Abstract
The objective of this study was to critically review the empirical evidence from all relevant disciplines regarding obesity stigma in order to (i) determine the implications of obesity stigma for healthcare providers and their patients with obesity and (ii) identify strategies to improve care for patients with obesity. We conducted a search of Medline and PsychInfo for all peer-reviewed papers presenting original empirical data relevant to stigma, bias, discrimination, prejudice and medical care. We then performed a narrative review of the existing empirical evidence regarding the impact of obesity stigma and weight bias for healthcare quality and outcomes. Many healthcare providers hold strong negative attitudes and stereotypes about people with obesity. There is considerable evidence that such attitudes influence person-perceptions, judgment, interpersonal behaviour and decision-making. These attitudes may impact the care they provide. Experiences of or expectations for poor treatment may cause stress and avoidance of care, mistrust of doctors and poor adherence among patients with obesity. Stigma can reduce the quality of care for patients with obesity despite the best intentions of healthcare providers to provide high-quality care. There are several potential intervention strategies that may reduce the impact of obesity stigma on quality of care.
Keywords: Delivery of health care, obesity, stereotyping, social stigma
Introduction
The goal of primary care is to improve patients' health, longevity and quality of life through the provision of patient-centred care. To do so, healthcare providers must identify modifiable behaviours that increase disease risk, and help patients change them. Recent US Preventive Services Task Force guidelines recommend screening adults for obesity and offering behavioural interventions to those with a body mass index (BMI) over 30 kg m−2 (1). However, obesity is a stigmatized condition; thus, one side effect of increased focus on body weight in health care may be the alienation and humiliation of these patients. The term ‘stigma’ describes physical characteristics or character traits that mark the bearer as having lower social value (2). A stigmatized trait can lead to experiences of discrimination, and the feeling of being stigmatized can put one at risk for low self-esteem (3), depression (4–6) and lower quality of life (7–10). However, the empirical evidence on stigma overall and obesity stigma in particular is scattered across diverse disciplines and lines of research, making it difficult to get a clear picture of the implication of obesity stigma for healthcare providers and their patients.
In order to address this gap, we critically reviewed literature related to the impact of obesity stigma on interpersonal encounters and decision-making. We discuss potential implications, including several mechanisms whereby stigma may affect patient-centred communication and care, defined by the Institute of Medicine (11) as ‘care that establishes a partnership among practitioners, patients, and their families (when appropriate) to ensure that decisions respect patients' wants, needs, and preferences and that patients have the education and support they need to make decisions and participate in their own care’ (p. 7). We also suggest several strategies that may help healthcare providers and clinics reduce the impact of stigma on patients with obesity.
Obesity is a commonly and strongly stigmatized characteristic (12,13). There is substantial empirical evidence that people with obesity elicit negative feelings such as disgust, anger, blame and dislike in others (14–16). Despite the high prevalence of obesity (approximately one-third of the US adult population (17) ), individuals with obesity are frequently the targets of prejudice, derogatory comments and other poor treatment in a variety of settings, including health care (12,18). Furthermore, there is a growing body of evidence that physicians and other healthcare professionals hold strong negative opinions about people with obesity (19–27).
Methods
We conducted a narrative review of this literature to highlight the ways that the obesity stigma may interrupt the healthcare process and impede many healthcare providers' goal of providing equitable high-quality care. We reviewed all original studies in the fall of 2014 on topics related to obesity stigma in medical care and/or the impact of stigma on interpersonal encounters and decision-making in PubMed and PsychInfo, with the majority of studies found in health communication, social psychology and health disparities research. We then selected papers relevant to the potential impact of obesity stigma on healthcare provider behaviour, patient healthcare outcomes and healthcare encounters.
Impact on providers
Primary care providers and health promotion specialists, who typically demonstrate a commitment to providing care for underserved populations, are unlikely to flagrantly and intentionally discriminate against their patients. Nevertheless, there are several ways that their attitudes about obesity may cause their patients with obesity to feel disrespected, inadequate or unwelcome, thus negatively affecting the encounter quality and their willingness to seek needed care (see Fig. 1). Behaviours that emanate from negative attitudes about a stigmatized group are known as enacted stigma (28). Enacted stigma on the part of the provider affects the patient in both measurable and immeasurable ways. It can reduce the quality, and even the quantity, of patient-centred care, and can signal to the patient that he or she is being perceived in terms of his or her stigmatized identity, which, in turn, may affect patient perception of, and compliance with, provider recommendations.
Figure 1.
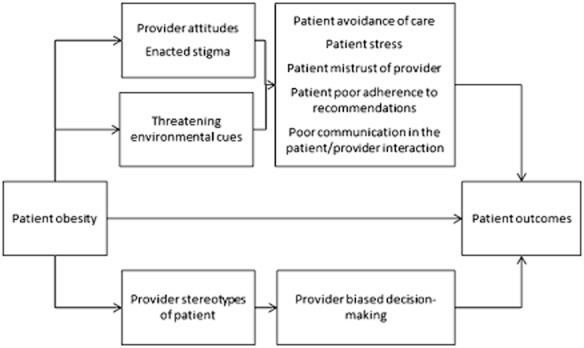
A conceptual model of hypothesized pathways whereby the associations between obesity and health outcomes are partially mediated by healthcare providers' attitudes and behaviours about obese patients, and patients' response to feeling stigmatized.
