Abstract
Objectives
The aim of this study is to describe blood lead levels (BLLs) and the prevalence of elevated blood lead levels (EBLLs) in children aged 0–6 years old and to analyze the BLL trend in children from 2009 to 2013 in China.
Methods
A total of 124,376 children aged 0–6 years old were recruited for this study from January 1st 2009 to December 31st 2013. Their blood lead levels were analyzed using atomic absorption spectrometry.
Results
The median BLL was 64.3 μg/L (IQR: 49.6–81.0), and the range was 4.3–799.0 μg/L. Blood lead levels were significantly higher in boys (66.0 μg/L) than in girls (61.9 μg/L) (P<0.001). The overall prevalence of BLLs≥100 μg/L was 10.54% in children aged 0–6 years in Hunan Province. Between 2009 and 2013, the prevalence of EBLLs (≥100 μg/L) decreased from 18.31% to 4.26% in children aged 0–6 years and increased with age. The prevalence of EBLLs has dramatically decreased in two stages (2009–2010 and 2012–2013), with a slight fluctuation in 2010 and 2011.
Conclusions
Both BLLs and the prevalence of EBLLs in children aged 0–6 years old declined substantially from 2009 to 2013 in Hunan Province; however, both remain at unacceptably high levels compared to developed countries. Comprehensive strategies are required to further reduce blood lead levels in children.
Introduction
It is well known that there is no safe blood lead level (BLL) in children. Many studies have demonstrated that lead exposure is related to the risk of behavioral and intellectual deficits, hypertension, nephropathy and infertility [1–7]. The National Toxicology Program (NTP) concluded that the presence of lead in blood at BLL<100 μg/L was associated with delayed puberty and poor cognitive performance and with a lower intelligence quotient (IQ) in the United States [8]. Liu JH et al. showed that Chinese children with BLLs ≥80 μg/L have lower scores than those with BLLs<80 μg/L in IQ tests and academic performance [9]. Children, especially younger children, are at greatest risk for elevated BLLs. Some studies have demonstrated that children appear to have approximately four to five times higher lead absorption than adults [10], and the detoxification capability of lead in adults was three times higher than in children [11].
Burning fossil fuels with lead, wall paints with lead, drinking water from lead containing pipes and industrial manufacturing processes are the major sources of lead pollution in air, water and soil. Lead in the air, water and dust can be absorbed by children through the respiratory tract and digestive tract. In Europe and the United States, control measures to regulate lead in petrol, paint, food and drinking water were implemented to reduce the lead exposure in daily surroundings since the 1970s. Blood lead levels in children have decreased considerably over the last several decades in the United States. In China, lead free gasoline was forcibly adopted by the Chinese Government to reduce lead exposure on July 1st 2000. Since then, the prevalence of EBLLs in children dramatically decreased from 34% in 1995–2003 to approximately 24% in 2001–2007 [12]. With the unprecedented growth of China’s lead-acid battery industry from the electric bike, automotive, and photovoltaic industries, lead exposure remains an important public health concern [13]. The aim of our study was to analyze the blood lead level (BLL) in children aged 0–6 years old from 2009–2013 and to reveal the trend of BLLs in Chinese children.
Materials and Methods
Ethics statement
The study was approved by the Ethics Committee of Hunan Children’s Hospital. Informed written consent was also obtained from a legal guardian of each child involved in our study before data collection. All of the samples were sent to the clinic laboratory to detect the BLLs, and all data collected from the participants were fully anonymous.
Study subjects
The Children who received regular health checkups at outpatient clinic of Hunan Children’s Hospital between Jan 1st 2009 and Dec 31st 2013 were recruited for the present study. All the children were residents of Hunan Province. Hunan Children’s Hospital is the largest tertiary hospital, providing service to a population of 71 million and a land area of 211,800 km2 in China. Hunan Province is located in central China and had a population of 222 million children in 2013.
Children who presented to the clinic for regular checkups and resided in Hunan Province were included in the study. 18 children with a typical symptom of lead toxicity such as seizures, neurological disorders and other symptoms were excluded in this study because these children who exposed to a severe lead poisoning outbreak in one area of Hunan Province in 2010. For any given year, a child was counted only once based children’s name, home address and the phone number of children’s parent. For a child with a confirmed EBLL among many tests in any given year, the highest value was considered as the blood lead level for the child. A total of 124,376 children were included in the study from 2009–2013. The annual subjects were 20,910, 22,802, 28,228, 28,278, and 24,158 children, respectively from the 2009 to 2013.
Blood lead level determinations
Blood samples were taken from each child by trained staff into lead-free vacutainer tubes containing sodium heparin and were stored at 4°C prior to lead analysis. The blood lead level was analyzed using atomic absorption spectrometry (Z-2700 Hitachi Limited). The spectrometer, reagents and standard method were all provided by Hitachi Limited in Japan. Analysis of each sample was performed in duplicate, and the mean of both values was used as the final value. All reagents, glassware and sample collection devices were checked for lead contamination. The sample measurement was carried out in accordance with the manufacturer’s instructions. The technicians in our laboratory had received the training of a CDC (Center for Disease Control and Prevention of China)-administered quality-control program (Blood Lead Proficiency Testing Program) for the measurement of lead in blood sample. The lead measurement was carried out according to standard procedure provided by CDC of China. We defined BLLs≥100 μg/l as elevated BLLs (EBLLs) based on the guidelines by the Medical Administration Department of the Ministry of Health of China in 2006.
