Abstract
The purpose of this study was to describe health promotion behaviors and work productivity loss in informal caregivers of individuals with advanced stage cancer. Using a cross-sectional, correlational design, 70 caregivers completed measures of health behaviors, mood, social support, and burden. Absenteeism and presenteeism were evaluated in employed caregivers (n = 40). Caregivers reported low levels of physical activity. The mean percentage of work productivity loss due to caregiving was 22.9%. Greater work productivity loss was associated with greater number of caregiving hours, higher cancer stage, married status, and greater anxiety, depression, and burden related to financial problems, disrupted schedule, and health. Nurses should assess caregivers and provide health promotion interventions, which may ultimately reduce the economic impact of caregiving.
Keywords: caregivers, cancer, health promotion behaviors, employment, work productivity
An estimated 48.9 million informal or family caregivers in the United States are assisting adult family members or friends with personal care or instrumental activities of living (National Alliance for Caregiving [NAC] & AARP, 2009). These caregivers provide an essential service to individuals, health-care professionals, and society, with an estimated economic value of $375 billion (AARP, 2008). Informal caregivers, often described as a national resource (Schulz & Sherwood, 2008), are also a vulnerable population as they are exposed to the stresses and strains of the caregiving role. Caregivers of individuals with cancer, who comprise approximately 7% of adult caregivers (NAC & AARP, 2009), often report high levels of burden and distress that are comparable to those experienced by caregivers of persons with dementia (Kim & Schulz, 2008) and AIDS (Stetz & Brown, 2004). The trajectory of the cancer experience, from the acute phase of treatment to survivorship or end of life, presents numerous significant and unique challenges that may negatively affect the quality of life of informal caregivers (Kim & Given, 2008; Kitrungrote & Cohen, 2006). Unlike caregiving associated with dementia or other chronic illnesses, cancer caregiving has been characterized as having an abrupt onset and a variable trajectory with greatest intensity during the treatment and end-of-life phases (Kim & Schulz, 2008).
Several evolving trends will require health-care professionals and policy makers to give greater attention to the individual and societal costs of informal caregiving within the context of cancer. With an aging population, it is anticipated that the prevalence of cancer will increase, leading to greater reliance on informal caregivers to assist individuals throughout the course of cancer treatment (Edwards et al., 2002). Additionally, medical advances in cancer treatment have led to a growing number of cancer survivors, including those living with advanced cancer, who will require some degree of caregiving to assist in coping with persistent treatment side effects, late effects of cancer treatment, psychosocial needs, and cancer recurrence (Haylock, 2010). With rising health-care costs, cancer patients will continue to be given intensive treatments in outpatient settings, with informal caregivers playing a critical role in the management of the patient. Informal cancer caregivers are an extension of the health-care team, yet report feeling inadequately trained for the clinical care tasks that they provide in addition to assistance with activities of daily living (van Ryn et al., 2011). Given these trends, it is essential for health-care professionals and policy makers to develop a more comprehensive understanding of the personal toll of informal caregiving and its potential downstream impact on society as a whole. In the current study we examined two costs of cancer caregiving that are often overlooked: the impact of caregiving on the health promotion and work behaviors of the caregiver.
There is a substantial body of literature describing the personal toll of cancer caregiving on the psychological health of the informal caregiver, often manifested as depression, burden, and anxiety (Stenberg, Ruland, & Miaskowski, 2010). Although cancer caregiver physical health problems such as fatigue, sleep disruption, pain, and loss of appetite have been described (Carter, 2002; Stenberg et al., 2010), the impact of cancer caregiving on caregivers’ health promotion behaviors has been explored to a much lesser degree. The range of health promotion behaviors is broad and includes activities such as exercising regularly, eating a nutritious diet, avoiding tobacco products, keeping wellness visits with health professionals, and engaging in health screenings. The assumption that caregivers do not practice health promotion behaviors due to stress or time constraints has been challenged, with conflicting reports in the general caregiver literature. In studies matching non-caregivers with caregivers of elders (Scharlach, Midanik, Runkle, & Soghikian, 1997) or spousal caregivers (Burton, Newsom, Schulz, Hirsch, & German, 1997), no significant differences were found in health promotion behaviors related to smoking, alcohol intake, or nutrition. However, the subgroup of caregivers who provided greater levels of assistance with activities of daily living were significantly less likely to exercise and get enough rest (Burton et al., 1997; Scharlach et al., 1997). In a more recent study of employees providing care to elderly relatives, caregivers were more likely than non-caregivers to smoke, to use alcohol, defer health screenings, and report having depression, diabetes, hypertension, or pulmonary disease (MetLife Mature Market Institute [MMI], National Alliance for Caregiving, & University of Pittsburgh Institute on Aging, 2010). In one of the few studies specific to cancer, Beesley, Price, Webb, Australian Ovarian Cancer Study Group, Australian Ovarian Cancer Study—Quality of Life Study Investigators (2010) found that 56% of 101 long-term caregivers of women with ovarian cancer reported having at least one negative change in their health behaviors since becoming a caregiver, with physical inactivity and weight gain most common.
Despite the conflicting results in the literature, caregivers who practice negative health behaviors, either habitually or as a result of assuming the caregiver role, are likely to be vulnerable to chronic illnesses such as diabetes or hypertension. The potential downstream societal costs are significant, as the negative physical health effects of caregiving may have a delayed onset of 2 years and may persist for 4 years in subgroups of caregivers (Coe & van Houtven, 2009). In one study, investigators estimated that health-care costs for caregivers would be 8% higher than non-caregivers, with a potential cost to employers of $13.4 billion per year (MMI et al., 2010). Identification of risk factors for negative health promotion behaviors in caregivers, such as high subjective burden (Sisk, 2000), low socioeconomic status (Scharlach et al., 1997), employment (Scharlach et al., 1997), and caring for a spouse with ADL impairment (Burton et al., 1997), may assist health professionals in providing targeted interventions to offset the onset of chronic illnesses.
