Abstract
Background
Screening for hepatitis C virus (HCV) is recommended in patients born between 1945 and 1965 (“baby boomers”) in the United States. Because these patients are often screened for colorectal cancer, dual screening for HCV may enhance case identification. Our objectives were to assess the acceptability and yield of screening for HCV among patients undergoing screening for colorectal cancer.
Methods
Patients referred for a colonoscopy to screen for colorectal cancer completed an anonymous survey regarding the acceptability of screening for HCV, risk factors and prior testing. The impacts of demographics and risk factors for HCV on willingness to be screened were determined using logistic regression, and the stored sera of 483 patients who had undergone screening for colorectal cancer between February 2011 and August 2012 were tested for HCV antibodies.
Results
Among 1012 survey respondents (median age 56 yr; 911 [90.0%] were baby boomers, 880 [87.0%] were white and 223 [22.0%] were born outside Canada), 123 patients (12.2%) reported prior testing for HCV. HCV was previously diagnosed in 9 of these patients (0.9%, representing 1.0% of the patients who were baby boomers): 5 (55.6% of those diagnosed) reported risk factors. Excluding patients diagnosed with HCV, 903 (90.0%) respondents indicated that they would consent to testing of blood or saliva for HCV. After adjusting for age, sex and status of immigration, patients who were white (odds ratio [OR] 3.38, 95% confidence interval [CI] 1.81–6.32) and patients with risk factors (> 1 v. 0: OR 3.67, 95% CI 1.12–12.02) had a greater acceptance of screening. Among 483 patients screened for colorectal cancer, 3 were anti-HCV positive (0.6%, 95% CI 0.1%–1.8%), representing 0.8% (95% CI 0.2%–2.4%) of the patients who were baby boomers.
Interpretation
Acceptance of screening for HCV is high among patients undergoing screening for colorectal cancer in the Calgary area. However, the low prevalence of HCV suggests that the cost-effectiveness of birth-cohort screening in this population warrants evaluation.
Chronic hepatitis C virus (HCV) infection is a leading cause of cirrhosis, hepatocellular carcinoma and liver transplantation in Canada.1 These complications are expected to increase substantially over the next decade2,3 and cause more years of life lost owing to mortality and suboptimal health compared with any other infectious disease.4 Canadian guidelines advocate testing for HCV in people with evidence of liver disease or risk factors including injection drug use, receipt of blood products before 1992, and those from endemic countries.5 However, several characteristics of HCV suggest that more widespread screening may be beneficial. First, HCV infection is common. Although the exact prevalence is unknown, at least 250 000 Canadians (0.8% of the population) are likely infected.2,3 Second, most patients are asymptomatic until advanced liver disease has developed; thus, many patients with HCV are unaware of their HCV infection (21%–70% in Canada3,6 and 50%–75% in the United States).7 Third, therapies are available that cure the infection in over 80% of patients,8,9 arrest progression of liver disease and reduce mortality.10 Based on these characteristics, recent US guidelines advocated one-time screening for HCV antibodies in individuals born between 1945 and 1965 (“baby boomers”) plus risk factor–based screening.11 This birth cohort has a high prevalence of HCV (3.6% in the US), accounts for 75% of all cases and has the greatest risk of HCV-related mortality.12,13 The Canadian Liver Foundation has endorsed similar recommendations.14 Salivary assays for HCV antibodies, which are approved for clinical use in the US but not Canada, may enhance the acceptance of screening owing to the noninvasive nature of these tests compared with blood-based assays.15
Prior to adopting birth-cohort screening in Canada, the prevalence of HCV and the feasibility of this approach require confirmation. Our study sought to address these issues among patients undergoing colonoscopy for colorectal cancer screening. This unique clinical setting offers several advantages relevant to birth-cohort HCV screening. Because screening for colorectal cancer is recommended for individuals starting at 50 years of age — many of whom undergo colonoscopy at regular intervals — this patient population is enriched with baby boomers.16 Second, patients who undergo screening for colorectal cancer are engaged in care and have shown acceptance of preventive interventions. Finally, gastroenterologists are in a unique position in that they frequently treat viral hepatitis and also perform screening colonoscopies.17 Unlike primary care–based HCV screening, this environment ensures direct linkage to counselling and antiviral therapy for infected cases.