Statistical analysis
Because BLLs were not normally distributed, the median and interquartile range were used to describe the blood lead level in children. The Mann-Whitney U test was used to compare the BLLs by gender. The Kruskal-Wallis test was used to compare the BLLs of different age groups. The percentage of EBLLs was calculated by age and gender. Differences between groups were assessed using the χ 2 test to evaluate the prevalence of EBLLs. The Spearman's rank correlation coefficient test was used to examine the temporal trends for BLLs, and the Cochran–Armitage test to examine the temporal trends for the prevalence of EBLLs. All analyses were performed using the Statistic Package for Social Sciences (SPSS) for Windows version 18.0. The figures were plotted using Microsoft Excel 2007. All of the statistical tests were two-sided. P values less than 0.05 were considered statistically significant.
Results
The median of the blood lead levels
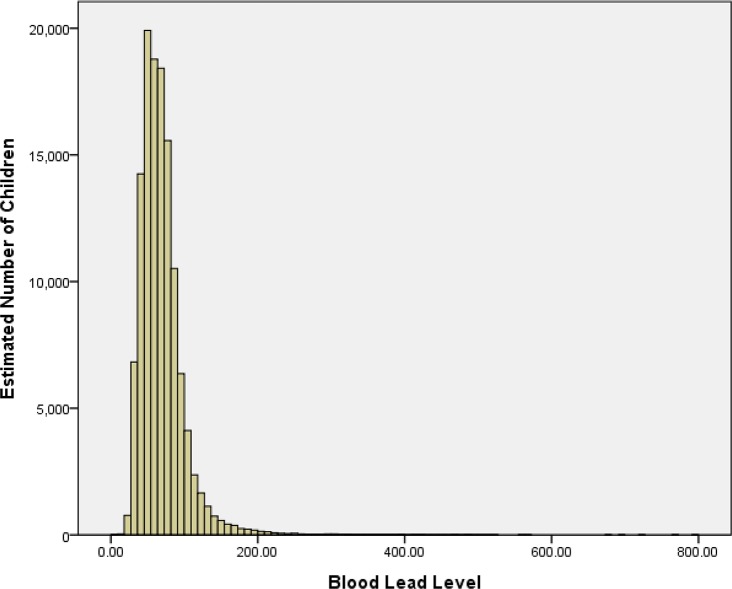
Of the 124,376 children enrolled in this study, 63.14% were boys. The average age was 3.2±2.4 years old. Fig 1 shows that the BLL has a positively skewed distribution. There were 13,112 (10.54%) children with elevated blood lead levels (≥100 μg/L) in this study, 12,247 (9.85%) children with values between 100 μg/L and 199 μg/L, 835 (0.67%) children with values between 200 μg/L and 449 μg/L, 27 (0.02%) children with values between 450 μg/L and 699 μg/L, and 3 children with values of more than 700μg/L.
Fig 1. Blood lead levels in children aged 0~6 years living in Hunan Province in 2009–2013.
For all children, the median BLL was 64.3 μg/L (IQR: 49.6–81.0), and the range was 4.3–799.0 μg/L. The median values were as follows: 73.0 μg/L (IQR: 53.0–92.0) in 2009, 63.0 μg/L (IQR: 47.5–82.0) in 2010, 66.0 μg/L (IQR: 51.4–81.8) in 2011, 65.0 μg/L (IQR: 51.0–79.0) in 2012 and 58.6 μg/L (IQR: 46.9–71.1) in 2013. Between 2009 and 2013, the median BLL decreased from 73.0 μg/L to 58.6 μg/L (rs = -0.137, P<0.001). However, the median BLL slightly increased in 2011 and 2012 compared to 2010. The median BLL was 66.0 μg/L (IQR: 51.0–82.5) in boys and 61.9 μg/L (IQR: 48.0–78.0) in girls. The median BLL for boys was higher than girls, and the difference was statistically significant (P<0.001). Table 1 shows that the median BLL for boys was significantly higher than for girls in each year (P<0.001).
Table 1. Comparison of the BLLs in children for different genders from 2009 to 2013.