Employed cancer caregivers are particularly vulnerable to the negative effects of stress as they attempt to juggle often competing demands of multiple roles, including work and caregiving (Gaugler et al., 2008; Kim, Baker, Spiller, & Wellisch, 2006). Higher levels of depressive symptoms were found in employed cancer caregivers (B. Given et al., 2004). Yet, working may also provide positive benefits to caregivers including respite from the strain of caregiving, social support, and economic security (Gysels & Higginson, 2009; Kim et al., 2006; Swanberg, 2006). For cancer caregivers, the sudden onset, uncertainty, and ambiguity of the cancer caregiving trajectory can lead to missed time from work, work interruptions and distractions, decreased productivity, and job resignation (Swanberg, 2006). All of these factors contribute to the economic burden of caregiving and have both personal and social implications.
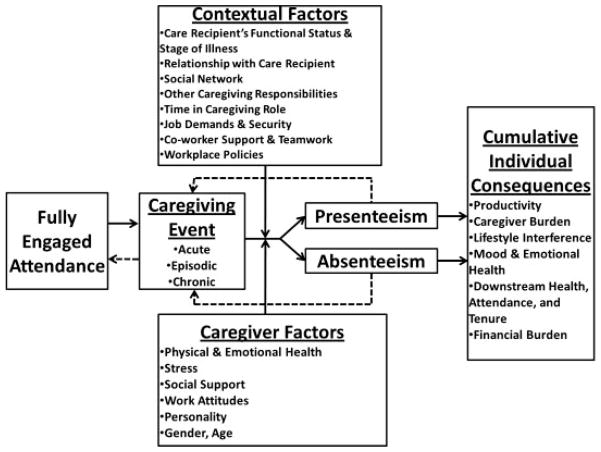
A comprehensive account of the economic impact of caregiving on work must measure both absenteeism (time away from work) and presenteeism, which refers to reduced productivity even though present at work, due to distractions of an illness or event (Giovannetti, Wolff, Frick, & Boult, 2009; Johns, 2010). Overall productivity loss is described by Johns (2010, p. 530) as an “iceberg effect,” with the visible portion of the iceberg representing absenteeism and the extensive area underneath the water as presenteeism, which is difficult to objectively measure. The relationships among fully engaged attendance, absenteeism, and presenteeism is dynamic and complex, with both contextual and individual factors influencing the relationship between the triggering event and the occurrence of presenteeism or absenteeism (Johns, 2010).
John’s (2010) dynamic model of presenteeism and absenteeism can be applied to a caregiving event (Fig. 1). Influenced by a myriad of contextual and personal factors, caregivers may cycle between episodes of absenteeism or presenteeism and ultimately experience cumulative individual consequences related to work productivity, perceived caregiver burden, lifestyle interference, and emotional health. It is important to acknowledge that presenteeism is not necessarily a loss from an employer’s perspective who may view the situation as a gain, as work productivity from a distracted present employee is still greater than that from one who is absent (Johns). Likewise, presenteeism is not necessarily a negative event for the caregiver who may gain positive benefits from working. However, with continued episodes of absenteeism or presenteeism, the caregiver may eventually experience negative effects related to emotional health (depression, low self-esteem) and employment (loss of tenure, missed promotions, loss in income, early retirement, and resignation). John’s model was not tested in the current study; it is presented solely as a framework for understanding possible relationships among these complex concepts. Due to the lack of empirical evidence for many of the relationships in the model, we undertook a preliminary step to model testing by exploring and describing possible relationships among variables in a sample of caregivers.
FIGURE 1.
Modification of John’s Dynamic Model of Presenteeism and Absenteeism for caregiving. Adapted with permission from “Presenteeism in the Workplace: A Review and Research Agenda,” by G. Johns (2010), Journal of Organizational Behavior, 31, p. 532. Copyright 2010 by John Wiley and Sons.
Greater absenteeism among cancer caregivers has been associated with having a care recipient in the terminal phase of illness (Grunfeld et al., 2004) or with increased instrumental activities of daily living (IADL) needs (Sherwood et al., 2008). Although reduced productivity has been described as an issue for caregivers (Gysels & Higginson, 2009), the extent of presenteeism in employed caregivers has not been well documented. In the only study found, Giovannetti et al. (2009) examined absenteeism, presenteeism, and overall productivity loss in a sample of 125 employed caregivers who were assisting older individuals with complex medical conditions. In that study, caregivers were absent for 4.9% of their work time and were only 81.5% productive while at work, which led to an overall loss of 20.1% in work productivity. Greater loss in work productivity was significantly associated with caregiver strain (r = .45, p < .001) and depression (r = .30, p < .001; Giovannetti et al., 2009).
In response to a need to expand our understanding of the personal toll of informal cancer caregiving, the purpose of the current study was to (a) describe the health promotion behaviors, work productivity loss, and daily activity impairment of caregivers with advanced cancer; (b) examine correlates of work productivity loss; and (c) pilot test the use of the Work Productivity and Activity Impairment (Reilly, Zbrozek, & Dukes, 1993) questionnaire in a sample of caregivers. Based on prior research, we hypothesized that greater work productivity loss would be significantly associated with greater perceived caregiver burden, greater depression, greater anxiety, and lower perceived social support. The research questions were:
What are the health promotion behaviors of informal caregivers of individuals with advanced cancer?
Are there differences in absenteeism, presenteeism, and overall work productivity loss by caregiver demographic variables and characteristics of the caregiving situation?
What is the relationship between work productivity loss and caregiver burden, depression, anxiety, and social support in caregivers of individuals with advanced cancer?
Methods
Participants
The sample for this analysis was drawn from informal caregivers who were currently active in a palliative care clinical trial Improving the Quality of Advanced Cancer Care with Disease Management at a Midwestern National Cancer Institute-designated Comprehensive Cancer Center (R01NR10787). In that study, 610 adult patients with stages II to IV pancreatic cancer or stages III or IV lung, gastrointestinal, or gynecologic cancer were enrolled during their initial visit to the cancer center along with the family member or friend whom the patient identified as a caregiver (n = 297). Caregiver was defined as an individual providing unpaid assistance with instrumental activities or activities of daily living. The patient and caregiver were followed for 15 months with data collected at enrollment and at 3, 9, and 15 months. Exclusion criteria for the palliative care trial were inability to provide informed consent, non-English speaking, pursuing treatment elsewhere, or going to hospice.
