Abstract
Background
Differences in the control of blood pressure, cholesterol, and glucose among the various racial and ethnic groups of Medicare enrollees may contribute to persistent disparities in health outcomes.
Methods
Among elderly enrollees in Medicare Advantage health plans in 2011 who had hypertension (94,171 persons), cardiovascular disease (112,039), or diabetes (105,848), we compared the respective age-and-sex-adjusted proportions with blood pressure lower than 140/90 mm Hg, low-density lipoprotein cholesterol levels below 100 mg per deciliter (2.6 mmol per liter), and a glycated hemoglobin value of 9.0% or lower, according to race or ethnic group. Comparisons were made nationally and within regions and health plans, and changes since 2006 were assessed.
Results
Black enrollees in 2006 and 2011 were substantially less likely than white enrollees to have adequate control of blood pressure (adjusted absolute differences in proportions of enrollees in the 2 years, 7.9 percentage points and 10.3 percentage points, respectively), cholesterol (11.4 percentage points and 10.2 percentage points, respectively), and glycated hemoglobin (10.1 percentage points and 9.4 percentage points, respectively) (P<0.001 for all comparisons). Differing distributions of enrollees among health plans accounted for 39 to 59% of observed disparities in 2011. These differences persisted in 2011 in the Northeast, Midwest, and South (6.9 to 14.1 percentage points, P<0.001 for all comparisons) but were eliminated in the West for all three measures (<1.5 percentage points, P≥0.15). Hispanic enrollees were less likely than whites in 2011 to have adequate control of blood pressure (adjusted difference, 1.6 percentage points), cholesterol (adjusted difference, 1.0 percentage points), and glycated hemoglobin (adjusted difference, 3.4 percentage points) (P≤0.02 for all comparisons). Asians and Pacific Islanders were more likely than whites to have adequate control of blood pressure (difference, 4.4 percentage points; P<0.001) and cholesterol (5.5 percentage points, P<0.001) and had similar control of glycated hemoglobin (0.3 percentage points, P = 0.63).
Conclusions
Disparities in control of blood pressure, cholesterol, and glucose have not improved nationally for blacks in Medicare Advantage plans, but these disparities were eliminated in the West in 2011. (Funded by the National Institute on Aging.)
Since Medicare was established in the United States nearly 50 years ago, disparities in health outcomes between whites and blacks have persisted,1 with only limited improvement in the past decade.2 In 2008, life expectancy was 5.4 years shorter for black men and 3.7 years shorter for black women than for white men and white women; cardiovascular disease and diabetes accounted for 38% of the racial gap in mortality among men and for 54% among women.2 Higher levels of blood pressure, cholesterol, and glucose among blacks with hypertension,3,4 cardiovascular disease,5,6 and diabetes,7 respectively, contribute to substantial excess morbidity and mortality from myocardial infarction, congestive heart failure, stroke, peripheral vascular disease, and kidney disease. Similar disparities in risk-factor control have been reported for Hispanic adults with those conditions,4,5,7 but reports on Asian or Pacific Islander adults have not been included in most national studies.
In 1997, the Medicare program began monitoring the quality of care in health maintenance organizations (HMOs) with the use of measures from the Healthcare Effectiveness Data and Information Set (HEDIS) developed by the National Committee for Quality Assurance.8 A previous study of black enrollees and white enrollees with cardiovascular disease or diabetes showed that disparities in annual testing of low-density lipo-protein (LDL) cholesterol and glycated hemoglobin levels were significantly narrowed between 1997 and 2003.9 Within most Medicare HMOs, however, racial disparities persisted in the control of these risk factors and in the control of blood pressure for enrollees with hypertension.10 Less is known about these measures for Hispanic, Asian, and Pacific Islander enrollees in Medicare HMOs, because accurate data on these racial and ethnic designations have been lacking.11,12 However, Medicare data now include more accurate designations of these groups.13
In this study, we assessed differences in the control of blood pressure, cholesterol, and glucose according to race or ethnic group in 2006 and 2011 in a national cohort of Medicare Advantage enrollees. We also evaluated how these differences were related to differences in performance among geographic regions and health plans. Because recent studies have documented major improvements in the care of patients with hypertension and diabetes in the Kaiser Permanente Northern California health plan,14,15 we also compared disparities in Kaiser health plans with disparities in non-Kaiser health plans.
Methods
Study Cohort
We studied elderly persons who were enrolled in Medicare HMOs in 2006 and 2011. We selected these years because the specification of HEDIS performance measures for control of LDL cholesterol changed in 2006, and 2011 was the most recent year for which HEDIS data were available when our study was conducted. Our study was approved by the Harvard Medical School Committee on Human Studies and by the Privacy Board of the Centers for Medicare and Medicaid Services (CMS).