Methods
Study setting
The Forzani and MacPhail Colon Cancer Screening Centre (the Centre) is an endoscopy unit in a nonhospital setting located in Calgary, Alberta, that is dedicated to providing colonoscopies for colorectal cancer screening (about 19 000 annually) to residents of Calgary and its surrounding communities (a population of about 1.5 million).18 The Centre accepts referrals for patients who are asymptomatic, in good health and eligible for colonoscopy for colorectal cancer screening (e.g., those at average or increased risk of colorectal cancer, to investigate positive fecal occult blood tests and surveillance in those with a history of adenomatous polyps or colorectal cancer). Colonoscopy for the investigation of symptoms, dysplasia surveillance in patients with inflammatory bowel disease or in patients with major comorbidities that preclude colonoscopy in a nonhospital setting (e.g., decompensated cirrhosis) is not provided.
Survey design and administration
Patients who are referred to the Centre attend an education session regarding colorectal cancer, which includes information about screening options and preparation for colonoscopy.18 For the first part of this study, during May 2013, we invited patients who attended this session to complete an anonymous survey that requested information about demographic characteristics and asked about the acceptability of HCV screening by blood- or saliva-based assays, risk factors for infection (e.g., injection drug use, blood transfusion) and previous testing for and pre-existing diagnoses of HCV (Appendix 1, available at www.cmajo.ca/content/3/1/E62/suppl/DC1). Pre-existing HCV diagnoses could not be confirmed owing to the anonymous nature of the survey. Patients were also asked about their willingness to be examined by a hepatologist if the HCV test result was positive. Owing to its simplicity, the survey was not piloted, and participation was entirely voluntary. The Conjoint Health Research Ethics Board at the University of Calgary, Calgary, Alberta, approved the study.
Serum HCV testing
The Centre maintains a biorepository of serum specimens (stored at –80ºC) from consenting patients who have undergone colonoscopy for colorectal cancer screening and records of their demographic, lifestyle and health information (excluding HCV status). Patients included in the biorepository are similar to the general population of patients who have undergone screening. For the second part of the study, we used a random number generator to select 496 patients (of a total of 671) who had provided serum specimens to the biorepository between February 2011 and August 2012. Because these patients had not consented to HCV testing, we contacted them by mail to outline the purpose of the study and to request permission to test their serum for HCV. Patients wishing to opt out were asked to return a preaddressed letter within one month of the initial mail out. Testing for anti-HCV antibodies in eligible patients was performed using the ARCHITECT anti-HCV chemiluminescent microparticle immunoassay (Abbott Laboratories, Abbott Park, Illinois) and confirmed with the MONOLISA anti-HCV Plus assay (Bio-Rad Laboratories, Montréal). In patients with positive results for anti-HCV in both assays, chronic HCV infection (i.e., persistent viremia) was confirmed by testing their sera for HCV RNA levels using the Abbott RealTime HCV assay (version 4.0; lower limit of virus detection was 12 IU/mL).
Statistical analyses
Data are presented as medians (interquartile range [IQR]) or proportions. Between-group comparisons were made using the Fisher exact test or the Mann–Whitney test.
In the first part of the study, the primary outcome measure was the willingness to be screened for anti-HCV antibodies using either blood- or saliva-based assays. Using logistic regression analysis, we determined the associations between the following factors and willingness to be screened: age, sex, race (white or other), immigrant status (Canadian or born elsewhere), marital status (married/common-law or other), education (university or lower), and the number of self-reported risk factors for HCV (categorized as 0, 1 and ≥ 2). Risk factors included injection drug use, blood transfusion, presence of tattoos, incarceration, family member or spouse with HCV, and sexual contact with an HCV-positive partner. Independent predictors of willingness to be screened were determined using a logistic regression model including age, sex and variables significant (p < 0.05) in univariate analyses. Associations are presented as odds ratios (ORs) and 95% confidence intervals (CIs).
In the second part of the study, the proportions of patients with positive test results for anti-HCV antibodies and positive test results for HCV RNA in serum were calculated with exact binomial 95% CIs. Subgroup analyses were conducted according to birth cohort (1945–1965 [baby boomers] v. other). All statistical analyses were performed using Stata v11.0 (StataCorp; College Station, Texas). Two-sided p values less than 0.05 were considered statistically significant.
