Abstract
Evidence-based interventions (EBIs) are effective in preventing ado-lescent pregnancy and sexually transmitted infections; however, prevention practitioners are challenged when selecting and adapting the most appropriate programs. While there are existing adaptation frameworks, there is little practical guidance in applying research in the field. To address this need, the Centers for Disease Control and Prevention (CDC) Division of Reproductive Health initiated the Adaptation Guidance Project. The project included the development of a comprehensive adaptation guidance framework and adaptation kits for select evidence-based teen pregnancy and HIV prevention programs. In addition, three innovative concepts emerged that have application to other adaptation program and evaluation efforts, including moving research into practice. First, the authors defined the core components of an EBI in three distinct ways: core content, core pedagogy, and core implementation. Second, they piloted a practitioner-friendly adaptation guidance-messaging schema—Green, Yellow, and Red Light Adaptations, and last they included fidelity/adaptation monitoring logs. This article will describe the process used to develop the adaptation guidance kits, including the main features and tools.
Keywords: Adaptation, teen pregnancy prevention, HIV prevention, evidence-based interventions, Getting to Outcomes, STI prevention
INTRODUCTION
In 2012, approximately 305,420 babies were born to women aged 15–19 years, for a live birth rate of 29.4 per 1,000 women. This is a record low for U.S. teens in this age group and a drop of 6% from 2011 (Hamilton, Martin, & Ventura, 2013). Despite significant declines, the United States continues to have higher rates of teen pregnancy, sexually transmitted infections (STIs), and HIV than any other industrialized country (Advocates for Youth, 2011). It is also estimated that young people aged 15–24 years, who comprise 25% of those who are sexually experienced, acquire approximately half of all new STIs annually (Weinstock, Berman, & Cates, 2004). Moreover, wide disparities in adolescent reproductive and sexual health outcomes persist. Underprivileged youth and youth of color, particularly Latinos and African Americans, are disproportionately affected by unintended pregnancy, STIs, and HIV (Hogben & Leichliter, 2008; Martin et al., 2012; Mathews, Sutton, Hamilton, & Ventura, 2010; Ventura, Abma, Mosher, & Henshaw, 2008). These disparate outcomes are due to complex, multilevel social determinants that significantly affect outcomes of youth living in at-risk situations (Leigh, Coleman, & Andrews, 2003; Viner et al., 2012).
Evidence-based interventions (EBIs) are programs that have undergone rigorous evaluation using experimental or quasi experimental designs and have demonstrated positive change in adolescent sexual risk behavior (e.g., delay in sexual debut, increase in the correct and consistent use of condoms among sexually active youth). They are one key strategy for reaching youth through prevention education, risk awareness activities, and the knowledge and skills to reduce sexual risk behaviors. A 2007 monograph released by Kirby and LePore (2007) comprehensively reviewed the adolescent reproductive health literature and identified more than 500 risk and protective factors associated with adolescent sexual risk-taking behaviors (e.g., initiating sex at a young age, having multiple sexual partners). In addressing teen pregnancy, STIs, and HIV, practitioners are often advised to view adolescents from a holistic perspective and address several risk and protective factors that influence their reproductive health, including family functioning, mental and physical health, school attachment, and sexual psychosocial determinants. Sexual psychosocial determinants (e.g., knowledge about HIV, attitudes about condoms, skill and self-efficacy to refuse sex) are considered to be those most closely associated with sexual behavior and the most likely to change with a curriculum-based intervention. EBIs designed to prevent teen pregnancy, STIs, and HIV are effective and relatively low-cost strategies to positively change these particular determinants (Kirby, 2007). However, sexual health behavior remains complicated and has many social and individual determinants, suggesting that there is not a “one-size-fits-all” solution to this complex issue.
