Abstract
This study tested the effect of a neonatal-bereavement-support DVD on parental grief after their baby’s death in our Neonatal Intensive Care Unit compared with standard bereavement care (controls). Following a neonatal death, we measured grief change from 3- to 12-month follow-up using a mixed-effects model. Intent-to-treat analysis was not significant, but only 18 parents selectively watched the DVD. Thus, we subsequently compared DVD-viewers with DVD-non-viewers and controls. DVD-viewers reported higher grief at 3-month interviews compared with DVD-non-viewers and controls. Higher grief at 3 months was negatively correlated with social support and spiritual/religious beliefs. These findings have implications for neonatal-bereavement care.
Keywords: Death of a child, grief, bereavement, depression
INTRODUCTION
Despite recent technological advances in newborn care, more children die in the newborn period or immediately prior to birth than any other period in childhood. In the United States, nearly 27,000 babies die before their first birthday, and approximately 26,000 fetuses >20 weeks gestation die before birth (Kochanek, Kirmeyer, Martin, Strobino, & Guyer, 2012; MacDorman & Kirmeyer, 2009). Nearly two-thirds of all infant deaths annually occur in the neonatal period (< 28 days after birth) (Christ, Bonanno, Malkinson, & Rubin, 2003; Kochanek et al., 2012), yet most grief research that includes newborn infants has focused on perinatal death (e.g., including miscarriage, stillbirth, and neonatal death in the first 28 days of life) (Badenhorst & Hughes, 2007; Kersting & Wagner, 2012).
The death of an infant has long-term impact on parents and is associated with a personal but predictable grief response (Kersting & Wagner, 2012; Wing, Clance, Burge-Callaway, & Armistead, 2001). The experience of loss can vary greatly by intensity, duration, and ways those individuals express it (Christ et al., 2003; Center for the Advancement of Health, 2004). The grief trajectory also may be influenced by age and stage of development, gender, history of loss and/or trauma, history of depression, the nature and quality of the relationship with the deceased, type of loss (e.g., anticipated, violent, or traumatic), familial relationships, social networks, religion, and culture (Breen & O'Connor, 2007; Center for the Advancement of Health, 2004; Klass & Walter, 2001). Bereaved parents are not only at increased risk for hospitalization for psychiatric hospitalization (Li, Laursen, Precht, Olsen, & Mortensen, 2005), but depression and anxiety associated with a previous prenatal loss may persist into subsequent pregnancies and after; even with the birth of a healthy child (Blackmore et al., 2011). In addition to clinical depression, parents who have lost a child are at are also increased risk for developing chronic health conditions, Post-traumatic Stress Disorder (PTSD), and cancer (Li, Johansen, Hansen, & Olsen, 2002; Youngblut, Brooten, Cantwell, del Moral, & Totapally, 2013).
Because of the frequency of death in the Neonatal Intensive Care Unit (NICU) and the acute and long-term impact of a neonatal death on families, many hospitals have bereavement support programs (Harvey, Snowdon, & Elbourne, 2008; Koopmans, Wilson, Cacciatore, & Flenady, 2013; Robertson, Aldridge, & Curley, 2011). However, efficacy of a bereavement support and counseling intervention has been evaluated by only one prospective, randomized controlled trial (RCT) of 25 mothers. Results demonstrated no significant difference in depression and anxiety at 14-month follow-up but shorter duration of bereavement reaction was observed in the intervention group (Forrest, Standish, & Baum, 1982).
To inform development of evidence-based practice to improve outcomes for grieving NICU parents, we conducted a RCT to evaluate the impact of viewing a neonatal-bereavement-support DVD on change in parental grief. We hypothesized that parents who received and watched the DVD would show greater decline in grief at follow-up compared with parents receiving standard bereavement care (SBC).
METHODS
DVD Development
To develop a DVD to improve parental outcome after neonatal loss, clinicians from the NICU at St. Louis Children’s Hospital and Washington University School of Medicine teamed with Digital Imaging Advancement (DIA) Productions LLC, a professional production company, SHARE Pregnancy and Infant Loss Support, Inc., and bereaved parents. The 90-minute DVD (Grieving in the NICU – Mending Broken Hearts When a Baby Dies) is divided into 5 chapters to permit parental choice of viewing topic and timing of viewing. Interviews with bereaved parents, grandparents, and siblings provide different perceptions of common early and later grief experiences. The DVD also includes a nationally recognized grief counselor’s and chaplain’s perspectives of the grief process.
Sample, Setting and Randomization
The Washington University Institutional Review Board approved this study. Between January 2008 and October 2010, all English-speaking parents whose babies died in the NICU were prospectively randomized with blocking by family at the time of baby’s death to either the control (SBC) or intervention group (SBC plus DVD [SBC/DVD]). Parents were excluded if they were non-English speaking. We used the SAS procedure PLAN to construct the treatment-allocation scheme. Research-team members who distributed the DVDs were not blinded to group assignment. When an infant died, NICU staff notified the research-team clinicians, who checked the randomization list to determine allocation and provided DVDs to parents randomized to the SBC/DVD arm with the other keepsakes given to every family as part of SBC. SBC includes care by an interdisciplinary NICU team of neonatologists, nurses, social workers, chaplains, and patient-care associates, a CD created with photographs, a memory packet, locks of baby’s hair, plaster hand- and foot-prints, the gown in which the baby is dressed after death, a ring for the mother, and engraved necklace for the father. To be sensitive to parents’ loss, we did not recruit them to participate at time of randomization.
SBC also includes follow-up meetings, which usually occur 8-12 weeks after the baby’s death. The team answers questions, reviews autopsy results, if applicable, and assesses for symptoms of pathologic grief in the family. After these meetings, a physician or nurse on the research team provided parents with information about the study, asked them about their willingness to participate, and if parents agreed, obtained their informed consent. Between April 2008 and February 2011, using a computer-assisted telephone interview system, an experienced interviewer not involved in the baby’s care conducted telephone interviews with parent participants at 3 and 12 months after the baby’s death. Participants were paid $25.00 per interview for time and effort.
Measures
During each telephone interview, we administered previously validated questionnaires and collected additional information about parents’ demographics.
We used the 33-item Perinatal Grief Scale (Potvin, Lasker, & Toedter, 1989) to measure parental grief, our primary outcome. Higher total scores indicate higher grief. The reliability of the measure is high (Cronbach’s alpha = .95) (Potvin et al., 1989).