Results
Characteristics of patients
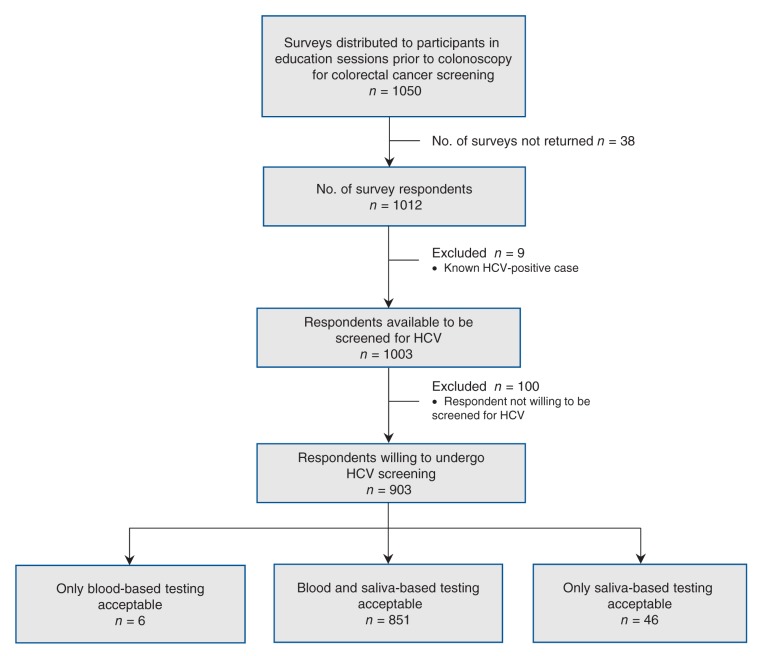
During May 2013, 2045 patients attended the education sessions at the Centre. Of the 1050 surveys that were distributed, 1012 were completed (response rate of 49.5%) (Figure 1). Demographic characteristics of the respondents are shown in Table 1. Twenty-six percent of the respondents (n = 266) reported at least one risk factor for HCV infection. Prior blood transfusions (n = 89, 8.9%) and tattoos (n = 86, 8.6%) were the most common risk factors reported; injection drug use (n = 22, 2.2%), patients with an infected family member (n = 15, 1.5%) or spouse (n = 2, 0.2%), incarceration (n = 7, 0.7%) and sexual contact with an infected partner (n = 5, 0.5%) were the least common.
Figure 1:
Flow diagram of participant recruitment in a colorectal cancer screening population to determine the acceptability of screening for hepatitis C virus (HCV). A convenience sample of attendees at an education session about screening for colorectal cancer completed a survey regarding their willingness to undergo screening for HCV.
Self-reported HCV infection
One hundred and twenty-three survey respondents (12.2%) reported previous HCV testing, and 9 patients (7.3%) disclosed a known diagnosis of HCV. If confirmed (and the remaining patients had negative test results), these infections would correspond to an HCV prevalence of 0.9% (95% CI 0.4%–1.7% [9/1012]) overall and 1.0% (95% CI 0.5%–1.9% [9/914]) among baby boomers. Five of the patients with HCV (55.6%) reported risk factors for HCV (4 patients reported injection drug use, and 1 patient reported an infected family member/blood transfusion).
Acceptability of HCV screening
Excluding the 9 patients with self-reported HCV infection, 903 (90.0%) of survey respondents (n = 1003) would consent to HCV antibody screening by blood- (85.4%) or saliva-based testing (89.4%; p = 0.009 v. blood) (Figure 1). Ninety-two percent of respondents (n = 919) would consent to an examination by a specialist if they were found to be HCV-positive. Table 1 shows the characteristics of patients referred for screening for colorectal cancer according to their willingness to undergo HCV screening. In the univariate analysis, white race, born in Canada and an increasing number of risk factors for HCV were associated with a willingness to be screened. After adjustment for age and sex, white patients were more likely to accept HCV screening (OR 3.38, 95% CI 1.81–6.32); country of origin was not significant (OR 0.70, 95% CI 0.39–1.26). Compared with patients with no reported risk factors for HCV, patients with 1 (OR 2.79, 95% CI 1.30–5.96) or at least 2 risk factors (OR 3.67, 95% CI 1.12–12.02) were more likely to accept HCV screening.
