Abstract
Objectives:
To evaluate students’ perception towards the problem based learning (PBL) session in a system-based hybrid curriculum.
Methods:
We conducted a cross-sectional study in the College of Medicine, King Saud University, Saudi Arabia at the end of the 2012-2013 academic year. The survey questionnaire was self-administered, and examined perceptions of PBL session benefits, appropriate running of sessions, and tutor’s roles.
Results:
Out of 510 students, 275 (53.9%) completed the questionnaire. Most of the students reported that PBL sessions were helpful in understanding basic sciences concepts (p=0.04). In addition, they agreed that PBL sessions increased their knowledge of basic sciences (p=0.01). Most students reported that PBL sessions encouraged self-directed learning, collaborative learning, and improved decision making skills. However, 54.5% of students reported lack of proper training before starting the PBL sessions, and only 25.1% of students agreed that the teaching staff are well prepared to run the sessions. Most students used the internet (93.1%), lecture notes (76.7%), and books (64.4%) as learning resources. Most students reported repetition of topics between PBL sessions and lectures (p=0.07).
Conclusion:
The study highlighted the significant role of PBL in a system-based hybrid curriculum and helped students improve their knowledge and different learning skills. Students and staff training is required before the utilizing the PBL as an instructional method.
The transformation of the medical curriculum from traditional teacher centered to integrated student centered problem based learning (PBL), has been adopted by many medical colleges around the globe.1 In the Kingdom of Saudi Arabia (KSA), medical colleges are reforming the curriculum based on current trends in education, to meet the required global medical education standards and accreditation.2,3 Problem based learning is implemented either as pure or hybrid models.4,5 A PBL hybrid model has been adapted in KSA, and most of the Gulf Cooperation Council country medical colleges.2 In a ‘pure-PBL model’, PBL is the main instructional method implemented throughout the entire curriculum.6 However in a ‘hybrid PBL model’, learning is supported by prior knowledge of students acquired during lectures, tutorial sessions, and skills laboratories before the PBL session.7 Problem based learning is an innovative approach to learning in medical education, which has many advantages, including increasing knowledge retention, better understanding of basic sciences topics, integration of basic and clinical sciences, and improvement of problem solving skills.8,9 In addition, it contributes to the development of interpersonal and communication skills, presentation skills, promotes self-directed learning (SDL), enhances students’ enthusiasm, and motivation.10,11 However, a few studies reported that PBL as an instructional method is time consuming, and does not impact knowledge acquisition.12,13 The tutors guide the group to achieve their goals by keeping them focused on their task. The PBL sessions involve clear roles for each member of the group, known steps of discussion, and identification of the learning objectives from the discussed problem.14 Therefore, a skilled tutor plays a crucial role in the success of the PBL session.9,15
In King Saud University (KSU), Riyadh, KSA, a traditional curriculum was in practice, which used to focus on the acquisition of medical knowledge, and the memorization of facts, before implementation of a system-based hybrid PBL curriculum in the academic year 2009-2010. In addition, traditional curriculum does not prepare medical graduates for the clinical years, and it does not fulfill the needs of competent medical graduates.16 The PBL sessions are conducted in 2 sessions per week. The first session lasts for 2 hours, where students can identify their learning issues followed by SDL sessions, to search the literature for their identified learning issues. The second session lasts for 2 hours, where students discuss the acquired information among the group and solve the problem.16 In addition, the learning activities of the week include lectures and laboratories sessions, which are presented on the same theme of the PBL session. Many worldwide studies have reported a positive impact of PBL on the learning process. However, a few studies were conducted in Asia, especially in KSA, on the student’s perception of the PBL session, and indicated controversy between Malaysia and KSA findings. In KSA, a study17 showed that PBL induced better interpersonal skills and knowledge, as well as a better attitude towards patients. However, in Malaysia they showed that PBL was time consuming, and can be substituted by other instructional methods.12 Therefore, the student’s impression of the PBL session is controversial. Thus, the current study was designed to investigate the student’s perception of PBL sessions in the College of Medicine, KSU, Riyadh, KSA.