Design and Procedures
A descriptive, correlational design using a cross-sectional approach was used to answer the research questions. Following IRB approval for the present study, a convenience sample of caregivers who were currently active in the palliative care trial received a one-time mailing of two additional surveys that measured work productivity and health behaviors. These were mailed with the standard surveys used in the palliative care trial at the caregivers’ 3, 9, or 15-month data collection time point from December 2009 to December 2010. If the surveys were not returned after a reminder phone call from the research assistant, they were included in the next routine mailing for the palliative care trial. For example, if a caregiver did not return the surveys at the 3-month data collection period, he or she received them at the 9-month time point.
Measures
Caregiver health promotion behaviors
An investigator-constructed survey consisting of 11 questions with categorical response choices explored caregivers’ current health promotion behaviors related to physical activity, diet, and cigarette use; co-morbid conditions; last well-care checkup; and number of days without adequate rest in the past month. They were also asked whether their caregiver responsibilities interfered with each health promotion behavior and their ability to seek care for a medical problem or undergo screening tests. These items were designed to provide a general description of caregiver health promotion behaviors and to minimize response burden. For example, the single item that addressed physical activity was: “Recently, how many days per week (on average) did you do 30 minutes of moderate activity (walking briskly, yard work, jogging, gardening, swimming, biking, golf, etc.)?” Response categories were: never, 1 day per week, 2–3 days per week, and >3 times per week. This item was followed by the question, “Overall, how much do your caregiver responsibilities limit your ability to get enough exercise?” Potential responses were: not at all, a little bit, quite a bit, and extremely.
Caregiver burden
Caregiver burden was conceptualized as the informal caregiver’s subjective response of imbalance between the perceived multidimensional demands of caregiving and his/her resources to meet the demands (Chou, 2000). Caregiver burden was assessed using the Caregiver Reaction Assessment (CRA), which is a 24-item survey assessing both positive and negative reactions to caregiving (C. W. Given et al., 1992). Four subscales assess the dimensions of burden: lack of family support, financial problems, disrupted schedule, and health problems. One subscale measures the caregiver’s self-esteem as a positive dimension of caregiving. Caregivers indicate their level of agreement to each statement using a 5-point Likert-type scale ranging from strongly disagree to strongly agree. The average score for each subscale is reported; there is no total score. The range of scores is 1–5, with higher scores representing greater impact of caregiving on the negative or positive dimension being measured. Reliability and construct validity of the CRA have been supported in caregivers of individuals with cancer, with Cronbach’s alphas ranging from .62 to .83 (Nijboer, Triemstra, Tempelaar, Sanderman, & van den Bos, 1999). Cronbach’s alphas for the subscales in the present study were: lack of family support .85, financial problems .85, disrupted schedule .85, health problems .66, and caregiver esteem .75.
Mood state
Caregivers’ mood states were assessed using two subscales of the 30-item short-form of the Profile of Mood States (POMS): tension/anxiety and depression/dejection (McNair, Lorr, & Droppleman, 1992). Each subscale consists of adjectives that reflect an affective mood state. Subjects rate on a 5-point scale from 0 (not at all) to 4 (extremely) if they experienced a particular mood or feeling during the past several days. Items are summed to produce a subscale score with a range from 0 to 20. Higher scores indicate more mood disturbance. Psychometric properties of the POMS have been established with Cronbach’s alphas ranging from .81 to .99, (McNair et al., 1992) and it has been used in cancer caregiver studies (Cameron, Franche, Cheung, & Stewart, 2002; Schumacher et al., 2008). For the current study, Cronbach’s alpha was .87 for the tension/anxiety subscale and .87 for the depression/dejection subscale.
Social support
Caregivers’ perceived social support was assessed using the 19 item, self-report Medical Outcomes Social Support Survey (MOS-SSS), which consists of four support subscales: emotional/informational, tangible, affectionate, and positive social interaction (Sherbourne & Stewart, 1991). Subjects rate how often each type of support is available to them using a 5-point Likert scale, ranging from 1 (none of the time) to 5 (all of the time). An overall support index is calculated by averaging the 19 items. A higher score indicates more support. Reliability and validity of the MOS-SSS subscales were established in a large sample of adult patients with chronic illnesses, with Cronbach’s alphas ranging from .91 to .97 (Sherbourne & Stewart, 1991). The Cronbach’s alpha for the total scale was .97 in this study.
Work productivity loss
The impact of caregiving on absenteeism, presenteeism, and non-work activity impairment was measured using the Work Productivity and Activity Impairment Questionnaire (WPAI; Reilly, Zbrozek, & Dukes, 1993). This 6-item questionnaire, which is either interviewer or self-administered, can be adapted to reflect the impact of a specific disease, health problem, or caregiving situation on work productivity and activity impairment. For this study, questions on a disease-specific caregiver version of the WPAI (WPAI-Crohn’s Disease-Caregiver V2.0) were modified to assess the impact of caring for an individual with cancer. The first question establishes whether the caregiver is currently employed. Using a 1-week recall period, employed caregivers then answer questions to determine the hours missed from work due to caregiving or other reasons, hours actually worked, and the extent to which caregiving affected his/her productivity while working. A single item measure of activity impairment is administered to all caregivers, regardless of employment status. Scores for the WPAI are reported as percentages for (a) absenteeism or work time missed due to caregiving, (b) presenteeism or reduced productivity while at work due to caregiving, (c) overall work impairment due to caregiving, and (d) activity impairment or reduced productivity for regular, daily, non-work activities due to caregiving. Detailed scoring information can be found at http://www.reillyassociates.net/WPAI_Scoring.html. Construct validity of the WPAI was supported in a sample of informal caregivers of older, chronically ill individuals (Giovannetti et al., 2009). Although test–retest reliability of the WPAI caregiver version has not been established, the disease-specific versions of the WPAI do demonstrate adequate reliability (Prasad, Wahlqvist, Shikiar, & Shih, 2004).