The negative attitudes underlying enacted stigma can be explicit or implicit. Explicit attitudes are conscious and reflect a person's opinions or beliefs about a group. Implicit attitudes are automatic and often occur outside of awareness and in contrast to explicitly held beliefs (29). The response to some stigmatized groups, such as racial minorities among egalitarian Caucasians, often consists of negative implicit attitudes, but neutral or positive explicit ones (30). In contrast, explicit negative attitudes about people with obesity are more socially acceptable than explicit racism: e.g. it is acceptable in many Western cultures that people with obesity are the source of derogatory humour and may thus be openly – and unquestionably – portrayed as lazy, gluttonous and undisciplined. Primary care providers, medical trainees, nurses and other healthcare professionals hold explicit as well as implicit negative opinions about people with obesity (21,31–33). This has important implications for communication in the clinical interview, because explicit attitudes influence verbal behaviours as well as decisions that are within conscious control, whereas implicit negative attitudes predict non-verbal communication and decisions under cognitive burden (29,34–36). There is evidence that providers' communication is less patient-centred with members of stigmatized racial groups (37–43), and other stigmatized groups including patients with obesity (44), and that provider attitudes contribute to this disparity (45–47). Implicit attitudes have also been found to be associated with lower patient ratings of care (46). The combination of implicit and explicit negative obesity attitudes may elevate the potential for impaired patient-centred communication, which is associated with a 19% higher risk of patient non-adherence, as well as mistrust, and worse patient weight loss, recovery and mental health outcomes (48–53).
There are several mechanisms by which provider attitudes may affect the quality of, or potential for, patient-centred care. First, primary care providers engage in less patient-centred communication with patients they believe are not likely to be adherent (54). A common explicitly endorsed provider stereotype about patients with obesity is that they are less likely to be adherent to treatment or self-care recommendations (23,24,55,56), are lazy, undisciplined and weak-willed (12,55,57–59). Second, primary care providers have reported less respect for patients with obesity compared with those without (59,60), and low respect has been shown to predict less positive affective communication and information giving (61). Third, primary healthcare providers may allocate time differently, spending less time educating patients with obesity about their health (62). For example, in one study of primary care providers randomly assigned to evaluate the records of patients who were either obese or normal weight, providers who evaluated patients who were obese were more likely to rate the encounter as a waste of time and indicated that they would spend 28% less time with the patient compared with those who evaluated normal-weight patients (59). Finally, physicians may over-attribute symptoms and problems to obesity, and fail to refer the patient for diagnostic testing or to consider treatment options beyond advising the patient to lose weight. In one study involving medical students, virtual patients with shortness of breath were more likely to receive lifestyle change recommendations if they were obese (54% vs. 13%), and more likely to receive medication to manage symptoms if they were normal weight (23% vs. 5%) (23).
Impact on patients
Experiences of discrimination and awareness of stigmatized social status can cause patients to experience stress and have other acute reactions that may reduce the quality of the encounter, regardless of their provider's attitudes and behaviour. Three conceptually overlapping processes – identity threat, stereotype threat and felt stigma – describe the stigmatized patient's reaction to being stigmatized. Identity threat occurs when patients experience situations that make them feel devalued because of a social identity. Social identities are the categories, roles, and social groups that define each person and give a sense of self (63,64). Each social identity, be it a professional identity, a gender identity, or identity as a person who is obese, has emotional significance for the individual, is closely tied to self-esteem, and can empower or make one vulnerable. Obesity is stigmatized, and thus is more likely to make the individual aware of the possibility for rejection or derogation than make him/her feel confident and empowered. Stereotype threat occurs when an individual is aware that he or she may be viewed as a member of a stigmatized group, and becomes preoccupied with detecting stereotyping on the part of the provider and monitoring his or her own behaviour to ensure that it does not confirm group stereotypes (65). Felt stigma is a term used to describe the expectation of poor treatment based on past experiences of discrimination (28).
The effects of stigma are both immediate and long-term. The direct effects of provider attitudes on patient-centred care may reduce the quality of the patient encounter, harming patient outcomes and reducing patient satisfaction. Patients with obesity who experience identity/stereotype threat or felt/enacted stigma may experience a high level of stress which can contribute to impaired cognitive function and ability to effectively communicate (66). Accumulated exposure to high levels of stress hormones (allostatic load) has several long-term physiological health effects, including heart disease, stroke, depression and anxiety disorder, diseases that disproportionately affect obese individuals and have been empirically linked to perceived discrimination (67–69). Indeed, stress pathways may present an alternate explanation for some proportion of the association between obesity and chronic disease (70).
Other effects include avoidance of clinical care if patients perceive that their body weight will be a source of embarrassment in that setting (71,72). For example, there is evidence that obese women are less likely to seek recommended screening for some cancers (72–76). The long-term result of avoidance and postponement of care is that people with obesity may present with more advanced, and thus more difficult to treat, conditions. Individuals who are stigmatized, or are vigilant for evidence of stigma, may withdraw from full participation in the encounter. Because of this, they may not recall advice or instructions given by the provider, reducing adherence to prescribed treatment or self-care. Experiencing stereotype threat may also cause patients to discount feedback provided by the source of the threat (77), which in turn may affect adherence. Patients who report feeling judged by their primary care provider are less likely to seek or achieve successful weight loss (78,79). Patients who have tried to lose weight and failed may ‘dis-identify’, or reduce their efforts to lose weight, in order to disconnect their self-esteem from achievement in a domain with which they have not had success (65), and may feel shame for failing to lose weight or maintain weight loss (78). Along similar lines, individuals who experience more obesity stigma report less health utility, or place lower value on health (80).
Setting factors
Felt stigma and identity/stereotype threat can be triggered by experiences in the healthcare clinical setting that signal to the patient that his/her identity as a person who is obese is salient and possibly devalued. A typical primary care clinical encounter has many such signals, including weight measurement, dietary assessment, and queries about physical activity. Providers are also encouraged to provide unsolicited weight loss counsel as well as to assess patients' willingness to alter behaviours that are associated with obesity. There is evidence that many providers dislike treating obesity, feel underprepared to do so, and have little hope that their patients will make lifestyle changes (55,81–84), which may be detectable in their tone of voice or language. They may also signal overly simplified assumptions about the causes of obesity, by suggesting, for example, that their patients cut back on fast food or consider taking the stairs instead of elevators. These assumptions ignore the complexity of energy balance and propagate a common misunderstanding that weight loss is as simple as ‘calories in < calories out’ (85). Such counsel, despite its positive intentions to optimize patient health, may create unrealistic expectations about the effects of small lifestyle changes, which may lead to disappointment and recidivism. This counsel can also have unintended side effects if it signals to patients that they are seen solely in terms of their stigmatized identity. This could create a state of threat that may affect the patient's emotional state, ability to communicate effectively, and attitude towards medical advice (86).