Methods
Study subjects
We conducted this cross-section study at the College of Medicine, KSU, Riyadh, KSA based on an anonymous and self-administered questionnaire on perceptions of PBL learning. The data was collected from male and female medical undergraduate students, of the first and second year, at the end of the 2012-2013 academic year. All students of the first and second academic years were included in this study. However, uncompleted questionnaires were excluded.
Data collection methods
The questionnaire was developed, based on an extensive literature search using the web based search engines PubMed, Medline, and Google scholar. We used key words ‘problem based learning’, ‘PBL in hybrid curriculum’, ‘PBL and increase of knowledge’, PBL and skill development’, ‘PBL and self-directed learning’, and ‘PBL and tutor role’. It was further revised by the PBL expert educationists and piloted on 20 students for validation. The questionnaire was divided into 3 parts. The first part consisted of 7 items, which measured the students’ perception toward the benefits of PBL sessions. The second part consisted of 7 items, which measured the students’ perception toward the PBL conduction and processes (appropriate running of PBL sessions). The third part consisted of 3 items, which measured the students’ perception toward the preparation of the tutors to facilitate the sessions, and their fairness on students’ evaluation. These items were answered on a 5-point’s Likert scale as strongly agree (5), agree (4), neutral (3), disagree (2), and strongly disagree (1). The internal consistency of all 17 items was measured by Cronbach’s alpha reliability test and showed 0.88 (χ2=1783.7, p=0.001). The questions representing the self-directed learning (SDL) resources, duration (hours) were included as yes/no answers.
Data analysis
Data were coded and entered into Microsoft Excel software and analyzed using SPSS® version 19.0 (IBM Corporation, Armonk, NY, USA) statistical software. The average score for each student was calculated on a 5-point’s Likert scale. The 5-point Likert scale responses were combined into 3 different categorical variables ‘agree’ (strongly agree plus agree), ‘neutral’, and ‘disagree’ (strongly disagree plus disagree). Chi-Square test was used to measure the associations between the different categorical variables (agree, neutral, and disagree) among the male and female or first and second year students. One-way analysis of variance (ANOVA) was used to compare the SDL resources and duration among the male and female students. A p<0.05 was considered statistically significant.
Ethical approval
All participants were informed of the objectives of the study, information on the items in the questionnaire was explained, and participant anonymity was assured by assigning each student with a code number for the analysis. The Research Ethical Committee, Department of Medical Education, College of Medicine, KSU, Riyadh, KSA approved the study.
Results
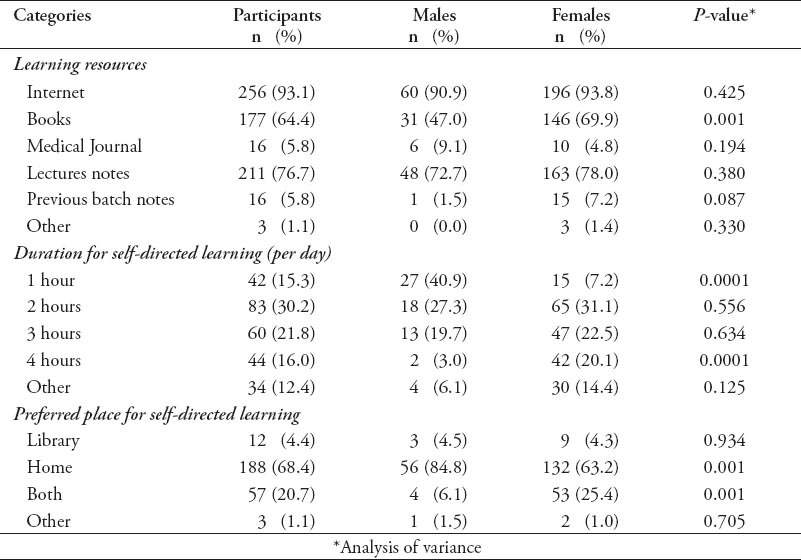
