Abstract
The Na-K-2Cl cotransporter 2 (NKCC2) was thought to be kidney specific. Here we show expression in the brain hypothalamo-neurohypophyseal system (HNS), wherein upregulation follows osmotic stress. The HNS controls osmotic stability through the synthesis and release of the neuropeptide hormone, arginine vasopressin (AVP). AVP travels through the bloodstream to the kidney, where it promotes water conservation. Knockdown of HNS NKCC2 elicited profound effects on fluid balance following ingestion of a high-salt solution—rats produced significantly more urine, concomitant with increases in fluid intake and plasma osmolality. Since NKCC2 is the molecular target of the loop diuretics bumetanide and furosemide, we asked about their effects on HNS function following disturbed water balance. Dehydration-evoked GABA-mediated excitation of AVP neurons was reversed by bumetanide, and furosemide blocked AVP release, both in vivo and in hypothalamic explants. Thus, NKCC2-dependent brain mechanisms that regulate osmotic stability are disrupted by loop diuretics in rats.
Keywords: fluid balance, GABA, hypothalamo-neurohypophyseal system, loop diuretics, Slc12a1/NKCC2
Introduction
An ability to maintain water balance is a fundamental requirement for terrestrial life (Antunes-Rodrigues et al., 2004). In mammals, this involves interactions between a control center in the brain called the hypothalamo-neurohypophyseal system (HNS) and the filtration machinery of the kidney.
The HNS is the source of the antidiuretic peptide hormone arginine vasopressin (AVP). Synthesized in cell bodies of the large magnocellular neurons (MCNs) of the supraoptic (SON) and paraventricular (PVN) nuclei, AVP is transported anterogradely to terminals in the posterior pituitary gland (Brownstein et al., 1980; de Bree, 2000). A rise in plasma osmolality is detected by intrinsic MCN osmoreceptor mechanisms (Bourque et al., 2002; Zhang and Bourque, 2003) and by osmoreceptive neurons in the circumventricular organs that project to (Bourque, 1998; McKinley et al., 1999, 2004; Anderson et al., 2000), and provide direct excitatory inputs (van den Pol et al., 1990) that shape the firing of MCNs (Hu and Bourque, 1992; Nissen et al., 1994), resulting in hormone secretion (Dyball et al., 1995; Onaka and Yagi, 2001). AVP travels through the bloodstream to the kidney where it promotes water reabsorption in the collecting duct (Breyer and Ando, 1994) and sodium reabsorption in the thick ascending limb of the loop of Henle (TAL; Ares et al., 2011).
The HNS also produces the closely related hormone oxytocin (OXT), which acts to promote kidney natriuresis (Huang et al., 1996). Single-cell RT-PCR enables AVP and OXT transcripts to be detected in the same MCN (Glasgow et al., 1999), but the expression levels of each neuropeptide RNA differ by orders of magnitude. Only a small percentage (2–3%) of MCNs express high, equivalent levels of both peptides (Mohr et al., 1988), although this proportion increases following dehydration (Telleria-Diaz et al., 2001).
Dehydration evokes a dramatic functional remodeling of the HNS (Hatton, 1997; Theodosis et al., 1998; Sharman et al., 2004), which might contribute to the facilitation of hormone production and delivery. Microarrays have been used to ask how dehydration evokes changes in the rat HNS transcriptome that may mediate these plastic events (Hindmarch et al., 2006; Yue et al., 2006; Qiu et al., 2007). One of the genes discovered to be upregulated in the HNS as a consequence of dehydration was Slc12a1, which encodes the Na(+)-K(+)-2Cl(−)cotransporter NKCC2, previously thought to be kidney specific. NKCC2 mediates the tightly coupled electroneutral movement of one each of Na(+) and K(+) and two Cl(−) ions across cell membranes (Ares et al., 2011; Markadieu and Delpire, 2014). In the kidney, NKCC2 localized to the apical membrane of epithelial cells in the TAL mediates the reabsorption of a considerable proportion of the NaCl filtered by the glomeruli. AVP, acting through V2 receptor activation and a subsequent increase in intracellular cAMP (Caceres et al., 2009), enhances NKCC2 activity through phosphorylation and membrane targeting (Giménez and Forbush, 2003).
In this study, we test the hypothesis that NKCC2 within the HNS has a role in the central neural integration of the processes that conserve water following a chronic osmotic challenge.
Materials and Methods
Animals and treatments.
Male Sprague Dawley rats weighing 250–300 g were obtained from Harlan. Rats were housed at a constant temperature of 22°C and a relative humidity of 50–60% (v/v) under a 14:10 h light/dark cycle. Rats were given free access to food and tap water for at least 1 week before experimentation. To induce hyperosmotic stress, water was removed for 3 d (dehydration) or replaced by 2% (w/v) NaCl in drinking water for up to 7 d (salt loading). Food was available ad libitum. The acute responses to elevated plasma osmolality were assessed after a single intraperitoneal injection of 1.5 ml/100 g body weight of 1.5 m NaCl solution. Rats were randomly allocated into one of six groups: control; 10 min; 30 min; and 1, 2, and 4 h after administration of hypertonic saline. The control group had access food and water ad libitum throughout the experimental period. After injection of hypertonic saline rats were placed back in their home cages and water was removed for the duration of the experiment. In the furosemide treatment protocol, a single vehicle or 20 mg/kg furosemide subcutaneous injection was performed, followed by 24 h with free access to sodium-deficient chow (0.001% sodium) and no water access. All animal experiments were performed between 10:00 A.M. and 1:00 P.M. All experiments were performed under the licensing arrangements of the UK Animals (Scientific Procedures) Act (1986) with local ethics committee approval.
Vasopressin, osmolality, and hematocrit.
After decapitation, trunk blood was collected in chilled heparinized plastic tubes. Plasma osmolality was measured by an osmometer (model 5004; Precision Systems), based on the freezing-point depression method, and expressed as mOsm/kg H2O. The hematocrit was determined using small aliquots of trunk blood collected in capillary tubes and expressed as the percentage of cells in the blood. AVP was extracted from 1 ml of plasma with acetone and petroleum ether and measured using a specific anti-AVP antibody (Peninsula T4561) for radioimmunoassay. Assay sensitivity and intra-assay and interassay coefficients of variation were 0.7 pg/ml, 8.1%, and 10.7%.
RNA extraction and cDNA synthesis.
Rats were stunned and decapitated. Brains were removed and immediately frozen in powdered dry ice. A 1 mm micro punch (Fine Scientific Tools) was used to collect SON and PVN samples from 60 μm coronal sections in a cryostat. Sections were mounted on glass slides and stained with 2% (w/v) toluidine blue, then visualized on a light microscope until the desired brain nuclei was visible. Using the optic chiasm (SON) or neurons mediolateral to the third ventricle (PVN) for reference, samples were punched from frozen brain slices and dispensed into 1.5 ml tubes kept on dry ice within the cryostat. Total RNA was extracted from punch samples by combining QIAzol Reagent with Qiagen's RNeasy kit protocols. The punch samples were removed from dry ice and rapidly resuspended, by vortexing, in 1 ml of QIAzol reagent. Following QIAzol phase separation with chloroform, 350 μl of the upper aqueous phase was removed, mixed with 350 μl 70% (v/v) ethanol, and applied to RNeasy columns. The remaining steps were performed as recommended by the manufacturer. For cDNA synthesis, 100 ng of total RNA was treated with DNAse I (Qiagen) and reverse transcribed using the QuantiTect reverse transcription kit (Qiagen).
RT qPCR analysis.
Steady-state RNA levels in the SON and PVN were assessed by qPCR. Slc12a1 QuantiTect primers were purchased from Qiagen, primers for RPL19 (Forward-5′-GTCCTCCGCTGTGGTAAAAA-3′ and Reverse-5′-GGCAGTACCCTTCCTCTTCC-3′), GAPDH (Forward-5′-ATGATTCTACCCACGGCAAG-3′ and Reverse-5′-CTGGAAGATGGTGATGGGTT-3′), GFP (Forward-5′-ACTTCTTCAAGTCCGCCATGCC-3′ and Reverse-5′-TGAAGTCGATGCCCTTCAGCTC-3′), and AVP (Forward-5′-TGCCTGCTACTTCCAGAACTGC-3′ and Reverse-5′-AGGGGAGACACTGTCTCAGCTC-3′) were designed using either OligoPerfect (Invitrogen Life Technologies) or Eurofins Genomics tools. The optimization and validation of primers was performed using standard ABI protocols. The cDNA from RT reaction was used as a template for subsequent PCRs, which were performed in duplicate. Quantitative PCR was conducted in 25 μl reaction volumes using SYBR Green Master Mix (Roche) and ABI 7500 Sequence Detection System (ABI). Dissociation curve analysis was performed for all qPCRs. For relative quantification of gene expression the 2-ΔΔCT method was used (Livak and Schmittgen, 2001). The internal control gene used for these analyses was the housekeeping gene RPL19.
Generation of NKCC2 riboprobes.