We obtained data on demographic characteristics (age, sex, race or ethnic group, and state of residence), HMO enrollment, and vital status from the Medicare Beneficiary Summary File. We included HMO enrollees who were identified as black, Hispanic, Asian or Pacific Islander, or non-Hispanic white by means of a new variable for race or ethnic group that was developed to identify Hispanic and Asian or Pacific Islander beneficiaries more accurately from surnames and preferred language in Medicare data.13,16 This new algorithm increased the sensitivity for identifying Hispanic beneficiaries in Medicare enrollment data from 30% to 77% and for identifying Asian or Pacific Islander beneficiaries from 55% to 79%, while maintaining a specificity of 99% for each group.13 As described previously, we excluded partial-year enrollees, those in HMOs with fewer than 500 enrollees, and those who died during the study years.17 In 2011, excluded enrollees represented less than 2% of all enrollees with HEDIS data on hypertension (1.5%), cardiovascular disease (1.3%), and diabetes (1.7%), and in 2006, excluded enrollees represented slightly higher proportions of enrollees with these conditions (5.7%, 1.4%, and 3.9%, respectively).
Outcome Measures
Medicare HMOs submit individual-level data on HEDIS measures to CMS as specified by the National Committee for Quality Assurance.18 For this study, we focused on blood-pressure control (a target blood pressure of <140/90 mm Hg) for enrollees 65 to 85 years of age who had hypertension, LDL cholesterol testing and control (a target level of <100 mg per deciliter [2.6 mmol per liter]) for those 65 to 75 years of age who had cardiovascular disease, and glycated hemoglobin testing and control (a target level of ≤9.0%) for those 65 to 75 years of age who had diabetes. We opted not to assess enrollees with diabetes for the more stringent glycated hemoglobin target of less than 7.0% because this goal may not be clinically appropriate for many elderly patients.19
Statistical Analysis
We calculated differences in age-and-sex-adjusted proportions of enrollees with blood-pressure control, LDL cholesterol testing and control, and glycated hemoglobin testing and control for each minority group relative to white enrollees nationally in 2011. We weighted all estimates to reflect the distribution of persons with hypertension, cardiovascular disease, and diabetes, respectively, in each health-plan contract across the strata of HMO enrollees defined according to age, sex, and race or ethnic group on the basis of the disease prevalence and population within each stratum. To estimate the prevalence of cardiovascular disease and diabetes, we used the Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey to tally self-reported rates of these conditions according to race and ethnic group among Medicare HMO enrollees. Medicare enrollees were not asked to report hypertension in this survey, so we used a published national report to estimate the prevalence of hypertension among elderly adults according to race and ethnic group.3
To estimate age-and-sex-adjusted disparities between whites and each minority group, we directly standardized (reweighted) the age and sex distributions of white enrollees to those of each minority group in turn and compared weighted rates. We subsequently assessed the contributions of regional and plan effects by reweighting the distributions of white enrollees to match the distributions of other racial or ethnic groups according to region and then to plan. Because national differences were largest between black enrollees and white enrollees, we stratified these differences according to year and to the four regions of the United States (Northeast, Midwest, South, and West), as defined by the Census Bureau, to compare the magnitude of adjusted differences in 2006 and 2011. Findings from intervening years are in the Supplementary Appendix (available with the full text of this article at NEJM.org). We also stratified differences between black enrollees and white enrollees in Kaiser Permanente and other health plans in the West and South.
All analyses were conducted with the use of SAS software, version 9.2 (SAS Institute). Two-sided P values and 95% confidence intervals are reported for statistical tests, with the use of estimators for stratified sampling.
Results
Study Population
The characteristics of the study cohorts with hypertension, cardiovascular disease, and diabetes in 2011 are shown in Table 1, weighted according to the prevalence of these conditions and distributions of black, Hispanic, and Asian or Pacific Islander enrollees in Medicare HMOs. Table 2 shows age-and-sex-adjusted rates of performance for each quality measure nationally for minority enrollees as compared with white enrollees in 2011. Adjusted differences between minority enrollees and white enrollees are also shown after matching racial and ethnic groups within regions and health plans. The frequency of testing for LDL cholesterol and glycated hemoglobin ranged from 89.6% to 94.9% across all racial and ethnic groups, and adjusted differences were less than 3% for each minority group as compared with whites nationally for both process measures.