Clinic equipment may also promote identity threat for patients with obesity (87,88). Waiting room chairs with armrests can be uncomfortable or too small. Equipment such as scales, blood pressure cuffs, examination gowns and pelvic examination instruments are often designed for use with smaller patients. When larger alternatives are not available, or are stored in a place that suggests infrequent use, it can signal to patients that their size is unusual and that they do not belong. These experiences, which are not delivered with malicious intent, can be humiliating.
Potential strategies to address obesity stigma in clinical care
Promising strategies to reduce stigma in the primary care setting include improving provider attitudes about patients with obesity and/or reducing the likelihood that negative attitudes influence provider behaviour; altering the clinic environment or procedures to create a setting where patients with obesity feel accepted and less threatened; and empowering patients to cope with stigmatizing situations and attain high-quality health care (86,89). Here we focus on strategies that clinics or healthcare organizations might implement to improve the experience of patients with obesity or overweight. Some of the studies discussed here are firmly rooted in research evidence, but some are untested strategies that will require research to test their effectiveness.
Our intent was to highlight the salience of obesity stigma in health care and the potential to re-frame and optimize provider–patient encounters. Our work recognizes the contributions of interdisciplinary scholars, in fat studies and elsewhere, who have raised awareness of how cultures conceptualize body size, and consequently, how body size itself can inform identity. Such scholars have thus set much of the theoretical foundation for our work, even though our suggestions are not consistent with their advocacy for a weight-inclusive approach to medical care, in which obesity is seen as independent of health and weight reduction is not a focus of medical care (90,91). While there is evidence supporting this viewpoint, we focus on interventions that are more consistent with the dominant medical and nursing paradigms of obesity as a risk factor.
Reducing weight stigma in clinical care is a shared responsibility of healthcare providers and other clinic staff, as well as the healthcare systems/organizations that have the power to implement intervention strategies broadly. Many of the strategies we discuss here can be implemented by providers or clinics, but any of these strategies could be implemented more efficiently, and have a wider influence, if uptake was required of providers and clinic staff by healthcare organizations.
Strategies that clinics can implement to improve provider attitudes about people with obesity include the following. (i) Increase provider empathy through perspective-taking exercises. Perspective-taking exercises have improved provider attitudes towards stigmatized groups (92), although findings are mixed about its effectiveness in reducing obesity stigma (93,94). (ii) Alter perceived norms regarding negative attitudes and stereotypes about people with obesity. In one study, researchers reduced explicit bias against obese people by providing individuals information and evidence that their peers did not hold negative attitudes (95). To minimize the perception that anti-fat bias is the norm, one untested strategy could include implementing a zero-tolerance policy for comments or humour that stereotypes or degrades anyone based on a physical identity or attribute. (iii) Encourage provider instruction and practice in emotion regulation techniques that foster positive affect. High cognitive load and time pressure, characteristic of clinical care settings, impair judgments and decision-making (96). Furthermore, frustration that providers may feel towards ‘difficult’ or ‘complex’ patients or patients who they perceive are harming their own health, may elicit strong negative emotions. Although no studies have directly tested their effect on weight bias, evidence from one study of prejudice reduction suggests that emotion regulation tools such as meditation or deep breathing may help providers overcome these negative emotions and improve compassion and other pro-social emotions (97,98). (iv) An untested strategy to build awareness of weight bias and a felt need to address it might include encouraging providers to examine their explicit beliefs and stereotypes about obese people, and complete an assessment of implicit attitudes (e.g. the online Implicit Association Test at http://www.implicit.harvard.edu). Provide information about the automatic nature of these attitudes and encourage providers to consciously strive to behave in ways consistent with helping and egalitarian values. And lastly, (v) educate providers on the genetic, environmental, biological, psychological and social contributors to weight gain and loss (99,100). Providers who understand this complex web of causality have more positive attitudes about patients with obesity (101). This information is likely less threatening for their patients than over-simplified messages like ‘eat less, move more’, or ‘calories in, calories out’ (102).
There are several strategies for providing a welcoming and less threatening healthcare environment to patients with obesity. (i) Reduce focus on body weight. Instead, focus on screening for the diseases and conditions for which obesity is a risk factor and encourage feasible behaviours that will improve health and well-being. This could be accomplished by weighing patients less frequently – for example, restricting weigh-ins to well-visit checkups and forgoing weigh-ins when visits are not associated with a weight-related reason. Increasing patients' knowledge of the health effects of obesity has shown little effect on weight loss (103,104). However, encouraging patients to not focus on weight or weight loss, but rather on the other benefits of physical activity and healthy eating, may reduce the threat of conversations about these behaviours, and thus increase the likelihood of behaviour change and maintenance (102,105). (ii) Adopt patient-centred communication strategies, such as motivational interviewing, which may be less threatening for patients and are associated with patient adherence and positive outcomes (48,51–53,106–108). (iii) Although its impact on felt stigma is not tested, one could ensure that the clinic environment is welcoming by providing chairs and medical equipment that are usable by patients of all sizes and by keeping specialized instruments for patients with obesity readily available to clinical staff. (iv) Convey a sense of identity safety by providing evidence that diversity is valued (109). Although untested, this could be accomplished by posting a mission statement that stresses the value of body size diversity or by using positive and non-stereotypical images of overweight and obese people in clinic advertisements, pamphlets or artwork. (v) Healthcare systems could ensure that the continuum of care includes adequate referral resources for behaviour change counselling, including providers or clinics specializing in weight loss strategies and remove barriers (e.g. requirement for a secondary diagnosis, long wait times for an appointment) to accessing these resources (78). Study is needed in this area to determine whether shifting the threat of discussing weight loss strategies from the primary care setting to a specialty care setting may improve utilization of primary health care. These providers may also be more skilled at using communication strategies that are not threatening.