There is clear agreement that the reproductive and sexual health of adolescents in the United States continues to require the attention and innovation of the practitioners who serve them. Increased use of evidence-based prevention is a critical strategy in any multicomponent effort to meet the needs of youth. However, adolescent reproductive health professionals are continuously challenged to customize available effective programs or strategies to better align the needs of different communities of young people, while maintaining programs’ effectiveness. Clearly, understanding the factors associated with adapting and implementing EBIs is an important step in strengthening the research-to-practice process and improving the likeli-hood that scientifically supported programs are integrated into community programs effectively. While the Centers for Disease Control and Prevention (CDC) has recognized the need for practitioner-oriented adaptation support and made strides to address it, the increasing emphasis on ensuring that federal funds are used only for evidence-based prevention strategies for teen pregnancy, HIV, and STIs demands quicker solutions. Thus, there is a renewed interest and an intense need for guidance related to making appropriate adaptations.
THE ADAPTATION GUIDANCE PROJECT
In 2006, CDC’s Division of Reproductive Health (DRH) initiated efforts to address the needs of adolescent health practitioners to make informed adaptations of EBIs being used in communities across the country. DRH, in collaboration with Education, Training, and Research Associates (ETR), established the Adaptation Guidance Project, which provides practitioners with recommendations, tools, and other resources for making informed adaptations to EBIs to better meet the needs of youth while also maintaining fidelity to the program’s core components. Although numerous EBIs exist, practitioners note that a key barrier to their use is a lack of information on how to select the most appropriate program and to adapt it to the unique characteristics of the target population and the organizations that serve them (Bliesner, Rolleri, & Lezin, 2007; Philliber & Nolte, 2008). For this project, adaptation was defined as the process of making changes to a program in order to make it more suitable for a particular population or for an organization, based upon its capacity. Changes to a program should be made without compromising or deleting the program’s core components, which are the essential characteristics responsible for its effectiveness.
Reasons for Making Adaptations
There are many reasons for practitioners to make adaptations to existing EBIs (e.g., time limitations, responsiveness to community values, local policy compliance, cultural fit to the targeted population, practitioner skill or comfort level regarding the content or teaching methods, desire for greater sense of ownership of the program). For this project, DRH and ETR maintained a perspective that adaptations were part of the natural course of wide-scale implementation and in many instances adaptation could increase the relevance of programs to youth and make wider implementation possible. Thus, we assert that making adaptations (i.e., additions, changes, enhancements) is an acceptable practice and encouraged, as long as the program’s core components are not compromised or deleted, which could potentially lead to poorer outcomes. Some common adaptations included adding or modifying activities, offering the program after school instead of during school, offering it in alternate settings, adjusting to lower reading levels, changing the gender and age composition of groups, and altering the sequence of activities or the details in a role play. Practitioners often were confronted with barriers that prevented them from implementing a program exactly as it was designed and tested and could potentially have an impact on its effectiveness. To overcome these barriers, guidelines and tools are needed to support practitioners in selecting the most appropriate EBI for their target population, identifying and making effective adaptations, and monitoring the effectiveness of these adaptations. It is also imperative that the guidance and tools remain accessible and freely available to a broad range of practitioners.
EXISTING FRAMEWORKS FOR MAKING ADAPTATIONS TO EVIDENCE-BASED PROGRAMS
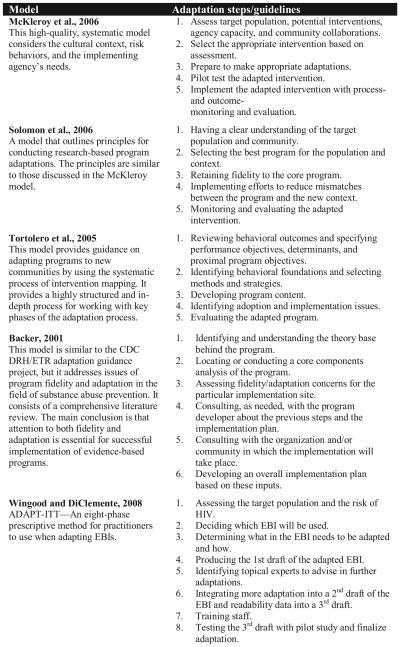
Several broad models have been proposed to assist researchers and practitioners with making program adaptations in the areas of substance abuse, HIV prevention, and adolescent reproductive health. While a few of the models focus exclusively on cultural adaptations, others provide more general guidance for adapting programs to new populations or settings (Backer, 2001; McKleroy et al., 2006; Solomon, Card, & Malow, 2006; Tortolero et al., 2005; Wingood & DiClemente, 2008). Figure 1 summarizes some key adaptation models on which the CDC DRH/ETR Adaptation Guidance Project was based.