To measure depression, we used the 20-item Center for Epidemiologic Studies-Depression (CES-D) questionnaire. Total scores can range from 0-60. Respondents with scores ≥16 are considered to have symptoms congruent with clinical depression (Radloff, 1977; Radloff & Locke, 1986). The computer-assisted interview system triggered notification of the need for referral of these patients for counseling or to their physician; the interviewer provided referral information. Respondents with scores > 23 also were contacted by the physician member of the team to assess the parent’s need for psychiatric consultation and ensure appropriate and timely care.
To measure the strength of parents’ spiritual beliefs, we used six items from The Royal Free Interview for Spiritual and Religious Beliefs, which uses a scale from 0-10 points (e.g., from not at all important to extremely important), with higher total scores indicating more strongly held spiritual beliefs. This previously validated spiritual and religious beliefs measure was reported to have high internal consistency (Cronbach’s alpha = .81) and test-retest reliability (intraclass correlation = .95) (King, Speck, & Thomas, 2001).
To measure social support, we used the 24-item Social Provisions Scale (SPS). Total scores range from 24-96; higher scores indicate greater support. Reliabilities of the measure were reported to be high in a variety of samples (Cutrona, 1986; Cutrona, Russell, & Rose, 1986).
We collected demographic data (parental age, gender, race/ethnicity, educational attainment, employment status, health insurance status, and marital status) using questions from the Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance System interview. The baby’s medical record provided information about date of birth and date of death. The interviewer also asked parents in the SBC/DVD arm to evaluate the DVD and whether they would recommend the DVD to other bereaved parents. Thus the interviewer was not blinded to treatment condition.
Sample Size
Based on previously published data (Potvin et al., 1989), the average number of deaths annually in the St. Louis Children’s Hospital NICU (about 60/year), and an expected participation rate of 50%, we estimated that 30 parents in each group would provide 80% power at a .05 level of significance to detect a 10-30% difference in grief between groups.
Statistical Analysis
We report descriptive statistics for all variables for participants who completed both interviews. Using the IBM SPSS Statistics Release 21.0.0.0 (Armonk, NY: IBM Corporation, 2012), we ran chi-square tests to examine associations among categorical variables, Pearson correlations to measure associations among continuous variables, and analyses of variance (ANOVAs) to measure between-groups differences in continuous variables. We used Cronbach’s alpha to test the internal consistency of items used to compute each multi-item scale for this study. We used a mixed-effects model to quantify the intervention effect and explore the intervention-by-time interaction, taking into consideration the correlation among responses within the same family; we specified intervention, time, and their interaction as fixed effects, and families (babies) as random intercept. In intention-to-treat analysis, we compared the outcome, change in grief, between the two groups based on the original randomization assignment. In addition, because we expected that some parents in the SBC/DVD arm might not watch the DVD, we planned to examine change in grief among three groups (control, DVD-watched, and DVD-no watched), comparing intervention effects across time using appropriate contrasts with 95% confidence intervals. Both the point and interval estimates are presented. The models were fitted and tested using PROC MIXED in SAS version 9.3 (SAS Institute, Cary, NC). Two-tailed p values < .05 were considered significant. There are some caveats in explaining our statistical results. We performed many tests and have not used multiple-comparison procedures to adjust our p values. So these p values can only be interpreted as comparison-wise p values (Westfall, Tobias, Rom, Wolfinger, & Hochberg, 1999).
RESULTS
We randomized 160 families to SBC (85 families) or SBC/DVD (75 families). Of 320 parents randomized, 14 fathers who were not identified or involved, one mother who was incapacitated from a car crash, and five who were otherwise ineligible (parent in jail or baby discharged to hospice) were not contacted. Although we randomized by family, both parents in a family did not always participate; and 25 parents declined to be interviewed after consenting. Overall, 213 parents (66.6%) were excluded because they did not meet eligibility criteria (n=36), declined to participate (n=98), or were unable to be contacted (n=79). A greater proportion of married than unmarried parents (62/149 [42%] vs. 45/171 [26%]; p = .004) and of mothers than fathers (70/159 [44%] vs. 37/161 [23%]; p < .001) participated.
At the 3-month contact with parents after the baby’s death (standard procedure in our NICU), 132 parents (41%) consented to be contacted for the study. Between April 2008 and February 2011, 107 parents (56 SBC; 51 SBC/DVD) completed at least one interview (81% of the 132 who consented to be contacted); 99 parents completed the 3-month interview, 82 participants completed the 12-month interview, and 74 (35 SBC; 39 SBC/DVD) completed both.
Cronbach’s alpha coefficients were acceptably high at 3-month and 12-month interviews for grief (alpha=.91 and .93), spiritual/religious beliefs (alpha=.80 and .83), social support (alpha=.91 and .93), and depressed mood (alpha=.80 and .81). Parents who completed only the 3-month interview (N=25) reported lower levels of social support (mean [SD]: 98.0 [13.9] vs. 105.9 [10.7]; p = .004) and had babies who lived longer (mean [SD]: 49.6 [63.7] vs. 23.6 [38.3] days; p = .02) compared with parents who completed both interviews; and although not statistically significant, a higher proportion of parents who were married completed both interviews than the proportion of unmarried parents who did so (48/59 [81.4%] vs. 26/40 [65%]; p = .07). Participants who were members of an unmarried couple (n=10) and never-married (n=14) were similar to each other in terms of greater proportions of each group reporting less than or equal to high school education and being unemployed compared with married participants; in addition, members of unmarried couples and never-married participants were similar with respect to reporting younger age, lower social support, and higher levels of grief and depressed mood compared with married participants (each comparison p < .05). Thus, for analysis, we combined all unmarried participants (including 2 divorced) in one group to compare with married participants. Parents who completed only the 12-month interview (N=8) did not differ significantly from parents who completed both interviews on any of the variables measured. The proportions of mothers (33/50 [66%]) and fathers (15/24 [62%]) who completed both interviews did not differ significantly by marital status (p = .77). Of these 74 participants, 73 had complete data for all variables of interest and were included in our analysis.
Fathers were older than mothers (mean [SD]: 33.8 [8.5] vs. 29.6 [5.6] years; p = .02). Mothers reported on average more severe depressive symptoms on the CES-D at 3 months than fathers reported (19.1 [12.0] vs. 12.0 [12.4]; p = .03) but not at 12 months (14.1 [11.8] vs. 10.9 [11.9]; p = .27). We observed no other significant gender differences in any of the other variables measured at either interview.
