Abstract
Background
Financial incentives and peer networks could be delivered through eHealth technologies to encourage older adults to walk more.
Methods
We conducted a 24-week randomized trial in which 92 older adults with a computer and internet access received a pedometer, daily walking goals, and weekly feedback on goal achievement. Participants were randomized to weekly feedback only (Comparison), entry into a lottery with potential to earn up to $200 each week walking goals were met (Financial Incentive), linkage to 4 other participants through an online message board (Peer Network), or both interventions (Combined). Main outcomes were the proportion of days walking goals were met during the 16-week intervention and 8-week follow-up. We conducted a content analysis of messages posted by Peer Network and Combined arm participants.
Results
During the 16-week intervention, there were no differences in the proportion of days walking goals were met in the Financial Incentive (39.7%; P = 0.78), Peer Network (24.9%; P = 0.08), and Combined (36.0%; P = 0.77) arms compared to the Comparison arm (36.0%). During 8 weeks of follow-up, the proportion of days walking goals were met was lower in the Peer Network arm (18.7%; P = 0.025), but not in the Financial Incentive (29.3%; P = 0.50) or Combined (24.8%; P = 0.37) arms, relative to the Comparison arm (34.5%). Messages posted by participants focused on barriers to walking and provision of social support.
Conclusions
Financial incentives and peer networks delivered through eHealth technologies did not result in older adults walking more.
Keywords: Financial incentives, behavioral economics, eHealth, walking, older adults
INTRODUCTION
Regular physical activity is associated with a decreased risk of obesity, heart disease, hypertension, diabetes, and premature mortality (Physical Activity Guidelines Advisory Committee, 2008; U.S. Department of Health and Human Services, 1996). However, less than half of all adults engage in regular physical activity (Centers for Disease Control and Prevention, 2007). Of all adults, those aged 65 and older are the least likely to be physically active, even though exercise in this group may have unique health benefits (Angevaren, Aufdemkampe, Verhaar, Aleman, & Vanhees, 2008; Stessman, Hammerman-Rozenberg, Cohen, Ein-Mor, & Jacobs, 2009).
One type of physical activity that is broadly applicable to the older adult population is walking. This activity does not require additional resources or training, is feasible and safe, has individual targets that are associated with health improvements (Tudor-Locke & Bassett, 2004; Tudor-Locke, Hart, & Washington, 2009), and can be tracked through highly-scalable eHealth technologies (Carr et al., 2013; Richardson et al., 2010).
Two strategies that capitalize on eHealth technologies and leverage advances in decision science hold particular promise for encouraging walking among older adults: financial incentives and peer networks. First, financial incentives are behavioral economic interventions that capitalize on people’s difficulty trading off immediate gratification for delayed health benefits (Loewenstein, Brennan, & Volpp, 2007). These strategies have tripled long-term tobacco cessation rates, increased weight loss, and improved medication adherence (Kimmel et al., 2012; Kullgren et al., 2013; Volpp et al., 2009). Such extrinsic rewards for engaging in a behavior may be particularly effective among individuals who exhibit more controlled motivation than autonomous motivation for the behavior (Ryan & Deci, 2000). While multiple recent studies have tested financial incentives for healthy behaviors, little research has examined whether financial incentives can promote walking among older adults (Mitchell et al., 2013). The only recent study in this area tested one variable, fixed weekly payout schedule for 4 weeks among adults with a mean age of 60 (Finkelstein, Brown, Brown, & Buchner, 2008). Second, connections within social networks have been shown to influence health behaviors (Christakis, 2004; Seeman, 1996). In the elderly, social networks can have benefits for individuals who are socially isolated (Cornwell & Waite, 2009; Golden, Conroy, & Lawlor, 2009; Seeman, 2000) and provide beneficial social comparisons (Carrieri, 2012; Yun & Silk, 2011). Because social networks evolve naturally, however, constructing a social network de novo is infeasible. An alternative strategy that might afford some interpersonal dynamics of a social network is an online “peer network”: a collection of similar persons who are engaged in individual but shared goals. This approach capitalizes on the efficacy of peer support in managing chronic diseases (Harvey, Eime, & Payne, 2009; Heisler et al., 2007; Heisler & Piette, 2005), older adults’ preferences for programs outside of a formal group setting (Brown, Finkelstein, Brown, Buchner, & Johnson, 2009), and evidence that online groups can increase social support and quality of life (Rains & Young, 2009). Existing research on peer support interventions, however, has focused mostly on internet-mediated peer support for managing chronic conditions like depression (Griffiths, Calear, Banfield, & Tam, 2009; Melling & Houguet-Pincham, 2011), diabetes (Ramadas, Quek, Chan, & Oldenburg, 2011), and cancer (Hoey, Ieropoli, White, & Jefford, 2008; Hong, Pena-Purcell, & Ory, 2012). The few internet-mediated peer support interventions that have sought to promote physical activity have focused on younger adults (Carr et al., 2013; Chang, Chopra, Zhang, & Woolford, 2013).
