Abstract
Objectives:
To assess preparedness for medical emergencies in private dental offices in Jeddah, Kingdom of Saudi Arabia (KSA).
Methods:
In this cross-sectional study, a survey was distributed to 70 dental offices and polyclinics in Jeddah, Saudi Arabia between October 2013 and January 2014. The questionnaire gathered information on the prevention of medical emergencies, the preparedness of the office personnel, and availability of emergency drugs and equipment.
Results:
For prevention, 92% (n=65) of the offices reported that they obtain a thorough medical history prior to treatment; however, only 11% (n=8) obtain vital signs for each visit. Using a preparedness percent score (0 to 100), the mean level of preparedness of the office personnel in all surveyed dental offices was 55.2±20. The availability of emergency drugs was 35±35, and equipment was 19±22.
Conclusion:
We found a deficiency in personnel training, availability of drugs, and emergency equipment in the surveyed dental clinics. More stringent rules and regulations for emergency preparedness must be reinforced to avoid disasters in these clinics.
Although uncommon, medical emergencies can occur at anytime in the dental office, possibly posing a direct threat to the patient’s life, and hindering the delivery of dental care.1,2 The prevalence, and severity of medical emergencies has been reported in various dental settings (academic or private) in many countries.3-5 In one 10-year survey study in Great Britain, an emergency event was reported, on average occurring with an average frequency of between one in 3.6-4.5 practice years.6 In a study published in 2009, Wilson et al7 found that the most prevalent medical emergency reported by dentists over a 12 month period was syncope (1.9 cases per year), followed by angina and hypoglycemia (0.17 per year), and epileptic fit (0.13 cases per year).7 Preparedness for acute medical emergencies in the dental office begins with a team approach by the dentist and staff members who have up-to date certification in basic life support (BLS) for health care providers. It also includes dentist and personnel training through mock drills and continuing education courses, a medical emergency protocol, availability of an emergency drug kit, and proper emergency equipment.8,9 The preparedness of dental offices was addressed through questionnaires for studies from different countries where a general consensus was reached for the need for continuous training and more stringent guidelines for medical emergencies.7,10 In the Kingdom of Saudi Arabia (KSA), there is a reported high prevalence of diabetes, obesity, and hypertension,11-13 all of which may contribute to a higher occurrence of medical emergencies in the dental office. A current literature search using the Medline and PubMed databases (from 1990-2014), revealed that there is a scarcity of published data on the prevalence, types, or severity of medical emergency events in government dental clinics, dental schools, or private dental practice. Additionally, no data could be found assessing the preparedness of private dental offices for medical emergencies in KSA. The Ministry of Health (MOH) in KSA oversees the licensing and operation of private dental clinics and polyclinics. It does not mandate that private dental offices have a specific emergency protocol, emergency drugs, or equipment. The objective of our study was to assess the preparedness and training of the office personnel, and availability of emergency drugs, and emergency equipment in a sample of private dental practices and polyclinics in Jeddah, KSA.
Methods
The Research Ethics Committee of the Faculty of Dentistry (REC-FD), at King AbdulAziz University, Jeddah, Saudi Arabia approved this cross-sectional study.
Subjects and questionnaire
A questionnaire was distributed to a sample of private practice dental offices and polyclinics. Inclusion criteria included any private dental practice or a polyclinic that possesses dental clinic(s) in the city of Jeddah, KSA. Random sampling was achieved by choosing offices from different geographic locations of Jeddah. No dental offices were excluded except if they refused to participate. The questionnaire was distributed and collected between October 2013 and January 2014. The dental offices participated on a voluntary basis and were assured of the confidentiality of the responses. The questionnaire was administered by one of the authors through an interview with the supervising dentist. The study was conducted in full accordance with the World Medical Association Declaration of Helsinki.
The questionnaire sought information on 4 main areas: 1) Prevention of medical emergencies: questions were asked on the frequency of the recording of vital signs (never, once during the initial visit, every visit) and on the taking of a thorough medical history prior to treatment. 2) The Preparedness of the office personnel (dentists and dental assistants): Do all the dentists and dental assistants have a valid BLS certification? Is there a written emergency protocol available and clearly posted? Are all the personnel knowledgeable of the emergency numbers to dial in cases of a medical emergency? Does the office have and implement a periodic mock emergency drill? Does the office have a registered nurse in the office? Is there a healthcare professional in the office that is able to perform advanced puncture techniques, such as an intravenous or intramuscular injection. 3) Availability of essential emergency drugs. 4) Availability of essential emergency equipment.