Table 1: Characteristics of patients referred for colorectal cancer screening by willingness to undergo screening for HCV.
| Variable* | Total cohort, no. (%)† n = 1012 |
Patients willing to be screened, no. (%)† n = 903‡ |
Patients unwilling to be screened, no. (%)† n = 100‡ |
Unadjusted OR for willingness to be screened (95% CI)‡ |
|---|---|---|---|---|
| Male |
529 (52.3) |
474 (52.5) |
51 (51.0) |
1.09 (0.74–1.59) |
| Age, yr, median (IQR) |
56 (53–62) |
56 (53–62) |
57 (53–61) |
0.99 (0.96–1.02) |
| Baby boomer (born 1945–1965) |
914 (90.5) |
814 (90.2) |
91 (91.9) |
0.81 (0.38–1.73) |
| White |
876 (87.1) |
803 (89.3) |
65 (66.3) |
4.25 (2.66–6.79) |
| Born outside of Canada |
221 (21.9) |
177 (19.6) |
42 (42.0) |
0.34 (0.22–0.52) |
| University education |
399 (42.3) |
358 (42.2) |
38 (43.7) |
0.94 (0.60–1.47) |
| Married or common-law |
831 (82.5) |
741 (82.4) |
83 (83.8) |
0.90 (0.52–1.59) |
| HCV risk factors |
||||
| 0 |
746 (73.7) |
653 (72.3) |
89 (89.0) |
Ref |
| 1 |
169 (16.7) |
158 (17.5) |
8 (8.0) |
2.69 (1.28–5.66) |
| ≥ 2 | 97 (9.6) | 92 (10.2) | 3 (3.0) | 4.18 (1.30–13.5) |
Note: CI = confidence interval, HCV = hepatitis C virus, IQR = interquartile range, OR = odds ratio. *Number of respondents missing for the following variables: sex (n = 1), age (n = 2), race (n = 6), immigration status (n =1), marital status (n = 5) and education level (n = 69). †Unless otherwise specified. ‡Excludes 9 patients with a self-reported diagnosis of HCV.
Prevalence of HCV in patients screened for colorectal cancer
Requests were sent to 496 patients with specimens stored in the biorepository for permission to test their sera for HCV; 8 patients refused, and the letters to 5 patients were returned as undeliverable. After excluding these 13 patients, 483 specimens (97.3%) were available for testing for anti-HCV antibodies. The median age of the patients was 56 years (IQR 56–61 yr); 76.6% (n = 370) were baby boomers, 48.2% (n = 233) were male, 26.0% (n = 125) were born outside of Canada and 43.2% (n = 208) had a university education. In total, 4 patients had positive test results for anti-HCV on initial screening, of which 3 were confirmed, corresponding to an anti-HCV prevalence of 0.6% (95% CI 0.1%–1.8%) overall and 0.8% (95% CI 0.2%–2.4%) among baby boomers. The 3 anti-HCV positive patients were male, baby boomers, and one was born outside of Canada. HCV RNA was positive in 2 of these cases (52 971 and 9 728 627 IU/mL, respectively), corresponding to a prevalence of chronic HCV infection (i.e., viremia) of 0.4% (95% CI 0.05%–1.5%) overall and 0.5% (0.07%–2.0%) among baby boomers.
Interpretation
Main findings
Our study confirms that there is a high acceptability of screening for HCV among patients undergoing colonoscopy for colorectal cancer screening in the Calgary area. However, the prevalence of HCV was lower than expected, suggesting that birth-cohort screening in this patient population may not be optimal for improving case identification in Canada. On the other hand, these patients are engaged in preventive care and would potentially be more likely to accept and complete anti-HCV treatment than other target screening populations.