The goals of this trial were to (1) test whether financial incentives and peer networks delivered through eHealth technologies increase walking among older adults and (2) to gain preliminary insights into the effects of these strategies through online messages posted by participants. We hypothesized that financial incentives, peer networks, and their combination would increase walking relative to a comparison group that did not receive these interventions.
RESEARCH METHODS
Setting and Participants
Our entire study protocol was approved by the Institutional Review Board of the University of Pennsylvania. Participants were adults at least 65 years of age who had a computer with a high-speed internet connection, could walk ¼ mile without stopping, had not recently used a pedometer, and wanted to be more physically active. Exclusion criteria included recent myocardial infarction, stroke, or orthopedic surgery; severe cardiac, lung, renal, or rheumatologic disease; dementia or a movement disorder; a major psychiatric disorder; or excessive alcohol consumption. Participants were recruited from March 2011 to February 2012 through opt-in mailings and web advertisements to United Health Group Supplemental Health Insurance Plan enrollees, flyers at Philadelphia retirement communities and an AARP member event, postings on an AARP internet message board, and email and letters to cognitively normal volunteers from a Penn Memory Center longitudinal cohort study who had previously consented to be contacted about research studies.
Randomization and Interventions
Participants completed screening and enrollment through a study website. Individuals who consented were mailed a Fitbit pedometer (www.fitbit.com). Upon receipt of the pedometer, participants entered a 14 day run-in period to measure their baseline level of walking. During this period, they wore their pedometer each day and connected their pedometer to their computer each night. To account for the monitoring effects of pedometer use (Bravata et al., 2007), we measured baseline daily steps using only data from days 8 to 14. Once baseline levels of walking were established, participants were given the goal of increasing their daily steps by 50% in 5 days per week for the next 16 weeks. For example, a participant who walked an average of 5,000 steps per day was given a walking goal of 7,500 steps per day. This goal was based on the proportional increase that would be needed for most community-dwelling older adults (Tudor-Locke et al., 2009) to achieve a level of walking associated with higher quality of life, better measures of immunity, and improved weight status (Tudor-Locke et al., 2011). Participants did not receive specific instructions on how to increase their steps, but were provided with links to information about exercise and walking from the National Institutes of Health.
Following establishment of walking goals, the study coordinator requested arm assignment via a web-based platform which assigned participants to the 4 study arms using 1:1:1:1 central computerized randomization. The allocation sequence was generated dynamically by the randomization program and research team members were unable to predict future assignments. Arm assignments were communicated to participants via an automated website message and email or text message. Neither participants nor the study coordinator could be blinded to arm assignment due to the nature of the interventions. Data analysts and all investigators were blinded to arm assignment until collection of primary outcome data was complete.
Comparison arm participants wore their pedometers each day and uploaded their walking data each evening. Each morning they received an automated email or text message that their data were received by the server. Each week participants received automated email or text feedback about how often they met their walking goal in the past week. Although each of these features had the potential to affect walking behaviors, their inclusion was necessary to isolate the effects of financial incentives and peer networks on walking behaviors.
Financial Incentive arm participants received the same information as Comparison arm participants. In addition, each week they were entered into a lottery with a 3 in 10 chance of winning $50 (a higher frequency smaller reward) and a 3 in 100 chance of winning $200 (a lower frequency larger reward). This lottery incentive aimed to leverage common decision biases like overoptimism (Svenson, 1981) and overweighting of small probabilities (Kahneman & Tversky, 1979), relative to a fixed payout with an equivalent expected value. We used an expected value for the lottery of approximately $21 per week because it is comparable to the magnitude of incentives that have been used in other health behavior research (Kullgren et al., 2013; Volpp, John, et al., 2008). Participants received lottery winnings only if they had met their walking goals in 5 of the past 7 days. In each intervention week, participants received an automated email or text message that described how often they had met their walking goals in the last 7 days, whether they had won money in the lottery, or whether they would have won money in the lottery if only they had met their walking goals.
Peer Network arm participants received the same information as Comparison arm participants and were provided access to an online message board where they could communicate with 4 other participants. At the beginning of the intervention period, participants received a list of ways in which the peer network could be used to support achievement of walking goals (e.g., posting tips or words of encouragement, sharing contact information to enable connections outside of the message board, or organizing group walks). Each week, a list of participants in the peer network who met their walking goals in 5 of the last 7 days was posted to the message board.
Subjects randomized to the Combined arm received the interventions that Financial Incentive and Peer Network arm participants received. Each week in each peer network, a list of participants who met their walking goals in 5 of the last 7 days and a list of participants who won money in the lottery was posted to the message board.
After the 16-week intervention, all participants entered an 8-week follow-up period during which the financial incentive and peer network interventions were no longer available but participants continued to wear their pedometers and upload their walking data. They continued to receive daily automated messages that their step counts were received and weekly automated messages about how often they had met their walking goal in the previous 7 days.