Other measures
Demographic data for the care recipient and caregiver were obtained on enrollment into the palliative care trial. Data regarding age, race/ethnicity, gender, marital status, education, employment, and annual household income were used to describe the sample. Medical information included type of cancer, history of prior cancers, stage, and functional status, as measured by the Eastern Cooperative Oncology Group (ECOG) performance status scale (Oken et al., 1982). The ECOG performance status is graded on a 5-point scale, from 0 (fully active, able to carry on all pre-disease performance without restriction) to 5 (dead).
Caregivers were also asked to rate their current physical health status using a 5-point Likert-type scale ranging from poor to excellent. A single item assessment of self-rated health reflects a global perception of one’s health and has been found to be a reliable predictor of mortality (Idler & Benyamini, 1997).
Data Analysis
Data were analyzed using IBM SPSS Statistics version 19. Tests of significance were one-tailed, with alpha set at .05, for examination of the relationship between work productivity loss and caregiver burden, depression, anxiety, and social support. All other tests of significance were two-tailed, with alpha set at .05. Descriptive statistics were used to describe sample demographics, medical characteristics of the care recipient, the caregiving context, and caregiver health promotion behaviors. Independent sample t-tests, analysis of variance, chi-square tests, Kruskal–Wallis test, and Mann–Whitney U-tests were used for univariate analyses. Due to the ordinal scales of the WPAI, non-parametric tests were used: (a) bivariate correlations were assessed using Spearman’s correlation coefficient and (b) group differences in WPAI scores were evaluated using the Mann–Whitney test.
Results
Sample Characteristics
Seventy of 91 caregivers returned surveys for a 77% response rate. Data from 69 care recipients were obtained as one caregiver participated in the palliative care clinical trial without the care recipient enrolling. The 21 caregivers who did not return their surveys were not significantly different from those who participated for the variables of age, gender, race, or cancer stage of the care recipient. Reasons for caregiver refusal were: 2 (9.5%) lost to follow-up or care was moved to another hospital, 6 (28.6%) worsening condition of care recipient, 6 (28.6%) dropped out of palliative care clinical trial, and 7 (33.3%) did not return any surveys for that time point in the palliative care clinical trial.
The mean age was 57.01 for caregivers and 62.19 for care-recipients. The typical caregiver was female, White, married, and had a household income of greater than $50,000. Forty-four (62.9%) caregivers were spouses; there were 11 daughters (15.7%), 1 son (1.4%), 3 friends (4.3%), 2 partners (2.9%), 3 siblings (4.3%), and 6 others (8.6%). Forty-seven caregivers (67.1%) resided in the same household as the care recipient, and 32 (46.4%) reported providing less than 9 hours of caregiving per week. Twenty-eight (40%) caregivers provided care to other persons in addition to the care recipient. The typical care recipient was female, White, married, and had a high functional status. The mean time since diagnosis was 19 months (SD = 26.93), and 50 (80.6%) care recipients were currently receiving treatment for their cancer. Descriptive statistics can be found in Table 1. As shown in Table 2, caregivers had, on average, low scores for anxiety/tension and depression/dejection, and high scores for social support. Their scores measuring burden were mid-range with the greatest area of burden being disrupted schedule.
Table 1.
Sample Characteristics
| Characteristic | Caregiver, n (%) | Care Recipient, n (%) |
|---|---|---|
| Gender: female | 49 (70.0) | 42 (60.9) |
| Race/ethnicity | ||
| Caucasian | 58 (82.9) | 58 (84.1) |
| African American | 11 (15.7) | 10 (14.5) |
| Asian | 1 (1.4) | 1 (1.4) |
| Marital status: married | 53 (75.7) | 47 (68.1) |
| Employment status: employed | 40 (57.1) | 24 (34.8) |
| Annual household income | ||
| $20,000 or less | 4 (6.3) | 9 (14.1) |
| $21,000–$49,999 | 16 (25.0) | 24 (37.5) |
| $50,000 or greater | 44 (68.8) | 31 (48.4) |
| Education | ||
| High school or less | 39 (55.7) | 42 (61.8) |
| College or more | 31 (44.3) | 26 (38.2) |
| Type of cancer | ||
| Colorectal | 10 (14.5) | |
| Gastrointestinal | 4 (5.8) | |
| Gynecologic | 19 (27.5) | |
| Lung | 22 (31.9) | |
| Pancreas | 11 (15.9) | |
| Other | 3 (4.3) | |
| Cancer stage | ||
| II | 2 (2.9) | |
| III | 30 (43.5) | |
| IV | 37 (53.6) | |
| ECOG performance status | ||
| 0 | 23 (36.5) | |
| 1 | 31 (49.2) | |
| 2 | 7 (11.1) | |
| 3 | 2 (3.2) | |
Note: N = 70 caregivers and 69 care recipients.
Table 2.
Mean Scores for Independent Variables (N = 70)
| Variable | M (SD) | Mdn | Possible Range |
|---|---|---|---|
| POMS anxiety/tension | 5.00 (4.12) | 4.00 | 0–20 |
| POMS depression/dejection | 4.38 (3.92) | 3.00 | 0–20 |
| CRA lack of family support | 1.98 (.90) | 1.80 | 1–5 |
| CRA financial problems | 2.23 (1.01) | 2.00 | 1–5 |
| CRA disrupted schedule | 2.96 (1.04) | 3.00 | 1–5 |
| CRA health problems | 2.12 (.82) | 2.00 | 1–5 |
| CRA self-esteem | 4.36 (.51) | 4.43 | 1–5 |
| MOS-SSS social support | 3.80 (.95) | 3.89 | 1–5 |
Note: POMS, Profile of Mood States; CRA, Caregiver Reaction Assessment; MOS-SSS, Medical Outcomes Social Support Survey.
Although 40 (57%) caregivers were employed, the final sample used in the work productivity analysis was 39 due to missing data on the WPAI. When comparing employed caregivers to unemployed caregivers, statistically significant differences were found for age, t(64) = −3.13, p < .01; relationship to care recipient, χ2 (1, N = 69) = 7.81, p < .01; residence, χ2 (1, N = 69) = 7.54, p < .01; and hours of caregiving, z = −3.27, p = .001. Employed caregivers were more likely to be younger, in a non-spousal relationship with the care recipient, not residing with the care recipient, and reporting fewer hours of caregiving per week. There were no statistically significant differences found between employed and unemployed caregivers in scores for depression, anxiety/tension, social support, and all of the burden scales.