Slc12a1 mRNA was detected by in situ hybridization using two riboprobes targeting distinct sequences to maximize signal intensity and specificity. Probes were generated by PCR using reverse-transcribed rat brain mRNA as a template, 2.5 U AmpliTaq polymerase (Applied Biosystems), and primers specific for rat Slc12a1 (GenBank accession no. NM_019134) Probe 1, bp 1783–2767: 5′-GCGAATTCTCAGTGCACCCAAAGTATTCC-3′ and 5′-GCAAGCTTAGAGCCAGTCTCTCCTGTTCC-3′ and Probe 2, bp 2601–3332: 5′-GCGAATTCAGGAAAGCTCCCTTGTCTGAG-3′ and 5′-GCAAGCTTGACTGCTTCCAGTTCTGCATC-3′). The primers included recognition sequences for the restriction endonucleases EcoRI and HindIII to enable subcloning of the PCR products into the RNA-generating vector pGEM4Z (Promega). The integrity of the probes was verified by DNA sequencing. Sense and antisense riboprobes were generated using T7 and SP6 polymerases with [35S]UTP and the MAXIscript in vitro transcription kit (Ambion). Briefly, 10–30 μg of plasmid containing the Slc12a1 sequences was linearized with HindIII (sense probes) or EcoRI (antisense probes) to generate DNA templates for in vitro transcription. Then 500 ng of DNA template was mixed with 1 μl of 10× Transcription Buffer; 0.5 μl of ATP, CTP, and GTP; 2.5 μl of 35S-UTP; 0.5 μl of SP6 (sense probe) or T7 polymerase (antisense probe); and dH2O to make a final volume of 10 μl. The mixture was incubated for 30 min at 37°C, after which the DNA template was removed by adding 0.5 μl DNase and 0.5 μl RNasin for 15 min at 37°C. The riboprobes were precipitated by adding 190 μl TE buffer, pH 7.6; 5 μl tRNA (10 mg/ml); 80 μl 7.5N NH4Ac; and 700 μl EtOH for 15 min on dry ice, followed by centrifuging for 15 min at 4°C. The RNA pellet was washed with 1 ml 70% (v/v) EtOH and resuspended in a buffer containing 97 μl TE, 2 μl 10% (w/v) SDS, and 1 μl 5 m DTT. The riboprobes were then hydrolyzed into ∼200 bp fragments in 100 μl dH2O and 100 μl of 2× carbonate buffer (80 mm NaHCO3 and 120 mm Na2CO3) for 30 min at 60°C. The hydrolyzed riboprobes were then precipitated and neutralized with 10 μl 10% (v/v) acetic acid and ready for in situ hybridization experiments.
Low resolution in situ hybridization.
Rats were killed by cervical dislocation and decapitated. Brains and kidneys were rapidly removed and snap frozen over liquid nitrogen. Coronal sections (12 μm) ranging from the beginning of the SON to the last of the PVN-containing tissue and transverse sections (12 μm) of the kidneys were cut on a cryostat (Cryocut CM3050; Leica Microsystems), thaw mounted on poly-l-lysine-coated microscope slides, and stored at −80°C. On the day of fixation, the slide-mounted brain sections were removed from storage and allowed to equilibrate to room temperature for 15–20 min. The sections were fixed with 4% (w/v) cold paraformaldehyde in 1× PBS solution (made up within the last 7 d and stored at 4°C) for 5 min at room temperature and were rinsed twice with 1× PBS. The sections were then placed in 0.25% (w/v) acetic anhydride in 0.1 m triethanolamine HCl/0.9% (w/v) NaCl for 10 min at room temperature, followed by dehydration for 1 min each in 70% (v/v), 80% (v/v), and then in 95% (v/v) for 2 min and 100% (v/v) EtOH for another minute. This was followed by a delipidation wash in chloroform for 5 min, followed by washes in 100 (v/v) and 90% (v/v) EtOH for 1 min each. The sections were then air dried. Labeled riboprobes (50,000–100,000 cpm) were diluted in 45 μl of a hybridization buffer containing 50% (v/v) deionized formamide, 4× SSC (1× SSC is 0.6 m NaCl and 0.06 m sodium citrate, pH 7.0), 500 mg/ml sheared DNA, 250 mg of yeast tRNA, 1× Denhardt's solution (0.02% w/v Ficoll, 0.02% w/v polyvinyl pyrrolidone, and 0.02% w/v BSA), and 10% (w/v) dextran sulfate. Slides were covered with glass coverslips and incubated overnight in a humidified atmosphere at 55°C. On the following day, the slides were rinsed in SSPE, followed by washing in 4 (v/v), 2 (v/v), and 1% (v/v) SSPE for 15 min each at 37°C. Slides were further washed in 1% (v/v) SSPE at 60°C (two times for 30 min), followed by additional washes in 70 (v/v), 80 (v/v), 90 (v/v), 95 (v/v), and 100% (v/v) EtOH for 1 min each at room temperature. When dry, slides were apposed to Hyperfilm (Eastman Kodak) with standard 14C microscales in autoradiographic cassettes for 3 d (kidney) or 7 d (brain). After development, the films were placed under the microscope (MZ6; Leica), and images were captured with the camera and analyzed with NIH ImageJ 1.62 software. The density of the hybridization signal was assessed by comparing the optical density of the autoradiograms to standard microscales. Results are presented both as raw data, as well as normalized and expressed as a ratio of dehydrated to control (euhydrated) levels. Four sections per rat taken at regular intervals through the PVN or SON of each rat from the respective groups were analyzed. Two sections from each rat were used to establish nonspecific binding.
High resolution in situ hybridization.
To obtain high-resolution images, hybridized and washed slides were emulsion dipped. In the dark, under the safelight, 30 μl of 50% (v/v) glycerol and 6 ml of dH2O was mixed with K-5 emulsion (Ilford Imaging) to a final volume of 10 ml. The mixture was incubated at 45°C for 20 min until the emulsion had melted. The molten emulsion was then poured into a dipping chamber in the water bath and left for another 20 min to allow any air bubbles to escape. Each slide was dipped into the bottom of the vessel with a steady action, and excess emulsion was drained off. The slides were placed in a rack in the dark, allowed to dry for 2 h, then placed in black boxes, and exposed at 4°C. After 7 d (kidney) or 21 d (brain), in the dark under the safelight, slides were removed from the black box and placed into metal racks. The racks were then placed in D19 developer for 3.5 min, indicator stop bath for 0.5 min, fixative for 3.5 min, and dH2O for 5–30 min to wash off the fixative. After development, the slides were dipped in 95% (v/v) EtOH for 1 min, 100% (v/v) EtOH for 1 min, and 0.5% (w/v) toluidine blue for 1–5 min, and then were rinsed with dH2O. Slides were air dried and mounted in DPX, covered with coverslips, and observed under the microscope (LeicaDM IRB). Photomicrographs were taken with a Leica DC-300F digital camera using IM50 software (version 1.2), and saved as TIFF images at 300 dpi resolution. Semiquantitative image analysis was conducted on emulsion-dipped sections. Cell counting was performed at 200× magnification on a Leica DM IRB microscope with C-plan optics. Grain counting was conducted under bright-field conditions at a magnification of 400× using the above microscope and a Leica 300DM digital camera. NIH ImageJ software was used to quantify the number of silver grains expressed in neurons of the SON and PVN. Only cells that expressed five times the background labeling (which was typically 5–15 grains per equivalent cellular area) were assessed. From each treatment group, two sections were selected from the middle region of each nucleus. These selected sections were carefully matched between groups. From each section, 10–15 labeled cells were selected at random from throughout the whole nucleus to determine the number of silver grains expressed in each cell. The automated “analyze particles” function was used, enabling the standardization of the size of particles to be counted. Any overlapping grains that exceed the particle size threshold were manually inspected and counted.
Immunohistochemistry.
Control euhydrated (n = 3) and dehydrated (n = 3) rats were anesthetized with sodium pentobarbitone (100 mg/kg, i.p.) and transcardially perfused with 0.1 m PBS, pH 7.4, followed by 4% (w/v) PFA in 0.1 m PBS. The brains were removed and postfixed overnight in 4% (w/v) PFA followed by 30% (w/v) sucrose prepared in PBS. Coronal sections (40 μm) of the forebrain were cut on a cryostat, washed in 0.1 m PBS, pH 7.4, and blocked for 1 h in 10% (v/v) horse serum (Sigma-Aldrich). Floating sections were incubated with primary antisera with 1% (w/v) normal horse serum and 0.3% (v/v) Triton X-100 in 0.1 m PBS for 1 h at room temperature and then at 4°C overnight. Two primary anti-NKCC2 rabbit antibodies were used: AB3562P (1:200; Millipore) and H-110 (1:100; Santa Cruz Biotechnology). Data obtained using both were comparable. The data obtained using H-110 is shown here. Colocalization analysis used primary mouse monoclonal antibodies recognizing AVP neurophysin (NP-II, PS41; 1:200) or OXT neurophysin (NP-I, PS38; 1:200). Sections were washed three times in PBS then incubated with biotinylated anti-rabbit IgG (Vector Laboratories; 1:500) in 0.1 m PBS containing 1% (v/v) normal horse serum, 0.3% (v/v) Triton X-100 for 1 h at room temperature. After three washes with 0.1 m PBS, sections were incubated with both Alexa Fluor 488-Streptavidin (1: 500; Vector Laboratories) and Alexa Fluor 594-conjugated anti-mouse IgG (1:500; Vector Laboratories) for1 h. Images were observed using a fluorescent Leica DMRB microscope with images captured using a DC300F camera run on Leica IM50 software. Adobe Photoshop was used to observe colocalization of and NKCC2 and either AVP or OXT.
Lentivirus production, purification, and titration.