Discussion
Healthcare providers strive to provide the highest quality health care for their patients. This effort may be hindered by interpersonal and environmental cues that convey that patients with obesity are not welcome or by behaviours that lower the quality of communication in the encounter. Attitudes towards obesity as a health risk factor can exacerbate and mask negative attitudes towards individuals with obesity. Healthcare providers often view obesity as an avoidable risk factor that impedes their ability to treat and prevent disease. As this is a largely unchallenged perspective on obesity, healthcare providers may be less self-aware of their propensity to, and feel less pressure (internally or from external sources) to, behave in a non-prejudicial way towards people with obesity.
A great deal more research is needed to understand the impact of stigma on care for people with obesity. Much of the extant research involves small or convenience samples and requires replication with more generalizable populations. There are several important gaps in the literature on weight bias and health care. While several studies have found high levels of explicit bias in healthcare providers, there is a need for more research on weight stigma using measures of implicit bias. More research is also needed to identify the impact of those attitudes on aspects of the medical encounter, including decision-making and communication, as well as the differential effects of those attitudes by gender, race, socioeconomic status, sexual orientation, and other characteristics. The development and testing of novel interventions is also needed to reduce bias or its impact on behaviour in medical trainees, practicing physicians, other healthcare providers, and other staff members of healthcare organizations.
It is important to note the tension between obesity stigma literature or literature advocating a weight-inclusive approach (91) and the body of literature that supports increased provider attention to body weight and weight loss as a strategy to encourage behaviour change. We believe that the strategies and perspectives reviewed here are not contrary to this evidence, but may inform the refinement of interventions in order to avoid unintended consequences brought on by stigma, and maximize the effectiveness of patient behaviour change intervention.
Acknowledgments
Dr. Phelan is supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under Award Number K01DK095924. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interest statement
Drs. Burgess, Hellerstedt, Griffin, and van Ryn do not report any potential conflicts of interest. Dr. Phelan and Dr. Yeazel report grants from the National Institutes of Health during the conduct of the study.
References
- 1.Moyer VA, on behalf of the United States Preventive Services Task Force Screening for and management of obesity in Adults: U.S. preventive services task force recommendation statement. Ann Intern Med. 2012;157:1–32. doi: 10.7326/0003-4819-157-5-201209040-00475. [DOI] [PubMed] [Google Scholar]
- 2.Goffman E. Stigma: Notes on the Management of Spoiled Identity. Englewood Cliffs: Prentice-Hall; 1963. [Google Scholar]
- 3.Link BG, Struening EL, Neese-Todd S, Asmussen S, Phelan JC. Stigma as a barrier to recovery: the consequences of stigma for the self-esteem of people with mental illnesses. Psychiatr Serv. 2001;52:1621–1626. doi: 10.1176/appi.ps.52.12.1621. [DOI] [PubMed] [Google Scholar]
- 4.Phelan SM, Griffin JM, Jackson GL, et al. Stigma, perceived blame, self-blame, and depressive symptoms in men with colorectal cancer. Psychooncology. 2013;22:65–73. doi: 10.1002/pon.2048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Phelan SM, Griffin JM, Hellerstedt WL, et al. Perceived stigma, strain, and mental health among caregivers of veterans with traumatic brain injury. Disabil Health J. 2011;4:177–184. doi: 10.1016/j.dhjo.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 6.Li L, Lee SJ, Thammawijaya P, Jiraphongsa C, Rotheram-Borus MJ. Stigma, social support, and depression among people living with HIV in Thailand. AIDS Care. 2009;21:1007–1013. doi: 10.1080/09540120802614358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Markowitz FE. The effects of stigma on the psychological well-being and life satisfaction of persons with mental illness. J Health Soc Behav. 1998;39:335–347. [PubMed] [Google Scholar]
- 8.Major B, O'Brien LT. The social psychology of stigma. Annu Rev Psychol. 2005;56:393–421. doi: 10.1146/annurev.psych.56.091103.070137. [DOI] [PubMed] [Google Scholar]
- 9.Link BG, Phelan JC. Stigma and its public health implications. Lancet. 2006;367:528–529. doi: 10.1016/S0140-6736(06)68184-1. [DOI] [PubMed] [Google Scholar]
- 10.Myers A, Rosen JC. Obesity stigmatization and coping: relation to mental health symptoms, body image, and self-esteem. Int J Obes Relat Metab Disord. 1999;23:221–230. doi: 10.1038/sj.ijo.0800765. [DOI] [PubMed] [Google Scholar]
- 11.Committee on the National Quality Report on Health Care Delivery. Envisioning the national health care quality report. In: Hurtado MP, Swift EK, Corrigan JM, editors. Board on Health Care Services. Washington, DC: National Academy Press; 2001. p. 256. [PubMed] [Google Scholar]
- 12.Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity (Silver Spring) 2009;17:941–964. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- 13.Latner JD, O'Brien KS, Durso LE, Brinkman LA, MacDonald T. Weighing obesity stigma: the relative strength of different forms of bias. Int J Obes (Lond) 2008;32:1145–1152. doi: 10.1038/ijo.2008.53. [DOI] [PubMed] [Google Scholar]