Last, 34 (48.6%) caregivers completed surveys for the present study at the 3-month data collection time point in the palliative care clinical trial. Eighteen (25.7%) caregivers were at the 9-month time point and 18 (25.7%) were at the 15-month time point. The groups responding at different time points did not differ on demographic (age, gender, employment status, education, and income) or caregiving characteristics (relationship to care recipient and residence), or on depression, anxiety, social support, and burden. Sixty-one caregivers (87%) were in the intervention phase of the palliative care clinical trial. The only statistically significant difference found between caregivers in the control and intervention groups was for age, t(65) = −2.69, p < .01. Caregivers in the control group were more likely to be younger.
Caregiver Health Behaviors
Fifty-three (75.7%) caregivers rated their health as good or excellent. Of the 54 caregivers who responded to the question about their medical condition, 47 (87.0%) reported having at least one medical condition, most commonly hypertension and arthritis. Fifty (71.4%) caregivers reported having had a well-care check-up within the past year. Caregiving responsibilities prevented 14 (20.0%) caregivers from seeing a doctor when they needed to and delayed 15 (21.4%) in getting a medical test or screening. The mean number of days during the past month on which caregivers did not get enough rest was 7.85 (SD = 9.61, Mdn = 4.00).
Caregivers rated their frequency of performing 30 minutes of moderate activity per week as: never (n = 16, 22.9%), 1 day per week (n = 7, 10.0%), 2–3 days per week (n = 22, 31.4%), and more than three times per week (n = 25, 35.7%). Forty-two (60%) caregivers indicated that their caregiving responsibilities did not limit his/her ability to get enough exercise. Physical activity had a significant, direct relationship with caregiver gender, rs = .46, p < .001 and caregiver self-rating of health, rs = .25, p < .05; and a significant, indirect relationship with the caregiver burden scales of lack of family support, rs = −.28, p < .05, and health problems, rs = −.23, p = .05. More frequent physical activity was associated with male gender, better health ratings, and low perceptions of burden related to family support and health problems. Physical activity was not significantly associated with any other caregiver demographic variables, depression, anxiety, caregiving hours, ECOG performance status of the care recipient, or cancer stage.
Sixty-two (88.6%) caregivers reported usually eating a healthy diet; 42 (60%) felt that their caregiving responsibilities did not interfere with his/her eating a healthy diet. Six (8.6%) caregivers reported currently smoking cigarettes; of these, four were employed caregivers. Employed caregivers did not differ significantly from unemployed caregivers on self-rating of health and all of the health promotion behaviors (well-care check-up, physical activity, nutrition, rest/sleep).
Work Productivity Loss
The 39 employed caregivers reported a 9.63% (SD = 23.73, Mdn = 0) loss in work time (absenteeism). Although 28 (74.4%) caregivers had not missed work in the past 7 days, 11 (28%) reported missing a mean of 17 hours in the last week, which translated into a mean 34.14% loss in work time for that subset of employed caregivers. There was 15.41% (SD = 19.38, Mdn = 10) impairment while working due to caregiving (presenteeism), indicating that caregivers were approximately 85% productive while working. Considering both absenteeism and presenteeism, the mean percentage of overall work productivity loss due to caregiving was 22.88% (SD = 28.47, Mdn = 10).
The WPAI also measures impairment in activities of daily living that are not work-related. In this study, the mean percentage of activity impairment due to caregiving for both employed and unemployed caregivers was 20.74% (SD = 25.00, Mdn = 10). Percent absenteeism, presenteeism, overall work productivity loss, and activity impairment did not differ based on caregiver gender, household income, residence, relationship to care recipient, or whether the caregiver provided care to other individuals than the care recipient.
Overall work productivity loss was not significantly correlated with caregiver age, gender, race, education, household income, relationship with care recipient, residence, provision of care to other individuals, health self-rating, time since diagnosis, receiving treatment, ECOG performance status, or any demographic characteristic of the care recipient. It was also not significantly associated with group assignment or data collection point in the palliative care clinical trial. Work productivity loss did have a significant, direct relationship with reported hours of caregiving (rs = .34, p < .05, one-tailed) and cancer stage (rs = .30, p < .05, one-tailed), with greater number of hours of caregiving and higher cancer stage associated with greater productivity loss. Work productivity loss had a significant, indirect relationship with caregiver’s marital status (rs = −.44, p < .01, one-tailed), with married status associated with greater productivity loss. Our hypothesis was partially supported in that overall work productivity loss had a significant, direct relationship with anxiety, depression, and caregiver perceived burdens of financial problems, disrupted schedule, and health problems (see Table 3). Work productivity loss was not significantly associated with social support as measured by both the MOS-SSS and CRA subscale.
Table 3.
Correlations Between Caregiver WPAI Scores and Independent Variables
| Variable | Work Productivity Loss (n = 39)
|
Activity Impairment (N = 70)
|
||||
|---|---|---|---|---|---|---|
| rs | 95% CIrs | pa | rs | 95% CIrs | pb | |
| Anxiety | .393 | [.090, .629] | .007 | .486 | [.282, .647] | <.001 |
| Depression | .357 | [.050, .604] | .013 | .471 | [.264, .635] | <.001 |
| Lack of family support | .233 | [−.090, .508] | .077 | .464 | [.254, .635] | <.001 |
| Financial problems | .291 | [−.030, .558] | .036 | .299 | [.060, .501] | .014 |
| Disrupted schedule | .410 | [.119, .641] | .005 | .669 | [.515, .782] | <.001 |
| Health problems | .551 | [.282, .740] | <.001 | .677 | [.523, .789] | <.001 |
| Self-esteem | −.092 | [−.397, .226] | .289 | −.217 | [−.430, .020] | .076 |
| Social support | −.112 | [−.414, .207] | .249 | −.299 | [−.501, −.060] | .013 |
Note: rs, Spearman’s rho; CI, confidence interval.
One-tailed.