Table 1. Characteristics of Enrollees in Medicare Advantage HMOs in 2011, According to Condition.*.
| Variable | Hypertension | Cardiovascular Disease | Diabetes | |||
|---|---|---|---|---|---|---|
| HEDIS Sample (N = 94,171) no. (%) |
Weighted Sample (N = 2,307,553)† % |
HEDIS Sample (N = 112,039) no. (%) |
Weighted Sample (N = 653,039)† % |
HEDIS Sample (N = 105,848) no. (%) |
Weighted Sample (N = 1,065,508)† % |
|
| Race or ethnic group‡ | ||||||
| White | 60,855 (64.6) | 69.1 | 81,952 (73.1) | 74.9 | 65,040 (61.4) | 60.7 |
| Black | 14,507 (15.4) | 13.3 | 11,045 (9.9) | 9.6 | 15,208 (14.4) | 15.5 |
| Hispanic | 13,556 (14.4) | 13.3 | 13,545 (12.1) | 12.0 | 20,132 (19.0) | 18.6 |
| Asian or Pacific Islander | 5,253 (5.6) | 4.2 | 5,497 (4.9) | 3.5 | 5,468 (5.2) | 5.3 |
| Age | ||||||
| 65–70 yr | 32,223 (34.2) | 31.7 | 51,028 (45.5) | 44.7 | 57,476 (54.3) | 53.1 |
| 71–75 yr | 26,132 (27.8) | 27.6 | 61,011 (54.5) | 55.4 | 48,372 (45.7) | 46.9 |
| 76–80 yr | 21,081 (22.4) | 23.5 | — | — | — | — |
| 81–85 yr | 14,735 (15.6) | 17.2 | — | — | — | — |
| Sex | ||||||
| Male | 39,107 (41.5) | 42.4 | 70,724 (63.1) | 62.6 | 50,586 (47.8) | 48.5 |
| Female | 55,064 (58.5) | 57.6 | 41,315 (36.9) | 37.4 | 55,262 (52.2) | 51.5 |
| Region | ||||||
| Northeast | 21,280 (22.6) | 21.7 | 14,698 (13.1) | 21.4 | 20,258 (19.1) | 21.3 |
| Midwest | 18,180 (19.3) | 13.6 | 14,836 (13.2) | 13.9 | 16,249 (15.4) | 12.6 |
| South | 27,169 (28.9) | 28.8 | 25,980 (23.2) | 29.2 | 29,587 (28.0) | 30.4 |
| West | 27,542 (29.2) | 35.9 | 56,525 (50.5) | 35.6 | 39,754 (37.6) | 35.6 |
HEDIS denotes Healthcare Effectiveness Data and Information Set, and HMO health maintenance organization. A dash indicates that no enrollees were assessed in the specified age group. Not all percentages sum to 100 because of rounding.
The samples were weighted on the basis of the prevalence of each condition according to race or ethnic group among elderly adults.
Data on race and ethnic group were obtained from the Medicare Beneficiary Summary File.
Table 2. Differences in Blood-Pressure Control, Cholesterol Testing and Control, and Glycated Hemoglobin Testing and Control between Minority Enrollees and White Enrollees in Medicare HMOs in 2011.*.
| Variable | Minority Enrollees | National Proportions† | Difference Between Minority and White Enrollees | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Minority | White | National† | Region‡ | Plan‡ | |||||
| no. | % | percentage points | P value | percentage points | P value | percentage points | P value | ||
| Black vs. white | |||||||||
| Blood pressure <140/90 mm Hg | 14,507 | 59.2±0.4 | 69.5±0.2 | 10.3 | <0.001 | 8.5 | <0.001 | 4.2 | <0.001 |
| Testing of LDL cholesterol level | 11,045 | 89.6±0.3 | 91.8±0.1 | 2.2 | <0.001 | 2.0 | <0.001 | 1.9 | <0.001 |
| LDLcholesterol level <100 mg/dl | 11,045 | 53.9±0.5 | 64.1±0.2 | 10.2 | <0.001 | 8.2 | <0.001 | 6.3 | <0.001 |
| Testing of glycated hemoglobin level | 15,208 | 91.7±0.2 | 93.8±0.1 | 2.1 | <0.001 | 1.7 | <0.001 | 1.4 | 0.005 |
| Glycated hemoglobin level ≤9.0% | 15,208 | 74.6±0.4 | 84.0±0.2 | 9.4 | <0.001 | 8.0 | <0.001 | 5.7 | <0.001 |
| Hispanic vs. white | |||||||||
| Blood pressure <140/90 mm Hg | 13,556 | 68.2±0.4 | 69.8±0.2 | 1.6 | <0.001 | 1.5 | 0.002 | −3.6 | 0.005 |