- 14.Vartanian LR. Disgust and perceived control in attitudes toward obese people. Int J Obes (Lond) 2010;34:1302–1307. doi: 10.1038/ijo.2010.45. [DOI] [PubMed] [Google Scholar]
- 15.Crandall CS. Prejudice against fat people: ideology and self-interest. J Pers Soc Psychol. 1994;66:882–894. doi: 10.1037//0022-3514.66.5.882. [DOI] [PubMed] [Google Scholar]
- 16.Puhl RM, Brownell KD. Psychosocial origins of obesity stigma: toward changing a powerful and pervasive bias. Obes Rev. 2003;4:213–227. doi: 10.1046/j.1467-789x.2003.00122.x. [DOI] [PubMed] [Google Scholar]
- 17.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 18.Wear D, Aultman JM, Varley JD, Zarconi J. Making fun of patients: medical students' perceptions and use of derogatory and cynical humor in clinical settings. Acad Med. 2006;81:454–462. doi: 10.1097/01.ACM.0000222277.21200.a1. [DOI] [PubMed] [Google Scholar]
- 19.Puhl RM, Luedicke J, Grilo CM. Obesity bias in training: attitudes, beliefs, and observations among advanced trainees in professional health disciplines. Obesity (Silver Spring) 2014;22:1008–1015. doi: 10.1002/oby.20637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tomiyama AJ, Finch LE, Incollingo Belsky AC, et al. Weight bias in 2001 versus 2013: contradictory attitudes among obesity researchers and health professionals. Obesity (Silver Spring) 2014;23:46–53. doi: 10.1002/oby.20910. [DOI] [PubMed] [Google Scholar]
- 21.Phelan SM, Dovidio JF, Puhl RM, et al. Implicit and explicit weight bias in a national sample of 4,732 medical students: the medical student CHANGES study. Obesity (Silver Spring) 2013;22:1201–1208. doi: 10.1002/oby.20687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hebl MR, Xu J, Mason MF. Weighing the care: patients' perceptions of physician care as a function of gender and weight. Int J Obes Relat Metab Disord. 2003;27:269–275. doi: 10.1038/sj.ijo.802231. [DOI] [PubMed] [Google Scholar]
- 23.Persky S, Eccleston CP. Medical student bias and care recommendations for an obese versus non-obese virtual patient. Int J Obes (Lond) 2010;35:728–735. doi: 10.1038/ijo.2010.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Puhl R, Wharton C, Heuer C. Weight bias among dietetics students: implications for treatment practices. J Am Diet Assoc. 2009;109:438–444. doi: 10.1016/j.jada.2008.11.034. [DOI] [PubMed] [Google Scholar]
- 25.Wigton RS, McGaghie WC. The effect of obesity on medical students' approach to patients with abdominal pain. J Gen Intern Med. 2001;16:262–265. doi: 10.1046/j.1525-1497.2001.016004262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Neumark-Sztainer D, Story M, Harris T. Beliefs and attitudes about obesity among teachers and school health care providers working with adolescents. J Nutr Educ. 1999;31:3–9. [Google Scholar]
- 27.Robertson N, Vohora R. Fitness vs. fatness: implicit bias toward obesity among fitness professionals and regular exercisers. Psychol Sport Exerc. 2008;9:547–557. [Google Scholar]
- 28.Jacoby A. Felt versus enacted stigma: a concept revisited. Evidence from a study of people with epilepsy in remission. Soc Sci Med. 1994;38:269–274. doi: 10.1016/0277-9536(94)90396-4. [DOI] [PubMed] [Google Scholar]
- 29.Dovidio J, Kawakami K, Johnson C, Johnson B, Howard A. On the nature of prejudice: automatic and controlled processes. J Exp Soc Psychol. 1997;33:510–540. [Google Scholar]
- 30.Gaertner SL, Dovidio JF. The aversive form of racism. In: Dovidio JF, Gaertner SL, editors. Prejudice, Discrimination, and Racism. Orlando, FL: Academic Press; 1986. pp. 61–89. [Google Scholar]
- 31.Schwartz MB, Chambliss HO, Brownell KD, Blair SN, Billington C. Weight bias among health professionals specializing in obesity. Obes Res. 2003;11:1033–1039. doi: 10.1038/oby.2003.142. [DOI] [PubMed] [Google Scholar]
- 32.Teachman BA, Brownell KD. Implicit anti-fat bias among health professionals: is anyone immune? Int J Obes Relat Metab Disord. 2001;25:1525–1531. doi: 10.1038/sj.ijo.0801745. [DOI] [PubMed] [Google Scholar]
- 33.Budd GM, Mariotti M, Graff D, Falkenstein K. Health care professionals' attitudes about obesity: an integrative review. Appl Nurs Res. 2009;24:127–137. doi: 10.1016/j.apnr.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 34.Dovidio JF, Penner LA, Albrecht TL, Norton WE, Gaertner SL, Shelton JN. Disparities and distrust: the implications of psychological processes for understanding racial disparities in health and health care. Soc Sci Med. 2008;67:478–486. doi: 10.1016/j.socscimed.2008.03.019. [DOI] [PubMed] [Google Scholar]
- 35.Greenwald AG, Poehlman TA, Uhlmann EL, Banaji MR. Understanding and using the Implicit Association Test: III. Meta-analysis of predictive validity. J Pers Soc Psychol. 2009;97:17–41. doi: 10.1037/a0015575. [DOI] [PubMed] [Google Scholar]
- 36.Dovidio J, Kawakami K, Gaertner S. Implicit and explicit prejudice and interracial interaction. J Pers Soc Psychol. 2002;82:62–68. doi: 10.1037//0022-3514.82.1.62. [DOI] [PubMed] [Google Scholar]
- 37.Gordon HS, Street RL, Jr, Sharf BF, Kelly PA, Souchek J. Racial differences in trust and lung cancer patients' perceptions of physician communication. J Clin Oncol. 2006;24:904–909. doi: 10.1200/JCO.2005.03.1955. [DOI] [PubMed] [Google Scholar]