Two-tailed.
Activity impairment was not significantly associated with any caregiver demographic variable, health self-rating, provision of care to other individuals, or cancer stage. It did have a significant, direct relationship with reported hours of caregiving (rs = .52, p < .001) and ECOG performance status (rs = .42, p = .001), with greater number of hours of caregiving and worse functional status of the care recipient associated with greater activity impairment.
Discussion
Health promotion behaviors and work productivity loss in a sample of informal caregivers of patients with advanced cancer were examined in this study. Most caregivers rated their health as excellent or good, were engaged in wellness checkups and screenings, and reported eating a healthy diet. Yet more than 50% did not meet the recommended guidelines for physical activity of 150 minutes of moderate-intensity activity per week (U.S. Department of Health and Human Services, 2008). This paradox of high overall health ratings and low self-reported physical activity levels may be due to both subject and measurement factors. Individuals may view health in a narrow sense as absence of disease and may not incorporate their health promotion behaviors into their overall assessment of health. Or they may over-rate the extent to which they are eating a healthy diet. It is also possible that they may actually not be getting enough activity because they are not aware of the activity guidelines. Our imprecise measurement of diet with a single global question may have also contributed to the discrepancy in reported health behaviors related to diet and physical activity. Levels of physical activity in this study are somewhat consistent with physical activity levels among adults in the United States. Tucker, Welk, and Beyler (2011) reported that when measured by self-report, 62.0% of a nationally representative sample of adults (n = 3,082) met the 2008 Physical Activity Guidelines for Americans. However, when activity levels were measured objectively by accelerometer, this percentage dropped to 9.6%.
Our results did not concur with the finding in general caregiver studies (Burton et al., 1997; Scharlach et al., 1997) that lower participation in exercise was associated with providing greater levels of assistance with activities of daily living. In this study, physical activity was not significantly associated with hours of caregiving or functional status of the care recipient. The discrepancy in findings may be due to the small sample size and differences in how caregiver assistance was evaluated. The general caregiver studies defined levels of caregiving intensity based on the number of IADLs or self-care ADLs with which the caregiver assisted, whereas we used time as the basis for caregiving level. Although increased hours of assistance have been significantly correlated with increased levels of caregiving (Burton et al., 1997), our time categories may not have been narrow enough to reflect caregiving intensity. Regardless of the differences in measurement, in our study caregivers who were female, with poor self-ratings of health, and perceived burdens of lack of family support and health problems, were likely to report lower levels of physical activity. This finding is consistent with those of Tucker et al. (2011) who noted that women reported fewer minutes per week of moderate and vigorous activity than men. These characteristics may be helpful in identifying high risk groups in need of targeted interventions as other studies have associated poor health (Scharlach et al., 1997) and high perceived burden (Sisk, 2000) with fewer health promoting behaviors.
The overall work productivity loss in this study of 22.9% was slightly higher than the 20.1% reported by Giovannetti et al. (2009), who also used the WPAI in a sample of informal caregivers. Our study underscores the importance of evaluating both absenteeism and presenteeism. Almost 75% of the employed caregivers had not missed work, and had we only assessed absenteeism, we would have been overly optimistic in our conclusions. The impact of caregiving on work was more evident in the 15.41% presenteeism reported by our caregivers, which again is very close to the 18.5% found by Giovannetti et al. (2009).
Greater work productivity loss was associated with higher levels of depression and anxiety, and with greater perceived caregiver burden related to financial problems, disrupted schedule, and health problems. Although caregiver burden related to lack of family support trended towards a significant relationship with work productivity, it was surprising that perceived social support did not. This may be due to the lack of variability in social support scores, making it difficult to examine the true relationship between work productivity and social support.
There are several findings in the correlational analyses that are worth noting. As expected and similar to findings in other studies, greater hours of caregiving were associated with greater work productivity loss (Giovannetti et al., 2009; Sherwood et al., 2008). Caregivers who provide more hours of care are likely to miss more work time. But, in contrast to Giovannetti et al. (2009), we did not find a significant correlation between coresidence and work productivity loss.
Like Giovannetti et al. (2009), we did not find significant gender differences in work productivity but did find that married status was moderately associated with greater productivity loss. This was an interesting finding considering we did find gender differences related to health problems. Gaugler et al. (2008) found that women who worked were more distressed than employed men and associated this finding with role overload. It is possible that women continue to work despite physical or emotional problems because they must keep their job or because they view work as respite from caregiving. Perhaps role overload or role strain plays a negative role in the productivity of married caregivers, regardless of gender.
The results of this study support the recommendations from the Family Caregiver Alliance (2006) to include assessment of emotional and physical well-being in routine, systematic evaluations of caregivers. The significant relationship between anxiety and depression and work productivity is supported in the literature (Giovannetti et al., 2009). Although due to the correlative design of this study we cannot determine if anxiety or depression causes work productivity loss, or vice-versa, Johns (2010) described depression as a strong contributor to presenteeism because it is often not viewed as a valid excuse for absence from work. Nurses should ask caregivers if they are working, explore the importance of work to the caregiver, and be attentive to depressive symptoms in the caregiver. Suggestions to access workplace caregiver assistance programs and to seek treatment of depression or anxiety if appropriate may help to improve the psychosocial well-being and work productivity of the caregiver.
Caregiver physical health, measured either as burden or self-rating, had the strongest correlation with work productivity loss and a significant association with physical activity. This finding, although somewhat intuitive, as individuals coping with health problems are more likely to be absent or pre-occupied while at work as well as less active physically, has implications for assessment of caregivers. In a meta-analysis of predictors of physical health in caregivers, depressive symptoms were more strongly related to physical health than were caregiving demands (Pinquart & Sorensen, 2007). Caregivers with poor health may be at risk not only for poor work productivity, but also for depression. Nurses should ask caregivers to rate their own health and should inquire about their health promotion behaviors, including physical activity. Routine interactions with the caregiver may provide an opportunity for the nurse to educate about healthy lifestyles or link caregivers to appropriate community resources.