FIGURE 1.
Key adaptation models. Note. EBIs = evidence-based interventions.
Each model differs in approach, level of intricacy, and applicability to frontline practitioners, yet all attempt to fit programs to the target audience and to meet the requirements of the implementing agency. In addition, maintaining fidelity to the core components in order to preserve program effectiveness is central to each model, and the significance of gathering accurate community information, selecting the most appropriate program for the population, and conducting quality program monitoring and evaluation are also included. The CDC DRH/ETR Adaptation Guidance Project aimed to build on the common concepts and steps in other published adaptation models for use in DRH grant programs focused on teen pregnancy, HIV, and STI prevention.
Method
After reviewing the various adaptation models (see Figure 1), the CDC DRH/ETR Adaptation Guidance Project asked DRH grantee partners to help guide the outcomes desired from the project. Key informant interviews were conducted at two sites, with a total of 12 practitioners representing CDC DRH Promoting Science-Based Approaches (PSBA) grantees. The one-day interviews included a step-by-step overview of the adaptation guidance and allowed practitioners to provide feedback on the clarity, logic, flow, and practicality of the guidance, using a Likert scale.
Respondents were also able to provide recommendations for improvement and general comments. Participants indicated that most adaptation models were not user-friendly and were too cumbersome, time consuming, and costly to implement. They also expressed that several of the models were research-focused and were not primarily designed for frontline practitioners who generally plan and implement program adaptations. As part of the CDC PSBA project, many partners had consistently articulated the need for practical guidance in implementing programs among populations and in settings different from the original research-based program. They needed access to guidance that was easy to convey to local implementing partners, cost-efficient, and required few resources or highly specialized skills. It was determined that practical (nuts and bolts), user-friendly, adaptation guidance for teen pregnancy and STI/HIV prevention programs was needed.
Embedding Adaptation into a Program-Planning Framework
Program adaptations do not happen in a vacuum but rather as part of a larger process of identifying, selecting, adapting, implementing, and evaluating prevention programming. CDC DRH/ETR recognized that, common to the adaptation models reviewed and to the experience of PSBA grantees, there was a broader context in which adaptation decisions were made. Thus, as part of our approach to the new guidance, a decision was made to integrate the adaptation guidance within a broader program-planning framework, the CDC Promoting Science-Based Approaches—Using Getting To Outcomes (PSBA-GTO) model.
PSBA-GTO successfully combines the approaches and best practices in teen pregnancy prevention with the capacity-building process of Getting To Outcomes (Lesesne et al., 2011). This 10-step program-planning, implementation, and evaluation process was also developed and used as part of the CDC PSBA project (Lesesne et al., 2008; Lesesne et al., 2011; Lewis et al., 2012). Selecting and appropriately adapting programs are vital to the overall PSBA-GTO process, including all critical steps and phases addressed in the adaptation literature. As such, these are the major prevention practice concepts for adapting guidance resources and increasing the probability that the implemented programs will be appropriate to and accepted by the targeted youth and the community (Lesesne et al., 2011). In PSBA-GTO, Step 4—Fit—applies most of these activities (Lesesne et al., 2011).
Selecting Evidence-Based Programs and Engaging Developers
The initial step in the project was to develop criteria, described in a supporting article, for classifying a program as evidence-based (Rolleri, Wilson, Paluzzi, & Sedivy, 2008). Next, DRH and ETR conducted an extensive review of existing EBIs, from which five programs were selected for the development of adaptation guidelines based on usage by CDC DRH PSBA grantees. The five initial programs included:
Becoming a Responsible Teen (St. Lawrence, 2005).
Making a Difference (Jemmott, Jemmott, & McCaffree, 2005).
Making Proud Choices (Jemmott, Jemmott, & McCaffree, 2006).
Reducing the Risk (Barth, 2004).
Safer Choices (Coyle et al., 2001; Coyle & Fetro, 2007).