The siRNA targeting sequence of Slc12a1 (GGTAACCTCTATCACTGGG) has previously been shown to specifically knockdown mouse Slc12a1 (Hao et al., 2011). A scrambled control (GGCTTACGTAGGCATCTCA) for this nucleotide sequence was generated using siRNA Wizard v3.1 (www.sirnawizard.com/scrambled.php). Two complementary oligonucleotides for these target sequences were generated using Ambion's siRNA-shRNA convertor (www.ambion.com/techlib/misc/psilencer_coverter.html) with loop structure TTCAAGAGA and cloned into RNAi expression vector pSilencer 1.0-U6 (Ambion). The U6-shRNA sequences were amplified (5′-CCTTAATTAAGGCGACTCACTATAGGGCGAATTGGG-3′ and 5′-CCCGCTCGAGCGGCTAGTGGATCCCCCGGGCTG-3′; italicized letters represent PacI and XhoI restriction enzyme site, respectively) from pSilencer 1.0-U6 using Phusion High-Fidelity DNA Polymerase (New England BioLabs) and cloned into compatible restriction sites of lentiviral vector pRRL.SIN.U6.shRNA.CPPT.CMV.GFP.WPRE (engineered from Addgene plasmid 12252). The transfer vectors were propagated in Stbl3-competent cells (Invitrogen) to reduce homologous recombination. All plasmid constructs were purified by Maxiprep using PureLink HiPure Plasmid Filter Maxiprep kit (Invitrogen). Viruses were generated by transient transfection of the shuttle vector together with three separate packaging plasmids (pMDLg/pRRE, pRSV-Rev, and PMD2.G; Addgene) into HEK293T cells by calcium phosphate method as previously described (Panyasrivanit et al., 2011). Culture supernatant-containing lentivirus was collected at 48 and 72 h after transfection, cell debris was removed by centrifugation, and the supernatant was filtered through 0.45 μm filter (Corning). High-titer lentiviruses were produced by centrifugation at 6000 × g for 16 h (400 ml), followed by ultracentrifugation of the resuspended pellet (10 ml PBS) for 1.5 h at 20,000 × g. The viral pellet was resuspended in 150 μl of prewarmed PBS and stored in 5 μl aliquots at −80°C. Viral titers were determined by counting GFP-positive cells at day 3 following transduction of HEK293T cells.
Lentiviral vector gene transfer into SON and PVN.
Rats were anesthetized by intramuscular administration of ketamine (60 mg/kg; Pfizer) and medetomidine hydrochloride (250 μg/kg; Pfizer) and placed in a stereotaxic frame in the flat skull position. A 2 cm rostrocaudal incision was made to expose the surface of the skull. Two 1 mm holes were drilled at coordinates 1.3 mm posterior to bregma and 1.95 mm lateral to midline for SON injection. An additional 1 mm hole was drilled at coordinates 1.8 mm posterior to bregma, and ±0.4 mm lateral to midline for PVN injection. A 5 μl pulled-glass pipette was positioned −8.8 mm (SON) or −7.5 mm (PVN) ventral to the surface of the brain and 1 μl of lentiviral vector at the concentration of 5 × 109 particles/ml was delivered separately into four nuclei over 5 min per nucleus. At the end of surgery anesthesia was reversed by a subcutaneous injection of atipamezole hydrochloride (1 mg/kg; Norden Laboratories) and postoperative analgesic, carprofen (5 mg/kg s.c.; Zoetis) given. After the surgery the animals were individually housed in standard laboratory cages for 2 weeks before being transferred to metabolic cages (TecniPlast) to allow precise daily measures of fluid intake, food intake, and urine output. Animals were weighed and allowed to acclimatize to the cage for 72 h. Fluid intake, food intake, urine output, urine osmolality, and body weight were recorded for 10 d. At the end of the experiment, blood samples were collected from the heart and the animals were perfused intracardially with 100 ml/100 g body mass of PBS, pH 7.4, followed by an equal amount of 4% PFA in PBS, pH 7.4. Osmolality was measured in 100 μl of plasma or urine (10× diluted) by freezing-point depression using a Roebling micro-osmometer (Camlab).
Mapping and assignment of groups.
Coronal hypothalamic sections from the virus-injected rats (40 μm) were analyzed using a wide-field fluorescent microscope with a 488 nm filter (Olympus) for GFP expression. Rats successfully injected with Slc12a1 shRNA lentivirus into three or four sides of the PVN and SON (i.e., 1–2 × sides of the SON plus 2 × sides of the PVN, or 2 × sides of the SON plus 1–2 × sides of the PVN) were used for subsequent data analysis.
Electrophysiology.
Transgenic Wistar rats that express eGFP driven by the AVP promoter were used (Ueta et al., 2005). Animals were anesthetized with isoflurane and decapitated. The brain was quickly removed; it was submerged and coronally sectioned on a vibratome (Leica) to 300 μm in slicing solution (0°C, 95% O2/5% CO2 saturated) containing the following (in mm): 87 NaCl, 2.5 KCl, 0.5 CaCl2, 7 MgCl2, 25 NaHCO3, 25 d-glucose, 1.25 NaH2PO4, and 75 sucrose. After placement into aCSF (30°C, 95% O2/5% CO2 saturated) containing the following (in mm):126 NaCl, 2.5 KCl, 26 NaHCO3, 2.5 CaCl2, 1.5 MgCl2, 1.25 NaH2PO4, and 10 glucose, hypothalamic slices recovered for at least 1 h. Once transferred to a recording chamber superfused with aCSF (1 ml/min; 30–32°C; 95% O2/5% CO2), slices were visualized using an upright microscope (BX51WI; Olympus) fitted with infrared differential interference contrast optics. Pulled borosilicate glass pipettes (3–6 MΩ) were filled with a solution containing the following (in mm): 116 K-gluconate, 2 MgCl2, 8 Na-gluconate, 1 K2-EGTA, 4 K2-ATP, 0.3 Na3-GTP, and 10 HEPES. In some experiments bumetanide was added to the bath. Whole-cell patch-clamp recordings were performed from MCNs identified by eGFP expression in transgenic rats (36) and current-clamp fingerprint. MCNs were initially voltage-clamped at −80 mV with constant perfusion of DNQX (10 μm; Tocris Bioscience) and eIPSCs were recorded. The membrane was stepped in 10 mV increments to different potentials every 2 min and the average synaptic current at each potential was calculated. This was used to generate a reversal potential for GABAA-mediated currents (EGABA). Junction potential (calculated: 17 mV) was not compensated. Bumetanide (50–100 μm) was applied in the bath.
Hypothalamic explants.
Hypothalamic explant protocols have been described previously (Gomes et al., 2004 and 2010). Briefly, animals were killed by decapitation, the brain was immediately removed, and the medial basal hypothalamus (MBH) was dissected and incubated in 0.5 ml cold Krebs Ringer bicarbonate buffer (KRBG; 0.9% w/v NaCl; 5.75% w/v KCl; 10.55% w/v KH2PO4; 9.27% w/v MgSO4*7H2O; 1.23% w/v NaHCO3; 6.1% w/v CaCl2; and 0.1% w/v glucose and 0.004% w/v bacitracin; osmolality 280 mOsm/kg H2O, pH 7.4) for 60 min under agitation (Dubnoff shaker, 20 cycles/min; 95% v/v O2/5% v/v CO2, 37°C) to wash the explants. Then, the solution was carefully removed and replaced by 0.5 ml of isotonic (280 mOsm/kg H2O) or hypertonic (340 mOsm/kg H2O) KRBG solution containing different concentrations of furosemide (0.1 up to 100 μm in 0.9% w/v NaCl, compared with vehicle alone) for 30 min. As explants exclude all of the osmosensitive circumventricular organs, inputs from which contribute to AVP secretion (van den Pol et al., 1990; Hu and Bourque, 1992; Nissen et al., 1994; Dyball et al., 1995; Bourque, 1998; McKinley et al., 1999, 2004; Anderson et al., 2000; Onaka and Yagi, 2001), a large increase in osmolality (60 mOsm/kg) is required to elicit a secretory response. At the end of the second incubation, the medium was collected and stored at −20°C until the AVP radioimmunoassay protocol. The osmolality of KRBG solutions was manipulated by the addition of a hypertonic NaCl solution and confirmed by freezing-point depression (Model 5004 osmometer; Precision Systems),
Statistical analysis.
All data are expressed as the mean ± SEM. Differences between qPCR experimental groups were evaluated using independent sample unpaired Student's t tests. Two-way ANOVA with uncorrected Fisher's LSD test or Dunnett's post hoc were used to determine the differences between more than two groups; p < 0.05 was considered significant.
Results
Slc12a1 transcripts are expressed in the HNS
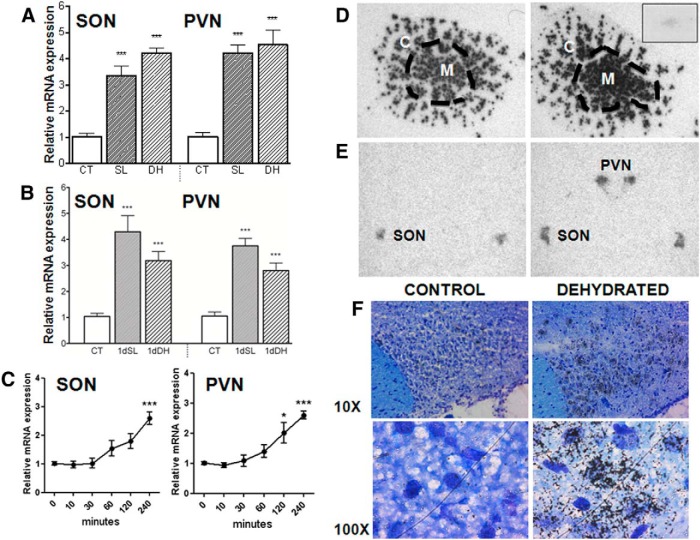
Affymetrix array analysis suggested the “kidney-specific” Slc12a1 gene was expressed in the SON and PVN, and predicted an upregulation as a consequence of 3 d of dehydration (Hindmarch et al., 2006). Quantitative PCR confirmed this (Fig. 1A), and also demonstrated an increase in expression following 7 d of salt loading. Upregulation of Slc12a1 expression rapidly follows the onset of an osmotic stimulus, evident by 1 d of dehydration or salt loading in both the SON and PVN (Fig. 1B). Indeed, following the acute osmotic stimulus of an intraperitoneal injection of hypertonic saline, a significant increase in Slc12a1 expression is seen by 240 min in the SON, and at 120 and 240 min in the PVN (Fig. 1C).