A total of 510 questionnaires were distributed, and 275 (53.9%) of students completed the questionnaire. Of these, 167 (60.7%) were first year students, 108 (39.3%) were second year students, 66 (24%) were male, and 209 (76%) were female students. Table 1 summarizes the students’ perception of the PBL sessions’ benefits, which included 7 items. The students overall responses showed that the students felt that the PBL sessions were beneficial in their learning process in a system-based hybrid curriculum (mean: 3.84 ± 0.90). Most students (84.8% of the males, and 75.6% of the females) reported that the PBL sessions were helpful in understanding basic sciences concepts. Furthermore, most of the students (86.4% of the males, and 71.3% of the females) reported that PBL sessions increased their knowledge of basic sciences. The students reported that the PBL sessions encouraged self-directed and collaborative learning, improved decision making skills, developed problem solving skills, and helped them to identify their strengths and weaknesses during the learning process. Table 2 summarizes that the perception of students regarding PBL sessions conduction and process, which included 7 items. The student’s responses showed that they were satisfied with the PBL session conduction and process, with an overall mean score of 3.76 ± 0.87, a male score of 3.63 ± 0.91, and a female score of 3.63 ± 0.93. First year students scored 3.61 ± 0.93, and second year students scored 3.65 ± 0.91. Only 50.3% of students agreed that the PBL sessions were appropriately run, whereas 22% gave a neutral response, and 27.7% of students disagreed. Most students (78.5%) did not agree with the substitution of lectures by PBL sessions; however, no significant correlation was observed between male and female students (p=0.95). The PBL session as an interactive method of learning was reported by 70.9% of students, comprising 83.3% of the males, and 67% of the females (p=0.03). Most students attended PBL sessions on the scheduled time (97.1%), contributed to group discussions (89.8%), and gave feedback to other students (65.5%). However, 54.5% of students reported a lack of proper student training before starting the PBL sessions. There was no significant difference between the response of first and second year students. Most male and female students (>80%) from the first and second years, agreed that there was a repetition of the PBL topics in lectures and vice versa, with no statistical differences between the groups (Table 2). Table 3 summarizes the student’s perception to the PBL tutors facilitation and their fairness, which included 3 items. The overall mean score of all 3 questions was 3.25±1.04. Only 25.1% of the students agreed that the tutors were well prepared to run the PBL session, including 23.9% of the females, and 28.8% of the males (p=0.52). Only 39.3% of the students felt that they have been evaluated in a fair way by their tutors. However, 55.3% of the students reported that the tutor’s feedback was helpful in improving their performance. Table 4 illustrates that the students’ SDL resources for the preparation of PBL sessions were internet (93.1%), lecture notes (76.7%), and books (64.4%). Medical journals were used only by 5.8% of the students. The time spent for the preparation of PBL sessions ranges from 1-4 hours. Most of the students preferred their homes (68.4%) for the preparation of PBL sessions. The college library was used only by 4.4% of the students. The female students used more books (p=0.001), and spent more time (4 hours) in preparation of PBL sessions in comparison with the male students (p=0.0001).
Table 1.
Student’s perception to problem based learning (PBL) session benefits (n=275).