Once the EBIs were selected for this project, DRH and ETR staff contacted the developers to discuss project details and determine how to involve them in the vetting of guidance related to their program(s). After all developers indicated willingness to participate in the project, the process of developing the guidance for each program was initiated. The resulting process and products are detailed below.
RESULTS
An adaptation kit, including multiple practitioner-friendly tools and resources, was developed for each of the five EBIs selected for this project, three of which are currently published: Becoming a Responsible Teen Adaptation Kit (Rolleri et al., 2011), Reducing the Risk Adaptation Kit (Lezin, Rolleri, Wilson, Fuller et al., 2011), and Safer Choices Adaptation Kit (Lezin, Rolleri, Wilson, Taylor et al., 2011). Each adaptation kit was developed to provide practitioners with a clear understanding of how the EBI was designed, its core components, and the types of adaptations that maintain the evidence-based core components. A six-step process was developed to create the tools and resources in each adaptation kit. Each of the tools underwent extensive reviews by experienced practitioners, CDC DRH PSBA grantees, behavioral scientists, and the chief developer of the selected EBI. The steps and tools resulting from completing each step are described below.
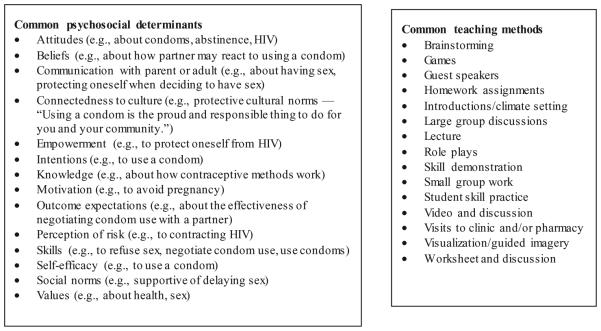
Step 1: Determinant-Activity Matrix
The adaptation team initiated analysis of each evidence-based intervention by reviewing the activities in every lesson and coding them for answers to the following two questions: a) What psychosocial determinant is this activity trying to change? b) What teaching method is being used to teach it? In addition, the team estimated the time spent on each determinant and on each teaching method in the program. Determinants are the psychosocial and environmental factors that have a causal influence on sexual behaviors. Equally important to understanding the determinants is understanding the pedagogy used to teach about those determinants. Figure 2 shows examples of common determinants found in EBIs designed to prevent teen pregnancy and STI/HIV and of common teaching methods used in these programs.
FIGURE 2.
Common psychosocial determinants and teaching methods found in five evidence-based teen pregnancy and STI/HIV prevention programs.
Step 2: Behavior-Determinant-Intervention (BDI) Logic Model
After analyzing each program’s activities, we developed a preliminary BDI logic model describing the link between activities and goals for each EBI. The BDI logic model is a program-development and evaluation tool that guides program developers through four sequential steps. The BDI logic model was selected for this project since it was widely used by CDC DRH PSBA grantees, was relatively easy to create, and was easy to interpret (Kirby, 2004). The four elements of a BDI logic model are a) establish a health goal (e.g., reduce teen pregnancy), b) identify and select teen behaviors directly related to that health goal (e.g., delay onset of sexual activity), c) identify and select the determinants related to those behaviors (e.g., attitudes about personal limits), and d) develop intervention activities directly related to changing those determinants (e.g., role play practice of refusal skills) (Figure 3) (Kirby, 2004). In effect, a BDI logic model reveals the developer’s theory of change, that is, which determinants need to be changed in order to get adolescents to change their sexual behaviors. Each preliminary BDI logic model for the five EBIs was reviewed, refined, and finalized in collaboration with the EBI developer.
FIGURE 3.
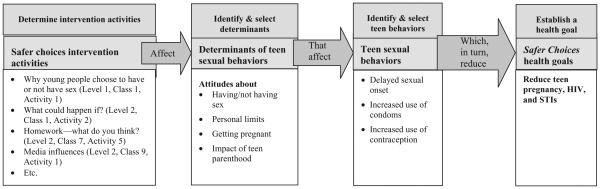
Graphic depiction of a partial behavioral-determinant-intervention (BDI) logic model for Safer Choices adaptation kit (Lezin et al., 2011). Note. STIs = sexually transmitted infections.