Figure 1.
Expression of Slc12a1 transcripts in the SON and PVN and upregulation by osmotic cues. A, Significant increase in Slc12a1 transcripts in the SON and PVN following 7 d of salt loading (SL) or 3 d of dehydration (DH). B, Significant increase in Slc12a1 transcripts in the SON and PVN following 1 d of salt loading (1 d SL) or 1 d of dehydration (1 d DH). C, Following an intraperitoneal injection hypertonic saline, the increase in the abundance of Slc12a1 transcripts reaches significance at 240 min in the SON, and at 120 and 240 min in the PVN; *p < 0.05, **p < 0.01, and ***p < 0.001. D, Low-resolution in situ hybridization analysis of the expression of Slc12a1 transcripts in the kidney of control and 3 d dehydrated rats as detected by specific antisense probes. The inset shows a representative picture of the low, nonspecific background signal produced by the same amount of sense probe incubated with a dehydrated kidney section. The sense and antisense experiments were processed identically at the same time. C, cortex; M, medulla. E, Low-resolution in situ hybridization analysis of the expression of Slc12a1 transcripts in the hypothalamus of control and 3 d dehydrated rats (SON and PVN). F, High-resolution in situ hybridization analysis of the expression of Slc12a1 transcripts in the SON of control and 3 d dehydrated rats viewed under low (10×) or high (100×) magnification. CT, control.
Spatial distribution of NKCC2 expression in the SON and PVN
Further validation was obtained by in situ hybridization. cRNA probes were first tested on the kidney. While sense probes did produce weak, diffuse nonspecific background signal (Fig. 1D, inset), antisense probes revealed the robust presence of Slc12a1-encoded transcripts in the cortex and medulla of the kidney (Fig. 1D), as expected. Slc12a1 expression in both the kidney medulla and cortex was upregulated by dehydration (Fig. 1D; medulla: control 1 ± 0.108, dehydrated 1.368 ± 0.118, p = 0.052, n = 4; cortex: control 1 ± 0.123, dehydrated 1.494 ± 0.130, p = 0.032, n = 4), consistent with a previous report of increased NKCC2 protein in the kidney as a consequence of water restriction (Ecelbarger et al., 2001). Importantly, Slc12a1 mRNA was detected in the SON of both control and 3 d dehydrated animals (Fig. 1E), wherein significant upregulation followed 3 d of dehydration (control 1 ± 0.109, dehydrated 1.585 ± 0.167, p = 0.019, n = 5). High-resolution in situ hybridization analysis suggested that the Slc12a1 gene is expressed in MCNs (Fig. 1F).
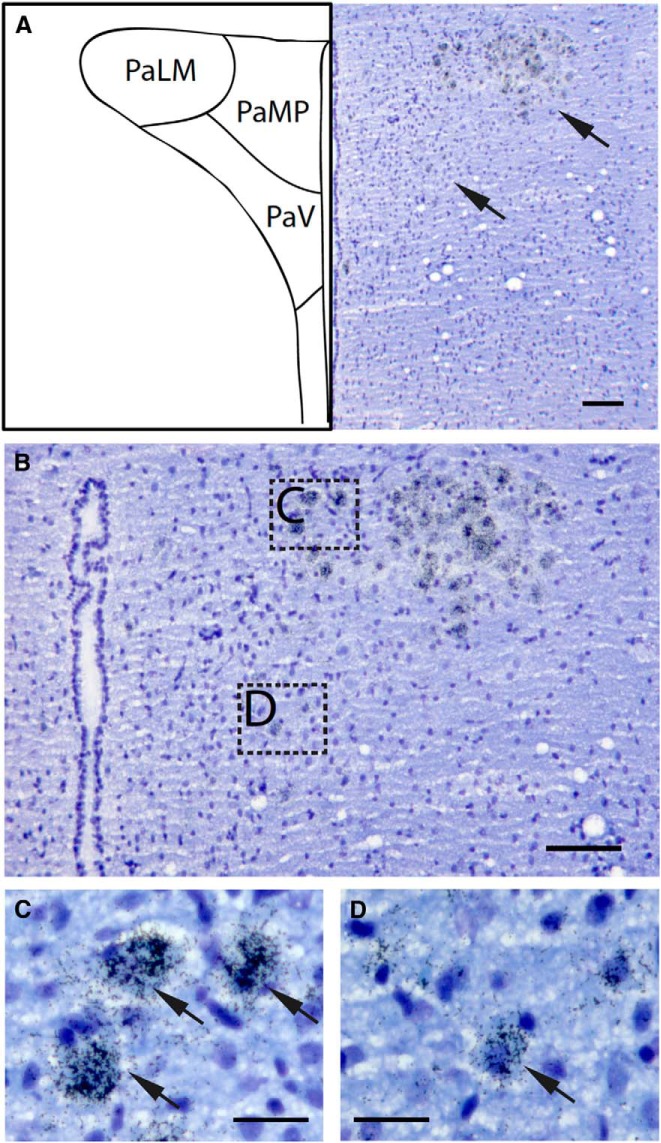
Grain counting revealed an overall increase in Slc12a1 expression in the SON (control 1 ± 0.076, dehydrated 1.585 ± 0.131, p = 0.005, n = 5; raw data: control 45.5 ± 7.21, dehydrated 67.4 ± 12.41, p = 0.00469), and an increase in the number of expressing cells (control 1 ± 0.122, dehydrated 2.973 ± 0.234, p = 0.00007, n = 5; raw data: control 33.3 ± 9.09, dehydrated 99 ± 17.45, p = 7.155E-05). In the PVN, no Slc12a1 transcripts could be detected in the control, euhydrated rats, but expression was seen following dehydration (Fig. 1E). High-resolution in situ hybridization revealed abundant expression in neurons of the magnocellular subdivision with a lower level of expression in parvocellular cells (Fig. 2; magnocellular 71.4 ± 14.25 grains/cell, n = 10; parvocellular 32 ± 7.97, n = 6, p = 7.495E-5). More magnocellular cells express Slc12a1 than parvocellular cells (magnocellular 61.33 ± 8.33, parvocellular 14.33 ± 7.77; p = 0.002, n = 3).
Figure 2.
The distribution of Slc12a1 mRNA in the PVN of a dehydrated rat. Representative photomicrographs showing the distribution of Slc12a1 mRNA in the PVN of a dehydrated rat as demonstrated by in situ hybridization histochemistry. A, Prominent labeling was observed in the magnocellular compartment of the PVN while lower expression was detected in the parvocellular regions. The pattern of distribution can be clearly observed in B. Higher power photomicrographs of the magnocellular and parvocellular subdivisions are shown in C and D, respectively (indicated by the dashed boxes in B). The arrows point to cells expressing the Slc12a1 transcript, where magnocellular neurons show much higher levels of expression. Scale bars: A, B, 100 μm; C, D, 50 μm. PaLM, paraventricular nucleus of the hypothalamus, lateral magnocellular part; PaMP, medial parvocellular part; PaV, ventral parvocellular part.
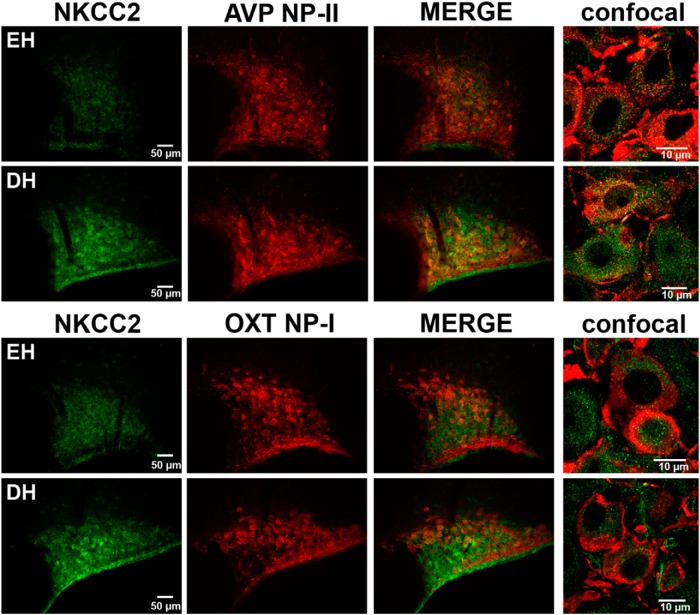
NKCC2 is expressed in AVP and OXT neurons following dehydration
We then asked whether the HNS Slc12a1 transcripts are translated. A low level of NKCC2-like immunoreactivity is seen in the SON of euhydrated rats, whereas robust expression is seen following 3 d of dehydration (Fig. 3). Both AVP and OXT neurons contain NKCC2-immunoreactive material (Fig. 3).
Figure 3.
NKCC2 is expressed in AVP and OXT neurons following dehydration. Immunocytochemistry reveals that the Slc12a1 transcripts expressed in the SON are translated into NKCC2-like material that colocalizes with both AVP and OXT. This is particularly evident in the higher magnification confocal images. Comparing the low level of NKCC2-like material in euhydrated (EH) rats with 3 d dehydrated (DH) animals reveals an increase in immunoreactivity following osmotic stimulation.