| Testing of LDL cholesterol level | 13,545 | 94.6±0.2 | 91.9±0.1 | −2.7 | <0.001 | −2.4 | <0.001 | −1.8 | <0.001 |
| LDL cholesterol level <100 mg/dl | 13,545 | 64.5±0.4 | 65.6±0.2 | 1.0 | 0.02 | 0.9 | 0.07 | 0.5 | 0.68 |
| Testing of glycated hemoglobin level | 20,132 | 94.8±0.2 | 93.8±0.1 | −1.0 | <0.001 | −0.8 | <0.001 | −1.4 | 0.01 |
| Glycated hemoglobin level ≤9.0% | 20,132 | 80.6±0.3 | 84.0±0.2 | 3.4 | <0.001 | 3.8 | <0.001 | 1.7 | 0.09 |
| Asian or Pacific Islander vs. white | |||||||||
| Blood pressure <140/90 mm Hg | 5,253 | 74.1±0.7 | 69.7±0.2 | −4.4 | <0.001 | −2.0 | 0.005 | −7.3 | <0.001 |
| Testing of LDL cholesterol level | 5,497 | 94.7±0.3 | 92.1±0.1 | −2.7 | <0.001 | −2.0 | <0.001 | −3.8 | <0.001 |
| LDL cholesterol level <100 mg/dl | 5,497 | 72.3±0.6 | 66.8±0.2 | −5.5 | <0.001 | −2.5 | <0.001 | −4.9 | <0.001 |
| Testing of glycated hemoglobin level | 5,468 | 94.9±0.3 | 93.7±0.1 | −1.1 | 0.002 | −0.5 | 0.20 | −3.0 | 0.001 |
| Glycated hemoglobin level ≤9.0% | 5,468 | 83.7±0.6 | 84.0±0.2 | 0.3 | 0.63 | 2.6 | <0.001 | −1.8 | 0.25 |
Plus–minus values are means ±SE. P values of 0.05 or less were considered to indicate statistical significance. LDL denotes low-density lipoprotein.
Proportions were directly standardized to the estimated distribution of prevalence according to age and sex for each minority group; in the comparisons, the proportions of white enrollees were standardized to the distribution of enrollees in the respective minority group.
The proportions of white enrollees were additionally weighted to match distributions of minority comparison groups across geographic regions and health plans.
Risk-Factor Control
Risk-factor control was substantially lower for blacks than for whites for blood pressure (adjusted difference, 10.3 percentage points), LDL cholesterol (10.2 percentage points), and glycated hemoglobin (9.4 percentage points) (P<0.001 for all comparisons) (Table 2). Matching within region reduced the relative magnitude of these differences by only 15 to 19%, whereas matching within health plans reduced the relative differences by 39 to 59%, indicating that blacks were disproportionately enrolled in lower-performing health plans.
Control among Hispanic enrollees nationally was only slightly lower than that among white enrollees for blood pressure (1.6 percentage points, P<0.001), LDL cholesterol (1.0 percentage point, P = 0.02), and glycated hemoglobin (3.4 percentage points, P<0.001). Nationally, control of blood pressure and LDL cholesterol was better for Asians and Pacific Islanders than for whites (absolute differences of 4.4 percentage points and 5.5 percentage points, respectively; P<0.001 for both comparisons); control of glycated hemoglobin was similar to that for whites (difference of 0.3 percentage points, P = 0.63).
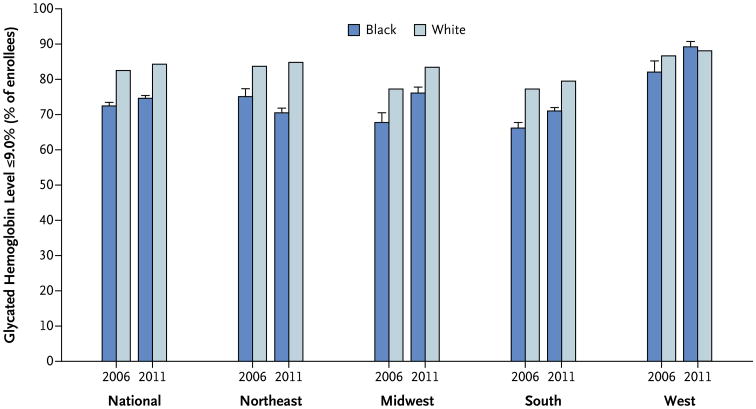
When we compared black enrollees and white enrollees within a region for control of blood pressure (Fig. 1), LDL cholesterol (Fig. 2), and glycated hemoglobin (Fig. 3) in 2006 and 2011, a consistent pattern emerged. Racial differences in 2006 were smaller in the West than in the Northeast, Midwest, or South, although the differences were still statistically worse for blacks than for whites in the West for control of LDL cholesterol and glycated hemoglobin.