Step 3: Core Components
After developing the BDI logic model for each program, the adaptation team was better able to identify the curriculum’s core components, the essential pieces of a curriculum that are responsible for its effectiveness. Core components, also referred to as core elements, include a variety of curriculum characteristics such as sequence of lessons, curriculum activities, and curriculum topics. In the CDC DRH/ETR project, the adaptation team created a typology for core components that included three categories: core content components, core pedagogical components, and core implementation components. This differentiation within the core components was an innovation developed by this effort. Each type of core component is equally important but qualitatively different.
Core content components describe the important content, subjects, or topics that must be taught in a curriculum to maintain its effectiveness. Core content components align very closely with the psychosocial determinants (e.g., attitudes about condoms, knowledge about where to obtain condoms, skill to use a condom effectively) addressed in the curriculum and the behavior change theories on which it is based.
Core pedagogical components describe how the content should be taught in order to be effective. For example, in order to learn a skill like refusing to have sex, students must have the opportunity to practice and receive feedback on how well they perform the skill. Simply listening to a teacher lecture about how to refuse a sexual advance or read a pamphlet about refusing to have sex is not effective in learning and mastering a skill (Kirby, 2007).
Core implementation components describe the logistics needed to implement a curriculum effectively. These components may include teacher-student ratio, setting, preparations, and so on.
These three categories allowed the adaptation team to analyze and communicate clearly about the core components of each curriculum, to emphasize the importance of each category, and to allow developers to think critically about which features among these could be adapted and how. Tables describing the core content, pedagogical, and implementation components (in comprehensive and at-a-glance versions) are found in each of the adaptation kits. Brief examples from tables can be found in Figures 4, 5, and 6.
FIGURE 4.
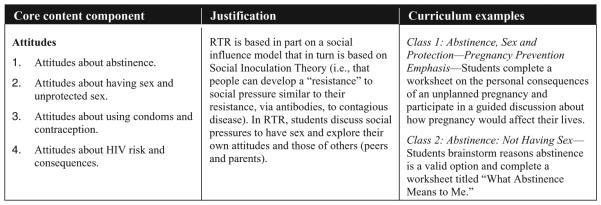
Example of core content components from Reducing the Risk (RTR) adaptation kit (Lezin et al., 2011).
FIGURE 5.
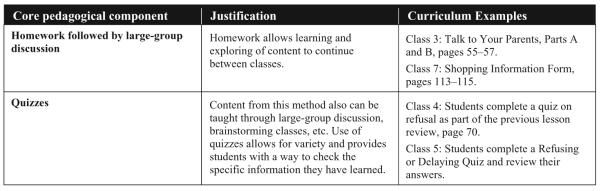
Example of core pedagogical components from Reducing the Risk (RTR) adaptation kit (Lezin et al., 2011).
FIGURE 6.
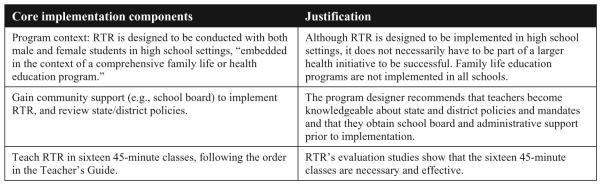
Example of core implementation components from Reducing the Risk (RTR) adaptation kit (Lezin et al., 2011).
Step 4: Green/Yellow/Red Light Adaptations
With the core components established, the team and developer partners moved to the specific adaptation guidance for each EBI. It was important to ensure that the guidance was straightforward and practitioner-friendly. Therefore, CDC DRH/ETR developed an easy system known as the Green/Yellow/Red (GYR) Light Adaptation guidance tool. The GYR framing allowed for a clear and practical way to define appropriate and inappropriate adaptations and to determine which changes could be made with minimal impact on effectiveness.
Specifically, the GYR light guidance tool described the types of adaptations that are safe (green); those that merit caution and the support of an expert in curriculum development, pedagogy, or health behavior change theory (yellow); and those that should be avoided (red). The tool contained two sections: a) GYR light adaptations that apply generally to the EBIs, and b) GYR light adaptations for each activity in each of the select EBI lessons. A list of general GYR light adaptations found in at least two of the three curricula used in the final adaptation kits is shown in Figure 7.