| Years | Boys | Girls | P | ||||
|---|---|---|---|---|---|---|---|
| n | P50(P25~P75) | max | n | P50(P25~P75) | max | ||
| 2009 | 13243 | 75(54~94) | 567 | 7667 | 70(51~89) | 352 | <0.001 |
| 2010 | 14431 | 65(49~84) | 490 | 8371 | 60(46~79) | 463 | <0.001 |
| 2011 | 17714 | 68(53~84) | 516 | 10514 | 63(49~79) | 498 | <0.001 |
| 2012 | 17805 | 67(52~80) | 573 | 10473 | 63(49~76) | 799 | <0.001 |
| 2013 | 15333 | 60(48~72) | 764 | 8825 | 57(46~69) | 483 | <0.001 |
| Total | 78526 | 66(51~83) | 764 | 45850 | 62(48~78) | 799 | <0.001 |
Table 2 shows that the median BLL was lowest (50 μg/L) for children between 0 and 12 months old and highest (69.7 μg/L) for children aged 6 years. The median BLL increased with age in all subjects. The median BLL for boys was higher than for girls in each age group from 2009 to 2013. The median BLL increased with age in children from 2009–2010; however, from 2011 to 2013, the median BLL increased with age until the age of five and then decreased for six year olds. In boys, the median BLL increased with age from 2009 to 2010, while the median BLL increased with age until the age of five and then decreased for six year olds from 2011 to 2013. In girls, the median BLL increased with age until the age of five and then decreased for six year olds in two stages (2009–2010 and 2012–2013).
Table 2. Blood lead level (ug/l), by sex and age, in children aged 0 to 6 years living in China in 2009–2013.
| Variants | 0~ | 1~ | 2~ | 3~ | 4~ | 5~ | 6~ | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | P50(P25~P75) | n | P50(P25~P75) | n | P50(P25~P75) | n | P50(P25~P75) | n | P50(P25~P75) | n | P50(P25~P75) | n | P50(P25~P75) | |
| 2009 | 2094 | 56(44~76) | 4585 | 70(50~86) | 3109 | 72(52~89) | 2626 | 76(55~93) | 2812 | 79(58~98) | 2679 | 79(57~99) | 3005 | 82(59~103) |
| Boys | 1210 | 58(45~77) | 2749 | 71(51~87) | 1973 | 73(53~91) | 1672 | 78(57~95) | 1829 | 81(60~99) | 1795 | 81(59~102) | 2015 | 83(61~105) |
| Girls | 884 | 55(43~75) | 1836 | 67(49~85) | 1136 | 70(50~87) | 954 | 74(52~90) | 983 | 75(55~94) | 884 | 75(54~95) | 990 | 78(56~98) |
| 2010 | 2226 | 49(39~64) | 4896 | 58(44~77) | 3473 | 63(48~80) | 2965 | 67(50~85) | 2998 | 67(51~85) | 3065 | 69(51~87) | 3179 | 69(52~89) |
| Boys | 1313 | 49(40~66) | 2884 | 59(45~79) | 2224 | 64(48~82) | 1929 | 69(51~87) | 1944 | 69(52~69) | 2012 | 71(53~89) | 2125 | 72(54~90) |
| Girls | 913 | 48(39~63) | 2012 | 56(43~74) | 1249 | 60(46~78) | 1036 | 62(48~82) | 1054 | 65(49~82) | 1053 | 67(49~85) | 1054 | 64(49~82) |
| 2011 | 3807 | 50(42~64) | 5874 | 62(49~77) | 4112 | 67(53~81) | 3651 | 70(56~85) | 3692 | 71(57~86) | 3450 | 72(58~87) | 3642 | 72(58~86) |