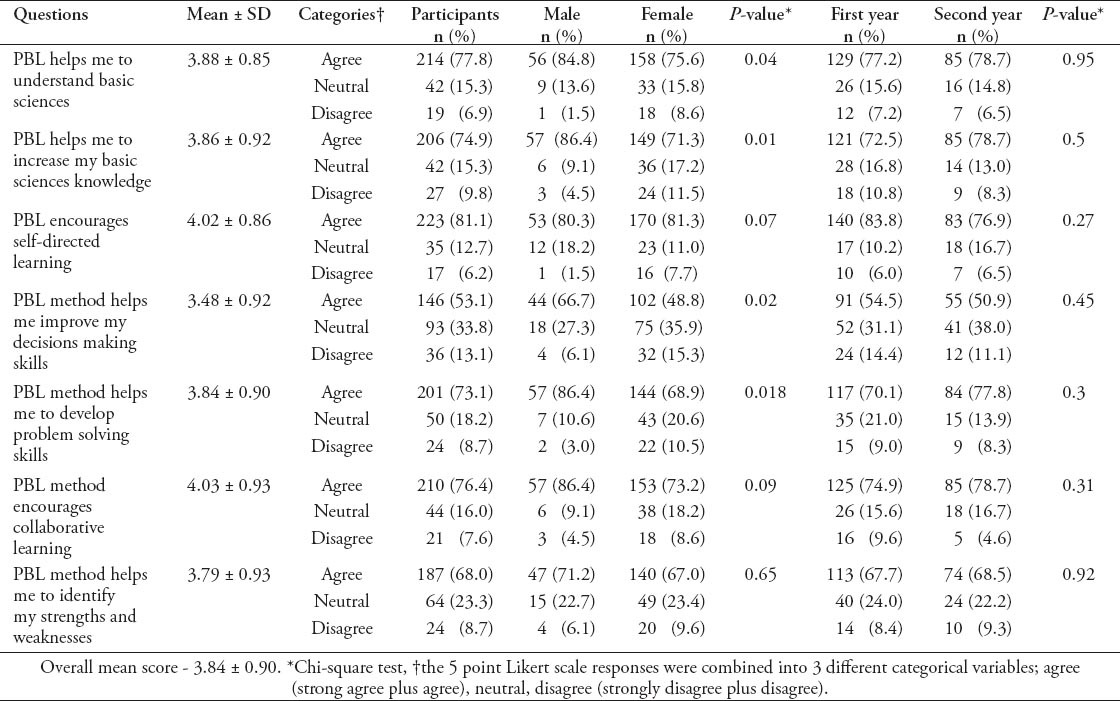
Table 2.
Student’s perception to the appropriately running of problem based learning (PBL) sessions (n=275).
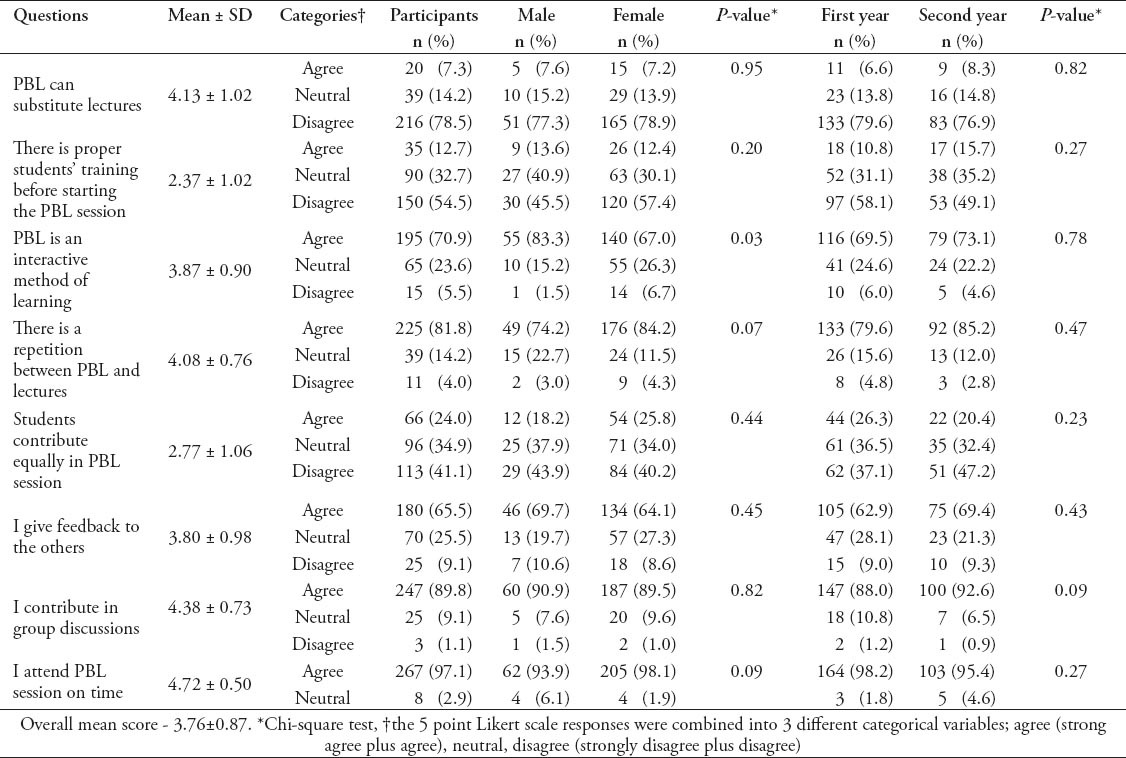
Table 3.