Figure 1. Estimated Age-and-Sex-Adjusted Proportions of Black Enrollees and White Enrollees with Hypertension in Medicare Advantage HMOs in Whom Blood Pressure Was Controlled, Overall and According to Region.
Blood-pressure control was defined as a blood pressure lower than 140/90 mm Hg. T bars indicate 95% confidence intervals for blacks. HMO denotes health maintenance organization.
Figure 2. Estimated Age-and-Sex-Adjusted Proportions of Black Enrollees and White Enrollees with Cardiovascular Disease in Medicare Advantage HMOs in Whom Low-Density Lipoprotein Cholesterol Was Controlled, Overall and According to Region.
Control of low-density lipoprotein (LDL) cholesterol was defined as a level of less than 100 mg per deciliter (2.6 mmol per liter). T bars indicate 95% confidence intervals for blacks.
Figure 3. Estimated Age-and-Sex-Adjusted Proportions of Black Enrollees and White Enrollees with Diabetes in Medicare Advantage HMOs in Whom Glycated Hemoglobin Was Controlled, Overall and According to Region.
Control of glycated hemoglobin was defined as a level of 9.0% or less. T bars indicate 95% confidence intervals for blacks.
The frequency of blood-pressure control in 2011 (Fig. 1) was identical for black enrollees and white enrollees in the West (74% for both, P = 0.81) but was much lower for blacks in the Northeast (60% vs. 71%), Midwest (60% vs. 69%), and South (53% vs. 63%) (P<0.001 for all comparisons). Similarly, the frequency of LDL cholesterol control in 2011 (Fig. 2) was nearly equivalent for black enrollees and white enrollees in the West (71% and 70%, respectively; P = 0.82) but was much lower for black enrollees than for white enrollees in the Northeast (51% vs. 65%), Midwest (53% vs. 62%), and South (49% vs. 57%) (P<0.001 for all comparisons). Control of glycated hemoglobin (Fig. 3) for black enrollees and white enrollees was also similar in the West (89% and 88%, respectively; P = 0.15) but not in the Northeast (71% vs. 85%), Midwest (76% vs. 83%), or South (71% vs. 79%) (P<0.001 for all comparisons).
In stratified analyses of Kaiser and other health plans in the West, significant disparities between black enrollees and white enrollees in the frequency of blood-pressure control were not evident in Kaiser health plans in 2006 (67% vs. 73%, P = 0.18) or 2011 (89% vs. 85%, P = 0.41), but there were significant disparities between the two groups in other health plans in 2006 (52% vs. 57%, P = 0.04) and in 2011 (58% vs. 66%, P<0.001). For control of LDL cholesterol, disparities were evident in 2006 in Kaiser health plans (59% vs. 68%, P<0.001) and in other health plans (47% vs. 60%, P<0.001). In 2011, these disparities between black enrollees and white enrollees were eliminated in Kaiser health plans (81% in both groups, P = 0.92) but not in other plans (56% vs. 64%, P = 0.001). In 2006, disparities in the control of glycated hemoglobin between black enrollees and white enrollees were evident in Kaiser health plans (84% vs. 90%, P = 0.01) and in other plans (77% vs. 82%, P = 0.02); in 2011 these disparities were eliminated in Kaiser health plans (92% vs. 94%, P = 0.43) and in other health plans (84% for both groups, P = 0.91). A less consistent pattern was evident among Kaiser health plans in the South, where disparities between black enrollees and white enrollees in 2011 persisted for control of blood pressure (70% vs. 81%, P = 0.01) and LDL cholesterol (65% vs. 84%, P = 0.001) but not for glycated hemoglobin (92% vs. 93%, P = 0.75).
Discussion
This study of risk-factor control for hypertension, cardiovascular disease, and diabetes in Medicare Advantage health plans provides a number of important insights about evolving racial and ethnic disparities for these major chronic conditions. First, testing of LDL cholesterol and glycated hemoglobin levels has continued to increase since 2003.9 In 2011, the frequency of testing was consistently high for all racial and ethnic groups, with minimal differences nationally. Second, Hispanic enrollees had only slightly lower rates of risk-factor control than did white enrollees in 2011, and Asian and Pacific Islander enrollees had rates that were similar to or higher than those of white enrollees. Third, despite overall improvements in risk-factor control for black enrollees and white enrollees in 2011 as compared with 2006, substantial disparities between these groups persisted nationally. Fourth, the enrollment of blacks in lower-performing health plans accounted for about half the disparity in each case, with the remainder explained by disparities within health plans. Fifth and most notably, disparities in risk-factor control for blacks have been eliminated in the West among Kaiser health plans. Approximately 43% of enrollees in Medicare Advantage plans in this region were enrolled in Kaiser health plans in 2011.