| Boys | 2211 | 51(42~65) | 3497 | 63(50~79) | 2565 | 68(54~83) | 2359 | 71(57~86) | 2409 | 72(58~86) | 2254 | 74(59~89) | 2419 | 74(60~88) |
| Girls | 1596 | 50.0(42.0~63) | 2377 | 60(48~74) | 1547 | 65(51~79) | 1292 | 67(54~82) | 1283 | 70(56~85) | 1196 | 69(56~83) | 1223 | 68(55~81) |
| 2012 | 2512 | 51(41~66) | 6919 | 60(47~74) | 4120 | 66(52~79) | 3729 | 68(54~81) | 3758 | 69(56~82) | 3589 | 70(57~83) | 3651 | 69(57~81) |
| Boys | 1465 | 51(42~67) | 4060 | 60(48~75) | 2581 | 68(54~80) | 2378 | 69(55~82) | 2469 | 70(57~83) | 2396 | 72(59~86) | 2456 | 71(59~84) |
| Girls | 1047 | 50(41~65) | 2859 | 59(46~73) | 1539 | 64(50~77) | 1351 | 66(53~78) | 1289 | 67(54~79) | 1193 | 68(55~79) | 1195 | 66(54~77) |
| 2013 | 1913 | 48(41.~59) | 5268 | 54(45~66) | 3576 | 59(46~71) | 3350 | 61(48~73) | 3447 | 62(49~73) | 3283 | 63(50~74) | 3321 | 62(50~74) |
| Boys | 1129 | 48.4(42~59) | 3143 | 55(45~67) | 2237 | 59(47~72) | 2134 | 63(49~74) | 2269 | 63(50~74) | 2232 | 64(51~75) | 2189 | 63(51~76) |
| Girls | 784 | 48.0(41~59) | 2125 | 54(44~66) | 1339 | 57(45~71) | 1216 | 59(47~71) | 1178 | 60(46~71) | 1051 | 60(49~71) | 1132 | 59(47~72) |
Elevated blood lead levels
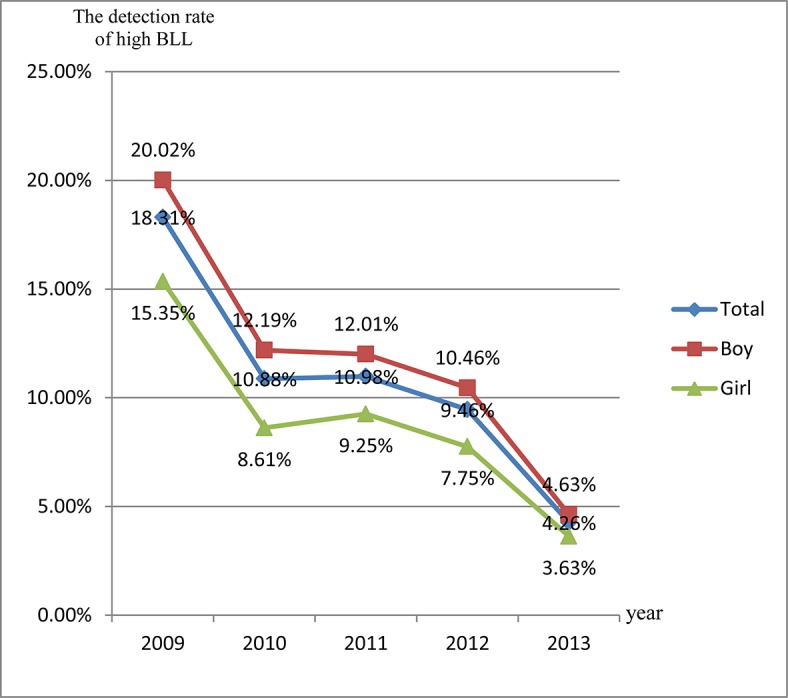
The overall prevalence of BLLs≥100μg/L was 10.54% in children aged 0–6 years. The prevalence of EBLLs was higher for boys (11.60%) than for girls (8.73%) from 2009 to 2013, and the difference was statistically significant (χ 2 = 252.71, P<0.001). Between 2009 and 2013, the prevalence of EBLLs decreased from 18.31% to 4.26% in children aged 0–6 years (Z = 43.41, P<0.001). Fig 2 shows that the prevalence of EBLLs dramatically decreased in 2009–2010 and 2012–2013. The prevalence of EBLLs decreased from 2009 to 2013 for boys and girls in this study. In each year, the prevalence of EBLLs was higher for boys than for girls between 2009 and 2013.
Fig 2. The detection rate of high BLL in different age groups from 2009 to 2013.
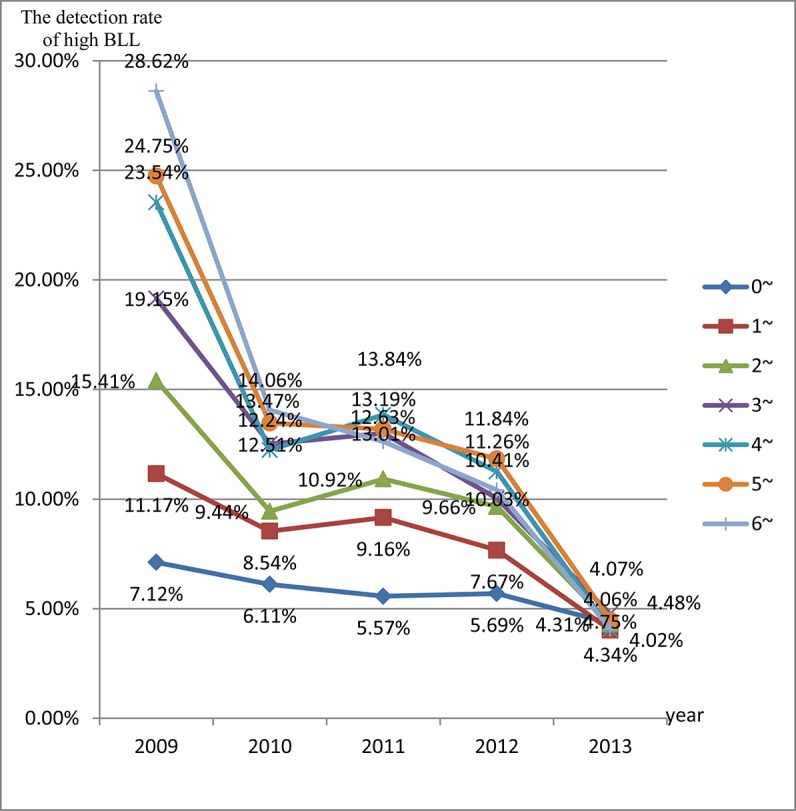
The prevalence of EBLLs was the lowest in children aged 0–12 months (5.76%), and the prevalence of EBLLs increased with age. In each year from 2009 to 2010, the prevalence of EBLLs increased with age. From 2011 to 2013, the prevalence of EBLLs increased with age until the age of five years and then decreased for six year olds (Fig 3). Between 2009 and 2013, the prevalence of EBLLs decreased among all age groups. Fig 3 shows that the prevalence of EBLLs was significantly reduced in 4–6 years old.
Fig 3. The detection rate of high BLL in different age groups from 2009 to 2013.