There were no significant differences in any of the variables measured at 3 or 12 months by study arm (SBC alone vs. SBC/DVD) as shown in Table 1. In the intention-to-treat analysis, grief changed significantly by time (p < .001), but neither the main effect by arm (p = .34) nor the intervention-by-time interaction (p=.35) was significant. As we expected might happen due to the timing of randomization, not all parents in the SBC/DVD arm watched the DVD; only 18 reported watching the DVD by the 12-month interview. Consequently, we computed a 3-category study-group variable for further data analyses (DVD/watched, DVD/did not watch, and control).
Table 1.
Descriptive statistics of participants who completed both 3-month and 12-month interviews, by study arm and by 3-category study group (N = 73)
|
Variable |
Control n = 34 |
DVD n = 39 |
p a | DVD-not watched by 12 months n = 21 |
DVD-watched by 12 months n = 18 |
p b |
|---|---|---|---|---|---|---|
| Parent, no. (%) | .88 | .56 | ||||
| Mother | 23 (67.6) | 27 (69.2) | 13 (61.9) | 14 (77.8) | ||
| Father | 11 (32.4) | 12 (30.8) | 8 (38.1) | 4 (22.2) | ||
| Marital status, no. (%) | .96 | .06 | ||||
| Married | 22 (64.7) | 25 (64.1) | 17 (81.0) | 8 (44.4) | ||
| Not married | 12 (35.3) | 14 (35.9) | 4 (19.0) | 10 (55.6) | ||
| Race, no. (%) | .47 | .56 | ||||
| White | 25 (73.5) | 32 (82.0) | (86.7) | (77.8) | ||
| Black | 6 (17.6) | 6 (15.4) | 2 (9.5) | 4 (22.2) | ||
| Other | 3 (8.8) | 1 (2.6) | 1 (4.8) | 0 (0.0) | ||
| Education, no. (%) | .12 | .02 | ||||
| ≤ high school graduate/GED | 11 (32.4) | 16 (41.0) | 4 (19.0) | 12 (66.7) | ||
| Some postsecondary education | 10 (29.4) | 7 (17.9) | 5 (23.8) | 2 (11.1) | ||
| College graduate/some post-baccalaureate education |
10 (29.4) | 6 (15.4) | 5 (23.8) | 1 (5.6) | ||
| Advanced degree (master’s/doctorate) | 3 (8.8) | 10 (25.6) | 7 (33.3) | 3 (16.7) | ||
| Employment status, no. (%) | .69 | .20 | ||||
| Employed at least part time | 25 (73.5) | 27 (69.2) | 17 (81.0) | 10 (55.6) | ||
| Unemployed/housewife/student/retired | 9 (26.5) | 12 (30.8) | 4 (19.0) | 8 (44.4) | ||
| Elevated depressed mood at 3 months, no. (%) | .52 | .29 | ||||
| Yes | 14 (41.2) | 19 (48.7) | 8 (38.1) | 11 (61.1) | ||
| No | 20 (58.8) | 20 (51.3) | 13 (61.9) | 7 (38.9) | ||
| Parents’ age (years) at 3 months, mean (SD) | 30.9 (6.8) | 31.0 (7.0) | .92 | 32.1 (6.7) | 29.8 (7.2) | .57 |
| Infants’ age at time of death (days), mean (SD) | 21.6 (36.1) | 25.7 (40.9) | .65 | 37.6 (45.6) | 11.9 (30.1) | .10 |
| Grief at 3 months, mean (SD) | 88.9 (16.3)c | 95.5 (20.6) | .14 | 87.5 (14.3)d | 104.8 (23.1)c,d | .005 |
| Depressed mood at 3 months, mean (SD) | 14.1 (10.9)e | 19.2 (13.9) | .09 | 14.0 (10.5)f | 25.2 (15.1)e,f | .004 |
| Spiritual/religious beliefs at 3 months, mean (SD) |
44.7 (11.3) | 43.6 (11.5) | .66 | 47.5 (10.0) | 38.9 (11.7) | .05 |
| Social support at 3 months, mean (SD) | 107.1 (8.7) | 107.1 (8.7) | .42 | 106.2 (12.0) | 103.8 (12.5) | .56 |
| Grief at 12 months, mean (SD) | 84.2 (19.2) | 87.4 (18.2) | .46 | 84.0 (15.6) | 91.4 (20.6) | .36 |
| Depressed mood at 12 months, mean (SD) | 12.2 (11.1) | 13.9 (12.4) | .54 | 13.1 (12.6) | 14.8 (12.4) | .75 |
| Spiritual/religious beliefs at 12 months, mean (SD) |
44.6 (10.9) | 40.6 (13.8) | .18 | 42.1 (14.6) | 38.7 (13.0) | .29 |
| Social support at 12 months, mean (SD) | 105.4 (12.7) | 106.7 (10.9) | .64 | 109.8 (9.7) | 103.2 (11.4) | .19 |
Tests of significance are chi-square tests or one-way analyses of variance measuring differences by arm (control or DVD).
Tests of significance are chi-square tests or one-way analyses of variance measuring differences by group (control, DVD-not-watched, or DVD-watched).
Scheffé’s post-hoc test between control and DVD-watched, p = .007.
Scheffé’s post-hoc test between DVD-not watched and DVD-watched, p = .007.
Scheffé’s post-hoc test between control and DVD-watched, p = .009.
Scheffé’s post-hoc test between DVD-not watched and DVD-watched, p = .02.
Parents who watched the DVD by 12-month follow-up reported significantly lower educational attainment, more severe depressive symptoms, and higher grief at 3 months compared with controls and parents who did not watch the DVD (Table 1). There were no significant differences among the 3 groups in severity of depressive symptoms and grief at 12 months.
We also examined correlations among continuous variables (Table 2). Grief at 3 months was positively correlated with depressive-symptom severity at 3 months and negatively correlated with parent’s age, social support, and spiritual/religious beliefs at 3 months. Grief at 12 months was positively correlated with baby’s age at death, grief at 3 months, and depressive-symptom severity at 3 and 12 months, and was negatively correlated with social support and spiritual/religious beliefs at 3 and 12 months. Because grief and depressive-symptom severity at 3 months were so highly correlated, we created a dichotomous variable for elevated depressed mood (yes [CES-D ≥ 16] vs. no [CES-D < 16]) for subsequent analysis (Radloff, 1977; Radloff & Locke, 1986).
Table 2.