- 38.Gordon HS, Street RL, Jr, Sharf BF, Souchek J. Racial differences in doctors' information-giving and patients' participation. Cancer. 2006;107:1313–1320. doi: 10.1002/cncr.22122. [DOI] [PubMed] [Google Scholar]
- 39.Ghods BK, Roter DL, Ford DE, Larson S, Arbelaez JJ, Cooper LA. Patient-physician communication in the primary care visits of African Americans and whites with depression. J Gen Intern Med. 2008;23:600–606. doi: 10.1007/s11606-008-0539-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cene CW, Roter D, Carson KA, Miller ER, III, Cooper LA. The effect of patient race and blood pressure control on patient–physician communication. J Gen Intern Med. 2009;24:1057–1064. doi: 10.1007/s11606-009-1051-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Beach MC, Saha S, Korthuis PT, et al. Differences in patient-provider communication for Hispanic compared to non-Hispanic white patients in HIV care. J Gen Intern Med. 2010;25:682–687. doi: 10.1007/s11606-010-1310-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Beach MC, Saha S, Korthuis PT, et al. Patient–provider communication differs for Black compared to White HIV-infected patients. AIDS Behav. 2010;15:805–811. doi: 10.1007/s10461-009-9664-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Johnson RL, Roter D, Powe NR, Cooper LA. Patient race/ethnicity and quality of patient–physician communication during medical visits. Am J Public Health. 2004;94:2084–2090. doi: 10.2105/ajph.94.12.2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gudzune KA, Beach MC, Roter DL, Cooper LA. Physicians build less rapport with obese patients. Obesity (Silver Spring) 2013;21:2146–2152. doi: 10.1002/oby.20384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cooper L. Overcoming Healthcare Disparities: The Role of Patient-Centered Care. College of Public Health and Health Professions Celebrating 50 Years. Gainesville: University of Florida; 2008. [Google Scholar]
- 46.Penner LA, Dovidio JF, West TV, et al. Aversive racism and medical interactions with black patients: a field study. J Exp Soc Psychol. 2010;46:436–440. doi: 10.1016/j.jesp.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cooper L, Roter D, Carson K, et al. The associations of clinicians' implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J Public Health. 2012;102:979–987. doi: 10.2105/AJPH.2011.300558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Armstrong MJ, Mottershead TA, Ronksley PE, Sigal RJ, Campbell TS, Hemmelgarn BR. Motivational interviewing to improve weight loss in overweight and/or obese patients: a systematic review and meta-analysis of randomized controlled trials. Obes Rev. 2011;12:709–723. doi: 10.1111/j.1467-789X.2011.00892.x. [DOI] [PubMed] [Google Scholar]
- 49.Jay M, Gillespie C, Schlair S, Sherman S, Kalet A. Physicians' use of the 5As in counseling obese patients: is the quality of counseling associated with patients' motivation and intention to lose weight? BMC Health Serv Res. 2010;10:159. doi: 10.1186/1472-6963-10-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zolnierek KB, Dimatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47:826–834. doi: 10.1097/MLR.0b013e31819a5acc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fiscella K, Meldrum S, Franks P, et al. Patient trust: is it related to patient-centered behavior of primary care physicians? Med Care. 2004;42:1049–1055. doi: 10.1097/00005650-200411000-00003. [DOI] [PubMed] [Google Scholar]
- 52.Wanzer MB, Booth-Butterfield M, Gruber K. Perceptions of health care providers' communication: relationships between patient-centered communication and satisfaction. Health Commun. 2004;16:363–383. doi: 10.1207/S15327027HC1603_6. [DOI] [PubMed] [Google Scholar]
- 53.Stewart M, Brown JB, Donner A, et al. The impact of patient-centered care on outcomes. J Fam Pract. 2000;49:796–804. [PubMed] [Google Scholar]
- 54.Street RL, Jr, Gordon H, Haidet P. Physicians' communication and perceptions of patients: is it how they look, how they talk, or is it just the doctor? Soc Sci Med. 2007;65:586–598. doi: 10.1016/j.socscimed.2007.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Foster GD, Wadden TA, Makris AP, et al. Primary care physicians' attitudes about obesity and its treatment. Obes Res. 2003;11:1168–1177. doi: 10.1038/oby.2003.161. [DOI] [PubMed] [Google Scholar]
- 56.Huizinga MM, Bleich SN, Beach MC, Clark JM, Cooper LA. Disparity in physician perception of patients' adherence to medications by obesity status. Obesity (Silver Spring) 2010;18:1932–1937. doi: 10.1038/oby.2010.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Harvey EL, Hill AJ. Health professionals' views of overweight people and smokers. Int J Obes Relat Metab Disord. 2001;25:1253–1261. doi: 10.1038/sj.ijo.0801647. [DOI] [PubMed] [Google Scholar]
- 58.Puhl R, Brownell K. Bias, discrimination, and obesity. Obes Res. 2001;9:788–805. doi: 10.1038/oby.2001.108. [DOI] [PubMed] [Google Scholar]
- 59.Hebl MR, Xu J. Weighing the care: physicians' reactions to the size of a patient. Int J Obes Relat Metab Disord. 2001;25:1246–1252. doi: 10.1038/sj.ijo.0801681. [DOI] [PubMed] [Google Scholar]
- 60.Huizinga MM, Cooper LA, Bleich SN, Clark JM, Beach MC. Physician respect for patients with obesity. J Gen Intern Med. 2009;24:1236–1239. doi: 10.1007/s11606-009-1104-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Beach MC, Roter DL, Wang NY, Duggan PS, Cooper LA. Are physicians' attitudes of respect accurately perceived by patients and associated with more positive communication behaviors? Patient Educ Couns. 2006;62:347–354. doi: 10.1016/j.pec.2006.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bertakis KD, Azari R. The impact of obesity on primary care visits. Obes Res. 2005;13:1615–1623. doi: 10.1038/oby.2005.198. [DOI] [PubMed] [Google Scholar]