Discussion
We analyzed BLL data for 124,376 children who presented to the clinic for regular checkups in Hunan Children’s Hospital from 2009 to 2013 and found that the median BLL for all children was 64.3μg/L. Both the BLLs and prevalence of EBLLs for boys were higher than for girls between 2009 and 2013. Overall, the BLLs and prevalence of EBLLs showed a clear downward trend from 2009 to 2013, but the trend showed a slight fluctuation from 2010 to 2012. The BLLs and prevalence of EBLLs increased with age in children in 2009 and 2010. The BLLs and prevalence of EBLLs increased with age until the age of five and then decreased for six-year-old children from 2011 to 2013.
In this study, the median BLL (64.3μg/L) and the prevalence of EBLLs (10.54%) for all children were different from other published literature in China. He K et al. analyzed articles published from 2004–2007 to assess the BLLs of Chinese children aged 0–14 years and found that the weighted mean BLL of 94,778 children was 80.7 μg/L and that 23.9% had an EBLL [12]. Li JM et al. showed that the mean BLL was 74.77 μg/L and that the prevalence of EBLLs was 20.05% in Changsha city among 1,431 children aged 0–6 years old [14]. The BLLs and prevalence of EBLLs in these previous studies were higher than in this study. There may be several explanations for this observation. First, besides leaded gasoline, other important sources of lead exposure, such as industrial emissions and lead-contaminated paints, have been gradually restricted by the government in recent years. In addition, the risk factors for high BLLs, such as eating (preserved eggs and canned food) and living habits (sucking and nail biting), have been recognized nationwide [15, 16]. Finally, the discrepancy may also be due to lead exposure in air, water and soil in different areas.
In 2008–2009, Etchevers A et al. demonstrated that the geometric mean of BLL was 14.9 μg/L and that the prevalence of BLLs exceeding 100 μg/L was 0.09% in a nationwide cross-sectional survey of children aged 6 months-6 years old in France [17]. Similarly, in the United States, the geometric mean of BLLs was 13 μg/L and the prevalence rate for confirmed EBLLs≥50 μg/L per 100 tested children was 2.6% in children aged 1–5 years according to the National Health and Nutrition Examination Survey 2007–2008 [18]. Obviously, the geometric mean BLL (64.24μg/L) in our study was higher than in Western countries. There are several possible explanations for this observation. First, the major source of lead exposure is household dust from deteriorating paint and tap water from lead branch pipes in western countries where the use of lead in paint and pipes was completely abolished in the 1970s [19]. However, the major lead sources in China may come primarily from the burning of fossil fuels; however, leaded petrol was not banned until 2000. Second, the prevalence of malnutrition, such as lower levels of calcium, iron, zinc and other elements, might increase the risk for enhanced absorption of ingested lead [19, 20]. With the improvement of living conditions, the intake of milk has improved the lack of trace elements in the diet, which may reduce intestinal lead absorption [20]. Finally, regional disparity, dietary habits, and ethnic difference may lead to the differences in BLLs and the prevalence of EBLLs [15, 21].
From the analysis, we found that boys had higher BLLs and a higher prevalence of lead poisoning than girls. The finding in our study is comparable to observations in the US and in Canada [22, 23]. The change may be due to several possible explanations. First, boys may be participated in more outdoors activities than girls, which results in higher lead exposure [24]. Second, boys are inclined to have behavioral patterns, such as being naughty; are active; and have worse health habits, which may lead to more lead absorption [25].
Both BLLs and the prevalence of EBLLs increased with aged from 0–6 years and reached a peak in children aged five or six years old. The phenomenon was consistent with previous studies in China [26, 27]. The explanation for this observation is that most of the primary Pb will be retained and more will continue to accumulate in the body tissues of children under conditions of continued exposure from inhalation of airborne Pb [28, 29] and a longer time line of ingestion and eat greater amounts [30, 31]. In addition, the heaviest lead-contaminated zone in air was 75–100 cm over ground, which is the same as the average height of pre-school and primary school children [32]. Finally, older children are more likely to participate in outdoor activities, which expose them to lead-contaminated environments. However, the BLLs and prevalence of EBLLs in children generally peaks approximately 18–30 months of age in the United States. This is likely because the major source of lead is household dust from deteriorating paint and some hand-to-mouth behaviors, such as crawling on the floor and putting hands and toys in the mouth, at that age [19]. Rahman A et al. demonstrated that the BLL in toddlers is associated with the BLL during pregnancy through the placenta and during breastfeeding [33]. Currently, experts in China strongly suggest that young couples who are ready to have children should have a blood lead measurement before pregnancy, which will lead to lower BLLs in pregnancy. This may be an important reason for the lower the blood lead level in the toddler group.
The findings show that from 2009 to 2013, 10.54% of the children in Hunan Province exceeded the Center for Disease Control and Prevention BLLs of concern (≥100μg/L). Moreover, the prevalence of EBLLs declined by 77% from 18.31% to 4.26% between 2009 and 2013. In China, compared with the studies in 1995–2003, both BLLs and the prevalence of EBLLs were lower in studies carried out after 2004 [12]. Li T et al. have shown that the prevalence of EBLLs(≥100μg/L) declined from 9.78% to 1.32% between 2004 and 2010 in China [34]. In Canada, the geometric mean BLL was 9 μg/L and fewer than 1% of children between 6 and 11 years old had EBLLs [35]. Kennedy BS et al. revealed that the prevalence of EBLL per 100 tested children decreased from 13.4 to 1.1 in Monroe County, 6.3 to 1.0 in New York State, and 7.6 to 0.6 in the United State between 1997 and 2011 [36].