Pearson correlations among the continuous variables for participants who completed both 3-month and 12-month interviews (N = 73)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||
|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Parents’ age, 3 months | 1.00 | ||||||||
| 2. | Baby’s age at death | −.05 | 1.00 | |||||||
| 3. | Grief, 3 months | −.29a | .19 | 1.00 | ||||||
| 4. | Social support, 3 months | −.01 | −.38c | −.46d | 1.00 | |||||
| 5. | Spiritual/religious beliefs, 3 months |
.01 | −.02 | −.37c | .277a | 1.00 | ||||
| 6. | Depressed mood, 3 months | −.27a | .16 | .81d | −.51c | −.39c | 1.00 | |||
| 7. | Grief, 12 months | −.19 | .35c | .70d | −.43d | −.32b | .69d | 1.00 | ||
| 8. | Social support, 12 months | .16 | −.39c | −.56d | .68d | .36c | −.62d | −.66d | 1.00 | |
| 9. | Spiritual/religious beliefs, 12months |
−.11 | .01 | −.12 | .20 | .56d | −.19 | −.26a | .14 | 1.00 |
| 10. | Depressed mood, 12 months | −.32b | .41d | .50d | −.36c | −.24a | .62d | .78d | −.60d | −.17 |
Two-tailed significance at p < .05.
Two-tailed significance at p < .01.
Two-tailed significance at p < .005.
Two-tailed significance at p < .001.
Since not all parents in the SBC/DVD arm watched the DVD, we used a multivariate logistic regression model to identify independent predictors of DVD viewing by 12-month follow-up among the 39 parents in the SBC/DVD arm. In this exploratory analysis, we included predictor variables measured at 3 months that were associated with DVD viewing in univariate tests at p < .20 to reduce chance of Type II error (i.e., not identifying an important predictor of DVD viewing). As this exploratory model was run to understand variables associated with DVD viewing to generate hypotheses for future research, we report the odds ratios (95% confidence intervals) and comparison-wise p values without adjusting for multiple comparisons (Table 3), recognizing the increased risk of overall Type I error. In this exploratory, multivariable model, parents with higher grief at 3 months were more likely, and parents whose babies were older at time of death were less likely, to watch the DVD by 12 months. Babies in this sample had died in the NICU an average of 23.8 days after birth, but parents who watched the DVD had babies who died an average of 11.9 days after birth (Table 1).
Table 3.
Adjusted multivariable logistic regression models identifying predictors of watching the DVD among only the 39 participants in the DVD arma
| Variable | aOR (95% CI) | p |
|---|---|---|
| Grief, 3 monthsb | 1.20 (1.03-1.40) | .02 |
| Baby’s age at death (days)c | 0.94 (0.90-0.98) | .01 |
| Spiritual/religious beliefs, 3 monthsd | 0.91 (0.79-1.04) | .15 |
| Elevated depressed mood, 3 monthse | ||
| Yes | 0.08 (0.00-2.36) | .14 |
| No (reference) | 1.00 (reference) | |
| Education | ||
| ≤ High school graduate/GED | 1.00 (reference) | |
| Some post-secondary education | 3.02 (0.10-93.83) | .53 |
| College graduate/some post-baccalaureate education | 0.01 (0.00-0.81) | .04 |
| Advanced degree (master’s/doctorate) | 3.62 (0.11-116.39) | .47 |
| Marital status | ||
| Not married | 15.66 (.72-342.96) | .08 |
| Married (reference) | 1.00 (reference) |
Notes: aOR, adjusted odds ratio; CI, confidence interval. All variables in this model were entered as a block. Hosmer-Lemeshow goodness-of-fit test indicated the model fit the data (p = .91).
Predictors included all variables associated with DVD viewing (vs. not viewed) at p < .20 in univariate tests to reduce chance of Type II error.
OR>1.00 indicates greater likelihood of watching the DVD by 12-month interview with each increasing unit (1) of grief reported at the 3-month interview.
OR<1.00 indicates lower likelihood of watching the DVD by 12-month interview with each increasing unit (1 day) of baby’s age at death.
OR<1.00 indicates lower likelihood of watching the DVD by 12-month interview with each increasing unit (1) of spiritual/religious beliefs reported at the 3-month interview.
We used the categorical variable for elevated depressed mood at 3 months due to collinearity of grief and depressive-symptom severity using the CES-D total score.
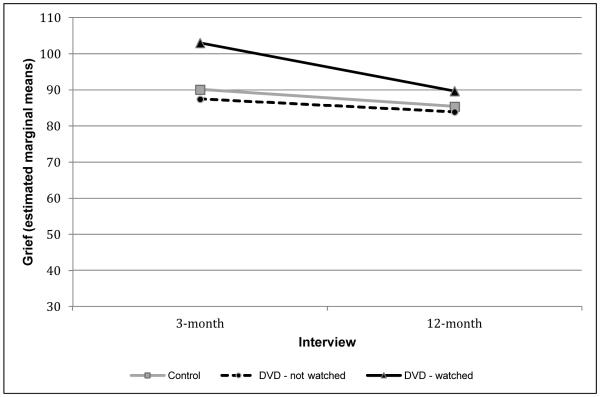
Since the intention-to-treat analysis was not significant, we ran a second adjusted mixed-effects model evaluating change in grief over time by the 3-category study-group variable (Table 4). In this model, we observed a significant interaction between change in grief and study group (p = .02); DVD viewers reported significantly higher grief at 3 months than either of the other 2 groups reported and showed a steeper decline in grief from 3-12 months than the decline observed in the other 2 groups (see Figure 1). As shown in Table 4, at 3 months, grief in the DVD-watched group was significantly higher than in the control group and in the SBC/DVD group who did not watch the DVD (each p < .01). By the 12-month interview, the 3 groups did not differ significantly in mean levels of grief, and the change from 3-12 months was significant only for the SBC/DVD-watched group (Table 4 and Figure 1).
Table 4.
