement of Children and Adolescents. Med Sci Sports Exerc. 2014;46(6):1140–46. doi: 10.1249/MSS.0000000000000215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Blair SN, Haskell WL, Ho P, Paffenbarger RS, Jr, Vranizan KM, Farquhar JW, et al. Assessment of habitual physical activity by a seven-day recall in a community survey and controlled experiments. Am J Epidemiol. 1985;122(5):794–804. doi: 10.1093/oxfordjournals.aje.a114163. Epub 1985/11/01. eng. [DOI] [PubMed] [Google Scholar]
- 34.Strong WB, Malina RM, Blimkie CJ, Daniels SR, Dishman RK, Gutin B, et al. Evidence based physical activity for school-age youth. J Pediatr. 2005;146(6):732–7. doi: 10.1016/j.jpeds.2005.01.055. Epub 2005/06/24. eng. [DOI] [PubMed] [Google Scholar]
- 35.Varni JW, Seid M, Rode CA. The PedsQL: measurement model for the pediatric quality of life inventory. Med Care. 1999;37(2):126–39. doi: 10.1097/00005650-199902000-00003. Epub 1999/02/19. eng. [DOI] [PubMed] [Google Scholar]
- 36.Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. 1995;51(6):768–74. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. Epub 1995/11/01. eng. [DOI] [PubMed] [Google Scholar]
- 37.Brown KW, West AM, Loverich TM, Biegel GM. Assessing adolescent mindfulness: validation of an adapted Mindful Attention Awareness Scale in adolescent normative and psychiatric populations. Psychol Assess. 2011;23(4):1023–33. doi: 10.1037/a0021338. Epub 2011/02/16. eng. [DOI] [PubMed] [Google Scholar]
- 38.de Bruin EI, Zijlstra BJ, van de Weijer-Bergsma E, Bogels SM. The Mindful Attention Awareness Scale for Adolescents (MAAS-A): Psychometric Properties in a Dutch Sample. Mindfulness. 2011;2(3):201–11. doi: 10.1007/s12671-011-0061-6. Epub 2011/09/13. Eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Resnicow K, Taylor R, Baskin M, McCarty F. Results of go girls: a weight control program for overweight African-American adolescent females. Obes Res. 2005;13(10):1739–48. doi: 10.1038/oby.2005.212. eng. [DOI] [PubMed] [Google Scholar]
- 40.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–96. [PubMed] [Google Scholar]
- 41.Choi WS, Patten CA, Gillin JC, Kaplan RM, Pierce JP. Cigarette smoking predicts development of depressive symptoms among U.S. adolescents. Ann Behav Med. 1997;19(1):42–50. doi: 10.1007/BF02883426. [DOI] [PubMed] [Google Scholar]
- 42.Spielberger CD. State-Trait Anxiety Inventory for Children. Palo Alto, CA: Consulting Psychologists Press; 1973. [Google Scholar]
- 43.Johnson SL, Birch LL. Parents’ and children’s adiposity and eating style. Pediatrics. 1994;94(5):653–61. Epub 1994/11/01. eng. [PubMed] [Google Scholar]
- 44.Robinson TN, Kiernan M, Matheson DM, Haydel KF. Is parental control over children’s eating associated with childhood obesity? Results from a population-based sample of third graders. Obes Res. 2001;9(5):306–12. doi: 10.1038/oby.2000.38. Epub 2001/05/11. eng. [DOI] [PubMed] [Google Scholar]
- 45.Bellg A, Borrelli B, Resnick B, Hecht J, Minicucci D, Ory M, et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium. Health Psychol. 2004;23(5):443–51. doi: 10.1037/0278-6133.23.5.443. [DOI] [PubMed] [Google Scholar]
- 46.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.SAS statistical software, version 9.2. Cary, NC: SAS Institute, Inc; 2009. [Google Scholar]
- 48.Pocock SJ. Clinical trials: a practical approach. John Wiley & Sons Ltd; 1983. Inclusion of withdrawals in analysis; pp. 182–6. [Google Scholar]
- 49.Molenberghs G, Verbeke G. Models for discrete longitudinal data. New York: Springer; 2005. [Google Scholar]