Among patients referred for colonoscopy for colorectal cancer screening at a nonhospital endoscopy facility, 90.0% would be willing to undergo dual screening for HCV by blood- or saliva-based assays. Patients with risk factors for HCV were more likely to accept screening, which suggests that screening based on risk factors could be effective if appropriately conducted. However, frequently cited barriers to this approach, including lack of physician time and knowledge about risk factors for HCV and patient reluctance to disclose their risk factors, were partially addressed by our administration of an anonymous survey.19 We also observed that patients born outside Canada were less likely to accept screening, although this difference did not persist after adjustment for race; white patients were more accepting of screening. Other studies have reported reduced screening in patients born outside Canada (e.g., for breast and cervical cancer),20,21 perhaps because of a fear of stigmatization or repercussions regarding immigration status.22 Not surprisingly, patients were more likely to accept screening for HCV via salivary tests compared with blood tests, presumably because of their noninvasive nature.23 Although this issue is less important in this setting because patients could have blood drawn with the insertion of their intravenous line before undergoing colonoscopy, the use of salivary tests when available may be preferable in other settings such as outreach programs,15 particularly among injection drug users who may have compromised venous access.24
The observed rates of self-reported HCV infection (0.9% of all patients; 1.0% of baby boomers) and anti-HCV positivity of screened blood samples (0.6% of all samples; 0.8% of baby boomer samples) were lower than we expected, particularly if only patients with chronic infection (i.e., viremic) are considered (0.4% of all patients; 0.5% of baby boomers). In British Columbia, 1.4% of the tests for HCV antibodies were positive (3.0% among baby boomers),25 and estimates of HCV prevalence in the US from the National Health and Nutrition Examination Survey are substantially higher (1.6% of patients overall and 3.6% among baby boomers).12 There are several possible explanations for these differences. Importantly, the prevalence of HCV in Canada may be lower than has been suggested. Our results are in line with modelled estimates from Remis (0.8% of patients overall and 1.2% of baby boomers).3 Moreover, in the only seroprevalence study of randomly selected persons in Canada, the Canadian Health Measures Survey reported an anti-HCV prevalence of 0.5% overall and 0.8% among persons aged 50–79 years.6 However, our study and the Canadian Health Measures Survey undersampled some high-risk groups, including injection drug users, people who are incarcerated, the homeless and people of Aboriginal origin. Although the population of people born outside Canada in our study (and in the Canadian Health Measures Survey6) was similar to the Canadian population, ours was a highly educated cohort engaged in their health care. Therefore, the generalizability of our findings may be questioned. Moreover, the CIs for our prevalence estimates are wide because of the small sample size of our study. For example, the HCV prevalence in baby boomers and overall could be as high as 2.4% and 1.8%, respectively. Despite these uncertainties, the main unanswered question is whether screening for HCV among patients undergoing screening for colorectal cancer (and in general) is cost-effective. In the US, screening of baby boomers in a primary care setting has been advocated based on an incremental cost-effectiveness ratio of approximately $36 000/QALY over screening based on risk factors.7 Whether combined screening for HCV and CRC is cost-effective in Canada warrants formal analysis, particularly in light of differences in HCV prevalence and the costs of screening for HCV and treatment in Canada versus the US. Similar to advanced colorectal cancer, the costs of managing end-stage liver disease secondary to HCV is high.2 Moreover, the fact that patients undergoing screening for colorectal cancer are already engaged in care with experts in the treatment of HCV, which reduces the necessity of additional referrals and appointments, must be considered.
Limitations
The ability to draw inferences regarding the prevalence of HCV in Canada is limited by the specific nature of our study population and small sample size. Validation of our findings in other regions and with a larger sample size would be informative. In addition, 8 patients (1.6%) declined to participate in the study and 5 could not be contacted. If these patients declined because of known HCV infection or perceived risks factors for infection, our prevalence figures could be underestimates.
Conclusion
Acceptance of screening for HCV is high among patients undergoing screening for colorectal cancer in Calgary and its surrounding communities. However, the relatively low prevalence of HCV suggests that the cost-effectiveness of birth-cohort screening in this population warrants evaluation before the widespread adoption of this approach.
Supplemental information
For reviewer comments and the original submission, please see www.cmajopen.ca/content/3/1/E62/suppl/DC1
Supplementary Material
References
- 1.Myers RP, Liu M, Shaheen AA. The burden of hepatitis C virus infection is growing: a Canadian population-based study of hospitalizations from 1994 to 2004. Can J Gastroenterol 2008;22:381-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Myers RP, Krajden M, Bilodeau M, et al. Burden of disease and cost of chronic hepatitis C infection in Canada. Can J Gastroenterol Hepatol 2014;28:243-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Remis RS. Modelling the incidence and prevalence of hepatitis C infection and its sequelae in Canada, 2007: final report Ottawa: Public Health Agency of Canada; 2007. Available: www.phac-aspc.gc.ca/sti-its-surv-epi/model/pdf/model07-eng.pdf (accessed 2015 Jan. 16).