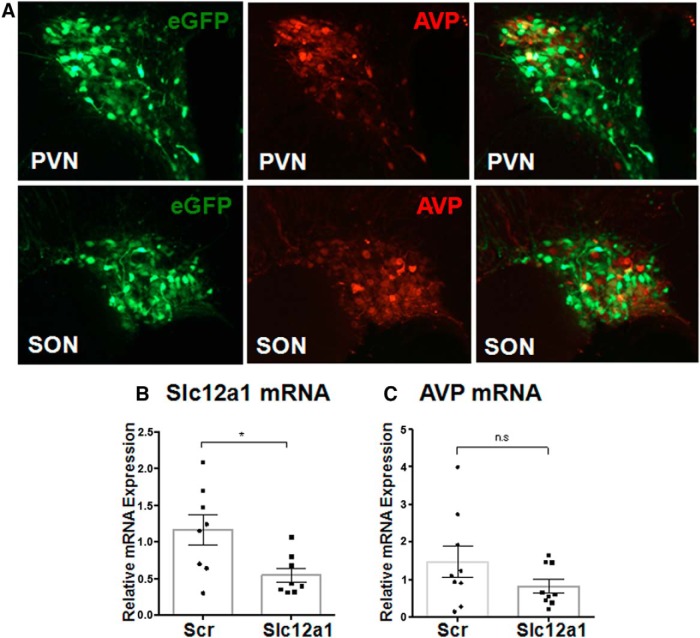
Knockdown of Slc12a1 expression affects fluid balance following salt loading
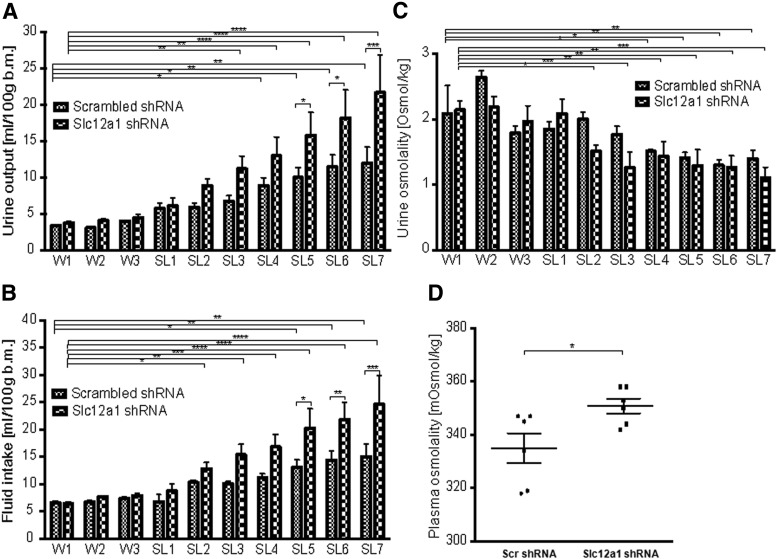
To test the hypothesis that HNS NKCC2 has a role in the central integration of the processes that conserve water following a chronic osmotic challenge, we used lentiviral-mediated shRNA delivery to knockdown Slc12a1 expression in the SON and PVN of rats in vivo. We first verified the efficacy of the shRNA knockdown strategy. First, by virtue of being tagged with an eGFP expression cassette, we showed effective delivery of lentivirus to the AVP neurons in both the PVN and SON (Fig. 4A). In PVN of salt-loaded rats, injection of the lentivirus expressing the Slc12a1-specific shRNA significantly reduced the level of endogenous Slc12a1 transcripts compared with scrambled controls (n = 8, p = 0.018; Fig. 4B), but had no effect of AVP mRNAs (Fig. 4C). In separate experiments, we showed that salt loading significantly increases fluid intake (Fig. 5A) and urine output (Fig. 5B), but lowers urine osmolality (Fig. 5C), in animals transduced in the both PVN and SON with either a lentivirus expressing an shRNA directed against Slc12a1 or a lentivirus expressing a scrambled shRNA. Compared with scrambled controls, SON and PVN Slc12a1 knockdown did not affect urine output (Fig. 5A), fluid intake (Fig. 5B), or urine osmolality (Fig. 5C) under euhydrated conditions. However, following salt loading, Slc12a1 knockdown increased urine output (significant at days 5–7; Fig. 5A) and fluid intake (significant at days 5–7; Fig. 5B), but had no significant effect on urine osmolality (Fig. 5C). Importantly, at the end of the experiment, after 7 d of salt loading, we saw a significant increase in plasma osmolality as a consequence of Slc12a1 knockdown (Fig. 5D).
Figure 4.
Expression of an eGFP-tagged lentiviral vector expressing a specific Slc12a1 shRNA reduces Slc12a1 mRNA levels. A, Lentiviral gene delivery into the SON and PVN as evidenced by robust expression of the eGFP expression tag. Colocalization reveals that eGFP is expressed in neurons containing AVP-like immunoreactivity. Lentiviral-mediated delivery of an shRNA specifically directed against Slc12a1 transcripts (Slc12a1) reduces Slc12a1 mRNA levels in the salt-loaded PVN compared with animals expressing a scrambled (Scr) shRNA (B), but has no significant effect on AVP transcripts (C).
Figure 5.
Knockdown of Slc12a1 expression affects fluid balance following salt loading. Impact of the shRNA-mediated Slc12a1 gene knockdown in the rat PVN and SON on fluid balance in comparison with animals receiving a scrambled (Scr) shRNA. Physiological parameters were monitored for 10 consecutive days, with the animals receiving water for 3 d (W1–W3) followed by 2% (w/v) NaCl for 7 d (SL1–SL7). Urine output (A), fluid intake (B), and urine osmolality (C) were measured daily. Two-way ANOVA with uncorrected Fisher's LSD test, mean ± SEM, n = 6 and 6. At the end of the experiment, plasma osmolality (D) and plasma AVP (E) was measured. Two-tailed unpaired Student's t test, mean ± SEM, n = 6 and 6. *p < 0.05, **p < 0.01, ***p < 0.001, and ****p < 0.0001.
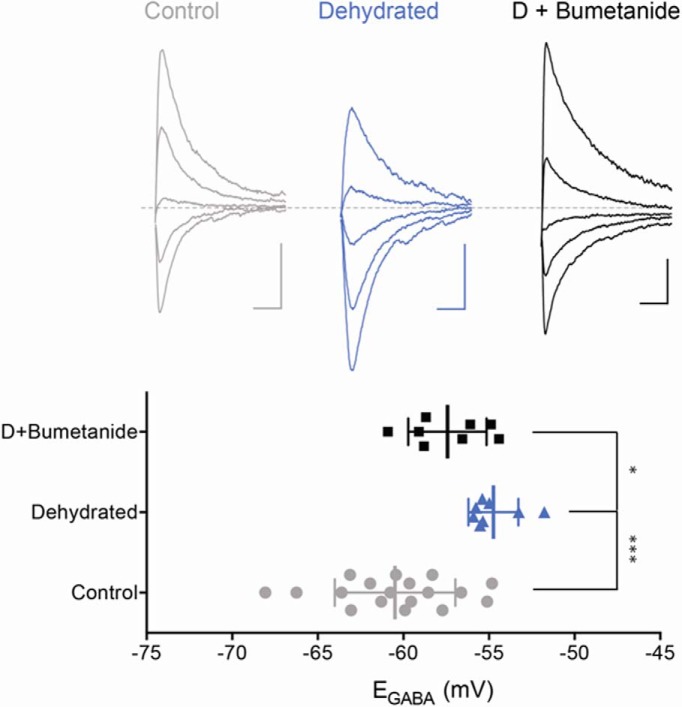
Dehydration-evoked GABA-mediated excitation of AVP neurons is reversed by bumetanide
Upregulation of NKCC2 in magnocellular neurons during dehydration predicts an enhanced Cl− intake into the cells resulting in a depolarized shift in the reversal potential of GABAA receptor (GABAAR)-mediated synaptic current (EGABA). To test this, we conducted electrophysiological recordings in ex vivo PVN slices prepared from normal and 3 d dehydrated rats. AVP-expressing MNCs were identified by the expression of eGFP driven by the promoter activities of AVP (Ueta et al., 2005) and the electrophysiological fingerprint characteristic of magnocellular neurons (Tasker and Dudek, 1993). Using whole-cell recording, we examined the relationship between postsynaptic membrane voltage and the amplitude of eIPSCs in control slices (Fig. 6). When this experiment was repeated following 3 d dehydration, we observed a significant depolarizing shift in EGABA (Fig. 6; control: −60 ± 0.8 mV, n = 18; and dehydrated: −54.7 ± 0.5, n = 8, p < 0.001). NKCC2 inhibition by bumetanide (50–100 μm) in slices from dehydrated rats caused a significant hyperpolarizing shift of EGABA (57.7 ± 0.7 mV, n = 10, p < 0.05), indicating NKCC2-dependent Cl− accumulation during dehydration.
Figure 6.
Dehydration causes a depolarizing shift in EGABA through a bumetanide-sensitive mechanism. Whole-cell recordings show that 3 d of dehydration causes a depolarizing shift in EGABA (p < 0.001). A bath application of bumetanide (50–100 μm) partially but significantly reversed the dehydration-induced polarizing shift (p < 0.05). Top traces are from holding potentials as −78, −68, −58, −48, and −38 mV. Calibration: 20 pA and 10 ms.