- 50.Miles J, Huberman A. Qualitative data analysis: An expanded sourcebook. 2. London: Sage Publications; 1994. [Google Scholar]
- 51.Patton MQ. Qualitative research & evaluation methods. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- 52.Fitzmaurice G, Laird N, Ware J. Applied longitudinal analysis. New York: Wiley; 2004. [Google Scholar]
- 53.Chuang-Stein C, Tong DM. The impact and implication of regression to the mean on the design and analysis of medical investigations. Stat Methods Med Res. 1997;6(2):115–28. doi: 10.1177/096228029700600203. Epub 1997/06/01. eng. [DOI] [PubMed] [Google Scholar]
- 54.Assmann SF, Pocock SJ, Enos LE, Kasten LE. Subgroup analysis and other (mis)uses of baseline data in clinical trials. Lancet. 2000;355(9209):1064–9. doi: 10.1016/S0140-6736(00)02039-0. Epub 2000/04/01. eng. [DOI] [PubMed] [Google Scholar]
- 55.Pocock SJ, Assmann SE, Enos LE, Kasten LE. Subgroup analysis, covariate adjustment and baseline comparisons in clinical trial reporting: current practice and problems. Stat Med. 2002;21(19):2917–30. doi: 10.1002/sim.1296. Epub 2002/09/27. eng. [DOI] [PubMed] [Google Scholar]
- 56.Leon AC, Davis LL, Kraemer HC. The role and interpretation of pilot studies in clinical research. J Psychiatr Res. 2011;45(5):626–9. doi: 10.1016/j.jpsychires.2010.10.008. Epub 2010/11/03. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kraemer HC, Mintz J, Noda A, Tinklenberg J, Yesavage JA. Caution regarding the use of pilot studies to guide power calculations for study proposals. Arch Gen Psychiatry. 2006;63(5):484–9. doi: 10.1001/archpsyc.63.5.484. Epub 2006/05/03. eng. [DOI] [PubMed] [Google Scholar]
- 58.Carmody JF, Crawford S, Salmoirago-Blotcher E, Leung K, Churchill L, Olendzki N. Mindfulness training for coping with hot flashes: results of a randomized trial. Menopause. 2011;18(6):611–20. doi: 10.1097/gme.0b013e318204a05c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kish L. Survey sampling. New York: Wiley; 1965. [Google Scholar]
- 60.Kabat-Zinn J. Mindfulness meditation: health benefits of an ancient buddhist practice. In: Goleman D, Gurin J, editors. Mind/Body Medicine. Yonkers, NY: Consumer Reports Books; 1993. [Google Scholar]
- 61.Baer RA. Self-focused attention and mechanisms of change in mindfulness-based treatment. Cogn Behav Ther. 2009;38(1):15–20. doi: 10.1080/16506070902980703. [DOI] [PubMed] [Google Scholar]
- 62.Nyklicek I, Kuijpers KF. Effects of mindfulness-based stress reduction intervention on psychological well-being and quality of life: is increased mindfulness indeed the mechanism? Ann Behav Med. 2008;35(3):331–40. doi: 10.1007/s12160-008-9030-2. Epub 2008/06/07. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kristeller JL, Wolever RQ. Mindfulness-based eating awareness training for treating binge eating disorder: the conceptual foundation. Eat Disord. 2010;19(1):49–61. doi: 10.1080/10640266.2011.533605. Epub 2010/12/25. eng. [DOI] [PubMed] [Google Scholar]
- 64.Salmoirago-Blotcher E, Hunsinger M, Morgan L, Fischer D, Carmody J. Mindfulness-Based Stress Reduction and change in health-related behaviors. J Evid Based Complementary Altern Med. doi: 10.1177/2156587213488600. Published online before print May 8, 2013. [DOI] [Google Scholar]