Tutors facilitation of the problem based learning (PBL) sessions and their fairness on students’ evaluation (n=275).
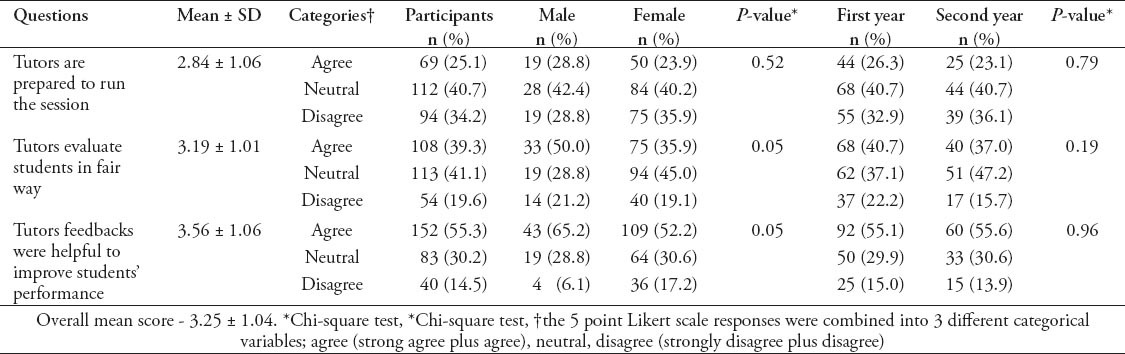
Table 4.
Utilization of self-directed learning resources, duration, and preferred places.
Discussion
Medical education in KSA requires ongoing improvement to keep cadence with the changing demands of the 21st century, especially in medical practice. Many medical colleges worldwide adopted PBL into their curriculum after conducting some research in their own environment.18,19 Local institutions utilizing PBL as an instructional method in a system-based hybrid curriculum need to conduct a series of studies on their educational environment to evaluate the benefits, and to identify areas of improvement.
The present study is based on students’ perceptions of PBL sessions in a system-based hybrid curriculum. The student’s self-assessment and evaluation of their knowledge and its application is a valuable process in learning to identify areas of improvement.20 Our study revealed that PBL sessions are a useful tool that helped students to identify their weakness (area of improvement), and strength as reported by the most of the students, especially male. However, another local study did not find differences between male and female students.14 Our study showed that the students reported a positive role of the PBL sessions in the students’ learning process. A high percentage of our sample reported that the PBL sessions helped them to understand basic sciences concepts, increase their knowledge, and improve problem solving skills. Our study is supported by previous studies that showed that PBL sessions lead to better factual recall, and a substantial increase in students’ knowledge and skills.16,21 In addition, the positive effects of PBL on physician competencies, especially in the cognitive domain have been reported.22 It has been reported that PBL students were better in applying basic sciences knowledge to a clinical case, and demonstrated greater skills in the areas of hypothesis generation, and communication skills.23,24 Contrarily, it has been reported that the PBL does not have an impact on the acquisition of knowledge, and only has a positive impact on its application.13
Students in the current study reported that PBL sessions helped them to develop their decision making skills, and encouraged collaborative learning, even though, most students, especially females reported that there is an exact repetition of the topics between PBL sessions and lectures. Similarly, it has been reported that the PBL sessions help in the development of student skills including decision making and analytical skills,25 inspire students to work as team members, feel confident about tackling unfamiliar problems, and improve expression skills.17,26 It was also found that deep learning can occur when students work together in small groups and when using SDL, where independent thinking is encouraged.27
An important finding in this study is that more than half of the students (most of the were females) reported lack of proper orientation and training before starting the PBL sessions. Lack of proper students’ training may explain their poor contribution during the PBL sessions, and indicates the training provided to our students before starting the PBL sessions as part of the learning skills course was not enough preparation. The PBL literature states that students need proper initial training before running the PBL sessions.28 Even without enough students training, a high percentage of our students recognized PBL as an interactive method of teaching, and contributed to group discussions.