FIGURE 7.
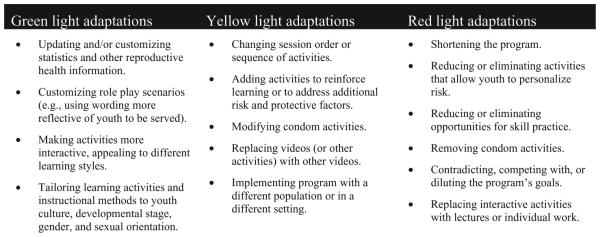
General green, yellow, and red light adaptations.
Step 5: Fidelity and Adaptation Monitoring Logs
Using the core components tables and the GYR light adaptation tables, fidelity and adaptation monitoring logs were developed for each of the adaptation kits. For an example of the logs, see Figure 8. These basic logs are a tool that can help practitioners assess their implementation of an EBI with planned adaptations, affirm what is going well in the implementation, and identify areas that can be in improved in the future. Based on many practitioner reviews, the adaptation team wanted to develop a tool that would take only a few minutes to complete while still asking questions that are specific enough to help the facilitator stay accountable to the program’s core components. A unique feature of the logs was allowing users to calculate a fidelity percentage based on how faithful the implementation was to the core components. Several fidelity/adaptation monitoring tools (Caldwell, 2005; Chinman, Imm, & Wandersman, 2004; Chinman et al., 2008; Clark & Miller, 2010) were reviewed prior to developing the logs that are part of this project.
FIGURE 8.
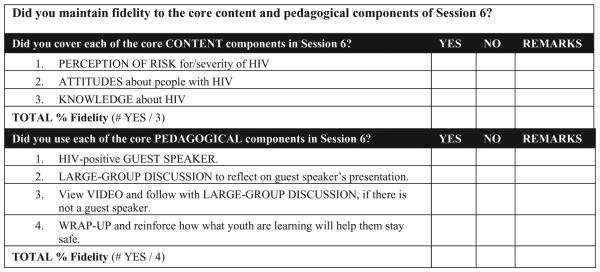
Excerpts from core content and pedagogical fidelity and monitoring logs from Becoming a Responsible Teen adaptation kit (Rolleri et al., 2011).
Step 6: Companion Resources
Based on practitioner feedback, we developed six annotated lists of re-sources for practitioners to use when making informed green and yellow light adaptations. These lists were resources related to adolescent reproductive health data; teen pregnancy, STIs, and HIV; common pedagogical methods used in evidence-based interventions; program assessment and evaluation; cultural competency; and program fidelity and adaptation.
GENERAL ADAPTATION GUIDANCE FOR EBIS
Once the resources specific to the three final adaptation guidance kits were developed, the authors analyzed the GYR light adaptations common to all three curricula. The purpose of this effort was to produce a general adaptation guidance document that would be useful to practitioners seeking to adapt EBIs with similar BDI logic models, since specific guidance on every EBI was beyond the scope of this project. General Adaptation Guidance: A Guide to Adapting Evidence-Based Sexual Health Curricula provides a practical summary of GYR light adaptations that can be used in many adaptation situations (Firpo-Triplett & Fuller, 2012). It is based upon analysis of the three published kits, but it may be applicable to other programs as well. It is available for practitioners seeking to adapt EBIs for which there currently is no specific adaptation guidance.
TRANSLATION OF ADAPTATION TOOLS AND RESOURCES TO THE FIELD
Effective program adaptations are best made when they are addressed throughout the program-planning process. For example, assessments of the youth to be served and the capacity of the organization to deliver the program will yield important data that can be used when planning adaptations. Similarly, an understanding of how to select the program best matched to the youth being served will help limit the number of adaptations that need to be made. Evaluating the adaptations made during one implementation of a program will help with future implementations, and the adaptation kits developed in this project will support practitioners in identifying, making, and monitoring adaptations. The kits were designed to be flexible because practitioners are not directed to use the tools in a particular order. The kits, however, do not address other important steps of a comprehensive program-planning process. As noted earlier, PSBA-GTO can serve as an excellent framework for planning program adaptations (Lesesne et al., 2011). The general adaptation guidance document is another resource that can help practitioners working to make quality adaptations in the absence of specific guidance.