Data and statistical analysis
The data was entered into a spreadsheet and analyzed using the IBM SPSS Statistics for Windows, version 22 (IBM Corp, Armonk, NY, USA). The variables were expressed as means and standard deviations, whereas the difference in responses between the dental offices and polyclinics was analyzed using a t-test. The level of significance was set at p<0.05. A numerical scale (rubric) was devised to rate 3 domains: a) preparedness of office personnel: the criteria scored are: 100% of dentists must be BLS certified, 100% of dental assistants must be BLS certified, a written emergency protocol, knowledge of all the personnel of the emergency number, implementing practice drills, and ability to perform IM injections; b) availability of drugs (Table 1); and c) availability of equipment (Table 2). The responses were numerically scored 0 and 1, where 1 is a positive score and 0 is a negative score. A pooled score was collected from the answers and converted to a 100 percent scale. A preparedness score of 0 is no preparation at all, whereas 100 is 100% preparedness.
Table 1.
List of essential emergency drugs and the availability of these drugs in the surveyed dental offices in Jeddah, Saudi Arabia (N=70).
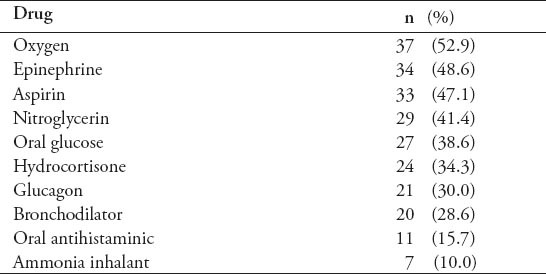
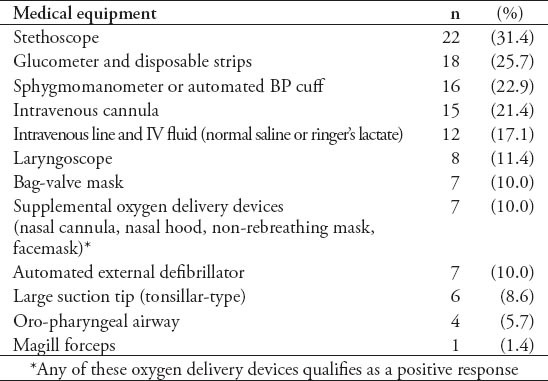
Table 2.
List of emergency medical equipment and their availability in the surveyed dental offices in Jeddah, Saudi Arabia (N=70).
Results
A total of 70 private practices participated in this survey, with 55 dental offices and 15 polyclinics. All participating dental practices performed dentistry under local anesthesia, and none performed intravenous sedation or ambulatory general anesthesia. Fifty-three percent of theses dental offices performed pediatric dentistry, whereas 45% performed oral surgery in addition to general dentistry.
Prevention
Ninety-two percent (n=65) of the offices reported that they obtained a thorough medical history prior to treatment. However, only 11% (n=8) obtain vital signs (blood pressure, heart rate, and respiratory rate) every visit, 34.3% (n=24) obtained vital signs at the initial visit only, and 57% (n=40) never take vital signs. Other vital signs (temperature, height, and weight) were reported to be taken by 18 % (n=12) of dental offices and 8.5% (n=6) of polyclinics. (Figure 1).
Figure 1.
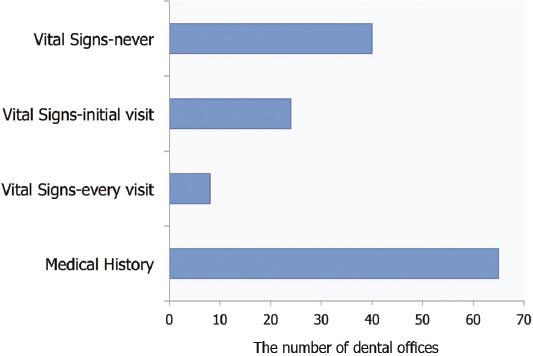
The number of respondents who obtained a medical history and vital signs prior to dental procedures among surveyed clinics in Jeddah, Saudi Arabia.