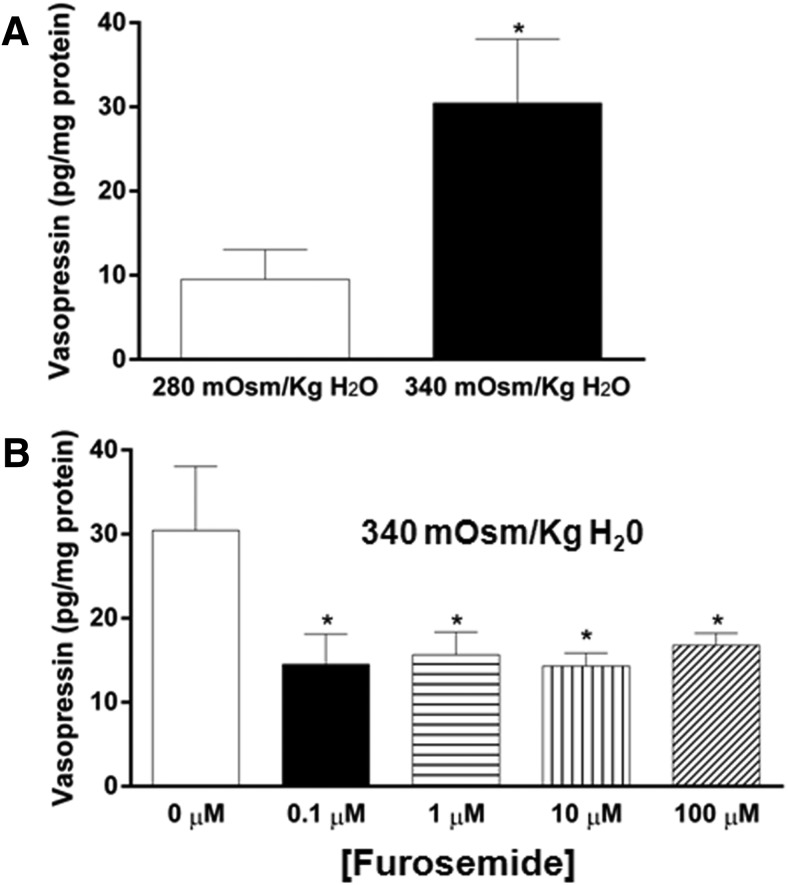
Furosemide blocks AVP release
As NKCC2 is the molecular target of the loop diuretics bumetanide and furosemide, drugs commonly used in clinical medicine for the treatment of the edema caused by congestive heart failure (Shankar and Brater, 2003), the possible effects of these drugs on HNS function should now be considered, particularly in patients with insufficient hydration. We therefore asked whether furosemide affected the response to 24 h of dehydration, during which time there is a robust and significant increase in Slc12a1 expression in both SON and PVN (Fig. 1B). As expected, dehydration for 1 d leads to a significant increase in plasma osmolality (Fig. 7A), hematocrit (Fig. 7B), and AVP (Fig. 7C) compared with the control rats (all p < 0.001). In contrast, the furosemide-treated rats (20 mg of furosemide/kg of body weight) showed an increase in hematocrit, with no differences in plasma osmolality, and significantly reduced plasma AVP levels compared with the control rats (Fig. 7D–F; p < 0.001).
Figure 7.
Effect of dehydration and furosemide treatment on plasma AVP. A–C, Significant increase in plasma AVP concentration associated with an increased plasma osmolality and hematocrit in 1 d dehydrated rats (DH). Control, CT. D–F, Significant decrease in plasma AVP concentration, with no changes in plasma osmolality and increase in hematocrit in furosemide-treated rats (Furo); ***p < 0.001.
We calculated that a peripheral dose of 20 mg/kg of furosemide should result in a CSF concentration of ∼12.59 μm, since 99% of furosemide is found bound to plasma proteins, and is unable to cross the BBB, and only 0.75% of free furosemide crosses the BBB (Javaheri et al., 1994). We thus asked whether low concentrations of furosemide (0.1–100 μm) could inhibit hyperosmolality-induced AVP secretion from hypothalamic explants (Gomes et al., 2004, 2010). First, we demonstrated that incubation of the hypothalamic explants with hypertonic KRBG solution (340 mOsm/kg H2O) induced an increase in AVP release (9.5 ± 3.5 vs 30.4 ± 7.6 pg/mg protein, p < 0.05) compared with iso-osmotic conditions (280 mOsm/kg H2O; Fig. 8A). The addition of furosemide to the hypertonic solution significantly reversed the increase in AVP release at all concentrations (for example, no furosemide: 30.4 ± 7.6 pg/mg protein; 10 mm furosemide: 14.3 ± 1.5 pg/mg protein; p < 0.05; Fig. 8B). Even at the lowest concentration used, furosemide has already achieved its maximal effect, suggesting that it is a potent inhibitor of AVP secretion.
Figure 8.
Low concentrations of furosemide inhibit hyperosmolality-induced AVP release from hypothalamic explants. A, Effect of osmolality on AVP release from MBH explants. Student's t test: t(9) = 2.645; *, differs from 280 mOsm/kg H2O, p < 0.005. B, Effect of 0.1, 1, 10, and 100 μm furosemide on hyperosmolality-induced AVP release from MBH explants. One-way factorial ANOVA: F(4,26) = 3.067, p < 0.05; *, differs from 0 μm, p < 0.05 (Dunnett's post hoc).
Discussion
For the first time, we have shown expression of the Slc12a1 gene that encodes the Na(+)-K(+)-2Cl(−)cotransporter 2, NKCC2, in the rat brain. In euhydrated animals, expression is very low in the SON and PVN, but is increased by the chronic osmotic stimuli of dehydration or salt loading (within 1 d of onset), and by the acute stimulus of an intraperitoneal injection of hypertonic saline (within hours). NKCC2-like immunoreactivity is found in both vasopressinergic and oxytocinergic neurons. Lentiviral-mediated knockdown of Slc12a1 gene in the SON and PVN significantly altered fluid handling during salt loading—rats produced more urine than scrambled shRNA-injected control, concomitant with an increased intake of hypertonic saline solution. Although urine osmolality was unchanged, plasma osmolality was increased by Slc12a1 knockdown. Drugs that inhibit NKCC2 activity affect HNS activity—dehydration-evoked GABA-mediated excitation of AVP neurons was reversed by bumetanide, and furosemide blocked AVP release both in vivo and in hypothalamic explants.
NKCC2 was previously thought to be kidney specific. We have now shown that this protein is also expressed in a region of the brain regulating salt and water homeostasis. More remarkable is the fact that it is expressed in the HNS, a specialized brain region that is responsible for the elaboration of peptide hormones that directly control kidney function. Thus, the same gene has been recruited both centrally and peripherally to participate in the crucial mechanisms that defend salt and water balance. At the level of the kidney, NKCC2 is regulated by AVP, acting through V2-type receptors linked to cAMP, both in terms of biosynthesis (Ecelbarger et al., 2001) and function (Giménez and Forbush, 2003; Caceres et al., 2009). We note that V2 receptors have recently been described in AVP neurons (Sato et al., 2011), where they mediate autocrine signaling of somatodendritically released AVP under hypo-osmotic conditions, hence enhancing volume-sensitive anion channel activity and thereby facilitating cell volume regulation. Further, it is known that cAMP levels increase in the SON and PVN following osmotic stimulation (Carter and Murphy, 1989), and that intranuclear somatodendritic release of AVP is increased by hyperosmolality (Ludwig et al., 1994; Gillard et al., 2007). It is thus intriguing to speculate that AVP from an endocrine source (acting on the kidney) or a paracrine/autocrine source (within the SON and PVN) is acting on the same receptor and signaling systems to provoke NKCC2 synthesis and activity.
Our in situ hybridization experiments did not detect any Slc12a1 expression outside of the SON and PVN at the level of the hypothalamus. However, we did not perform a comprehensive screen of the entire brain, as our aim was simply to validate the array data. That said, our transcriptomic analyses of the neuro-intermediate lobe of the pituitary (Hindmarch et al., 2006), the nucleus of the solitary tract (Colombari et al., 2011) the area postrema (Hindmarch et al., 2011), and the subfornical organ (Hindmarch et al., 2008) in both control and dehydrated rats would suggest that the Slc12a1 gene is not expressed in these osmoregulatory brain regions.
Although our immunocytochemistry results revealed expression in both AVP and OXT neurons, our studies have focused on the former. The release of AVP is governed by MCN firing frequency and pattern (Dutton and Dyball, 1979), which, in turn, is regulated by synaptic activity (MacVicar et al., 1982). The SON and PVN are densely innervated by GABAergic afferents (Decavel and van den Pol, 1990). In adult brain, GABA is an inhibitory neurotransmitter (Macdonald and Olsen, 1994). A low extracellular Cl− concentration, as found in the adult brain, causes the GABA reversal potential (EGABA) to be more negative relative to resting potential, which leads to membrane hyperpolarization following an opening of GABAAR channels. However, a high extracellular Cl− concentration causes a depolarizing shift in EGABA and either attenuates GABAAR-dependent hyperpolarizations at resting membrane potential, or causes GABAA-dependent depolarizations (Prescott et al., 2006; Choi et al., 2008). Recently, it has been shown that GABA is excitatory in adult AVP neurons (Kim et al., 2011; Haam et al., 2012) and that this effect is increased by chronic hyperosmotic stress of salt loading. These authors attributed these effects to Na(+)-K(+)-2Cl(−)cotransporter 1 (NKCC1), encoded by the Slc12a2 gene. We suggest that NKCC2, the product of the Slc12a1 gene, may also be important in this regard. While structurally closely related, NKCC1 and NKCC2 differ in functional properties, transcriptional regulation, and post-translational modulation of activity (Markadieu and Delpire, 2014), all of which may contribute to their relative role in AVP neuron function. Whether NKCC2 plays a similar role in OXT neurons, perhaps in the context of lactation, remains to be determined.
We show that the Slc12a1 gene is also expressed in the parvocellular portion of the PVN following dehydration (Fig. 4). These neurons project to the external zone of the median eminence (Vandesande et al., 1977), thus mediating stress responses (Smith and Vale, 2006), and to pre-autonomic areas, including the intermediolateral cell column of the spinal cord and the rostral ventrolateral medulla (Stocker et al., 2004), which are key premotor components of the sympathetic nervous system that regulates blood pressure and heart rate (Coote, 2005). We cannot assign a specific function to the Slc12a1-expressing parvocellular neurons that we have identified, but we note that blood pressure increases following dehydration, which is mediated by increased sympathetic nerve activity (Colombari et al., 2011). It is possible that this could be mediated via GABAergic excitation of PVN parvocellular neurons, which, in turn, would mediate activation of the sympathetic nervous system. Such a mechanism might have implications for the etiology of neurogenic hypertension.