The elimination of racial disparities in control of blood pressure, LDL cholesterol, and glycated hemoglobin between black enrollees and white enrollees in Kaiser health plans in the West may reflect systematic efforts by the health plans to improve control of these risk factors over the past decade. Previous studies have shown that well-organized health care systems can achieve racial equity in processes of care through quality monitoring and improvement,9,20 as we found nationally for testing of LDL cholesterol and glycated hemoglobin. However, substantial disparities in intermediate outcomes (i.e., control of risk factors) have persisted for blacks with hypertension, cardiovascular disease, and diabetes.9,10, 20-22 Our findings in the West of nearly identical control of three major risk factors among black Medicare enrollees and white Medicare enrollees in Kaiser health plans and control of glycated hemoglobin in other health plans show the potential to achieve equity in these key health outcomes.
Our findings build on observational and quasi-experimental studies from Kaiser health plans in California that showed substantial improvements in control of blood pressure, LDL cholesterol, and glycated hemoglobin with implementation of an electronic health record,14 electronic messaging between patients and physicians,23 and a large-scale program to improve control of hypertension.15 These initiatives were also associated with reduced rates of emergency department visits and hospitalizations for enrollees who had diabetes24 and with a reduced incidence of acute myocardial infarction.25 However, these published studies have not reported whether quality-improvement initiatives reduced racial and ethnic disparities in intermediate outcomes for common chronic conditions.
A strength of our study was the nationally representative sample of enrollees from all Medicare Advantage HMOs in 2006 and 2011. We also used more accurate designations of Hispanic ethnic background and Asian and Pacific Islander race than the designations available for previous studies.
Our study had several limitations. First, although Medicare health plans follow established HEDIS reporting protocols, health plans with integrated electronic health records, such as Kaiser Permanente, may have more complete ascertainment of risk-factor measures. Second, better control of intermediate outcomes for blacks in the West may arise from changes in unmeasured factors, such as regional differences in socioeconomic status or health status, that may affect these outcomes or from increased screening to identify enrollees with less severe hypertension, cardiovascular disease, or diabetes. However, in a supplemental assessment of nationally representative CAHPS survey data for Medicare enrollees, we found no evidence of differential changes in education, health status, or prevalence of self-reported diabetes or heart disease according to race and region that might explain the elimination of racial disparities in the West (see the Supplementary Appendix).
Third, we lacked data on changes in factors that may contribute to improved control of blood pressure, LDL cholesterol, or glucose, such as increased medication prescribing and dosage intensification by physicians and greater adherence by patients,26-28 more generous Medicare Part D drug coverage,29-31 and improvement in such health behaviors as diet and physical activity.32 Fourth, we lacked information on clinical complications, such as myocardial infarction, stroke, chronic kidney disease, and premature death, which may result from inadequate control of blood pressure, cholesterol, or glucose among persons with hypertension, cardiovascular disease, or diabetes.
A new national guideline for the treatment of hypertension has recommended a blood-pressure goal of less than 150/90 mm Hg for adults 60 years of age or older and less than 140/90 mm Hg for adults with diabetes or chronic kidney disease.33 For the treatment of persons with cardiovascular disease, the new primary goal of care has shifted from the achievement of a target LDL cholesterol level to the use of high-intensity statins.34 These recent guidelines have not yet been incorporated into the HEDIS performance measures.
Measures of blood-pressure, cholesterol, and glucose control have not been routinely collected in traditional fee-for-service Medicare. Such measures are now being implemented for accountable care organizations participating in the Medicare Pioneer and the Medicare Shared Savings programs,35 so analyses of racial and ethnic disparities may become feasible in these components of traditional Medicare. Medicare HMOs have performed better than traditional Medicare on numerous HEDIS process measures, such as testing of LDL cholesterol and glycated hemoglobin, particularly among more established, larger, nonprofit health plans.17 Moreover, disparities in mammography use have been eliminated for minority women in Medicare HMOs but not in traditional Medicare.16
In conclusion, our study shows that substantial disparities in intermediate outcomes continued to persist in Medicare Advantage health plans nationally for blacks as compared with whites with hypertension, cardiovascular disease, or diabetes in 2011. These disparities were seen in all regions except the West, where Kaiser health plans achieved substantially better control overall. Future studies should identify the efforts to improve care that have been most effective in achieving equitable outcomes, so that these efforts can be replicated more broadly.36,37
Supplementary Material
Acknowledgments
Supported by a grant from the National Institute on Aging (P01 AG032952).