Baseline Survey
We used an online survey to collect baseline data from participants on their gender, age, household size, educational attainment, employment status, annual household income, race/ethnicity, and health status. The survey also included the Treatment Self-Regulation Questionnaire (TSRQ) to collect data on participants’ motivation for increasing their walking (Ryan & Connell, 1989). The TSRQ includes subscales that measure autonomous motivation, controlled motivation, and amotivation for a behavior. Scores for these 3 subscales can be combined into an aggregate measure termed the Relative Autonomy Index (RAI), in which higher scores indicate more autonomous motivation and lower scores denote more controlled motivation.
Outcomes
The primary outcome was the proportion of days in which daily step goals were met during the 16-week intervention. Secondary outcomes included the proportion of days in which step goals were met during the 8 week follow-up period, change in mean daily steps during the 16-week intervention period, and change in mean daily steps during the 8 week follow-up period.
Content Analysis
We conducted an exploratory content analysis of messages posted to the online message boards (Gilbert & Omisore, 2009; Hoffman-Goetz & Donelle, 2007) by Peer Network and Combined arm participants. Two coders blind to the hypotheses coded the messages for information support, tangible support, esteem support, network support, and emotional support (Cutrona & Suhr, 1992) as well as references to barriers to meeting walking goals. Discrepant posts were analyzed by a third coder to determine the final count. The average kappa was 0.71.
Statistical Quantitative Data Analysis
All analyses were intent-to-treat testing for differences between the 4 arms. For the primary outcome we used generalized estimation equation regression to model longitudinal change in rates of meeting walking goals, adjusted for baseline levels of walking, to obtain robust standard errors based on repeated observations of participants. For the secondary outcome analyses we used mixed effects regression to model longitudinal change in rates of meeting walking goals adjusted for baseline levels of walking and mean change in daily steps from baseline. All hypothesis tests were 2-sided and used a Holm-Bonferroni approach to maintain the Type I error rate while testing multiple hypotheses. We used SAS Version 9.3 to analyze the data.
Assuming approximate normality for the proportions, we determined a sample of 80 participants would provide 85% power to detect an absolute increase of 0.2 in the proportion of days in which step per day goals were met. This calculation used a Holm-Bonferroni correction to maintain an overall Type I Error rate of 5% and assumed no interaction between the incentives and the peer network. To account for dropout at rates observed in similar randomized trials (Angevaren et al., 2008), we applied a 25% inflation factor and aimed to enroll 100 subjects.
RESULTS
We recruited 92 participants (Figure 1) who were on average 71.9 years old. Seventy percent were female and 93% were Caucasian (data not in Tables). Most (83%) had at least a bachelor’s degree (i.e., they were a college graduate or post-college graduate) and 74% were retired. Nearly three quarters (73%) were in excellent or very good health. Participants had high RAI scores (Ryan & Connell, 1989), indicating high levels of autonomous motivation to increase their walking. At baseline, participants walked an average of 6,405 steps per day which translated into an average daily goal of 9,597 steps. Participants in the Combined arm had higher levels of mean baseline steps (7,721) than participants in the Peer Network arm (5,242; P = 0.005).
Figure 1.
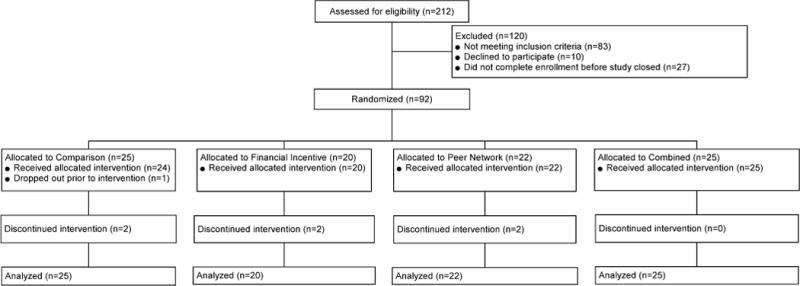
Study flow
Eighty-five participants (92%) completed the 16-week intervention. There were no differences in the mean proportion of days walking goals were met in the Financial Incentive (39.7%, 95% CI 26.6%, 52.8%; P = 0.78), Peer Network (24.9%, 95% CI 13.7%, 36.0%; P = 0.08), and Combined (36.0%, 95% CI 23.4%, 48.5%; P = 0.77) arms relative to the Comparison arm (36.0%, 95% CI 24.3%, 47.6%) (Figure 2). There were no differences in mean change in daily steps in the Financial Incentive (1,361, 95% CI −628, 3,350; P = 0.84), Peer Network (833, 95% CI −1,256, 2,922; P = 0.51), and Combined (1,178, 95% CI −1,081, 3,437; P = 0.93) arms relative to the Comparison arm (1,247, 95% CI 411, 2,082).
Figure 2.