Finally, we note that NKCC2 is the molecular target of the loop diuretics bumetanide and furosemide, drugs commonly used in clinical medicine for the treatment of the edema caused by congestive heart failure (Shankar and Brater, 2003). As both furosemide (Javaheri et al., 1994) and bumetanide (Li et al., 2011) are able to cross the blood–brain barrier, the possible effects of these drugs on HNS function should now be considered, particularly in patients with insufficient hydration.
Footnotes
We gratefully acknowledge the support of the Biotechnology and Biological Sciences Research Council (BB/G006156/1 to A.K., M.P.G., J.P., D.M.; BB/J015415/1 to M.G., J.P., D.M.), the BHF (RG/11/6/28714 to M.P.G., J.P., D.M.; FS/12/5/29339 to A.M.), a Wellcome Trust ISSF-Postdoctoral Research Staff Award (097822/Z/11/Z to A.K.), the University of Cardiff (A.K.), and a University of Malaya High Impact Research Chancellory Grant (UM.C/625/1/HIR/MOHE/MED/22 H-20001-E000086S to S.Z.H., A.d.S.M., C.H., D.M.). We thank Harold Gainer (National Institute of Neurological Disorders and Stroke—National Institutes of Health) for providing us with antibodies recognizing AVP NP-II and OXT NP-I.
The authors declare no competing financial interests.
References
- Anderson JW, Washburn DL, Ferguson AV. Intrinsic osmosensitivity of subfornical organ neurons. Neuroscience. 2000;100:539–547. doi: 10.1016/S0306-4522(00)00313-4. [DOI] [PubMed] [Google Scholar]
- Antunes-Rodrigues J, de Castro M, Elias LL, Valença MM, McCann SM. Neuroendocrine control of body fluid metabolism. Physiol Rev. 2004;84:169–208. doi: 10.1152/physrev.00017.2003. [DOI] [PubMed] [Google Scholar]
- Ares GR, Caceres PS, Ortiz PA. Molecular regulation of NKCC2 in the thick ascending limb. Am J Physiol Renal Physiol. 2011;301:F1143–F1159. doi: 10.1152/ajprenal.00396.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourque CW. Osmoregulation of vasopressin neurons: a synergy of intrinsic and synaptic processes. Prog Brain Res. 1998;119:59–76. doi: 10.1016/S0079-6123(08)61562-9. [DOI] [PubMed] [Google Scholar]
- Bourque CW, Voisin DL, Chakfe Y. Stretch-inactivated cation channels: cellular targets for modulation of osmosensitivity in supraoptic neurones. Prog Brain Res. 2002;139:85–94. doi: 10.1016/S0079-6123(02)39009-5. [DOI] [PubMed] [Google Scholar]
- Breyer MD, Ando Y. Hormonal signaling and regulation of salt and water transport in the collecting duct. Annu Rev Physiol. 1994;56:711–739. doi: 10.1146/annurev.ph.56.030194.003431. [DOI] [PubMed] [Google Scholar]
- Brownstein MJ, Russell JT, Gainer H. Synthesis, transport, and release of posterior pituitary hormones. Science. 1980;207:373–378. doi: 10.1126/science.6153132. [DOI] [PubMed] [Google Scholar]
- Caceres PS, Ares GR, Ortiz PA. cAMP stimulates apical exocytosis of the renal Na(+)-K(+)-2Cl(−) cotransporter NKCC2 in the thick ascending limb: role of protein kinase A. J Biol Chem. 2009;284:24965–24971. doi: 10.1074/jbc.M109.037135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter DA, Murphy D. Cyclic nucleotide dynamics in the rat hypothalamus during osmotic stimulation: in vivo and in vitro studies. Brain Res. 1989;487:350–356. doi: 10.1016/0006-8993(89)90839-1. [DOI] [PubMed] [Google Scholar]
- Choi HJ, Lee CJ, Schroeder A, Kim YS, Jung SH, Kim JS, Kim do Y, Son EJ, Han HC, Hong SK, Colwell CS, Kim YI. Excitatory actions of GABA in the suprachiasmatic nucleus. J Neurosci. 2008;28:5450–5459. doi: 10.1523/JNEUROSCI.5750-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colombari DS, Colombari E, Freiria-Oliveira AH, Antunes VR, Yao ST, Hindmarch C, Ferguson AV, Fry M, Murphy D, Paton JF. Switching control of sympathetic activity from forebrain to hindbrain in chronic dehydration. J Physiol. 2011;589:4457–4471. doi: 10.1113/jphysiol.2011.210245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coote JH. A role for the paraventricular nucleus of the hypothalamus in the autonomic control of heart and kidney. Exp Physiol. 2005;90:169–173. doi: 10.1113/expphysiol.2004.029041. [DOI] [PubMed] [Google Scholar]
- de Bree FM. Trafficking of the vasopressin and oxytocin prohormone through the regulated secretory pathway. J Neuroendocrinol. 2000;12:589–594. doi: 10.1046/j.1365-2826.2000.00521.x. [DOI] [PubMed] [Google Scholar]
- Decavel C, Van den Pol AN. GABA: a dominant neurotransmitter in the hypothalamus. J Comp Neurol. 1990;302:1019–1037. doi: 10.1002/cne.903020423. [DOI] [PubMed] [Google Scholar]
- Dutton A, Dyball RE. Phasic firing enhances vasopressin release from the rat neurohypophysis. J Physiol. 1979;290:433–440. doi: 10.1113/jphysiol.1979.sp012781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyball RE, McKenzie DN, Thomas GP. Osmoresponsiveness of the rat supraoptic nucleus in vivo depends on glutamatergic inputs. Neurobiology. 1995;3:351–362. [PubMed] [Google Scholar]
- Ecelbarger CA, Kim GH, Wade JB, Knepper MA. Regulation of the abundance of renal sodium transporters and channels by vasopressin. Exp Neurol. 2001;171:227–234. doi: 10.1006/exnr.2001.7775. [DOI] [PubMed] [Google Scholar]
- Gillard ER, Coburn CG, de Leon A, Snissarenko EP, Bauce LG, Pittman QJ, Hou B, Currás-Collazo MC. Vasopressin autoreceptors and nitric oxide-dependent glutamate release are required for somatodendritic vasopressin release from rat magnocellular neuroendocrine cells responding to osmotic stimuli. Endocrinology. 2007;148:479–489. doi: 10.1210/en.2006-0995. [DOI] [PubMed] [Google Scholar]
- Giménez I, Forbush B. Short-term stimulation of the renal Na-K-Cl cotransporter (NKCC2) by vasopressin involves phosphorylation and membrane translocation of the protein. J Biol Chem. 2003;278:26946–26951. doi: 10.1074/jbc.M303435200. [DOI] [PubMed] [Google Scholar]
- Glasgow E, Kusano K, Chin H, Mezey E, Young WS, 3rd, Gainer H. Single cell reverse transcription-polymerase chain reaction analysis of rat supraoptic magnocellular neurones: neuropeptide phenotypes and high voltage-gated calcium channel subtypes. Endocrinology. 1999;140:5391–5401. doi: 10.1210/endo.140.11.7136. [DOI] [PubMed] [Google Scholar]
- Gomes DA, Reis WL, Ventura RR, Giusti-Paiva A, Elias LL, Cunha FQ, Antunes-Rodrigues J. The role of carbon monoxide and nitric oxide in hyperosmolality-induced atrial natriuretic peptide release by hypothalamus in vitro. Brain Res. 2004;1016:33–39. doi: 10.1016/j.brainres.2004.04.047. [DOI] [PubMed] [Google Scholar]
- Gomes DA, Giusti-Paiva A, Ventura RR, Elias LL, Cunha FQ, Antunes-Rodrigues J. Carbon monoxide and nitric oxide modulate hyperosmolality-induced oxytocin secretion by the hypothalamus in vitro. Biosci Rep. 2010;30:351–357. doi: 10.1042/BSR20090010. [DOI] [PubMed] [Google Scholar]
- Haam J, Popescu IR, Morton LA, Halmos KC, Teruyama R, Ueta Y, Tasker JG. GABA is excitatory in adult vasopressinergic neuroendocrine cells. J Neurosci. 2012;32:572–582. doi: 10.1523/JNEUROSCI.3826-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao S, Zhao H, Darzynkiewicz Z, Battula S, Ferreri NR. Differential regulation of NFAT5 by NKCC2 isoforms in medullary thick ascending limb (mTAL) cells. Am J Physiol Renal Physiol. 2011;300:F966–FF975. doi: 10.1152/ajprenal.00408.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatton GI. Function-related plasticity in hypothalamus. Annu Rev Neurosci. 1997;20:375–397. doi: 10.1146/annurev.neuro.20.1.375. [DOI] [PubMed] [Google Scholar]
- Hindmarch C, Yao S, Beighton G, Paton J, Murphy D. A comprehensive description of the transcriptome of the hypothalamo-neurohypophyseal system in euhydrated and dehydrated rats. Proc Natl Acad Sci U S A. 2006;103:1609–1614. doi: 10.1073/pnas.0507450103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hindmarch C, Fry M, Yao ST, Smith PM, Murphy D, Ferguson AV. Microarray analysis of the transcriptome of the subfornical organ in the rat: regulation by fluid and food deprivation. Am J Physiol Regul Integr Comp Physiol. 2008;295:R1914–R1920. doi: 10.1152/ajpregu.90560.2008. [DOI] [PubMed] [Google Scholar]