CONCLUSION AND NEXT STEPS
The CDC DRH/ETR Adaptation Guidance Project designed a six-step method for developing EBI-specific adaptation guidance. The project culminated in three published comprehensive adaptation tool kits: Becoming a Responsible Teen Adaptation Kit (Rolleri et al., 2011), Reducing the Risk Adaptation Kit (Lezin, Rolleri, Wilson, Fuller et al., 2011), and Safer Choices Adaptation Kit (Lezin, Rolleri, Wilson, Taylor et al., 2011). These program-specific adaptation kits each contain: a BDI logic model, core components, GYR light adaptation guidance, and fidelity and adaptation monitoring logs. Key constructs for understanding and making appropriate adaptations have further contributed to the field of evidence-based practice, notably:
The core component categories of content, pedagogy, and implementation;
The GYR light system for understanding adaptations; and
General adaptation guidance for use with sexual health EBIs that have similar BDI logic models.
In addition, other CDC DRH/ETR adaptation tools are available, including the Sisters, Informing, Healing, Living, Empowering (SiHLE) Adaptation Kit (Lezin, Firpo-Triplett, Fuller, & Wingood, 2012). This kit utilizes the same process as the published kits and provides extensive guidance to those interested in adapting a clinic-based HIV prevention program developed specifically for young African American females.
Our distinctive guidance to adapting EBIs and the resulting tools inform the work of practitioners and researchers in various topic areas, including sexual and reproductive health, violence, physical education, and school health (CDC, 2012; CDC Division of Adolescent and School Health, 2010; CDC National Center for Chronic Disease Prevention and Health Promotion Work Group on Translation, 2010; Coyle, 2011). The concept and practitioner-friendly format of the adaptation guidance have been well received and have been used as a model for the development of similar kits for other EBIs. In 2010, the Office of the Assistant Secretary for Health/Office of Adolescent Health (OASH/OAH), with ETR, developed and published three EBI-specific adaptation kits: Draw the Line/Respect the Line: Setting Limits to Prevent HIV, STD and Pregnancy (Coyle et al., 2003; Marin, Coyle, Gomez, Jinich, & Kirby, 2003; Marin, Coyle, Cummings et al., 2003), All4You: Preventing HIV, Other STD and Pregnancy Among Young People in Alternative Education Settings (Coyle, 2011), and Safer Sex Intervention: An Individualized Intervention for High-Risk Adolescent Girls (Shrier et al., 2010). These adaptation kits underscore the necessity for program adaptation at the local level and the need to continue to provide resources for practitioners as they select, adapt, and implement EBIs across the country. It also reinforces our belief that the transferability and applicability of the CDC DRH/ETR adaptation concepts can help practitioners to bridge science and practice while focusing on practicality.
As the role of adaptation has increased in recent years and the literature continues to emerge, more intervention developers have expressed plans to produce their own EBI-specific adaptation guidance. Whenever possible, this approach is highly desirable since intervention developers are familiar with their own programs and often have the ability to connect to the conceptual foundations on which the programs were designed. This insight is crucial to the development of adaptation guidance and provides further credibility to the process. We strongly support and encourage intervention developers and others tasked with developing adaptation guidance to devote a good deal of attention to producing user-friendly tools for published EBI, including logic models, core components, and clear direction on appropriate, acceptable adaptations—using the GYR light rubric where possible so practitioners can easily manage the process of making informed adaptations. These tools, as previously discussed, are items practitioners have found most useful to them in the field.
Limitations
The adaptation field is an emerging area with many issues subject to individual developer interpretation, as well as to the changes that occur as new information becomes available and new challenges arise. This continuous evolution can render guidelines outdated as core components are changed, new information emerges from the field, or new evaluation results arise. Because of this evolution, we recommend that adaptation guidelines be updated periodically. It is also important to note that we conducted extensive reviews of published and non-published adaptation related materials to guide this project. In the absence of research-based information, the expertise of project staff and intervention developers guided the conclusions. However, this article would not be complete without mentioning some of the challenges encountered.