The BLLs and prevalence of EBLLs have demonstrated a clear downward trend from 2009 to 2013, but the trend exhibited a slight fluctuation from 2010 to 2012 in our study. Regarding the downward trends in both BLLs and the prevalence of EBLLs, there are some explanations. First, the major cause of lower BLLs is attributable to government policies to decrease the amount of lead in air, dust and water. For example, leaded petrol has been completely banned in China since 2000, and heavy industry enterprises were closed down or rectified in China, which led to the reduction of lead emission. In addition, the Ministry of Environmental Protection formally promulgated “Clean Production Standards for the Lead Battery Industry” and implemented this policy in February 2009. Second, the risk factors of high blood lead levels, such as not washing hands before meals, eating paint, ink, or crayons, and frequently eating preserved eggs or canned food, have been recognized nationwide [37–39]. Furthermore, nutritional factors such as iron, zinc and calcium, are thought to play an important role in lead accumulation and poisoning [40, 41]. Therefore, parents pay more attention to children’s healthy eating and living habits, which has led to the reduction of lead exposure. Regarding the slight fluctuation from 2010 to 2012, this may be attributed to the lead-acid battery (LAB) industry. The production of lead-acid battery (LAB) goods, such as electric bikes, automobiles, and photovoltaic systems, dramatically increased in China. Moreover, China’s LAB industry is the world’s largest in terms of production and consumption, accounting for over 30% of global LAB output [42, 43] and using over 67% of China’s total Pb production [44]. However, the Ministry of Environmental Protection along with the National Development and Reform Commission jointly issued an environmental protection special action decree in March 2011. With the enforcement of the decree, 1930 LAB enterprises were completely shut down and 405 LAB enterprise operations were suspended for rectification. Therefore, the rapid development of China’ lead-acid battery industry may be responsible for a slight fluctuation of EBLLs from 2010 to 2012.
Limitations
Our study has some limitations. First, all subjects were outpatients for regular checkups at the largest tertiary hospital. These children might be from families with higher income or more educated parents Thus, there is a selection bias in this study. Second, we were not able to collect confounding information, such as parents’ education and occupation, family income, drinking water sources, living location and so on, which previous studies have been shown to have a link to EBLLs.
Conclusion
In conclusion, blood lead levels in children have declined substantially from 2009 to 2013 in Hunan Province in China; however, the prevalence of elevated lead levels in children remains unacceptably high compared to developed countries. Hence, the government should initiate measures to improve health behaviors, such as washing hands before eating and eating food enriched with iron, zinc and/or calcium.
Acknowledgments
The authors are indebted to all outpatients who volunteered to participate in the study. We are also grateful to Niziri for the language input. We also appreciate all of the support of the data collectors.
Data Availability
All relevant data are within the paper.
Funding Statement
This study was supported by a grant from the Ministry of Science and Technology in China (Grant#:2012GS430101 and Grant#:2012BAI04B01). The funding institution had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. No additional external funding was given to the study.
References
- 1. Canfield RL, Henderson CR Jr., Cory-Slechta DA, Cox C, Jusko TA, Lanphear BP. Intellectual impairment in children with blood lead concentrations below 10 microg per deciliter. N Engl J Med. 2003;348(16):1517–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rogan WJ, Ware JH. Intellectual impairment in children with blood lead concentrations below 10 microg per deciliter. J Pediatr. 2003;143(5):687–8. [PubMed] [Google Scholar]