Preparedness of office personnel
All the dental offices and polyclinics replied that all their dentists were BLS certified (n=70), whereas only 81.2% (n=56) of the surveyed dental offices and polyclinics responded that all their dental assistants were BLS certified. Only 58.6% (n=41) of the surveyed clinics responded that all their office personnel were knowledgeable of the number to dial in case of an emergency. The number of offices that reported performing periodic practice (mock) drills for medical emergencies was 9 of 70 (12.9%). The presence of a registered nurse among the office personnel was in 60% (n=42) of the offices. More than half of the dental offices have an auxiliary staff member trained in intravenous injections (57%, n=40), and intramuscular injections (60%, n=42). Very few, (20%, n=14) clinics have a written protocol and flow chart for medical emergencies available to the office personnel (Figure 2).
Figure 2.
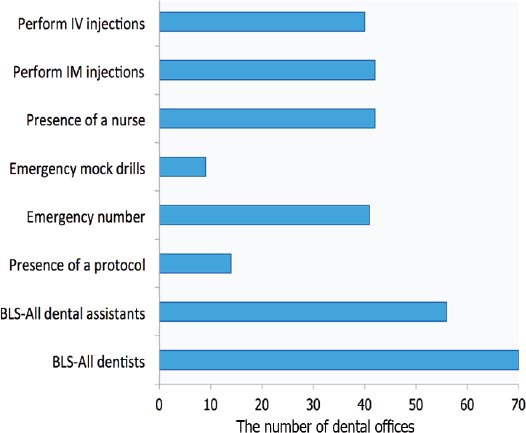
Personnel preparedness for medical emergencies among surveyed clinics in Jeddah, Saudi Arabia. IV - intravenious, IM - intramascular, BLS - basic life support
Availability of drugs
Oxygen was the most available drug in 52.9% of the surveyed offices, followed by epinephrine (48.6%), and aspirin (47.1%). The 2 least available drugs were ammonia inhalants (10%), and oral anti-histamine (15.7%). Table 2 shows the drugs available in the surveyed dental clinics. In response to the question on verifying the expiration date of the drugs, only 45.6% (n=31) responded positively.
Availability of equipment
A total of 7 of 70 offices (10%) reported that they have at least one type of supplemental oxygen delivery device, such as a facemask, non-rebreathing mask, nasal cannula, or nasal hood. Eighteen dental offices (26%, n=18) owned a glucose-meter and disposable strips. Sixteen dental offices (22.9%) have an automatic blood pressure monitor or sphygmomanometer with different size cuffs (small, medium, and large). A total of 9 of 70 (12.9%) offices reported having a laryngoscope, and only one office (1.4%) had a McGill forceps in their emergency kit. Only 7 of the 70 (10%) offices had an automated external defibrillator (AED) and bag-valve mask (BVM) for the delivery of oxygen. A full list of the available emergency equipment in each dental office is shown in Table 2.
Preparedness score
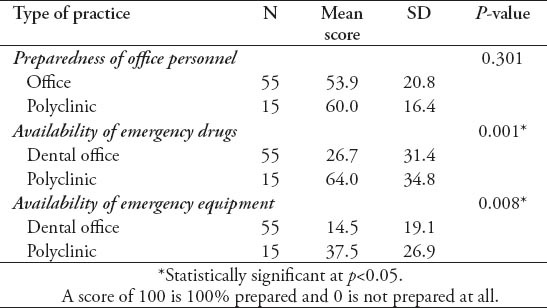
Using the preparedness percent scale (0 to 100), the mean level of preparedness of the office personnel in all surveyed dental offices was 55.2±20. The availability score for the essential emergency drugs was 35±35, and the emergency equipment was 19±22. When comparing private dental practices to polyclinics, there was no difference between the preparedness of the personnel (p=0.301). Polyclinics had a statistically significantly higher availability of emergency drugs (p<0.001) and equipment (p=0.008) (Table 3).
Table 3.
The difference in preparedness scores between the dental offices and polyclinics in Jeddah, Saudi Arabia.