Tutors play an important role in facilitating learning in PBL sessions.29 Student perceptions of tutors’ facilitation skills in the current study showed an average score of 3.25 on a 5 point scale, which is lower than the average score of other international studies.29 The lowest scoring of this item may be attributed to the lack of proper staff training, even though, the college Faculty Development Unit provided PBL tutors training programs for both basic scientists and clinicians. It has been documented in the literature that proper tutor training is an essential step for the success of PBL sessions.10,30,31 Inadequate tutor skills have been reported as a barrier to effective feedback.32 In addition, tutor feedback is an essential element in the process of student’s learning and development.32,33
In the present study, approximately half of students (mostly males) agreed that the tutor feedback was helpful in improving their performance. Moreover, only 39% of students (mostly males) agreed that the tutors fairly evaluated them in the PBL session. Therefore, these findings indicate that further tutor training is required. The tutor training should include introduction to the PBL process, role of students and tutor with emphasis on methods of encouraging the students to contribute during the PBL sessions, giving effective feedback, and objective evaluation. Similarly, Al-Shawwa34 recommended the same tutor training program.34
Students included in this study have similar educational backgrounds (high school graduates). The high school learning environment in KSA is teacher centered, with all information, usually, provided to students, which encourages students to work alone rather than in groups. Our current study results show that students spent more time undertaking SDL time at home, and poorly utilized the college library. In addition, most students reported that internet material, textbooks, and lecturer notes available at home were the main resources used during the SDL to prepare for the PBL sessions. Student training before starting PBL should include information on utilizing the different available resources for seeking information, prioritizing, planning their approach, making decisions, assessing, interpreting, evaluating, comparing, weighing evidence, and using resources.30,35 Successful reform curriculum implementation requires considerable student and staff training before the introduction of a new instructional method of teaching.
Study limitations
This cross-sectional study was based on a convenient sampling method and self-reported information provided by the students. However, small sample size may be exploiting the data to their full potential, with a considerable increase in statistical power. Therefore, other similar studies can be conducted in all the medical college, which introduces the PBL as a method of learning in system-based hybrid curriculum, to approve or disapprove our results.
In conclusion, the study highlighted the significant role of PBL in a system-based hybrid curriculum, which helped the students feel there was an improvement of knowledge and different learning skills. Students reported that the PBL sessions promote and enhance students’ knowledge, enthusiasm, and motivation. They also reported that the sessions contribute to the development of interpersonal, communication, and presentation skills. Student and tutor training is an important component before introducing PBL. However, the non-response rate was high; therefore, result should be interpreted with caution.
Footnotes
Copyright.
Whenever a manuscript contains material (tables, figures, etc.) which is protected by copyright (previously published), it is the obligation of the author to obtain written permission from the holder of the copyright (usually the publisher) to reproduce the material in Saudi Medical Journal. This also applies if the material is the authors own work. Please submit copies of the material from the source in which it was first published.