- 4.Kwong, JC, Crowcroft, NS, Campitelli, MA, et al.; Ontario Burden of Infectious Disease Study Advisory Group. Ontario Burden of Infectious Disease Study (ONBOIDS): an OAHPP/ICES report. Toronto: Ontario Agency for Health Protection and Promotion, Institute for Clinical Evaluative Sciences; 2010. [Google Scholar]
- 5.Myers RP, Ramji A, Bilodeau M, et al. An update on the management of hepatitis C: consensus guidelines from the Canadian Association for the Study of the Liver. Can J Gastroenterol 2012;26:359-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rotermann M, Langlois K, Andonov A, et al. Seroprevalence of hepatitis B and C virus infections: results from the 2007 to 2009 and 2009 to 2011 Canadian Health Measures Survey. Health Rep 2013;24:3-13. [PubMed] [Google Scholar]
- 7.Rein DB, Smith BD, Wittenborn JS, et al. The cost-effectiveness of birth-cohort screening for hepatitis C antibody in US primary care settings. Ann Intern Med 2012;156:263-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lawitz E, Mangia A, Wyles D, et al. Sofosbuvir for previously untreated chronic hepatitis C infection. N Engl J Med 2013;368:1878-87. [DOI] [PubMed] [Google Scholar]
- 9.Jacobson IM, Dore GJ, Foster GR, et al. Simeprevir with pegylated interferon alfa 2a plus ribavirin in treatment-naive patients with chronic hepatitis C virus genotype 1 infection (QUEST-1): a phase 3, randomised, double-blind, placebo-controlled trial. Lancet 2014;384;403-13. [DOI] [PubMed] [Google Scholar]
- 10.van der Meer AJ, Veldt BJ, Feld JJ, et al. Association between sustained virological response and all-cause mortality among patients with chronic hepatitis C and advanced hepatic fibrosis. JAMA 2012;308:2584-93. [DOI] [PubMed] [Google Scholar]
- 11.Screening for hepatitis C virus infection in adults: final recommendation statement. Rockville (MD): US Preventive Services Task Force; 2013. Report no.: 12-05174-EF-2.
- 12.Armstrong GL, Wasley A, Simard EP, et al. The prevalence of hepatitis C virus infection in the United States, 1999 through 2002. Ann Intern Med 2006;144:705-14. [DOI] [PubMed] [Google Scholar]
- 13.Ly KN, Xing J, Klevens RM, et al. The increasing burden of mortality from viral hepatitis in the United States between 1999 and 2007. Ann Intern Med 2012;156:271-8. [DOI] [PubMed] [Google Scholar]
- 14.National hepatitis C survey prompts call for all Canadian boomers to get tested. Markham (ON): Canadian Liver Foundation; 2013. Available: www.liver.ca/newsroom/press-releases/29-01_2013_CLF_recommends_hepC_testing.aspx (accessed 2015 Jan. 16).
- 15.Drobnik A, Judd C, Banach D, et al. Public health implications of rapid hepatitis C screening with an oral swab for community-based organizations serving high-risk populations. Am J Public Health 2011;101:2151-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leddin DJ, Enns R, Hilsden R, et al. Canadian Association of Gastroenterology position statement on screening individuals at average risk for developing colorectal cancer: 2010. Can J Gastroenterol 2010;24:705-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sears DM, Cohen DC, Ackerman K, et al. Birth cohort screening for chronic hepatitis during colonoscopy appointments. Am J Gastroenterol 2013;108:981-9. [DOI] [PubMed] [Google Scholar]
- 18.Hilsden RJ, Rostom A, Dube C, et al. Development and implementation of a comprehensive quality assurance program at a community endoscopy facility. Can J Gastroenterol 2011;25:547-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shah HA, Heathcote J, Feld JJ. A Canadian screening program for hepatitis C: Is now the time? CMAJ 2013;185:1325-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Borkhoff CM, Saskin R, Rabeneck L, et al. Disparities in receipt of screening tests for cancer, diabetes and high cholesterol in Ontario, Canada: a population-based study using area-based methods. Can J Public Health 2013;104:e284-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khadilkar A, Chen Y. Rate of cervical cancer screening associated with immigration status and number of years since immigration in Ontario, Canada. J Immigr Minor Health 2013;15:244-8. [DOI] [PubMed] [Google Scholar]
- 22.Li D, Tang T, Patterson M, et al. The impact of hepatitis B knowledge and stigma on screening in Canadian Chinese persons. Can J Gastroenterol 2012;26:597-602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shivkumar S, Peeling R, Jafari Y, et al. Accuracy of rapid and point-of-care screening tests for hepatitis C: a systematic review and meta-analysis. Ann Intern Med 2012;157:558-66. [DOI] [PubMed] [Google Scholar]
- 24.Wong VW, Wong GL, Chim AM, et al. Targeted hepatitis C screening among ex-injection drug users in the community. J Gastroenterol Hepatol 2014;29:116-20. [DOI] [PubMed] [Google Scholar]
- 25.Krajden M, Cook D, Buller-Taylor T, et al. Cost implications of one-time HCV screening of the 1945 to 1965 birth cohort in British Columbia, Canada. J Hepatol 2013;58 (Suppl; Abstract 467).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.