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
We thank Lin Ding, Ph.D., for assistance with statistical programming.
References
- 1.Harper S, Lynch J, Burris S, Davey Smith G. Trends in the black-white life expectancy gap in the United States, 1983-2003. JAMA. 2007;297:1224–32. doi: 10.1001/jama.297.11.1224. [DOI] [PubMed] [Google Scholar]
- 2.Harper S, Rushani D, Kaufman JS. Trends in the black-white life expectancy gap, 2003-2008. JAMA. 2012;307:2257–9. doi: 10.1001/jama.2012.5059. [DOI] [PubMed] [Google Scholar]
- 3.Ong KL, Cheung BM, Man YB, Lau CP, Lam KS. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999-2004. Hypertension. 2007;49:69–75. doi: 10.1161/01.HYP.0000252676.46043.18. [DOI] [PubMed] [Google Scholar]
- 4.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010;303:2043–50. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 5.Vital signs: prevalence, treatment, and control of high levels of low-density lipoprotein cholesterol — United States, 1999–2002 and 2005–2008. MMWR Morb Mortal Wkly Rep. 2011;60:109–14. [PubMed] [Google Scholar]
- 6.Vulic D, Lee BT, Dede J, Lopez VA, Wong ND. Extent of control of cardiovascular risk factors and adherence to recommended therapies in US multiethnic adults with coronary heart disease: from a 2005-2006 national survey. Am J Cardiovasc Drugs. 2010;10:109–14. doi: 10.2165/11535240-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 7.Selvin E, Parrinello CM, Sacks DB, Coresh J. Trends in prevalence and control of diabetes in the United States, 1988-1994 and 1999-2010. Ann Intern Med. 2014;160:517–25. doi: 10.7326/M13-2411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schneider EC, Zaslavsky AM, Epstein AM. Racial disparities in the quality of care for enrollees in Medicare managed care. JAMA. 2002;287:1288–94. doi: 10.1001/jama.287.10.1288. [DOI] [PubMed] [Google Scholar]
- 9.Trivedi AN, Zaslavsky AM, Schneider EC, Ayanian JZ. Trends in the quality of care and racial disparities in Medicare managed care. N Engl J Med. 2005;353:692–700. doi: 10.1056/NEJMsa051207. [DOI] [PubMed] [Google Scholar]
- 10.Trivedi AN, Zaslavsky AM, Schneider EC, Ayanian JZ. Relationship between quality of care and racial disparities in Medicare health plans. JAMA. 2006;296:1998–2004. doi: 10.1001/jama.296.16.1998. [DOI] [PubMed] [Google Scholar]
- 11.Arday SL, Arday DR, Monroe S, Zhang J. HCFA's racial and ethnic data: current accuracy and recent improvements. Health Care Financ Rev. 2000;21:107–16. [PMC free article] [PubMed] [Google Scholar]
- 12.Zaslavsky AM, Ayanian JZ, Zaborski LB. The validity of race and ethnicity in enrollment data for Medicare beneficiaries. Health Serv Res. 2012;47:1300–21. doi: 10.1111/j.1475-6773.2012.01411.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Agency for Healthcare Research and Quality. Creation of new race-ethnicity codes and socioeconomic status (SES) indicators for Medicare beneficiaries: final report. 2012 http://www.ahrq.gov/research/findings/final-reports/medicareindicators/index.html.