References
- 1.Rehman R, Afzal K, Kamran A. Interactive lectures: A perspective of students and lecturers. J Postgrad Med Inst. 2013;27:152–156. [Google Scholar]
- 2.Khalid BA. The current status of medical education in the Gulf Cooperation Council countries. Ann Saudi Med. 2008;28:83–88. doi: 10.5144/0256-4947.2008.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Telmesani A, Zaini RG, Ghazi HO. Medical education in Saudi Arabia: a review of recent developments and future challenges. East Mediterr Health J. 2011;17:703–707. [PubMed] [Google Scholar]
- 4.Lee YM, Mann KV, Frank BW. What drives students’ self-directed learning in a hybrid PBL curriculum. Adv Health Sci Educ Theory Pract. 2010;15:425–437. doi: 10.1007/s10459-009-9210-2. [DOI] [PubMed] [Google Scholar]
- 5.Telang A. Problem-based learning in health professions education: an overview. Arch Med Health Sci. 2014;2:243–246. [Google Scholar]
- 6.Masek A, Yamin S. Problem Based Learning model: a collection from the literature. Asian Soc Sci. 2010;6:148–156. [Google Scholar]
- 7.Azer SA. What makes a great lecture? Use of lectures in a hybrid PBL curriculum. Kaohsiung J Med Sci. 2009;25:109–115. doi: 10.1016/S1607-551X(09)70049-X. [DOI] [PubMed] [Google Scholar]
- 8.Rakhudu MA, Amaize A, Useh U, Maselesele M. Inter and intra professional collaboration in the implementation of problem based learning in nursing education: lesson for South Africa. Life Sci J. 2012;9:344–353. [Google Scholar]
- 9.Azer SA, Peterson R, Guerrero AP, Edgren G. Twelve tips for constructing problem-based learning cases. Med Teach. 2012;34:361–367. doi: 10.3109/0142159X.2011.613500. [DOI] [PubMed] [Google Scholar]
- 10.Chan EA. Reflecting on the essence of our problem-based learning discussions: the importance of faculty development and our continuous quest for applications of problem based learning. Kaohsiung J Med Sci. 2009;25:276–281. doi: 10.1016/S1607-551X(09)70074-9. [DOI] [PubMed] [Google Scholar]
- 11.Yew EH, Schmidt HG. Evidence for constructive, self-regulatory, and collaborative process in problem-based learning. Adv Health Sci Educ Theory Pract. 2009;14:251–273. doi: 10.1007/s10459-008-9105-7. [DOI] [PubMed] [Google Scholar]
- 12.Emerald NM, Aung PP, Han TZ, Yee KT, Myint MH, Soe TT, et al. Students’ perception of problem based learning conducted in phase1 medical program, UCSI University, Malaysia. South East Asian Journal of Medical Education. 2013;7:45–48. [Google Scholar]
- 13.Hartling L, Spooner C, Tjosvold L, Oswald A. Problem-based learning in pre-clinical medical education: 22 years of outcome research. Med Teach. 2010;32:28–35. doi: 10.3109/01421590903200789. [DOI] [PubMed] [Google Scholar]
- 14.AlHaqwi AI. Learning outcomes and tutoring in problem based-learning: how do undergraduate medical students perceive them? Int J Health Sci (Qassim) 2014;8:125–132. doi: 10.12816/0006078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Husain A. Problem-based learning: A current model of education. Oman Med J. 2011;26:295. doi: 10.5001/omj.2011.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Azer SA, Hasanato R, Al-Nassar S, Somily A, AlSaadi MM. Introducing integrated laboratory classes in a PBL curriculum: impact on student's learning and satisfaction. BMC Med Educ. 2013;13:1–12. doi: 10.1186/1472-6920-13-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shamsan B, Sayed AT. Evaluation of problem based learning course at college of medicine, qassim university, Saudi Arabia. Int J Health Sci (Qassim) 2009;3:249–258. [PMC free article] [PubMed] [Google Scholar]
- 18.Schmidt HG, Cohen-Schotanus J, Arends LR. Impact of problem-based, active learning on graduation rates for 10 generations of Dutch medical students. Med Educ. 2009;43:211–218. doi: 10.1111/j.1365-2923.2008.03287.x. [DOI] [PubMed] [Google Scholar]