Limitations
This descriptive study adds to our understanding of the health promotion and work behaviors of informal caregivers of individual with cancer. However, the use of a convenience sample and the small number of employed caregivers limits generalizability of results and more importantly increases the risk of a Type 2 error. The study’s cross-sectional design prevents us from making any conclusions relating to causality. Future researchers should use a longitudinal approach to (a) monitor patterns in caregiver health promotion and work behaviors along the cancer trajectory from the treatment period through survivorship and end-of-life, and (b) identify the downstream effects on caregiver health and employment.
Last, the measures used in this study were limited. Although the WPAI quantifies work productivity loss, evaluation of other factors would enrich the description of the impact of caregiving on work. Caregivers often reduce work hours, quit their jobs, take leaves of absences, retire early, use vacation or sick time for caregiving, or decline promotions or training (Pitsenberger, 2006). Other caregiving responsibilities may also influence work productivity loss. Reliance on self-reports of health behaviors is another limitation and consideration should be given to supplementing self-report with objective measures of physical activity.
Conclusion
The WPAI was effectively used in a self-administered format and provided a comprehensive measure of the impact of caregiving on work productivity in a sample of informal caregivers of individuals with advanced cancer. A psychological dimension to work productivity loss was evident in its associations with depression, anxiety, and burden, and is suggestive that interventions to improve mood and lessen burden may also improve work productivity. Caregivers in this sample generally reported positive health promotion behaviors related to nutrition and engagement in wellness visits and health screening, but were not meeting guidelines for physical activity. Nurses, with their expertise in family-centered care and knowledge of the cancer care trajectory, are in a unique position to assess caregivers and provide health promotion education, which may ultimately improve the health of caregivers and reduce the economic impact of caregiving.
Acknowledgments
Grant sponsor: NINR; Grant number: R01NR010787.
References
- AARP. Valuing the invaluable: The economic value of family caregiving, 2008 update. Insight on the Issues. 2008:13. Retrieved from http://assets.aarp.org/rgcenter/il/i13_caregiving.pdf.
- Beesley VL, Price MA, Webb PM Australian Ovarian Cancer Study Group, & Australian Ovarian Cancer Study—Quality of Life Study Investigators. Loss of lifestyle: Health behaviour and weight changes after becoming a caregiver of a family member diagnosed with ovarian cancer. Supportive Care in Cancer. 2010 doi: 10.1007/s00520-010-1035-2. advance online publication. [DOI] [PubMed] [Google Scholar]
- Burton LC, Newsom JT, Schulz R, Hirsch CH, German PS. Preventive health behaviors among spousal caregivers. Preventive Medicine. 1997;26:162–169. doi: 10.1006/pmed.1996.0129. [DOI] [PubMed] [Google Scholar]
- Cameron JI, Franche R, Cheung AM, Stewart DE. Lifestyle interference and emotional distress in family caregivers of advanced cancer patients. Cancer. 2002;94:521–527. doi: 10.1002/cncr.10212. [DOI] [PubMed] [Google Scholar]
- Carter PA. Caregivers’ descriptions of sleep changes and depressive symptoms. Oncology Nursing Forum. 2002;29:1277–1283. doi: 10.1188/02.ONF.1277-1283. [DOI] [PubMed] [Google Scholar]
- Chou KR. Caregiver burden: A concept analysis. Journal of Pediatric Nursing. 2000;15:398–407. doi: 10.1053/jpdn.2000.16709. [DOI] [PubMed] [Google Scholar]
- Coe NB, van Houtven CH. Caring for mom and neglecting yourself? The health effects of caring for an elderly parent. Health Economics. 2009;18:991–1010. doi: 10.1002/hec.1512. [DOI] [PubMed] [Google Scholar]
- Edwards BK, Howe HL, Ries LAG, Thun MJ, Rosenberg HM, Yancik R, Feigal EG. Annual report to the nation on the status of cancer, 1973–1999, featuring implications of age and aging on U.S. cancer burden. Cancer. 2002;94:2766–2792. doi: 10.1002/cncr.10593. [DOI] [PubMed] [Google Scholar]
- Family Caregiver Alliance. Caregiver assessment: Principles, guidelines and strategies for change. Report from a National Consensus Development Conference; San Francisco, CA: Author; 2006. [Google Scholar]
- Gaugler JE, Given WC, Linder J, Kataria R, Tucker G, Regine WF. Work, gender, and stress in family cancer caregiving. Supportive Care in Cancer. 2008;16:347–357. doi: 10.1007/s00520-007-0331-y. [DOI] [PubMed] [Google Scholar]
- Giovannetti ER, Wolff JL, Frick KD, Boult C. Construct validity of the Work Productivity and Activity Impairment Questionnaire across informal caregivers of chronically ill older patients. Value in Health. 2009;12:1011–1017. doi: 10.1111/j.1524-4733.2009.00542.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Given B, Wyatt G, Given C, Sherwood P, Gift A, DeVoss D, Rahbar M. Burden and depression among caregivers of patients at the end of life. Oncology Nursing Forum. 2004;31:1105–1115. doi: 10.1188/04.ONF.1105-1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Given CW, Given B, Stommel M, Collins C, King S, Franklin S. The Caregiver Reaction Assessment (CRA) for caregivers to persons with chronic physical and mental impairments. Research in Nursing & Health. 1992;15:271–283. doi: 10.1002/nur.4770150406. [DOI] [PubMed] [Google Scholar]
- Grunfeld E, Coyle D, Whelan T, Clinch J, Reyno L, Earle CC, Glossop R. Family caregiver burden: Results of a longitudinal study of breast cancer patients and their principal caregivers. Canadian Medical Association Journal. 2004;170:1795–1801. doi: 10.1503/cmaj.1031205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gysels M, Higginson IJ. Reconciling employment with caring for a husband with an advanced illness. BMC Health Services Research. 2009;9:216. doi: 10.1186/1472-6963-9-216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haylock PJ. Advanced cancer: Emergence of a new survivor population. Seminars in Oncology Nursing. 2010;26:144–150. doi: 10.1016/j.soncn.2010.05.008. [DOI] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Johns G. Presenteeism in the workplace: A review and research agenda. Journal of Organizational Behavior. 2010;31:519–542. doi: 10.1002/job.630. [DOI] [Google Scholar]
- Kim Y, Baker F, Spillers RL, Wellisch D. Psychological adjustment of cancer caregivers with multiple roles. Psycho-Oncology. 2006;15:795–804. doi: 10.1002/pon.1013. [DOI] [PubMed] [Google Scholar]
- Kim Y, Given BA. Quality of life of family caregivers of cancer survivors. Cancer Supplement. 2008;112:2556–2568. doi: 10.1002/cncr.23449. [DOI] [PubMed] [Google Scholar]
- Kim Y, Schulz R. Family caregivers’ strains. Comparative analysis of cancer caregiving with dementia, diabetes, and frail elderly caregiving. Journal of Aging and Health. 2008;20:483–503. doi: 10.1177/0898264308317533. [DOI] [PubMed] [Google Scholar]
- Kitrungrote L, Cohen M. Quality of life of family caregivers of patients with cancer: A literature review. Oncology Nursing Forum. 2006;33:625–632. doi: 10.1188/06.ONF.625-632. [DOI] [PubMed] [Google Scholar]
- Metlife Mature Market Institute, National Alliance for Caregiving, & University of Pittsburgh Institute on Aging. The MetLife study of working caregivers and employer health care costs. 2010 Retrieved from http://www.metlife.com/mmi/research/working-caregiver-employer-health-care-costs.html#findings.