- 3. Jusko TA, Henderson CR, Lanphear BP, Cory-Slechta DA, Parsons PJ, Canfield RL. Blood lead concentrations < 10 microg/dL and child intelligence at 6 years of age. Environ Health Perspect. 2008;116(2):243–8. 10.1289/ehp.10424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Surkan PJ, Zhang A, Trachtenberg F, Daniel DB, McKinlay S, Bellinger DC. Neuropsychological function in children with blood lead levels <10 microg/dL. Neurotoxicology. 2007;28(6):1170–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Glenn BS, Bandeen-Roche K, Lee BK, Weaver VM, Todd AC, Schwartz BS. Changes in systolic blood pressure associated with lead in blood and bone. Epidemiology. 2006;17(5):538–44. [DOI] [PubMed] [Google Scholar]
- 6. Kim R, Rotnitsky A, Sparrow D, Weiss S, Wager C, Hu H. A longitudinal study of low-level lead exposure and impairment of renal function. The Normative Aging Study. JAMA. 1996;275(15):1177–81. [PubMed] [Google Scholar]
- 7. Gennart JP, Buchet JP, Roels H, Ghyselen P, Ceulemans E, Lauwerys R. Fertility of male workers exposed to cadmium, lead, or manganese. Am J Epidemiol. 1992;135(11):1208–19. [DOI] [PubMed] [Google Scholar]
- 8. NTP (National Toxicology Program). Monograph on Health Effects of Low Level Lead. U.S. Department of Health and Human Services, Washington, DC: 2012; Available: http://ntp.niehs.nih.gov/go/36443. [Google Scholar]
- 9. Liu J, Li L, Wang Y, Yan C, Liu X. Impact of low blood lead concentrations on IQ and school performance in Chinese children. PLoS One. 2013;8(5):e65230 10.1371/journal.pone.0065230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cleveland LM, Minter ML, Cobb KA, Scott AA, German VF. Lead hazards for pregnant women and children: part 1: immigrants and the poor shoulder most of the burden of lead exposure in this country. Part 1 of a two-part article details how exposure happens, whom it affects, and the harm it can do. Am J Nurs. 2008;108(10):40–9; quiz 50. 10.1097/01.NAJ.0000337736.76730.66 [DOI] [PubMed] [Google Scholar]
- 11. Abadin H, Ashizawa A, Stevens YW, Llados F, Diamond G, Sage G, et al. Agency for Toxic Substances and Disease Registry Toxicological Profile for Lead. Atlanta, GA: Public Health Service; 2007. [PubMed] [Google Scholar]
- 12. He K, Wang S, Zhang J. Blood lead levels of children and its trend in China. Sci Total Environ. 2009;407(13):3986–93. 10.1016/j.scitotenv.2009.03.018 [DOI] [PubMed] [Google Scholar]
- 13. van der Kuijp TJ, Huang L, Cherry CR. Health hazards of China's lead-acid battery industry: a review of its market drivers, production processes, and health impacts. Environ Health. 2013;12:61 10.1186/1476-069X-12-61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Li JM, Yi ZW, Luo XM, Sun XH, Jin Y, Li YP, et al. An epidemiological study on blood lead level among childrenaged 0–6 years in Changsha. CHINESE JOURNAL OF EPIDEMIOLOGY. 2005;22(7). [Google Scholar]
- 15. Schnur J, John RM. Childhood lead poisoning and the new Centers for Disease Control and Prevention guidelines for lead exposure. J Am Assoc Nurse Pract. 2014;26(5):238–47. 10.1002/2327-6924.12112 [DOI] [PubMed] [Google Scholar]
- 16. Li Y, Wu S, Xiang Y, Liang X. An investigation of outpatient children's blood lead level in Wuhan China. PLoS One. 2014;9(4):e95284 10.1371/journal.pone.0095284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Etchevers A, Bretin P, Lecoffre C, Bidondo ML, Le Strat Y, Glorennec P, et al. Blood lead levels and risk factors in young children in France, 2008–2009. Int J Hyg Environ Health. 2014;217(4–5):528–37. [DOI] [PubMed] [Google Scholar]
- 18. CDC. National Health and Nutrition Examination Survey 2007–2008 data documentation, codebook, and frequencies Hyattsville, MD: US Department of Health and Human Services, CDC, National Center for Health Statistics; 2009; Available: http://www.cdc.gov/nchs/nhanes/nhanes2007-2008/pbcd_e.htm. [Google Scholar]
- 19. Chandran L, Cataldo R. Lead poisoning: basics and new developments. Pediatr Rev. 2010;31(10):399–405; quiz 6. 10.1542/pir.31-10-399 [DOI] [PubMed] [Google Scholar]
- 20. Baker RD, Greer FR. Diagnosis and prevention of iron deficiency and iron-deficiency anemia in infants and young children (0–3 years of age). Pediatrics. 2010;126(5):1040–50. 10.1542/peds.2010-2576 [DOI] [PubMed] [Google Scholar]
- 21.New York City [NYC] Department of Health and Mental Hygiene. Lead poisoning in New York City, Annual Data Report. New York City. 2009; Available: www.nyc.gov/lead.