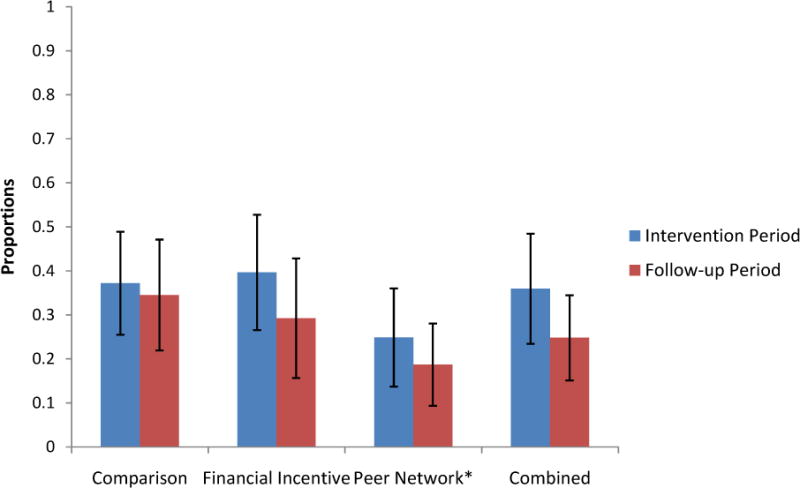
Mean proportions of days in which step goals were met
Vertical black lines represent 95% confidence intervals for each mean proportion.
*P = .025 for difference in mean proportion of Follow-up Period days in which step goals were met between Peer Network (18.7%) and Comparison (34.5%) arms.
To gauge the robustness of our findings to alternative analytic approaches and examine additional hypotheses, we conducted several exploratory post hoc analyses. First, we analyzed the data for both outcomes as a 2 × 2 factorial design study and our results were qualitatively unchanged. Second, we tested for evidence of late (i.e., weeks 9–16) vs. early (i.e., weeks 1–8) intervention effects and found none. Third, we examined whether the intervention arms had greater changes in physical activity relative to the Comparison group and found no significant differences in mean change in weekly minutes of moderate or vigorous physical activity from baseline to 16 weeks. Fourth, in the Financial Incentive and Combined arms there were no differences in the amount of incentives earned.
Eight-five participants (92%) completed the 8 week follow-up period. The mean proportion of days walking goals were met was lower in the Peer Network arm (18.7%, 95% CI 9.4%, 28.1%; P = 0.025), but not in the Financial Incentive (29.3%, 95% CI 15.7%, 42.8%; P = 0.50) or Combined (24.8%, 95% CI 15.1%, 34.5%; P = 0.37) arms, relative to the Comparison arm (34.5%, 95% CI 21.9%, 47.1%) (Figure 2). There were no differences in mean change in daily steps from baseline in the Financial Incentive (559, 95% CI −1,866, 2,984; P = 0.42), Peer Network (279, 95% CI −1,969, 2,527; P = 0.18), and Combined (309, 95% CI −2,172, 2,791; P = 0.27) arms compared to the Comparison arm (1,151, 95% CI 162, 2,140).
In the content analysis, there was variation in the number of Peer Network and Combined arm message posts by individual (median 1 post, range 0 to 27 posts) and peer group (median 5 posts, range 0 to 71 posts). Nearly half of participants (47%) never posted a message. One third of posts focused on barriers to meeting walking goals (Table 2). The content of these messages discussed goals that were perceived to be too high, environmental limitations to walking, illness, travel, forgetting to wear the pedometer, and technological difficulties. More than half of posts conveyed social support. The most common form was esteem support such as notes of congratulation or acknowledgement of group members’ efforts. Of all supportive posts, only esteem posts differed statistically across arms, with more esteem posts in the Peer Network arm than in the Combined arm (55 vs. 12, P < 0.01). One fifth of all posts demonstrated informational support such as tips on how to meet walking goals or navigate logistical challenges with the pedometer and website. Emotionally supportive posts were the least common, and involved expressions of concerns for group members’ well-being or sympathetic responses to frustrations with the website.
Table 2.
Themes from online message board posts
| Characteristic | Peer Network arm (n = 22) |
Combined arm (n = 25) |
||
|---|---|---|---|---|
| # posts | % | # posts | % | |
| Barriers to meeting goals | 33 | 31 | 17 | 38 |
| Types of support | ||||
| Informational | 18 | 17 | 12 | 27 |
| Esteem | 55 | 52 | 12 | 27* |
| Emotional | 17 | 16 | 3 | 9 |
| Total posts | 105 | 45 | ||
P < .01 compared to Peer Network arm.
DISCUSSION
In this mixed methods randomized controlled trial we found that financial incentives and peer networks delivered through eHealth technologies did not lead to more walking among older adults. These results suggest a lower-dose intervention that utilizes a pedometer, goal setting, and regular feedback on goal attainment may be as effective in promoting walking among older adults as higher-dose interventions using financial incentives, peer networks, or both. Our study also provides important preliminary data on the effects of these strategies and suggests ways in which these approaches might be enhanced to have greater effectiveness among older adults.