- 19.Usmani A, Sultan ST, Ali S, Fatima N, Babar S. Comparison of students and facilitators’ perception of implementing problem based learning. J Pak Med Assoc. 2011;61:332–335. [PubMed] [Google Scholar]
- 20.Abdulghani HM, Shaik SA, Khamis N, Al-Drees AA, Irshad M, Khalil MS, et al. Research methodology workshops evaluation using the Kirkpatrick's model: translating theory into practice. Med Teach. 2014;36(Suppl 1):S24–S29. doi: 10.3109/0142159X.2014.886012. [DOI] [PubMed] [Google Scholar]
- 21.Abou-Elhamd KA, Rashad UM, Al-Sultan AI. Applying problem-based learning to otolaryngology teaching. J Laryngol Otol. 2011;125:117–120. doi: 10.1017/S0022215110001702. [DOI] [PubMed] [Google Scholar]
- 22.Koh GC, Khoo HE, Wong ML, Koh D. The effects of problem-based learning during medical school on physician competency: a systematic review. CMAJ. 2008;178:34–41. doi: 10.1503/cmaj.070565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Callis AN, McCann AL, Schneiderman ED, Babler WJ, Lacy ES, Hale DS. Application of basic science to clinical problems: traditional vs. hybrid problem-based learning. J Dent Educ. 2010;74:1113–1124. [PubMed] [Google Scholar]
- 24.Nanda B, Manjunatha S. Indian medical students’ perspectives on problem-based learning experiences in the undergraduate curriculum: one size does not fit all. J Educ Eval Health Prof. 2013;10:1–11. doi: 10.3352/jeehp.2013.10.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Downing K, Ning F, Shin K. Impact of problem-based learning on student experience and metacognitive development. Multicult Educ Technol J. 2011;5:55–69. [Google Scholar]
- 26.Albarrak AI, Mohammed R, Abalhassan MF, Almutairi NK. Academic satisfaction among traditional and problem based learning medical students. A comparative study. Saudi Med J. 2013;34:1179–1188. [PubMed] [Google Scholar]
- 27.Abdulghani HM, Al-Drees AA, Khalil MS, Ahmad F, Ponnamperuma GG, Amin Z. What factors determine academic achievement in high achieving undergraduate medical students? A qualitative study. Med Teach. 2014;36(Suppl 1):S43–S48. doi: 10.3109/0142159X.2014.886011. [DOI] [PubMed] [Google Scholar]
- 28.Dent JA, Harden RM. A practical guide for medical teachers. 3rd ed. Edinburgh (UK): Churchill Livingstone; 2009. [Google Scholar]
- 29.Chung EK, Hitchcock MA, Oh SA, Han ER, Woo YJ. The relationship between student perceptions of tutor performance and tutors’ background in problem-based learning in South Korea. Int J Med Educ. 2011;2:7–11. [Google Scholar]
- 30.Dalrymple KR, Wuenschell C, Rosenblum A, Paine M, Crowe D, von Bergmann HC, et al. PBL core skills faculty development workshop 1: an experiential exercise with the PBL process. J Dent Educ. 2007;71:249–259. [PubMed] [Google Scholar]
- 31.Aarnio M, Lindblom-Ylanne S, Nieminen J, Pyorala E. How do tutors intervene when conflicts on knowledge arise in tutorial groups? Adv in Health Sci Educ. 2014;19:329–345. doi: 10.1007/s10459-013-9473-5. [DOI] [PubMed] [Google Scholar]
- 32.Al-Haqwi AI, Al-Wahbi AM, Abdulghani HM, Van der Molen HT. Barriers to feedback in undergraduate medical education. Male students’ perspective in central Saudi Arabia. Saudi Med J. 2012;33:557–561. [PubMed] [Google Scholar]
- 33.AlHaqwi AI. Importance and process of feedback in undergraduate medical education in Saudi Arabia. Saudi J Kidney Dis Transpl. 2012;23:1051–1055. doi: 10.4103/1319-2442.100949. [DOI] [PubMed] [Google Scholar]
- 34.Al-Shawwa LA. Preparing faculty members as PBL tutors in King Abdul Aziz University, Jeddah Saudi Arabia. Med J Cairo Univ. 2011;79:185–191. [Google Scholar]
- 35.El-Aziz El Naggar MAA, Maklady FAH, Hamam AM, Omar AS. Effectiveness of implementing a tutor training workshop for problem based learning class tutors at the Faculty of Medicine, Suez Canal University. Intel Prop Rights. 2013;1:104. [Google Scholar]