- McNair DM, Lorr M, Droppleman LF. EdITS manual for the profile of mood states. San Diego, CA: EdITS/Educational and Industrial Testing Service; 1992. [Google Scholar]
- National Alliance for Caregiving & AARP. Caregiving in the US 2009. 2009 Retrieved from http://www.caregiving.org/data/Caregiving_in_the_US_2009_full_report.pdf.
- Nijboer C, Trienstra M, Tempelaar R, Sanderman R, van den Bos G. Measuring both negative and positive reactions to giving care to cancer patients: Psychometric qualities of the Caregiver Reaction Assessment (CRA) Social Science & Medicine. 1999;48:1259–1269. doi: 10.1016/s0277-9536(98)00426-2. [DOI] [PubMed] [Google Scholar]
- Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP. Toxicity and response criteria of the Eastern Oncology Cooperative Group. American Journal of Clinical Oncology. 1982;5:649–655. [PubMed] [Google Scholar]
- Pinquart M, Sorensen S. Correlates of physical health of informal caregivers: A meta-analysis. Journal of Gerontology: Psychological Sciences. 2007;62B:126–137. doi: 10.1093/geronb/62.2.p126. [DOI] [PubMed] [Google Scholar]
- Pitsenberger DJ. Juggling work and elder caregiving. AAOHN Journal. 2006;54:181–185. doi: 10.1177/216507990605400408. [DOI] [PubMed] [Google Scholar]
- Prasad M, Wahlqvist P, Shikiar R, Shih YT. A review of self-reported instruments measuring health-related work productivity: A patient-reported outcomes perspective. Pharmacoeconomics. 2004;22:225–244. doi: 10.2165/00019053-200422040-00002. [DOI] [PubMed] [Google Scholar]
- Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4:353–365. doi: 10.2165/00019053-199304050-00006. [DOI] [PubMed] [Google Scholar]
- Scharlach AE, Midanik LT, Runkle MC, Soghikian K. Health practices of adults with elder care responsibilities. Preventive Medicine. 1997;26:155–161. doi: 10.1006/pmed.1996.0128. [DOI] [PubMed] [Google Scholar]
- Schulz R, Sherwood PR. Physical and mental health effects of family caregiving. American Journal Nursing. 2008;108(9):23–27. doi: 10.1097/01.NAJ.0000336406.45248.4c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schumacher KL, Stewart BJ, Archbold PG, Caparro M, Mutale F, Agrawal S. Effects of caregiving demand, mutuality, and preparedness on family caregiver outcomes during cancer treatment. Oncology Nursing Forum. 2008;35:49–56. doi: 10.1188/08.ONF.49-56. [DOI] [PubMed] [Google Scholar]
- Sherbourne CD, Stewart AL. The MOS social support survey. Social Science & Medicine. 1991;32:705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- Sherwood PR, Donovan HS, Given CW, Lu X, Given BA, Hricik A, Bradley S. Predictors of employment and lost hours from work in cancer caregivers. Psycho-Oncology. 2008;17:598–605. doi: 10.1002/pon.1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sisk RJ. Caregiver burden and health promotion. International Journal of Nursing Studies. 2000;37:37–43. doi: 10.1016/s0020-7489(99)00053-x. [DOI] [PubMed] [Google Scholar]
- Stenberg U, Ruland CM, Miaskowski C. Review of the literature on the effects of caring for a patient with cancer. Psycho-Oncology. 2010;19:1013–1025. doi: 10.1002/pon.1670. [DOI] [PubMed] [Google Scholar]
- Stetz KM, Brown M. Physical and psychosocial health in family caregiving: A comparison of AIDS and cancer caregivers. Public Health Nursing. 2004;21:533–540. doi: 10.1111/j.0737-1209.2004.21605.x. [DOI] [PubMed] [Google Scholar]
- Swanberg JE. Making it work: Informal caregiving, cancer, and employment. Journal of Psychosocial Oncology. 2006;24(3):1–18. doi: 10.1300/J077v24n03_01. [DOI] [PubMed] [Google Scholar]
- Tucker JM, Weld GJ, Beyler NK. Physical activity in U.S. adults. Compliance with the Physical Activity Guideline for Americans. American Journal of Preventive Medicine. 2011;40:454–461. doi: 10.1016/j.amepre.2010.12.016. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Physical activity guidelines for Americans. ODPHP Publication No. U0036. 2008 Retrieved from http://www.health.gov/paguidelines/guidelines/default.aspx.
- van Ryn M, Sanders S, Kahn K, van Houtven C, Griffin JM, Martin M, Rowland J. Objective burden, resources, and other stressors among informal cancer caregivers: A hidden quality issue? Psycho-Oncology. 2011;20:44–52. doi: 10.1002/pon.1703. [DOI] [PMC free article] [PubMed] [Google Scholar]