- 65.Daubenmier J, Kristeller J, Hecht FM, Maninger N, Kuwata M, Jhaveri K, et al. Mindfulness intervention for stress eating to reduce cortisol and abdominal fat among overweight and obese women: an exploratory randomized controlled study. J Obes. 2011;2011:651936. doi: 10.1155/2011/651936. Epub 2011/10/07. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kearney DJ, Milton ML, Malte CA, McDermott KA, Martinez M, Simpson TL. Participation in mindfulness-based stress reduction is not associated with reductions in emotional eating or uncontrolled eating. Nutr Res. 2012;32(6):413–20. doi: 10.1016/j.nutres.2012.05.008. Epub 2012/07/04. eng. [DOI] [PubMed] [Google Scholar]
- 67.Hebert JR, Hurley TG, Harmon BE, Heiney S, Hebert CJ, Steck SE. A diet, physical activity, and stress reduction intervention in men with rising prostate-specific antigen after treatment for prostate cancer. Cancer Epidemiol. 2012;36(2):e128–e36. doi: 10.1016/j.canep.2011.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Carmody J, Olendzki B, Reed G, Andersen V, Rosenzweig P. A dietary intervention for recurrent prostate cancer after definitive primary treatment: results of a randomized pilot trial. Urology. 2008;72(6):1324–8. doi: 10.1016/j.urology.2008.01.015. Epub 2008/04/11. eng. [DOI] [PubMed] [Google Scholar]
- 69.Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84(4):822–48. doi: 10.1037/0022-3514.84.4.822. Epub 2003/04/22. eng. [DOI] [PubMed] [Google Scholar]
- 70.Kabat-Zinn J. Mindfulness-based interventions in context: past, present, and future. Clin Psychol Sci Prac. 2003;10(2):144–56. [Google Scholar]
- 71.Jasinska AJ, Yasuda M, Burant CF, Gregor N, Khatri S, Sweet M, et al. Impulsivity and inhibitory control deficits are associated with unhealthy eating in young adults. Appetite. 2012;59(3):738–47. doi: 10.1016/j.appet.2012.08.001. Epub 2012/08/14. Eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Veloso SM, Matos MG, Carvalho M, Diniz JA. Psychosocial factors of different health behaviour patterns in adolescents: association with overweight and weight control behaviours. J Obes. 2012;2012:852672. doi: 10.1155/2012/852672. Epub 2012/07/20. Eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Shapiro S, Walsh R. An analysis of recent meditation research and suggestions for future directions. Palo Alto: VA Palo Alto Health Care System; 2002. [Google Scholar]
- 74.Lazarus RS. Coping theory and research: past, present, and future. Psychosom Med. 1993;55(3):234–47. doi: 10.1097/00006842-199305000-00002. Epub 1993/05/01. eng. [DOI] [PubMed] [Google Scholar]
- 75.Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: developmental issues and implications for DSM-V. Psychiatr Clin North Am. 2009;32(3):483–524. doi: 10.1016/j.psc.2009.06.002. Epub 2009/09/01.eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.McCracken M, Jiles R, Blanck HM. Health behaviors of the young adult U.S. population: behavioral risk factor surveillance system, 2003. Prev Chronic Dis. 2007;4(2):A25. Epub 2007/03/17. eng. [PMC free article] [PubMed] [Google Scholar]
- 77.Kashani JH, Carlson GA, Beck NC, Hoeper EW, Corcoran CM, McAllister JA, et al. Depression, depressive symptoms, and depressed mood among a community sample of adolescents. Am J Psychiatry. 1987;144(7):931–4. doi: 10.1176/ajp.144.7.931. Epub 1987/07/01. eng. [DOI] [PubMed] [Google Scholar]
- 78.Lewinsohn PM, Rohde P, Seeley JR. Major depressive disorder in older adolescents: prevalence, risk factors, and clinical implications. Clin Psychol Rev. 1998;18(7):765–94. doi: 10.1016/s0272-7358(98)00010-5. Epub 1998/11/25. eng. [DOI] [PubMed] [Google Scholar]
- 79.Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication--Adolescent Supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2010;49(10):980–9. doi: 10.1016/j.jaac.2010.05.017. Epub 2010/09/22. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]