- 22. Blood lead levels in children aged 1–5 years—United States, 1999–2010. MMWR Morb Mortal Wkly Rep. 2013;62(13):245–8. [PMC free article] [PubMed] [Google Scholar]
- 23. Health Canada. Second Report on Human Biomonitoring of Environmental Chemicals in Canada: Health Canada; 2013; Available: http://www.hc-sc.gc.ca/ewh-semt/pubs/contaminants/chms-ecms-cycle2/index-eng.php [Google Scholar]
- 24. Freeman NC, Jimenez M, Reed KJ, Gurunathan S, Edwards RD, Roy A, et al. Quantitative analysis of children's microactivity patterns: The Minnesota Children's Pesticide Exposure Study. J Expo Anal Environ Epidemiol. 2001;11(6):501–9. [DOI] [PubMed] [Google Scholar]
- 25. Ko S, Schaefer PD, Vicario CM, Binns HJ. Relationships of video assessments of touching and mouthing behaviors during outdoor play in urban residential yards to parental perceptions of child behaviors and blood lead levels. J Expo Sci Environ Epidemiol. 2007;17(1):47–57. [DOI] [PubMed] [Google Scholar]
- 26. Liu J, Ai Y, McCauley L, Pinto-Martin J, Yan C, Shen X, et al. Blood lead levels and associated sociodemographic factors among preschool children in the South Eastern region of China. Paediatr Perinat Epidemiol. 2012;26(1):61–9. 10.1111/j.1365-3016.2011.01234.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Xie XH, Tan ZW, Jia N, Fan ZY, Zhang SM, Lu YY, et al. Blood lead levels among children aged 0 to 6 years in 16 cities of China, 2004–2008. Chin Med J (Engl). 2013;126(12):2291–5. [PubMed] [Google Scholar]
- 28. Jun L, Chunbao S, Yun L, Jiangang L, Dian J, Wendan L. Concentration of Lead in Atmosphere and Emission Characteristics of Pollution SourCeS in China. Environmental Protection of Chemical Industry. 2009;29(4):376–80. [Google Scholar]
- 29. Meng Q, Richmond-Bryant J, Davis JA, Cohen J, Svendsgaard D, Brown JS, et al. Contribution of particle-size-fractionated airborne lead to blood lead during the National Health and Nutrition Examination Survey, 1999–2008. Environ Sci Technol. 2014;48(2):1263–70. 10.1021/es4039825 [DOI] [PubMed] [Google Scholar]
- 30. Maduabuchi JM, Nzegwu CN, Adigba EO, Aloke RU, Ezomike CN, Okocha CE, et al. Lead and cadmium exposures from canned and non-canned beverages in Nigeria: a public health concern. Sci Total Environ. 2006;366(2–3):621–6. [DOI] [PubMed] [Google Scholar]
- 31. Akinyele IO, Shokunbi OS. Concentrations of Mn, Fe, Cu, Zn, Cr, Cd, Pb, Ni in selected Nigerian tubers, legumes and cereals and estimates of the adult daily intakes. Food Chem. 2015;173:702–8. 10.1016/j.foodchem.2014.10.098 [DOI] [PubMed] [Google Scholar]
- 32. Wang S, Zhang J. Blood lead levels in children, China. Environ Res. 2006;101(3):412–8. [DOI] [PubMed] [Google Scholar]
- 33. Rahman A, Al-Rashidi HA, Khan AR. Association of maternal blood lead level during pregnancy with child blood lead level and pregnancy outcome in Kuwait. Ecol Food Nutr. 2012;51(1):40–57. 10.1080/03670244.2012.635571 [DOI] [PubMed] [Google Scholar]
- 34. Li T, Dai YH, Xie XH, Tan ZW, Zhang SM, Zhu ZH. Surveillance of childhood blood lead levels in 11 cities of China. World J Pediatr. 2014;10(1):29–37. 10.1007/s12519-014-0452-6 [DOI] [PubMed] [Google Scholar]
- 35. Wong SL, Lye EJ. Lead, mercury and cadmium levels in Canadians. Health Rep. 2008;19(4):31–6. [PubMed] [Google Scholar]
- 36. Kennedy BS, Doniger AS, Painting S, Houston L, Slaunwhite M, Mirabella F, et al. Declines in elevated blood lead levels among children, 1997–2011. Am J Prev Med. 2014;46(3):259–64. 10.1016/j.amepre.2013.11.007 [DOI] [PubMed] [Google Scholar]
- 37. Malcoe LH, Lynch RA, Keger MC, Skaggs VJ. Lead sources, behaviors, and socioeconomic factors in relation to blood lead of native american and white children: a community-based assessment of a former mining area. Environ Health Perspect. 2002;110 Suppl 2:221–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Piomelli S. Childhood lead poisoning. Pediatr Clin North Am. 2002;49(6):1285–304. [DOI] [PubMed] [Google Scholar]
- 39. von Lindern I, Spalinger S, Petroysan V, von Braun M. Assessing remedial effectiveness through the blood lead:soil/dust lead relationship at the Bunker Hill Superfund Site in the Silver Valley of Idaho. Sci Total Environ. 2003;303(1–2):139–70. [DOI] [PubMed] [Google Scholar]
- 40. Keramati MR, Manavifar L, Badiee Z, Sadeghian MH, Farhangi H, Mood MB. Correlation between blood lead concentration and iron deficiency in Iranian children. Niger Med J. 2013;54(5):325–8. 10.4103/0300-1652.122353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wang H, Shi H, Chang L, Zhang X, Li J, Yang Y, et al. Association of blood lead with calcium, iron, zinc and hemoglobin in children aged 0–7 years: a large population-based study. Biol Trace Elem Res. 2012;149(2):143–7. 10.1007/s12011-012-9413-x [DOI] [PubMed] [Google Scholar]
- 42. Chen HY, Li AJ, Finlow DE. The lead and lead-acid battery industries during 2002 and 2007 in China. J Power Sources. 2009;191:22–7. [Google Scholar]
- 43.Research in China. China BI portal- China lead-acid battery industry report, 2011–2012. 2012; Available: http://www.researchinchina.com/htmls/report/2012/6394.html.
- 44. Chen L, Xu Z, Liu M, Huang Y, Fan R, Su Y, et al. Lead exposure assessment from study near a lead-acid battery factory in China. Sci Total Environ. 2012;429:191–8. 10.1016/j.scitotenv.2012.04.015 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.