Adjusted mixed-effects model of change in grief by study group from 3-month to 12-month interviews, with pairwise contrastsa
| Grief estimated marginal means (95% CI) |
F value | p | |
|---|---|---|---|
| Study groupb | 4.17 | .02 | |
| Timec | 17.56 | <.001 | |
| Study group-by-time interaction | 2.83 | .06 | |
| Control, 3-month | 90.10 (84.84, 95.37) | ||
| DVD-not watched, 3-month | 87.44 (80.89, 94.00) | ||
| DVD-watched, 3-month | 103.03 (96.16, 109.91) | ||
| Control, 12-month | 85.37 (80.10, 90.63) | ||
| DVD-not watched, 12-month | 83.92 (77.37, 90.47) | ||
| DVD-watched, 12-month | 89.70 (82.82, 96.58) | ||
|
| |||
| Pairwise Contrasts (Differences) | t value | ||
|
| |||
| Between-groups differences in grief at 3 months (95% CI) | |||
|
| |||
| DVD-not watched – control | −2.66 (−11.10, 5.79) | −0.63 | .53 |
| DVD-watched – control | 12.93 (4.27, 21.59) | 2.97 | .004 |
| DVD-watched – DVD-not watch | 15.59 (6.58, 24.60) | 3.44 | <.001 |
|
| |||
| Between-groups differences in grief at 12 months (95% CI) | |||
|
| |||
| DVD-not watched – control | −1.45 (−9.89, 7.00) | −.0.34 | .73 |
| DVD-watched – control | 4.33 (−4.33, 12.99) | 1.00 | .32 |
| DVD-watched – DVD-not watch | 5.78 (−3.23, 14.79) | 1.28 | .21 |
|
| |||
| Change in grief (12 month – 3 month) within each group (95% CI) | |||
|
| |||
| Control | −4.74 (−9.56, 0.09) | −1.95 | .05 |
| DVD-not watched | −3.52 (−9.67, 2.62) | −1.14 | .26 |
| DVD-watched | −13.33 (−19.97, −6.70) | −4.00 | <.001 |
Abbreviation: CI, confidence interval.
Model adjusted for parent’s age, baby’s age at death, spiritual/religious beliefs, social support, and elevated depressed mood at 3 months.
Control, DVD-not watched, DVD-watched.
3-month to 12-month interviews.
Fig. 1.
Mixed-effects model of grief, by 3-category study group at 3-month and 12-month interviews, adjusting for elevated depressed mood, spiritual/religious beliefs, and social support at 3 months, parent’s age, and baby's age at death (N = 73).
Among the 18 parents who viewed the DVD, all reported that the DVD helped normalize their feelings, and 17 indicated they would recommend the DVD to other parents who experienced the death of a baby in the NICU.
DISCUSSION
We evaluated the efficacy of our bereavement-support DVD provided to parents after their baby’s death in the NICU. We found that parents in the SBC/DVD group who watched the DVD by the 12-month interview reported higher grief at 3 months than parents in either the control or SBC/DVD group who did not watch the DVD. Our study suggests that a bereavement-support DVD may be effective in helping some parents cope with neonatal loss. In addition to reporting higher grief at 3 months, parents who watched the DVD experienced the death of their newborn on average within the first 11-12 days of life (Table 1). It has long been recognized that unanticipated infant death does not allow time for anticipatory grief (Benfield, Leib, & Reuter, 1976; Rando, 1983; Sweeting & Gilhooly, 1990) and might have prompted these parents to look for additional support and resources to aid in their grief process.
Typically, normal, or non-pathologic, grief is a dysphoric state characterized by a variety of emotions, including intense sadness, anxiety, guilt and anger (Dyer, 2005; Zisook, Shear, & Kendler, 2007). Normal grief has clinical features and intensity that are similar to clinical depression and can be very pronounced in parents who have lost children, especially in the first few months of life, e.g., due to sudden infant death syndrome (SIDS) (Murphy, 1997). Symptoms of anxiety and depression in parents who experience perinatal death or death due to SIDS can persist more than a year (Vance, Boyle, Najman, & Thearle, 1995). Although grief and depression are not the same, our study demonstrated high correlation between grief and depression at 3- and 12-month interviews and suggests that screening for depression or very high levels of grief in the first few months after a child’s death may help identify parents at risk of unresolved or complicated grief (Shear et al., 2011). In fact, parents in our study who watched the DVD reported higher levels of grief and depressive symptomatology at the 3-month interview compared with parents who did not watch the DVD. It could be that these parents sought help or solace by watching the DVD. Others have reported that participants with high levels of grief sought grief counseling more frequently than participants with lower levels of grief, and they reported benefits from grief counseling (Gamino, Sewell, Hogan, & Mason, 2009-2010).
This study includes one of the largest cohorts of grieving fathers reported in the literature. A number of studies have demonstrated that mothers experience higher levels of grief and depression for longer periods after perinatal loss than fathers (Beutel, Willner, Deckardt, Von Rad, & Weiner, 1996; Kersting, Brahler, Glaesmer, & Wagner, 2011; Stinson, Lasker, Lohmann, & Toedter, 1992). However, we found that only severity of depressive symptoms at 3 months, but not grief, was higher in mothers than fathers, and we observed no gender differences in either grief or depressive symptoms at 12 months. Studies on the psychological effects of perinatal death and death of a child in the NICU/PICU also have identified themes common to both mothers and fathers, such as risk for psychiatric disease, development of PTSD symptoms, and increased risk of chronic health conditions (Badenhorst, Riches, Turton, & Hughes, 2006; Youngblut et al., 2013). Fewer studies have looked at gender-specific relationships between grief and depression. More research is needed related to neonatal bereavement and paternal grief response.
Studies suggest that bereaved families have great spiritual needs. Parents who have lost a child have reported that they were able to find comfort in their beliefs in God and make meaning out of their child’s death (Brosig, Pierucci, Kupst, & Leuthner, 2007). Other investigators note the importance of parents maintaining a connection with their child that transcends death (Meert, Thurston, & Briller. 2005). As previously reported, lower grief was associated with stronger spiritual/religious beliefs (Walsh, King, Jones, Tookman, & Blizard, 2002; Wortmann & Park, 2008), which also has been reported to be a predictor of bereavement recovery (Anderson, Marwit, Vandenberg, & Chibnall, 2005; Cowchock, Lasker, Toedter, Skumanich, & Koenig, 2010; Walsh et al., 2002). However, many of these studies were cross sectional and retrospective, which could be affected by recall bias, changes in health, mood or personal development (Cowchock et al., 2010; Higgins, 2002; Swanson, Pearsall-Jones, & Hay, 2002; Walsh et al., 2002).
We also found that lower support was associated with higher grief. Our neonatal study adds to the findings of previously reported perinatal studies that demonstrated an association between more intense grief and lack of support or poor marital relationships (Cuisinier, Kuijpers, Hoogduin, de Graauw, & Janssen, 1993; Forrest et al., 1982; Kersting & Wagner, 2012; Lasker & Toedter, 1991). Family members, particularly a caring partner (Forrest et al., 1982), healthcare providers (Kreicbergs, Lannen, Onelov, & Wolfe, 2007), and close friends (van Baarsen, 2002) may provide this much-needed support. Lack of support from a partner and poor marital relations have both been described in association with more intense grief after the loss of a baby (Kersting & Wagner, 2012). Having a partner per se may not be equivalent to having support. In our study, participants who described themselves as “a member of an unmarried couple” gave similar responses to other questions as parents who said they were “never married.” Therefore, we grouped participants who reported being a member of an unmarried couple with never-married participants, because their responses to our questions indicated that these two groups belonged together, regardless of their partner status.