- 14.Reed M, Huang J, Graetz I, et al. Outpatient electronic health records and the clinical care and outcomes of patients with diabetes mellitus. Ann Intern Med. 2012;157:482–9. doi: 10.7326/0003-4819-157-7-201210020-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jaffe MG, Lee GA, Young JD, Sidney S, Go AS. Improved blood pressure control associated with a large-scale hypertension program. JAMA. 2013;310:699–705. doi: 10.1001/jama.2013.108769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ayanian JZ, Landon BE, Zaslavsky AM, Newhouse JP. Racial and ethnic differences in use of mammography between Medicare Advantage and traditional Medicare. J Natl Cancer Inst. 2013;105:1891–6. doi: 10.1093/jnci/djt333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ayanian JZ, Landon BE, Zaslavsky AM, Saunders RC, Pawlson LG, New-house JP. Medicare beneficiaries more likely to receive appropriate ambulatory services in HMOs than in traditional Medicare. Health Aff (Millwood) 2013;32:1228–35. doi: 10.1377/hlthaff.2012.0773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Committee for Quality Assurance. Volume 2: technical specifications. Washington, DC: National Committee for Quality Assurance; 2012. HEDIS 2012. [Google Scholar]
- 19.Gerstein HC, Miller ME, Byington RP, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358:2545–59. doi: 10.1056/NEJMoa0802743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sequist TD, Adams AS, Zhang F, Ross-Degnan D, Ayanian JZ. Effect of quality improvement on racial disparities in diabetes care. Arch Intern Med. 2006;166:675–81. doi: 10.1001/archinte.166.6.675. [DOI] [PubMed] [Google Scholar]
- 21.Trivedi AN, Grebla RC, Wright SM, Washington DL. Despite improved quality of care in the Veterans Affairs health system, racial disparity persists for important clinical outcomes. Health Aff (Millwood) 2011;30:707–15. doi: 10.1377/hlthaff.2011.0074. [DOI] [PubMed] [Google Scholar]
- 22.McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Differences in control of cardiovascular disease and diabetes by race, ethnicity, and education: U.S. trends from 1999 to 2006 and effects of Medicare coverage. Ann Intern Med. 2009;150:505–15. doi: 10.7326/0003-4819-150-8-200904210-00005. [DOI] [PubMed] [Google Scholar]
- 23.Zhou YY, Kanter MH, Wang JJ, Garri-do T. Improved quality at Kaiser Permanente through e-mail between physicians and patients. Health Aff (Millwood) 2010;29:1370–5. doi: 10.1377/hlthaff.2010.0048. [DOI] [PubMed] [Google Scholar]
- 24.Reed M, Huang J, Brand R, et al. Implementation of an outpatient electronic health record and emergency department visits, hospitalizations, and office visits among patients with diabetes. JAMA. 2013;310:1060–5. doi: 10.1001/jama.2013.276733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362:2155–65. doi: 10.1056/NEJMoa0908610. [DOI] [PubMed] [Google Scholar]
- 26.Lewey J, Shrank WH, Bowry AD, Kilabuk E, Brennan TA, Choudhry NK. Gender and racial disparities in adherence to statin therapy: a meta-analysis. Am Heart J. 2013;165:665–78. doi: 10.1016/j.ahj.2013.02.011. [DOI] [PubMed] [Google Scholar]
- 27.Brown AF, Gregg EW, Stevens MR, et al. Race, ethnicity, socioeconomic position, and quality of care for adults with diabetes enrolled in managed care: the Translating Research Into Action for Diabetes (TRIAD) study. Diabetes Care. 2005;28:2864–70. doi: 10.2337/diacare.28.12.2864. [DOI] [PubMed] [Google Scholar]
- 28.Heisler M, Faul JD, Hayward RA, Langa KM, Blaum C, Weir D. Mechanisms for racial and ethnic disparities in glycemic control in middle-aged and older Americans in the Health and Retirement Study. Arch Intern Med. 2007;167:1853–60. doi: 10.1001/archinte.167.17.1853. [DOI] [PubMed] [Google Scholar]
- 29.Kaiser Family Foundation. Medicare Part D prescription drug plans: the marketplace in 2013 and key trends, 2006-2013. 2013 http://kaiserfamilyfoundation.files.wordpress.com/2013/12/8524-medicare-part-d-pdp-marketplace-2013-and-trends1.pdf.
- 30.Zhang YDJ, Donohue JM, Lave JR, O'Donnell G, Newhouse JP. The effect of Medicare Part D on drug and medical spending. N Engl J Med. 2009;361:52–61. doi: 10.1056/NEJMsa0807998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li PMS, McElligott S, Bergquist H, Schwartz JS, Doshi JA. Effect of the Medicare Part D coverage gap on medication use among patients with hypertension and hyperlipidemia. Ann Intern Med. 2012;156:776–84. doi: 10.7326/0003-4819-156-11-201206050-00004. [DOI] [PubMed] [Google Scholar]
- 32.August KJ, Sorkin DH. Racial/ethnic disparities in exercise and dietary behaviors of middle-aged and older adults. J Gen Intern Med. 2011;26:245–50. doi: 10.1007/s11606-010-1514-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311:507–20. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 34.Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(Suppl 2):S1–S45. doi: 10.1161/01.cir.0000437738.63853.7a. [DOI] [PubMed] [Google Scholar]
- 35.Centers for Medicare and Medicaid Services. Quality measures and performance standards. http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Quality_Measures_Standards.html.
- 36.Jones RG, Trivedi AN, Ayanian JZ. Factors influencing the effectiveness of interventions to reduce racial and ethnic disparities in health care. Soc Sci Med. 2010;70:337–41. doi: 10.1016/j.socscimed.2009.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Thorlby R, Jorgensen S, Siegel B, Ayanian JZ. How health care organizations are using data on patients' race and ethnicity to improve quality of care. Milbank Q. 2011;89:226–55. doi: 10.1111/j.1468-0009.2011.00627.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.