Discussion
Last year, the death of a 20-year-old healthy woman in a private dental office in Jeddah, Saudi Arabia was reported in a Saudi newspaper. Her death was secondary to an undisclosed emergency that the dentist could not manage. Moreover, 13 deaths in dental offices were reported in Jeddah, in which the Directory of Health Affairs is currently investigating with a forensic committee.14 The MOH, which oversees the private dental offices, conducts periodic checks on valid practice licensing and proper infection control. The MOH does not mandate that dental offices have an emergency drug kit or equipment. It does not conduct unannounced visits or field-checks for medical emergency training and availability of emergency drugs and equipment. The average emergency response time of emergency response systems varies from one country to another. The only study assessing the response time in Saudi Arabia was in the capital city of Riyadh, where the average response time to the scene of an emergency was 10.23±5.66 minutes.15 No similar data was found in the Western region of Saudi Arabia, or Jeddah city. The response time may vary according to the traffic and availability of units in the nearby vicinity. In Makkah and Jeddah and during the Holy month of Du-Hijja, where the annual Islamic Pilgrimage takes place, Red Crescent units are dispatched near the Holy City where approximately 3 million people aggregate to perform the Hajj pilgrimage. This creates a serious potential delay in the response of an ambulance.
Dental offices must be prepared to diagnose and manage an emergency until an ambulance arrives, and the patient is transported to a hospital setting, particularly those who exist as dental practices or polyclinics that are not connected to a hospital with an emergency department. The basic algorithm for management of acute medical conditions in the dental office is; position (P), airway (A), breathing (B), circulation (C) and definitive treatment, differential diagnosis, drugs, and defibrillation (D).1,8
The 6 links of survival is a checklist of educational needs and physical items necessary to fulfill the needs of a dental patient in that time period between the identification of a medical problem and arrival of outside assistance. The links consist of doctor training, staff training, mock drills, medical emergency plan, emergency drug kit, and proper equipment.9 The emergency number to contact in case of an emergency in Saudi Arabia is 997. It was alarming that only half of the dental offices reported that all their personnel were aware of this number. When a medical emergency occurs, it is critical that office personnel respond without delay, and not knowing the number creates chaos and delays the summoning of professional help.
The Saudi Commission for Health Specialties requires proof of valid BLS training for license renewal for dentists and dental assistants. A valid BLS certification is a requirement for issuing or renewal of the Saudi Commission for Health Specialties license, which is mandatory for work in the private sector. Therefore in any dental clinic, 100% of all dentists and dental assistants in any private dental clinic or polyclinic are required to possess a valid BLS certification.
Although BLS training is considered fundamental to cope with medical emergencies, training of personnel extends beyond BLS. It also includes attending continuing education courses, practice drills, and online courses to sharpen the diagnosis and management skills of acute medical events. In a study of Brazilian dental practitioners,4 only 41% of the dentists reported feeling confident to diagnose a medical event in the dental office. The majority of them felt unable to treat anaphylaxis, myocardial infarction, or perform cardiopulmonary resuscitation (CPR) or an intravenous injection. In the UK, 20.8% of dentists felt competent to diagnose a medical emergency,2 while a study in Germany reported that 57% of the surveyed dentists believed they are able to perform bag/valve ventilation, and 49% were confident performing BLS.5
According to the American Heart Association, brain death, and permanent death start 4-6 minutes after cardiac arrest.17 The time to defibrillation is the most important determinant of survival from cardiac arrest.16 The victim’s survival rate is reduced by 7-10% with every minute that passes without defibrillation and advanced life support intervention. Few attempts at resuscitation succeed after 10 minutes.17 The use of an automated external defibrillator (AED) is essential skill in BLS training, yet this device was found in only 10% of the dental offices. Therefore, the dentist may have a BLS certificate to practice, yet the office lacks the necessary equipment to implement the BLS protocol set forth by the American Heart Association. The data presented by Muller et al5 in Germany shows that 84% of the responding dentists own an emergency bag, which contains a ventilation bag, airway equipment and oxygen, while only 2% of the dentists own a defibrillator.