The observed decline in grief at 1 year is consistent with findings from other bereavement studies (Harmon, Glicken, & Siegel, 1984; Janssen, Cuisinier, de Graauw, & Hoogduin, 1997). Longer-term longitudinal studies have demonstrated that, in a normal perinatal grieving process, grief declines over a period of 2 years after a pregnancy loss (Harmon et al., 1984; Janssen et al., 1997; Kersting & Wagner, 2012; Lasker & Toedter, 1991). In our study, even those parents with the highest levels of grief at 3 months who watched the DVD reached similar levels of grief as the other two groups by one year. We cannot infer that this steep decline in grief by 12 months was due to viewing the DVD, since parents who reported high levels of grief in the SBC arm also showed a decline in grief by 12 months. Thus our hypothesis was not supported, and the decline in grief in the group who watched the DVD, as in the SBC arm, might be due only to the passage of time. However, the subgroup of parents in the SBC/DVD arm with very high levels of grief at 3 months and whose babies were younger when they died were more likely to watch the DVD, even controlling for other variables in the logistic regression model (Table 3). Murphy et al. (1998) found that a parent support intervention after the death of an adolescent or young adult child helped parents who had higher grief but had no effect for parents with lower grief. Since the passage of time might have accounted for the decline in grief among those parents in the DVD arm who watched the DVD in our study, an RCT of bereaved parents with high levels of grief and whose babies died at a younger age would be required to determine the impact of DVD viewing on grief reduction over time in this group. Nevertheless, parents who viewed the DVD (and who also happened to report higher levels of grief and depressed mood at 3 months compared with parents who did not view the DVD) reported that the DVD helped them understand that their feelings were normal and that they would recommend it to other parents. Thus, having the DVD available to these parents at this crucial time was viewed as a resource that helped them through the grieving process in the first year.
Limitations of this study are that participants were from one NICU and might represent a subset of bereaved parents seeking additional help after their baby’s death, thereby introducing selection bias and limiting generalizability of our findings. In addition, we interviewed parents only twice to minimize their emotional burden (Parkes, 1995). Thus, we may have missed identification of varying patterns in grief responses in the first year (Badenhorst & Hughes, 2007; Lin & Lasker, 1996; Maciejewski, Zhang, Block, & Prigerson, 2007) and identification of parents who may be at risk of developing complicated grief over a longer period of time. Some of these parents may have experienced other preterm or infant/child deaths, about which we also lacked data. Accessing additional grief support was not measured, which also could have affected our results. Despite these limitations, we observed a significant decline in grief in that subset of parents who watched the DVD; controlling for covariates of grief and DVD viewing in the mixed-effects model minimized the effect of any bias introduced by selectively watching the DVD.
In conclusion, although we cannot infer a causal effect of DVD viewing on grief, parents who watched it reported benefits of viewing. Since independent predictors of DVD viewing in our exploratory, multivariate model included very high grief at 3 months and baby’s early death after birth, an RCT of parents with these characteristics could determine the impact of DVD viewing on grief reduction over time. Longer-term longitudinal research is needed to evaluate patterns of parental grief following a neonatal loss over time, perhaps to help identify factors that may put parents at risk for developing unresolved or complicated grief years after such a devastating loss.
ACKNOWLEDGMENTS
We thank Dr. F. Sessions Cole for his support of this project; the St. Louis Children’s Hospital NICU staff; Cathi Lammert, RN, Executive Director of Share Pregnancy and Infant Loss Support, Inc., 1992-2013; Dan and Ray Duffy at DIA Productions LLC, for production of the Neonatal-Bereavement-Support DVD; Deb Ksiazek for conducting the interviews, and Irene Fischer for data management services provided through the Health Behavior, Communication, and Outreach Core of the Siteman Cancer Center. We also deeply thank the bereaved family members, chaplains and grief counselors who participated in the creation of the DVD and the parents who participated in this study.
FUNDING
Funding for this study was provided by the Department of Pediatrics at Washington University School of Medicine and by the National Cancer Institute Cancer Center Support Grant to the Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine in St. Louis, Missouri (P30 CA091842).
ABBREVIATIONS
- NICU
neonatal intensive care unit
- SBC
standard bereavement care
- RCT
randomized controlled trial
- IRB
institutional review board
- CES-D
Center for Epidemiologic Studies-Depression
- OR
Odds ratio
- CI
confidence interval
Footnotes
CONFLICT OF INTEREST
The authors report no conflicts of interest.