There are several possible reasons why the financial incentive intervention was not effective. First, although many participants had baseline levels of walking comparable to most community-dwelling adults (Tudor-Locke et al., 2009), others had high baseline levels of walking that produced high daily step goals which may have been difficult to achieve. Also, our approach sought an immediate increase in walking that may have been less effective than encouraging gradual increases (Finkelstein et al., 2008; Moy, Weston, Wilson, Hess, & Richardson, 2012; Richardson et al., 2007). Second, our incentive design provided weekly feedback. Daily feedback similar to what has been successful in other studies (Finkelstein et al., 2008; Kimmel et al., 2012; Volpp, John, et al., 2008) might have been more effective. Third, participants reported high baseline levels of autonomous motivation to increase their walking. Financial incentives could be less effective among these types of individuals than among individuals who exhibit more controlled motivation (Ryan & Deci, 2000). Fourth, we tested one type of lottery incentive. A variety of other approaches are possible (Mitchell et al., 2013) and this is a fruitful area for future research.
Similarly, there are several potential reasons why the peer network intervention did not increase walking. First, nearly half of participants did not post any online messages. This suggests that for a significant number of individuals message boards may not be successful ways to encourage communication. Next, while a subset of participants used the message board to share and solicit emotional and esteem support from their peers, many individuals used the space to share frustrations with their inability to meet walking goals. Such messages may have created a perceived social norm that diminished motivation (Yun & Silk, 2011). This dynamic may have carried over into the follow-up period when Peer Network arm participants met their walking goals less often than Comparison arm participants. Interestingly, less esteem support was provided in the Combined arm than in the Peer Network arm. This difference may suggest the presence of financial incentives changed how participants interacted with one another. Finally, it is possible that smaller or larger peer networks could have been more effective. More research is needed to determine the effective ingredients of group-based interventions.
Our study has limitations. First, participants were highly educated, primarily white, and had very high health status which limits external validity. Second, our strategy for calculating walking goals often led to high step goals that may have been difficult for participants to achieve. Alternative targets for financial incentive or peer support interventions would be valuable areas to explore in future work. Third, the intervention and follow-up periods were fairly short. Fourth, we did not ask participants about their views of the financial incentive and peer network interventions. Thus, we are unable to discern the exact reasons for why they were not effective. Fifth, smaller sample sizes limit our ability to examine whether participant characteristics such as locus of motivation predicted response to the interventions.
CONCLUSIONS
In conclusion, interventions that use eHealth technologies have great potential to improve health behaviors among older adults. Although we found that financial incentives and peer networks did not lead to more walking among older adults, our results suggest that delivery of such interventions through wireless devices and the internet is highly feasible. Given the promise of these approaches to foster engagement and independence among community-dwelling older adults, more evidence is needed to determine how such interventions can be optimized to improve health and health behaviors in this population.
Table 1.
Participant characteristics
| Characteristic | Peer Network (n = 22) |
Financial Incentive (n = 20) |
Combined (n = 25) |
Comparison (n = 25) |
|---|---|---|---|---|
| N (%) or Mean (SD) | ||||
| Female, n (%)a | 16 (72.7) | 15 (75.0) | 15 (62.5) | 18 (72.0) |
| Age, mean (SD) | 71.9 (5.6) | 72.4 (5.8) | 71.9 (5.8) | 71.5 (5.1) |
| Household residents, mean (SD) | 1.9 (0.6) | 2.0 (1.3) | 1.9 (0.4) | 1.7 (0.5) |
| Education, n (%) | ||||
| Less than college graduate | 2 (9.1) | 3 (15.0) | 1 (4.0) | 10 (40.0) |
| College graduate | 4 (18.2) | 3 (15.0) | 10 (40.0) | 5 (20.0) |
| Post-college degree | 16 (72.7) | 14 (70.0) | 14 (56.0) | 10 (40.0) |
| Employment status, n (%)b | ||||
| Employed for wages | 5 (22.7) | 2 (10.0) | 3 (12.5) | 0 (0.0) |
| Self-employed | 1 (4.5) | 2 (10.0) | 4 (16.7) | 3 (12.0) |
| Homemaker | 0 (0.0) | 2 (10.0) | 1 (4.2) | 1 (4.0) |
| Retired | 16 (72.7) | 14 (70.0) | 16 (66.7) | 21 (84.0) |
| Annual household income, n (%)c | ||||
| < $50,000 | 6 (28.6) | 6 (30.0) | 5 (20.8) | 9 (40.9) |
| $50,000 to < $100,000 | 11 (52.4) | 9 (45.0) | 13 (54.2) | 9 (40.9) |
| ≥ $100,000 | 4 (19.0) | 5 (25.0) | 6 (25.0) | 4 (18.2) |
| Race/ethnicity, n (%)d | ||||
| White, non-Hispanic | 21 (95.5) | 19 (95.0) | 22 (91.7) | 23 (92.0) |
| African American, non-Hispanic | 0 (0.0) | 0 (0.0) | 2 (8.3) | 0 (0.0) |
| Other non-Hispanic | 1 (4.5) | 1 (5.0) | 0 (0.0) | 0 (0.0) |
| Hispanic | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (8.0) |
| Health status, n (%)e | ||||
| Excellent | 1 (4.5) | 0 (0.0) | 7 (29.2) | 2 (8.0) |
| Very good | 14 (63.6) | 15 (75.0) | 12 (50.0) | 15 (60.0) |
| Good | 6 (27.3) | 5 (25.0) | 5 (20.8) | 6 (24.0) |
| Fair or poor | 1 (4.5) | 0 (0.0) | 0 (0.0) | 2 (8.0) |
| Motivation to increase walking, mean (SD) | ||||
| Autonomous motivation | 6.3 (0.8) | 6.5 (0.6) | 6.4 (0.8) | 6.3 (0.8) |
| Controlled motivation | 2.3 (1.0) | 2.2 (1.2) | 2.0 (0.9) | 2.1 (0.8) |
| Amotivation | 1.8 (0.7) | 1.5 (0.7) | 2.2 (1.2) | 2.0 (0.7) |
| Relative autonomy indexf | 3.9 (1.0) | 4.3 (1.4) | 4.4 (1.4) | 4.2 (1.1) |
| Baseline steps per day, mean (SD) | 5242 (2433) | 5856 (2240) | 7721 (3616)g | 6420 (2997) |
Gender missing for 1 participant in the Combined arm.