For emergency drugs in the dental office, a dentist should never administer a poorly understood medication because there is no drug that can take the place of properly trained health care professionals in diagnosing conditions and treating patients in emergency situations.1,18 In this survey, there was a significant lack of availability of emergency drugs. Oxygen is essential in any medical emergency, and must be available in a portable E-cylinder to administer to a spontaneously breathing patient or under positive pressure in situations in which the patient is unconscious and not ventilating adequately.18 It was interesting to find that while approximately half the responding offices claim they have an oxygen tank, only 10% actually have at least one type of oxygen delivery device, including a bag-valve mask. The oxygen tank becomes a useless piece of equipment that cannot be utilized during an emergency without a delivery device. Syncope and pre-syncope were the most common medical emergencies in the dental office according to many studies.5,19 The initial treatment of syncope, which occurs due to inadequate cerebral perfusion consists of placement in a supine position and oxygen delivery.19 The management of emergencies in the dental office starts with prevention by obtaining a good medical history, vital signs, and referral to a specialist for further investigation if necessary. One study in Belgium found a link between the years since graduation and obtaining a medical history, the older the dentist, the less consistent was the medical history updated.19
Monitoring equipment that provides basic information for primary assessment should include a stethoscope and a sphygmomanometer or an automated blood pressure device. An automated vital signs monitor can provide physiological data, including systolic, diastolic, and mean blood pressure, along with the patient’s oxygen saturation level, heart rate, and temperature.18 Furthermore, the management of medical emergencies in the dental office is limited to supporting the vital functions of the patient until emergency medical services arrive. There is a significant concern that approximately one-fourth of the surveyed dental offices in this study owned a blood pressure monitor and glucometer. This indicates that not only are the patients not being assessed properly before the dental procedure, but it posses a risk that proper vital signs monitoring during a medical emergency cannot take place.
The limitation of this study is the number of surveyed dental offices and polyclinics as the study utilized a random sample of different geographic locations in Jeddah. Future studies should aim at including other cities and comparing the preparedness in rural and suburban office locations.
In conclusion, there is a deficiency in the preparedness of the dental offices for medical emergencies in Jeddah, Saudi Arabia in 3 main areas, personnel preparedness and training, availability of drugs, and availability of emergency equipment. Polyclinics scored higher on the preparedness score for availability of emergency drugs and emergency equipment. A preparedness of less than 100% is unacceptable. More stringent regulations for the preparedness of these dental offices should exist. The renewal of clinic licenses should be based on criteria, such as the implementation of practice emergency drills, continuing education hours in medical emergencies, a written protocol, availability of emergency drugs and equipment. Unannounced field evaluations of emergency drug and equipment availability should take place regularly by the MOH. Staff and personnel should have periodic exams to test their knowledge of emergency phone numbers, basic action plans, and protocols. A written and readily accessible protocol should exist in every dental office, for basic action plan and management of the more common emergencies that occur in the dental office, such as vasovagal syncope, hypoglycemia, chest pain, and seizures. Further studies are necessary to evaluate the prevalence of medical emergencies in private dental offices over the course of a few years. This enables the health legislator to custom-fit specific emergency algorithms according to the community’s needs and health-care problems. Additionally, a national database of adverse outcomes secondary to medical emergencies in the dental office, across Saudi Arabia, is necessary to ensure patient safety.