Trial Registration clinicaltrials.gov Identifier: NCT01926080
REFERENCES
- Anderson MJ, Marwit SJ, Vandenberg B, Chibnall JT. Psychological and religious coping strategies of mothers bereaved by the sudden death of a child. Death Studies. 2005;29(9):811–826. doi: 10.1080/07481180500236602. doi: 10.1080/07481180500236602. [DOI] [PubMed] [Google Scholar]
- Badenhorst W, Hughes P. Psychological aspects of perinatal loss. Best Practice & Research in Clinical Obstetrics & Gynaecology. 2007;21(2):249–259. doi: 10.1016/j.bpobgyn.2006.11.004. [DOI] [PubMed] [Google Scholar]
- Badenhorst W, Riches S, Turton P, Hughes P. The psychological effects of stillbirth and neonatal death on fathers: systematic review. Journal of Psychosomatic Obstetrics & Gynecology. 2006;27(4):245–256. doi: 10.1080/01674820600870327. [DOI] [PubMed] [Google Scholar]
- Benfield DG, Leib SA, Reuter J. Grief response of parents after referral of the critically ill newborn to a regional center. New England Journal of Medicine. 1976;294(18):975–978. doi: 10.1056/NEJM197604292941803. [DOI] [PubMed] [Google Scholar]
- Beutel M, Willner H, Deckardt R, Von Rad M, Weiner H. Similarities and differences in couples' grief reactions following a miscarriage: results from a longitudinal study. Journal of psychosomatic research. 1996;40(3):245–253. doi: 10.1016/0022-3999(95)00520-x. [DOI] [PubMed] [Google Scholar]
- Blackmore ER, Cote-Arsenault D, Tang W, Glover V, Evans J, Golding J, et al. Previous prenatal loss as a predictor of perinatal depression and anxiety. British Journal of Psychiatry. 2011;198(5):373–378. doi: 10.1192/bjp.bp.110.083105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breen LJ, O'Connor M. The fundamental paradox in the grief literature: a critical reflection. Omega (Westport) 2007;55(3):199–218. doi: 10.2190/OM.55.3.c. [DOI] [PubMed] [Google Scholar]
- Brosig CL, Pierucci RL, Kupst MJ, Leuthner SR. Infant end of life care: the parents’ perspective. Journal of Perinatology. 2007;27:510–516. doi: 10.1038/sj.jp.7211755. [DOI] [PubMed] [Google Scholar]
- Center for the Advancement of Health Report on bereavement and grief research. Death Studies. 2004;28(6):491–575. doi: 10.1080/07481180490461188. doi: 10.1080/07481180490461188. [DOI] [PubMed] [Google Scholar]
- Christ F, Bonanno G, Malkinson R, Rubin S. Bereavement experiences after the death of a child. In: Field M, Berhman R, editors. When children die: improving palliative and end-of-life care for children and their families. National Academy Press; Washington, DC: 2003. pp. 553–579. [Google Scholar]
- Cowchock FS, Lasker JN, Toedter LJ, Skumanich SA, Koenig HG. Religious beliefs affect grieving after pregnancy loss. Journal of Religion and Health. 2010;49(4):485–497. doi: 10.1007/s10943-009-9277-3. doi: 10.1007/s10943-009-9277-3. [DOI] [PubMed] [Google Scholar]
- Cuisinier MC, Kuijpers JC, Hoogduin CA, de Graauw CP, Janssen HJ. Miscarriage and stillbirth: time since the loss, grief intensity and satisfaction with care. European Journal of Obstetrics, Gynecology, and Reproductive Biology. 1993;52:163–168. doi: 10.1016/0028-2243(93)90066-l. [DOI] [PubMed] [Google Scholar]
- Cutrona C. Behavioral manifestations of social support: A microanalytic investigation. Journal of Personality and Social Psychology. 1986;51:201–208. doi: 10.1037/0022-3514.51.1.201. [DOI] [PubMed] [Google Scholar]
- Cutrona C, Russell D, Rose J. Social support and adaptation to stress by the elderly. Journal of Psychology and Aging. 1986;1(1):47–54. doi: 10.1037//0882-7974.1.1.47. [DOI] [PubMed] [Google Scholar]
- Dyer KA. Identifying, understanding, and working with grieving parents in the NICU: Identifying and understanding loss and the grief response. Neonatal Network. 2005;24:35–46. doi: 10.1891/0730-0832.24.3.35. [DOI] [PubMed] [Google Scholar]
- Forrest GC, Standish E, Baum JD. Support after perinatal death: a study of support and counselling after perinatal bereavement. British Medical Journal. 1982;285(6353):1475–1479. doi: 10.1136/bmj.285.6353.1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gamino LA, Sewell KW, Hogan NS, Mason SL. Who needs grief counseling? A report from the Scott & White Grief Study. Omega - Journal of Death & Dying. 2009-2010;60;(3):199–223. doi: 10.2190/om.60.3.a. [DOI] [PubMed] [Google Scholar]
- Harmon RJ, Glicken AD, Siegel RE. Neonatal loss in the intensive care nursery: effects of maternal grieving and a program for intervention. Journal of the American Academy of Child Psychiatry. 1984;23(1):68–71. doi: 10.1097/00004583-198401000-00009. [DOI] [PubMed] [Google Scholar]
- Harvey S, Snowdon C, Elbourne D. Effectiveness of bereavement interventions in neonatal intensive care: a review of the evidence. Seminars in Fetal & Neonatal Medicine. 2008;13(5):341–356. doi: 10.1016/j.siny.2008.03.011. doi: 10.1016/j.siny.2008.03.011. [DOI] [PubMed] [Google Scholar]
- Higgins MP. Parental bereavement and religious factors. Omega (Westport) 2002;45:187–207. [Google Scholar]
- Janssen HJ, Cuisinier MC, de Graauw KP, Hoogduin KA. A prospective study of risk factors predicting grief intensity following pregnancy loss. Archives of General Psychiatry. 1997;54(1):56–61. doi: 10.1001/archpsyc.1997.01830130062013. [DOI] [PubMed] [Google Scholar]
- Kersting A, Brahler E, Glaesmer H, Wagner B. Prevalence of complicated grief in a representative population-based sample. Journal of Affective Disorders. 2011;131:339–343. doi: 10.1016/j.jad.2010.11.032. [DOI] [PubMed] [Google Scholar]
- Kersting A, Wagner B. Complicated grief after perinatal loss. Dialogues in Clinical Neuroscience. 2012;14(2):187–194. doi: 10.31887/DCNS.2012.14.2/akersting. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King M, Speck P, Thomas A. The royal free interview of spiritual and religious beliefs: development and validation of a self-report version. Psychological Medicine. 2001;31:1015–1023. doi: 10.1017/s0033291701004160. [DOI] [PubMed] [Google Scholar]
- Klass D, Walter T. Processes of grieving: how bonds are continued. In: Stroebe MS, Hansson RO, Stroebe W, Schut H, editors. Handbook of Bereavement: Consequences, Coping, and Care. American Psychological Association; Washington, DC: 2001. pp. 431–448. [Google Scholar]