Employment status missing for 1 participant in the Combined arm.
Household income missing for 1 participant in the Peer Network arm, 1 participant in the Combined arm, and 3 participants in the Comparison arm.
Race/ethnicity missing for 1 participant in the Combined arm.
Health status missing for 1 participant in the Combined arm.
Higher scores indicate more autonomous motivation and lower scores denote more controlled motivation.
Significantly different from Peer Network arm (P = 0.005).
Acknowledgments
Funding/support: This work was supported by grant RC2103282621 from the National Institute on Aging (Mult PIs Volpp and Asch). Support was also provided by the Department of Veterans Affairs and the Robert Wood Johnson Foundation. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Contributor Information
Jeffrey T. Kullgren, Email: jkullgre@med.umich.edu.
Kristin A. Harkins, Email: kristin.harkins@uphs.upenn.edu.
Scarlett L. Bellamy, Email: bellamys@mail.med.upenn.edu.
Amy Gonzales, Email: gonzaamy@indiana.edu.
Yuanyuan Tao, Email: ytao@mail.med.upenn.edu.
Jingsan Zhu, Email: jingsan@mail.med.upenn.edu.
Kevin G. Volpp, Email: volpp70@exchange.upenn.edu.
David A. Asch, Email: asch@wharton.upenn.edu.
Michele Heisler, Email: jkullgre@med.umich.edu.
Jason Karlawish, Email: Jason.Karlawish@uphs.upenn.edu.
References
- Angevaren M, Aufdemkampe G, Verhaar HJ, Aleman A, Vanhees L. Physical activity and enhanced fitness to improve cognitive function in older people without known cognitive impairment. Cochrane Database of Systematic Reviews. 2008;(3):CD005381. doi: 10.1002/14651858.CD005381.pub2. [DOI] [PubMed] [Google Scholar]
- Bravata DM, Smith-Spangler C, Sundaram V, Gienger AL, Lin N, Lewis R, Sirard JR. Using pedometers to increase physical activity and improve health: a systematic review. Journal of the American Medical Association. 2007;298(19):2296–2304. doi: 10.1001/jama.298.19.2296. [DOI] [PubMed] [Google Scholar]
- Brown DS, Finkelstein EA, Brown DR, Buchner DM, Johnson FR. Estimating Older Adults’ Preferences for Walking Programs via Conjoint Analysis. American Journal of Preventive Medicine. 2009;36(3):201–207. doi: 10.1016/j.amepre.2008.10.014. [DOI] [PubMed] [Google Scholar]
- Carr LJ, Dunsiger SI, Lewis B, Ciccolo JT, Hartman S, Bock B, Marcus BH. Randomized controlled trial testing an internet physical activity intervention for sedentary adults. Health Psychology. 2013;32(3):328–336. doi: 10.1037/a0028962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrieri V. Social comparison and subjective well-being: does the health of others matter? Bulletin of Economic Research. 2012;64(1):31–55. doi: 10.1111/j.1467-8586.2011.00393.x. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Prevalence of regular physical activity among adults–United States, 2001 and 2005. Morbidity and Mortality Weekly Report. 2007;56(46):1209–1212. [PubMed] [Google Scholar]
- Chang T, Chopra V, Zhang C, Woolford SJ. The role of social media in online weight management: systematic review. Journal of Medical Internet Research. 2013;15(11):e262. doi: 10.2196/jmir.2852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christakis NA. Social networks and collateral health effects. British Medical Journal. 2004;329(7459):184–185. doi: 10.1136/bmj.329.7459.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell EY, Waite LJ. Social disconnectedness, perceived isolation, and health among older adults. Journal of Health and Social Behavior. 2009;50(1):31–48. doi: 10.1177/002214650905000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutrona CE, Suhr JA. Controllability of stressful events and satisfaction with spouse support behaviors. Communication Research. 1992;19:154–174. [Google Scholar]
- Finkelstein EA, Brown DS, Brown DR, Buchner DM. A randomized study of financial incentives to increase physical activity among sedentary older adults. Preventive Medicine. 2008;47(2):182–187. doi: 10.1016/j.ypmed.2008.05.002. [DOI] [PubMed] [Google Scholar]
- Gilbert LK, Omisore F. Common questions about herpes: analysis of chat-room transcripts. Herpes. 2009;15(3):57–61. [PubMed] [Google Scholar]