- Hindmarch CC, Fry M, Smith PM, Yao ST, Hazell GG, Lolait SJ, Paton JF, Ferguson AV, Murphy D. The transcriptome of the medullary area postrema: the thirsty rat, the hungry rat and the hypertensive rat. Exp Physiol. 2011;96:495–504. doi: 10.1113/expphysiol.2010.056515. [DOI] [PubMed] [Google Scholar]
- Hu B, Bourque CW. NMDA receptor-mediated rhythmic bursting activity in rat supraoptic nucleus neurones in vitro. J Physiol. 1992;458:667–687. doi: 10.1113/jphysiol.1992.sp019440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang W, Lee SL, Arnason SS, Sjöquist M. Dehydration natriuresis in male rats is mediated by oxytocin. Am J Physiol. 1996;270:R427–R433. doi: 10.1152/ajpregu.1996.270.2.R427. [DOI] [PubMed] [Google Scholar]
- Javaheri S, Corbett W, Adams JM, Davis PJ, Gartside PS. Acute respiratory acidosis: large-dose furosemide and cerebrospinal fluid ions. J Appl Physiol. 1994;76:2651–2655. doi: 10.1152/jappl.1994.76.6.2651. [DOI] [PubMed] [Google Scholar]
- Kim JS, Kim WB, Kim YB, Lee Y, Kim YS, Shen FY, Lee SW, Park D, Choi HJ, Hur J, Park JJ, Han HC, Colwell CS, Cho YW, Kim YI. Chronic hyperosmotic stress converts GABAergic inhibition into excitation in vasopressin and oxytocin neurones in the rat. J Neurosci. 2011;31:13312–13322. doi: 10.1523/JNEUROSCI.1440-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Cleary R, Kellogg M, Soul JS, Berry GT, Jensen FE. Sensitive isotope dilution liquid chromatography/tandem mass spectrometry method for quantitative analysis of bumetanide in serum and brain tissue. J Chromatogr B Analyt Technol Biomed Life Sci. 2011;879:998–1002. doi: 10.1016/j.jchromb.2011.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- Ludwig M, Callahan MF, Neumann I, Landgraf R, Morris M. Systemic osmotic stimulation increases vasopressin and oxytocin release within the supraoptic nucleus. J Neuroendocrinol. 1994;6:369–373. doi: 10.1111/j.1365-2826.1994.tb00595.x. [DOI] [PubMed] [Google Scholar]
- Macdonald RL, Olsen RW. GABAA receptor channels. Annu Rev Neurosci. 1994;17:569–602. doi: 10.1146/annurev.ne.17.030194.003033. [DOI] [PubMed] [Google Scholar]
- MacVicar BA, Andrew RD, Dudek FE, Hatton GI. Synaptic inputs and action potentials of magnocellular neuropeptidergic cells: intracellular recording and staining in slices of rat hypothalamus. Brain Res Bull. 1982;8:87–93. doi: 10.1016/0361-9230(82)90031-4. [DOI] [PubMed] [Google Scholar]
- Markadieu N, Delpire E. Physiology and pathophysiology of SLC12A1/2 transporters. Pflugers Arch. 2014;466:91–105. doi: 10.1007/s00424-013-1370-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinley MJ, Gerstberger R, Mathai ML, Oldfield BJ, Schmid H. The lamina terminalis and its role in fluid and electrolyte homeostasis. J Clin Neurosci. 1999;6:289–301. doi: 10.1016/S0967-5868(99)90050-4. [DOI] [PubMed] [Google Scholar]
- McKinley MJ, Mathai ML, McAllen RM, McClear RC, Miselis RR, Pennington GL, Vivas L, Wade JD, Oldfield BJ. Vasopressin secretion: osmotic and hormonal regulation by the lamina terminalis. J Neuroendocrinol. 2004;16:340–347. doi: 10.1111/j.0953-8194.2004.01184.x. [DOI] [PubMed] [Google Scholar]
- Mohr E, Bahnsen U, Kiessling C, Richter D. Expression of the vasopressin and oxytocin genes in rats occurs in mutually exclusive sets of hypothalamic neurones. FEBS Lett. 1988;242:144–148. doi: 10.1016/0014-5793(88)81003-2. [DOI] [PubMed] [Google Scholar]
- Nissen R, Hu B, Renaud LP. N-methyl-d-aspartate receptor antagonist ketamine selectively attenuates spontaneous phasic activity of supraoptic vasopressin neurones in vivo. Neuroscience. 1994;59:115–120. doi: 10.1016/0306-4522(94)90103-1. [DOI] [PubMed] [Google Scholar]
- Onaka T, Yagi K. Involvement of N-methyl-D-aspartic acid receptor activation in oxytocin and vasopressin release after osmotic stimuli in rats. J Neuroendocrinol. 2001;13:166–174. doi: 10.1046/j.1365-2826.2001.00607.x. [DOI] [PubMed] [Google Scholar]
- Panyasrivanit M, Greenwood MP, Murphy D, Isidoro C, Auewarakul P, Smith DR. Induced autophagy reduces virus output in dengue infected monocytic cells. Virology. 2011;418:74–84. doi: 10.1016/j.virol.2011.07.010. [DOI] [PubMed] [Google Scholar]
- Prescott SA, Sejnowski TJ, De Koninck Y. Reduction of anion reversal potential subverts the inhibitory control of firing rate in spinal lamina I neurones: towards a biophysical basis for neuropathic pain. Mol Pain. 2006;2:32. doi: 10.1186/1744-8069-2-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu J, Yao S, Hindmarch C, Antunes V, Paton J, Murphy D. Transcription factor expression in the hypothalamo-neurohypophyseal system of the dehydrated rat; up-regulation of gonadotrophin inducible transcription factor 1 mRNA is mediated by cAMP-dependent protein kinase A. J Neurosci. 2007;27:2196–2203. doi: 10.1523/JNEUROSCI.5420-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato K, Numata T, Saito T, Ueta Y, Okada Y. V2 receptor-mediated autocrine role of somatodendritic release of AVP in rat vasopressin neurones under hypo-osmotic conditions. Sci Signal. 2011;4:ra5. doi: 10.1126/scisignal.2001279. [DOI] [PubMed] [Google Scholar]
- Shankar SS, Brater DC. Loop diuretics: from the Na-K-2Cl transporter to clinical use. Am J Physiol Renal Physiol. 2003;284:F11–F21. doi: 10.1152/ajprenal.00119.2002. [DOI] [PubMed] [Google Scholar]
- Sharman G, Ghorbel M, Leroux M, Beaucourt S, Wong LF, Murphy D. Deciphering the mechanisms of homeostatic plasticity in the hypothalamo-neurohypophyseal system–genomic and gene transfer strategies. Prog Biophys Mol Biol. 2004;84:151–182. doi: 10.1016/j.pbiomolbio.2003.11.005. [DOI] [PubMed] [Google Scholar]
- Smith SM, Vale WW. The role of the hypothalamic-pituitary-adrenal axis in neuroendocrine responses to stress. Dialogues Clin Neurosci. 2006;8:383–395. doi: 10.31887/DCNS.2006.8.4/ssmith. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stocker SD, Cunningham JT, Toney GM. Water deprivation increases Fos immunoreactivity in PVN autonomic neurons with projections to the spinal cord and rostral ventrolateral medulla. Am J Physiol Regul Integr Comp Physiol. 2004;287:R1172–R1183. doi: 10.1152/ajpregu.00394.2004. [DOI] [PubMed] [Google Scholar]
- Tasker JG, Dudek FE. Electrophysiological properties of neurones in the region of the paraventricular nucleus in slices of rat hypothalamus. J Physiol. 1993;469:179–192. doi: 10.1113/jphysiol.1993.sp019810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telleria-Diaz A, Grinevich VV, Jirikowski GF. Colocalization of vasopressin and oxytocin in hypothalamic magnocellular neurones in water-deprived rats. Neuropeptides. 2001;35:162–167. doi: 10.1054/npep.2001.0859. [DOI] [PubMed] [Google Scholar]
- Theodosis DT, El Majdoubi M, Pierre K, Poulain DA. Factors governing activity-dependent structural plasticity of the hypothalamoneurohypophysial system. Cell Mol Neurobiol. 1998;18:285–298. doi: 10.1023/A:1022577105819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ueta Y, Fujihara H, Serino R, Dayanithi G, Ozawa H, Matsuda K, Kawata M, Yamada J, Ueno S, Fukuda A, Murphy D. Transgenic expression of enhanced green fluorescent protein enables direct visualization for physiological studies of vasopressin neurones and isolated nerve terminals of the rat. Endocrinology. 2005;146:406–413. doi: 10.1210/en.2004-0830. [DOI] [PubMed] [Google Scholar]
- van den Pol AN, Wuarin JP, Dudek FE. Glutamate, the dominant excitatory transmitter in neuroendocrine regulation. Science. 1990;250:1276–1278. doi: 10.1126/science.1978759. [DOI] [PubMed] [Google Scholar]
- Vandesande F, Dierickx K, De Mey J. The origin of the vasopressinergic and oxytocinergic fibres of the external region of the median eminence of the rat hypophysis. Cell Tissue Res. 1977;180:443–452. doi: 10.1007/BF00220167. [DOI] [PubMed] [Google Scholar]
- Yue C, Mutsuga N, Verbalis J, Gainer H. Microarray analysis of gene expression in the supraoptic nucleus of normoosmotic and hypoosmotic rats. Cell Mol Neurobiol. 2006;26:959–978. doi: 10.1007/s10571-006-9017-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z, Bourque CW. Osmometry in osmosensory neurones. Nat Neurosci. 2003;6:1021–1022. doi: 10.1038/nn1124. [DOI] [PubMed] [Google Scholar]