- 63.Tajfel H. Social psychology of intergroup relations. Annu Rev Psychol. 1982;33:1–39. [Google Scholar]
- 64.Hogg MA, Terry DJ. Social identity and self-categorization processes in organizational contexts. Acad Manage Rev. 2000;25:121–140. [Google Scholar]
- 65.Steele CM. A threat in the air. How stereotypes shape intellectual identity and performance. Am Psychol. 1997;52:613–629. doi: 10.1037//0003-066x.52.6.613. [DOI] [PubMed] [Google Scholar]
- 66.Schmader T, Johns M, Forbes C. An integrated process model of stereotype threat effects on performance. Psychol Rev. 2008;115:336–356. doi: 10.1037/0033-295X.115.2.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychol Bull. 2009;135:531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. Am J Public Health. 2008;98:S29–S37. doi: 10.2105/ajph.98.supplement_1.s29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lewis TT, Everson-Rose SA, Powell LH, et al. Chronic exposure to everyday discrimination and coronary artery calcification in African–American women: the SWAN Heart Study. Psychosom Med. 2006;68:362–368. doi: 10.1097/01.psy.0000221360.94700.16. [DOI] [PubMed] [Google Scholar]
- 70.Muennig P. The body politic: the relationship between stigma and obesity-associated disease. BMC Public Health. 2008;8:128. doi: 10.1186/1471-2458-8-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Drury CA, Louis M. Exploring the association between body weight, stigma of obesity, and health care avoidance. J Am Acad Nurse Pract. 2002;14:554–561. doi: 10.1111/j.1745-7599.2002.tb00089.x. [DOI] [PubMed] [Google Scholar]
- 72.Amy NK, Aalborg A, Lyons P, Keranen L. Barriers to routine gynecological cancer screening for White and African–American obese women. Int J Obes (Lond) 2006;30:147–155. doi: 10.1038/sj.ijo.0803105. [DOI] [PubMed] [Google Scholar]
- 73.Cohen SS, Palmieri RT, Nyante SJ, et al. Obesity and screening for breast, cervical, and colorectal cancer in women: a review. Cancer. 2008;112:1892–1904. doi: 10.1002/cncr.23408. [DOI] [PubMed] [Google Scholar]
- 74.Rosen AB, Schneider EC. Colorectal cancer screening disparities related to obesity and gender. J Gen Intern Med. 2004;19:332–338. doi: 10.1111/j.1525-1497.2004.30339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Aldrich T, Hackley B. The impact of obesity on gynecologic cancer screening: an integrative literature review. J Midwifery Womens Health. 2010;55:344–356. doi: 10.1016/j.jmwh.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 76.Fontaine KR, Faith MS, Allison DB, Cheskin LJ. Body weight and health care among women in the general population. Arch Fam Med. 1998;7:381–384. doi: 10.1001/archfami.7.4.381. [DOI] [PubMed] [Google Scholar]
- 77.Cohen GL, Steele CM, Ross LD. The mentor's dilemma: providing critical feedback across the racial divide. Pers Soc Psychol Bull. 1999;25:1302–1318. [Google Scholar]
- 78.Thomas SL, Hyde J, Karunaratne A, Kausman R, Komesaroff PA. ‘They all work … when you stick to them’: a qualitative investigation of dieting, weight loss, and physical exercise, in obese individuals. Nutr J. 2008;7:34. doi: 10.1186/1475-2891-7-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Gudzune KA, Bennett WL, Cooper LA, Bleich SN. Perceived judgment about weight can negatively influence weight loss: a cross-sectional study of overweight and obese patients. Prev Med. 2014;62:103–107. doi: 10.1016/j.ypmed.2014.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wee CC, Davis RB, Huskey KW, Jones DB, Hamel MB. Quality of life among obese patients seeking weight loss surgery: the importance of obesity-related social stigma and functional status. J Gen Intern Med. 2013;28:231–238. doi: 10.1007/s11606-012-2188-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Huang J, Yu H, Marin E, Brock S, Carden D, Davis T. Physicians' weight loss counseling in two public hospital primary care clinics. Acad Med. 2004;79:156–161. doi: 10.1097/00001888-200402000-00012. [DOI] [PubMed] [Google Scholar]
- 82.Block JP, DeSalvo KB, Fisher WP. Are physicians equipped to address the obesity epidemic? Knowledge and attitudes of internal medicine residents. Prev Med. 2003;36:669–675. doi: 10.1016/s0091-7435(03)00055-0. [DOI] [PubMed] [Google Scholar]
- 83.Forman-Hoffman V, Little A, Wahls T. Barriers to obesity management: a pilot study of primary care clinicians. BMC Fam Pract. 2006;7:35. doi: 10.1186/1471-2296-7-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Campbell K, Engel H, Timperio A, Cooper C, Crawford D. Obesity management: Australian general practitioners' attitudes and practices. Obes Res. 2000;8:459–466. doi: 10.1038/oby.2000.57. [DOI] [PubMed] [Google Scholar]
- 85.Hall KD, Heymsfield SB, Kemnitz JW, Klein S, Schoeller DA, Speakman JR. Energy balance and its components: implications for body weight regulation. Am J Clin Nutr. 2012;95:989–994. doi: 10.3945/ajcn.112.036350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Burgess DJ, Warren J, Phelan S, Dovidio J, van Ryn M. Stereotype threat and health disparities: what medical educators and future physicians need to know. J Gen Intern Med. 2010;25(Suppl. 2):S169–S177. doi: 10.1007/s11606-009-1221-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kaminsky J, Gadaleta D. A study of discrimination within the medical community as viewed by obese patients. Obes Surg. 2002;12:14–18. doi: 10.1381/096089202321144513. [DOI] [PubMed] [Google Scholar]