- Golden J, Conroy RM, Lawlor BA. Social support network structure in older people: underlying dimensions and association with psychological and physical health. Psychology, Health & Medicine. 2009;14(3):280–290. doi: 10.1080/13548500902730135. [DOI] [PubMed] [Google Scholar]
- Griffiths KM, Calear AL, Banfield M, Tam A. Systematic review on Internet Support Groups (ISGs) and depression (2): What is known about depression ISGs? Journal of Medical Internet Research. 2009;11(3):e41. doi: 10.2196/jmir.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey JT, Eime RM, Payne WR. Effectiveness of the 2006 Commonwealth Games 10,000 Steps Walking Challenge. Medicine & Science in Sports & Exercise. 2009;41(8):1673–1680. doi: 10.1249/MSS.0b013e31819d591d. [DOI] [PubMed] [Google Scholar]
- Heisler M, Halasyamani L, Resnicow K, Neaton M, Shanahan J, Brown S, Piette JD. “I am not alone”: the feasibility and acceptability of interactive voice response-facilitated telephone peer support among older adults with heart failure. Congestive Heart Failure. 2007;13(3):149–157. doi: 10.1111/j.1527-5299.2007.06412.x. [DOI] [PubMed] [Google Scholar]
- Heisler M, Piette JD. “I help you, and you help me”: facilitated telephone peer support among patients with diabetes. The Diabetes Educator. 2005;31(6):869–879. doi: 10.1177/0145721705283247. [DOI] [PubMed] [Google Scholar]
- Hoey LM, Ieropoli SC, White VM, Jefford M. Systematic review of peer-support programs for people with cancer. Patient Education and Counseling. 2008;70(3):315–337. doi: 10.1016/j.pec.2007.11.016. [DOI] [PubMed] [Google Scholar]
- Hoffman-Goetz L, Donelle L. Chat room computer-mediated support on health issues for aboriginal women. Health Care for Women International. 2007;28(4):397–418. doi: 10.1080/07399330601180057. [DOI] [PubMed] [Google Scholar]
- Hong Y, Pena-Purcell NC, Ory MG. Outcomes of online support and resources for cancer survivors: a systematic literature review. Patient Education and Counseling. 2012;86(3):288–296. doi: 10.1016/j.pec.2011.06.014. [DOI] [PubMed] [Google Scholar]
- Kahneman D, Tversky A. Prospect Theory – Analysis of Decision under Risk. Econometrica. 1979;47(2):263–291. [Google Scholar]
- Kimmel SE, Troxel AB, Loewenstein G, Brensinger CM, Jaskowiak J, Doshi JA, Volpp K. Randomized trial of lottery-based incentives to improve warfarin adherence. American Heart Journal. 2012;164(2):268–274. doi: 10.1016/j.ahj.2012.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kullgren JT, Troxel AB, Loewenstein G, Asch DA, Norton LA, Wesby L, Volpp KG. Individual-versus group-based financial incentives for weight loss: a randomized, controlled trial. Annals of Internal Medicine. 2013;158(7):505–514. doi: 10.7326/0003-4819-158-7-201304020-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loewenstein G, Brennan T, Volpp KG. Asymmetric paternalism to improve health behaviors. Journal of the American Medical Association. 2007;298(20):2415–2417. doi: 10.1001/jama.298.20.2415. [DOI] [PubMed] [Google Scholar]
- Melling B, Houguet-Pincham T. Online peer support for individuals with depression: a summary of current research and future considerations. Psychiatric Rehabilitation Journal. 2011;34(3):252–254. doi: 10.2975/34.3.2011.252.254. [DOI] [PubMed] [Google Scholar]
- Mitchell MS, Goodman JM, Alter DA, John LK, Oh PI, Pakosh MT, Faulkner GE. Financial Incentives for Exercise Adherence in Adults: Systematic Review and Meta-Analysis. American Journal of Preventive Medicine. 2013;45(5):658–667. doi: 10.1016/j.amepre.2013.06.017. [DOI] [PubMed] [Google Scholar]
- Moy ML, Weston NA, Wilson EJ, Hess ML, Richardson CR. A pilot study of an Internet walking program and pedometer in COPD. Respiratory Medicine. 2012;106(9):1342–1350. doi: 10.1016/j.rmed.2012.06.013. [DOI] [PubMed] [Google Scholar]
- Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Report, 2008. Washington, D.C.: U.S. Department of Health and Human Services; 2008. [Google Scholar]
- Rains SA, Young V. A meta-analysis of research on formal computer-mediated support groups: Examining group characteristics and health outcomes. Human Communication Research. 2009;35:309–336. [Google Scholar]