Footnotes
References
- 1.Reed KL. Basic management of medical emergencies: recognizing a patient's distress. J Am Dent Assoc. 2010;141(Suppl 1):20S–24S. doi: 10.14219/jada.archive.2010.0349. [DOI] [PubMed] [Google Scholar]
- 2.Girdler NM, Smith DG. Prevalence of emergency events in British dental practice and emergency management skills of British dentists. Resuscitation. 1999;41:159–167. doi: 10.1016/s0300-9572(99)00054-4. [DOI] [PubMed] [Google Scholar]
- 3.Anders PL, Comeau RL, Hatton M, Neiders ME. The nature and frequency of medical emergencies among patients in a dental school setting. J Dent Educ. 2010;74:392–396. [PubMed] [Google Scholar]
- 4.Arsati F, Montalli VA, Florio FM, Ramacciato JC, da Cunha FL, Cecanho R, et al. Brazilian dentists’ attitudes about medical emergencies during dental treatment. J Dent Educ. 2010;74:661–666. [PubMed] [Google Scholar]
- 5.Muller MP, Hansel M, Stehr SN, Weber S, Koch T. A state-wide survey of medical emergency management in dental practices: incidence of emergencies and training experience. Emerg Med J. 2008;25:296–300. doi: 10.1136/emj.2007.052936. [DOI] [PubMed] [Google Scholar]
- 6.Atherton GJ, McCaul JA, Williams SA. Medical emergencies in general dental practice in Great Britain. Part 1: Their prevalence over a 10-year period. Br Dent J. 1999;186:72–79. doi: 10.1038/sj.bdj.4800023. [DOI] [PubMed] [Google Scholar]
- 7.Wilson MH, McArdle NS, Fitzpatrick JJ, Stassen LF. Medical emergencies in dental practice. J Ir Dent Assoc. 2009;55:134–343. [PubMed] [Google Scholar]
- 8.Haas DA. Preparing dental office staff members for emergencies: developing a basic action plan. J Am Dent Assoc. 2010;141(Suppl 1):8S–13S. doi: 10.14219/jada.archive.2010.0352. [DOI] [PubMed] [Google Scholar]
- 9.Sangrik LJ. The six links of survival: a comprehensive approach to medical emergency preparedness for dental offices. Tex Dent J. 2011;128:464–465. [PubMed] [Google Scholar]
- 10.Amirchaghmaghi M, Sarabadani J, Delavarian Z, Mosannen Mozafary P, Shahri A, Dalirsani Z. The knowledge and preparedness of general dentists about medical emergencies in Iran. Iran Red Crescent Med J. 2011;13:217–218. [PMC free article] [PubMed] [Google Scholar]
- 11.Al-Nozha MM, Abdullah M, Arafah MR, Khalil MZ, Khan NB, Al-Mazrou YY, et al. Hypertension in Saudi Arabia. Saudi Med J. 2007;28:77–84. [PubMed] [Google Scholar]
- 12.Al-Nozha MM, Al-Maatouq MA, Al-Mazrou YY, Al-Harthi SS, Arafah MR, Khalil MZ, et al. Diabetes mellitus in Saudi Arabia. Saudi Med J. 2004;25:1603–1610. [PubMed] [Google Scholar]
- 13.Al-Nozha MM, Al-Mazrou YY, Al-Maatouq MA, Arafah MR, Khalil MZ, Khan NB, et al. Obesity in Saudi Arabia. Saudi Med J. 2004;25:1603–1610. [PubMed] [Google Scholar]
- 14.Dentist's error blamed for woman's death. Saudi Gazette. [Updted 2013 September 20; Access 2014 April 24]. Available from URL: http://www.saudigazette.com.sa.
- 15.Al-Ghamdi AS. Emergency medical service rescue times in Riyadh. Accident Analysis and Prevention. 2002;34:499–505. doi: 10.1016/s0001-4575(01)00047-1. [DOI] [PubMed] [Google Scholar]
- 16.Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, et al. Writing Group Members. Heart disease and stroke statistics--2010 update: a report from the American Heart Association. Circulation. 2010;121:e46–e215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 17.American Heart Association. 2005 American Heart Association (AHA) guidelines for cardiopulmonary resuscitation (CPR) and emergency cardiovascular care (ECC) of pediatric and neonatal patients: pediatric basic life support. Circulation. 2005;112(24 Suppl):IV1–IV203. doi: 10.1161/CIRCULATIONAHA.105.166550. [DOI] [PubMed] [Google Scholar]
- 18.Rosenberg M. Preparing for medical emergencies: the essential drugs and equipment for the dental office. J Am Dent Assoc. 2010;141(Suppl 1):14S–19S. doi: 10.14219/jada.archive.2010.0351. [DOI] [PubMed] [Google Scholar]
- 19.Marks LA, Van Parys C, Coppens M, Herregods L. Awareness of dental practitioners to cope with a medical emergency: a survey in Belgium. Int Dent J. 2013;63:312–316. doi: 10.1111/idj.12046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shukla GJ, Zimetbaum PJ. Cardiology patient page. Syncope. Circulation. 2006;113:e715–e717. doi: 10.1161/CIRCULATIONAHA.105.602250. [DOI] [PubMed] [Google Scholar]