- 88.Merrill E, Grassley J. Women's stories of their experiences as overweight patients. J Adv Nurs. 2008;64:139–146. doi: 10.1111/j.1365-2648.2008.04794.x. [DOI] [PubMed] [Google Scholar]
- 89.Burgess D, van Ryn M, Dovidio J, Saha S. Reducing racial bias among health care providers: lessons from social-cognitive psychology. J Gen Intern Med. 2007;22:882–887. doi: 10.1007/s11606-007-0160-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.O'Reilly C, Sixsmith J. From theory to policy: reducing harms associated with the weight-centered health paradigm. Fat Stud. 2012;1:97–113. [Google Scholar]
- 91.Tylka TL, Annunziato RA, Burgard D, et al. The weight-inclusive versus weight-normative approach to health: evaluating the evidence for prioritizing well-being over weight loss. J Obes. 2014;2014:983495. doi: 10.1155/2014/983495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Batson CD, Lishner DA, Carpenter A, et al. ‘… As you would have them do unto you’: does imagining yourself in the other's place stimulate moral action? Pers Soc Psychol Bull. 2003;29:1190–1201. doi: 10.1177/0146167203254600. [DOI] [PubMed] [Google Scholar]
- 93.Puhl R, Brownell K. Psychosocial origins of obesity stigma: toward changing a powerful and pervasive bias. Obes Rev. 2003;4:213–227. doi: 10.1046/j.1467-789x.2003.00122.x. [DOI] [PubMed] [Google Scholar]
- 94.Danielsdottir S, O'Brien KS, Ciao A. Anti-fat prejudice reduction: a review of published studies. Obes Facts. 2010;3:47–58. doi: 10.1159/000277067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Puhl RM, Schwartz MB, Brownell KD. Impact of perceived consensus on stereotypes about obese people: a new approach for reducing bias. Health Psychol. 2005;24:517–525. doi: 10.1037/0278-6133.24.5.517. [DOI] [PubMed] [Google Scholar]
- 96.Burgess DJ. Are providers more likely to contribute to healthcare disparities under high levels of cognitive load? How features of the healthcare setting may lead to biases in medical decision making. Med Decis Making. 2010;30:246–257. doi: 10.1177/0272989X09341751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lillis J, Hayes SC. Applying acceptance, mindfulness, and values to the reduction of prejudice: a pilot study. Behav Modif. 2007;31:389–411. doi: 10.1177/0145445506298413. [DOI] [PubMed] [Google Scholar]
- 98.Kemeny ME, Foltz C, Cavanagh JF, et al. Contemplative/emotion training reduces negative emotional behavior and promotes prosocial responses. Emotion. 2012;12:338–350. doi: 10.1037/a0026118. [DOI] [PubMed] [Google Scholar]
- 99.Faith MS, Kral TV. Social, environmental, and genetic influences on obesity and obesity-promoting behaviors: fostering research integration. In: Hernandez LM, Blazer DG, editors. Genes, Behavior, and the Social Environment: Moving Beyond the Nature/Nurture Debate. Washington, DC: National Academies Press; 2006. pp. 236–280. [Google Scholar]
- 100.Sumithran P, Prendergast LA, Delbridge E, et al. Long-term persistence of hormonal adaptations to weight loss. N Engl J Med. 2011;365:1597–1604. doi: 10.1056/NEJMoa1105816. [DOI] [PubMed] [Google Scholar]
- 101.O'Brien KS, Puhl RM, Latner JD, Mir AS, Hunter JA. Reducing anti-fat prejudice in preservice health students: a randomized trial. Obesity (Silver Spring) 2010;18:2138–2144. doi: 10.1038/oby.2010.79. [DOI] [PubMed] [Google Scholar]
- 102.Lewis S, Thomas SL, Hyde J, Castle D, Blood RW, Komesaroff PA. ‘I don't eat a hamburger and large chips every day!’ A qualitative study of the impact of public health messages about obesity on obese adults. BMC Public Health. 2010;10:309. doi: 10.1186/1471-2458-10-309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Franz MJ, VanWormer JJ, Crain AL, et al. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc. 2007;107:1755–1767. doi: 10.1016/j.jada.2007.07.017. [DOI] [PubMed] [Google Scholar]
- 104.Riddell LJ, Inman V. Body weight and weight loss: are health messages reaching their target? Asia Pac J Clin Nutr. 2007;16:683–687. [PubMed] [Google Scholar]
- 105.Yancey AK, Simon PA, McCarthy WJ, Lightstone AS, Fielding JE. Ethnic and sex variations in overweight self-perception: relationship to sedentariness. Obesity (Silver Spring) 2006;14:980–988. doi: 10.1038/oby.2006.112. [DOI] [PubMed] [Google Scholar]
- 106.West DS, DiLillo V, Bursac Z, Gore SA, Greene PG. Motivational interviewing improves weight loss in women with type 2 diabetes. Diabetes Care. 2007;30:1081–1087. doi: 10.2337/dc06-1966. [DOI] [PubMed] [Google Scholar]
- 107.Carels RA, Darby L, Cacciapaglia HM, et al. Using motivational interviewing as a supplement to obesity treatment: a stepped-care approach. Health Psychol. 2007;26:369–374. doi: 10.1037/0278-6133.26.3.369. [DOI] [PubMed] [Google Scholar]
- 108.Pollak KI, Alexander SC, Coffman CJ, et al. Physician communication techniques and weight loss in adults: project CHAT. Am J Prev Med. 2010;39:321–328. doi: 10.1016/j.amepre.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Purdie-Vaughns V, Steele CM, Davies PG, Ditlmann R, Crosby JR. Social identity contingencies: how diversity cues signal threat or safety for African Americans in mainstream institutions. J Pers Soc Psychol. 2008;94:615–630. doi: 10.1037/0022-3514.94.4.615. [DOI] [PubMed] [Google Scholar]