- Ramadas A, Quek KF, Chan CK, Oldenburg B. Web-based interventions for the management of type 2 diabetes mellitus: a systematic review of recent evidence. International Journal of Medical Informatics. 2011;80(6):389–405. doi: 10.1016/j.ijmedinf.2011.02.002. [DOI] [PubMed] [Google Scholar]
- Richardson CR, Buis LR, Janney AW, Goodrich DE, Sen A, Hess ML, Piette JD. An online community improves adherence in an internet-mediated walking program. Part 1: results of a randomized controlled trial. Journal of Medical Internet Research. 2010;12(4):e71. doi: 10.2196/jmir.1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson CR, Mehari KS, McIntyre LG, Janney AW, Fortlage LA, Sen A, Piette JD. A randomized trial comparing structured and lifestyle goals in an internet-mediated walking program for people with type 2 diabetes. International Journal of Behavioral Nutrition and Physical Activity. 2007;4:59. doi: 10.1186/1479-5868-4-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan RM, Connell JP. Perceived locus of causality and internalization: examining reasons for acting in two domains. Journal of Personality and Social Psychology. 1989;57(5):749–761. doi: 10.1037//0022-3514.57.5.749. [DOI] [PubMed] [Google Scholar]
- Ryan RM, Deci EL. Intrinsic and Extrinsic Motivations: Classic Definitions and New Directions. Contemporary Educational Psychology. 2000;25(1):54–67. doi: 10.1006/ceps.1999.1020. [DOI] [PubMed] [Google Scholar]
- Seeman TE. Social ties and health: the benefits of social integration. Annals of Epidemiology. 1996;6(5):442–451. doi: 10.1016/s1047-2797(96)00095-6. [DOI] [PubMed] [Google Scholar]
- Seeman TE. Health promoting effects of friends and family on health outcomes in older adults. American Journal of Health Promotion. 2000;14(6):362–370. doi: 10.4278/0890-1171-14.6.362. [DOI] [PubMed] [Google Scholar]
- Stessman J, Hammerman-Rozenberg R, Cohen A, Ein-Mor E, Jacobs JM. Physical activity, function, and longevity among the very old. Archives of Internal Medicine. 2009;169(16):1476–1483. doi: 10.1001/archinternmed.2009.248. [DOI] [PubMed] [Google Scholar]
- Svenson O. Are We All Less Risky and More Skillful Than Our Fellow Drivers. Acta Psychologica. 1981;47(2):143–148. [Google Scholar]
- Tudor-Locke C, Bassett DR., Jr How many steps/day are enough? Preliminary pedometer indices for public health. Sports Medicine. 2004;34(1):1–8. doi: 10.2165/00007256-200434010-00001. [DOI] [PubMed] [Google Scholar]
- Tudor-Locke C, Craig CL, Aoyagi Y, Bell RC, Croteau KA, De Bourdeaudhuij I, Blair SN. How many steps/day are enough? For older adults and special populations. International Journal of Behavioral Nutrition and Physical Activity. 2011;8:80. doi: 10.1186/1479-5868-8-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tudor-Locke C, Hart TL, Washington TL. Expected values for pedometer-determined physical activity in older populations. International Journal of Behavioral Nutrition and Physical Activity. 2009;6:59. doi: 10.1186/1479-5868-6-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Physical Activity and Health: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; 1996. [Google Scholar]
- Volpp KG, John LK, Troxel AB, Norton L, Fassbender J, Loewenstein G. Financial incentive-based approaches for weight loss: a randomized trial. Journal of the American Medical Association. 2008;300(22):2631–2637. doi: 10.1001/jama.2008.804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volpp KG, Loewenstein G, Troxel AB, Doshi J, Price M, Laskin M, Kimmel SE. A test of financial incentives to improve warfarin adherence. BMC Health Services Research. 2008;8:272. doi: 10.1186/1472-6963-8-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volpp KG, Troxel AB, Pauly MV, Glick HA, Puig A, Asch DA, Audrain-McGovern J. A randomized, controlled trial of financial incentives for smoking cessation. New England Journal of Medicine. 2009;360(7):699–709. doi: 10.1056/NEJMsa0806819. [DOI] [PubMed] [Google Scholar]
- Yun D, Silk KJ. Social norms, self-identity, and attention to social comparison information in the context of exercise and healthy diet behavior. Health Communication. 2011;26(3):275–285. doi: 10.1080/10410236.2010.549814. [DOI] [PubMed] [Google Scholar]