- Kochanek KD, Kirmeyer SE, Martin JA, Strobino DM, Guyer B. Annual summary of vital statistics: 2009. Pediatrics. 2012;129(2):338–348. doi: 10.1542/peds.2011-3435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koopmans L, Wilson T, Cacciatore J, Flenady V. Support for mothers, fathers and families after perinatal death. Cochrane Database of Systematic Reviews. 2013 doi: 10.1002/14651858.CD000452.pub3. No.: CD000452. DOI: 10.1002/14651858.CD000452.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreicbergs UC, Lannen P, Onelov E, Wolfe J. Parental grief after losing a child to cancer: impact of professional and social support on long-term outcomes. Journal of Clinical Oncology. 2007;25(22):3307–3312. doi: 10.1200/JCO.2006.10.0743. doi: 10.1200/jco.2006.10.0743. [DOI] [PubMed] [Google Scholar]
- Lasker JN, Toedter LJ. Acute vs. chronic grief: the case of pregnancy loss. American Journal of Orthopsychiatry. 1991;61:510–522. doi: 10.1037/h0079288. [DOI] [PubMed] [Google Scholar]
- Li J, Laursen TM, Precht DH, Olsen J, Mortensen PB. Hospitalization for mental illness among parents after the death of a child. The New England Journal of Medicine. 2005;352:1190–1196. doi: 10.1056/NEJMoa033160. [DOI] [PubMed] [Google Scholar]
- Li J, Johansen C, Hansen D, Olsen J. Cancer incidence in parents who lost a child. A nationwide study in Denmark. Cancer. 2002;95:2237–2242. doi: 10.1002/cncr.10943. [DOI] [PubMed] [Google Scholar]
- Lin SX, Lasker JN. Patterns of grief reaction after pregnancy loss. The American Journal of Orthopsychiatry. 1996;66(2):262–271. doi: 10.1037/h0080177. [DOI] [PubMed] [Google Scholar]
- MacDorman MF, Kirmeyer S. Fetal and perinatal mortality, United States, 2005. National Vital Statistics Reports. 2009;57(8):1–19. [PubMed] [Google Scholar]
- Maciejewski PK, Zhang B, Block SD, Prigerson HG. An empirical examination of the stage theory of grief. Journal of the American Medical Association. 2007;297(7):716–723. doi: 10.1001/jama.297.7.716. doi: 10.1001/jama.297.7.716. [DOI] [PubMed] [Google Scholar]
- Meert K, Thurston C, Briller S. The spiritual needs of parents at the time of their child’s death in the pediatric intensive care unit and during bereavement: a qualitative study. Pediatric Critical Care Medicine. 2005;6(4):420–427. doi: 10.1097/01.PCC.0000163679.87749.CA. [DOI] [PubMed] [Google Scholar]
- Murphy SA. A bereavement intervention for parents following the sudden, violent deaths of their 12-28-year-old children: description and applications to clinical practice. The Canadian Journal of Nursing Research. 1997;29(4):51–72. [PubMed] [Google Scholar]
- Murphy SA, Johnson C, Cain KC, Gupta AD, Dimond M, Lohan M, et al. Broad spectrum group treatment for parents bereaved by the violent deaths of their 12 to 28-year-old children: A randomized controlled trial. Death Studies. 1998;22(3):209–235. doi: 10.1080/074811898201560. doi:10.1080/074811898201560. [DOI] [PubMed] [Google Scholar]
- Parkes CM. Guidelines for conducting ethical bereavement research. Death Studies. 1995;19(2):171–181. doi: 10.1080/07481189508252723. doi: 10.1080/07481189508252723. [DOI] [PubMed] [Google Scholar]
- Potvin L, Lasker J, Toedter L. Measuring grief: a short version of the Perinatal Grief Scale. Journal of Psychopathology and Behavioral Assessment. 1989;11(1):29–45. [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Radloff LS, Locke BZ. The community mental health assessment survey and CES-D Scale. In: Weissman MM, Myers JK, Ross CE, editors. Community surveys of psychiatric disorders. Rutgers University Press; New Brunswick, NJ: 1986. pp. 177–187. [Google Scholar]
- Rando TA. An investigation of grief and adaptation in parents whose children have died from cancer. Journal of Pediatric Psychology. 1983;8(1):3–20. doi: 10.1093/jpepsy/8.1.3. [DOI] [PubMed] [Google Scholar]
- Robertson MJ, Aldridge A, Curley AE. Provision of bereavement care in neonatal units in the United Kingdom. Pediatric Critical Care Medicine. 2011;12(3):e111–115. doi: 10.1097/PCC.0b013e3181e911e3. doi: 10.1097/PCC.0b013e3181e911e3. [DOI] [PubMed] [Google Scholar]
- Shear MK, Simon N, Wall M, Zisook S, Neimeyer R, Duan N, et al. Complicated grief and related bereavement issues for DSM-5. Depression and Anxiety. 2011;28(2):103–117. doi: 10.1002/da.20780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stinson KM, Lasker JN, Lohmann J, Toedter LJ. Parents' grief following pregnancy loss: a comparison of mothers and fathers. Family Relations. 1992;41:218–223. [Google Scholar]
- Swanson PB, Pearsall-Jones JG, Hay DA. How mothers cope with the death of a twin or higher multiple. Twin Research. 2002;5:156–64. [PubMed] [Google Scholar]
- Sweeting HN, Gilhooly MLM. Anticipatory grief: a review. Social Science & Medicine. 1990;30(10):1073–1080. doi: 10.1016/0277-9536(90)90293-2. [DOI] [PubMed] [Google Scholar]
- van Baarsen B. Theories on coping with loss: the impact of social support and self-esteem on adjustment to emotional and social loneliness following a partner's death in later life. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 2002;57(1):S33–42. doi: 10.1093/geronb/57.1.s33. [DOI] [PubMed] [Google Scholar]
- Vance JC, Boyle FM, Najman JM, Thearle MJ. Gender differences in parental psychological distress following perinatal death or sudden infant death syndrome. The British Journal of Psychiatry. 1995;167(6):806–811. doi: 10.1192/bjp.167.6.806. [DOI] [PubMed] [Google Scholar]
- Walsh K, King M, Jones L, Tookman A, Blizard R. Spiritual beliefs may affect outcome of bereavement: prospective study. BMJ. 2002;324(7353):1551. doi: 10.1136/bmj.324.7353.1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westfall PH, Tobias RD, Rom D, Wolfinger RD, Hochberg Y. Multiple comparison and multiple tests using the SAS system. SAS Institute Inc.; Cary, NC: 1999. Concepts and basic methods for multiple comparisons and tests; pp. 13–40. [Google Scholar]
- Wing D, Clance P, Burge-Callaway K, Armistead L. Understanding gender difference in bereavement following the death of an infant: implications for treatment. Psychotherapy. 2001;38:60–72. [Google Scholar]
- Youngblut JM, Brooten D, Cantwell GP, del Moral T, Totapally B. Parent health and functioning 13 months after infant or child NICU/PICU death. Pediatrics. 2013;132(5):e1295–1301. doi: 10.1542/peds.2013-1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wortmann JH, Park CL. Religion and spirituality in adjustment following bereavement: an integrative review. Death Studies. 2008;32(8):703–736. doi: 10.1080/07481180802289507. doi: 10.1080/07481180802289507. [DOI] [PubMed] [Google Scholar]
- Zisook S, Shear K, Kendler KS. Validity of the bereavement exclusion criterion for the diagnosis of major depressive episode. World Psychiatry. 2007;6(2):102–107. [PMC free article] [PubMed] [Google Scholar]