Because of limited resources and the immediate need for practitioners to use EBIs and adapt them with quality, the specific guidance, while expert-informed, has not been validated through research. The cost to validate each specific type of guidance is simply too great and not feasible given the large body of EBIs that exist today. For this reason and in support of quality prevention program practice, we strongly encourage practitioners to use a program-planning, implementation, and evaluation process similar to PSBA-GTO (Lesesne et al., 2011) so that process and outcome evaluation are part of ensuring that adapted EBIs are still achieving their intended health outcomes.
The CDC DRH/ETR Adaptation Guidance Project’s novel approach to making program-specific adaptation kits and general adaptation guidance tools has been well received by practitioners and researchers. As evaluation of innovative adapted EBIs under the OASH/OAH Teen Pregnancy Prevention Initiative continues, understanding of how well the adaptation guidance performs in a community context will increase.
The CDC/DRH Adaptation Kits and General Adaptation Guidance can be found at: http://www.etr.org/recapp/index.cfm?fuseaction=pages.AdaptationsHome.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Contributor Information
LORI A. ROLLERI, Independent Consultant, Bellerose, NY, USA.
TALERIA R. FULLER, Division of Reproductive Health, Centers for Disease Control and Prevention, Atlanta, GA, USA.
REGINA FIRPO-TRIPLETT, Center for Sexual and Reproductive Health Promotion, Education, Training and Research Associates, Scotts Valley, CA, USA.
CATHERINE A. LESESNE, Public Health Division, ICF Macro, Atlanta, GA, USA.
CLAIRE MOORE, Independent Contractor, Austin, TX, USA.
KIMBERLY D. LEEKS, Division of HIV/AIDS Prevention, Centers for Disease Control and Prevention, Atlanta, GA, USA.
REFERENCES
- Advocates for Youth . Advocates for youth: Adolescent sexual health in Europe and the U.S. 4th Author; Washington, DC: 2011. [Google Scholar]
- Backer TE. Finding the balance: Program fidelity and adaptation in substance abuse prevention: Executive summary of a state-of-the-art review. U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration Center of Substance Abuse Prevention; Rockville, MD: 2001. [Google Scholar]
- Barth RB. Reducing the risk: Building skills to prevent pregnancy, STD and HIV. 4th ETR Associates; Scotts Valley, CA: 2004. [Google Scholar]
- Bliesner M, Rolleri L, Lezin N. Interviews with representatives of state adolescence pregnancy prevention coalitions (APPCs) and regional training centers (RTCs): Study findings and implications. ETR Associates; Scotts Valley, CA: 2007. [Google Scholar]
- Caldwell LL. TimeWise: Taking charge of leisure time, preventing substance abuse. ETR Associates; Scotts Valley, CA: 2005. [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Implementing and Adapting Evidence-Based Interventions. CDC Division of Violence Prevention: Federal Partner Adaptation Panel; Atlanta, GA: Sep, 2012. [Google Scholar]
- CDC Division of Adolescent and School Health . Identifying Efficacious Programs to Reduce Adolescent Sexual Risk Behavior. Expert Panel Meeting; Atlanta, GA: Aug, 2010. [Google Scholar]
- CDC National Center for Chronic Disease Prevention and Health Promotion Work Group on Translation . Providing Technical Assistance on Using Evidence Workshop; Atlanta, GA: Jun, 2010. [Google Scholar]
- Chinman M, Hunter SB, Ebener P, Paddock SM, Stillman L, Imm P, Wandersman AA. The getting to outcomes demonstration and evaluation: An illustration of the prevention support system. American Journal of Community Psychology. 2008;41:3–4. doi: 10.1007/s10464-008-9163-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinman M, Imm P, Wandersman A. Getting to outcomes 2004: Promoting accountability through methods and tools for planning, implementation, and evaluation. RAND Corporation; Santa Monica, CA: 2004. [Google Scholar]
- Clark L, Miller K. Project AIM (adult identity mentoring): A program to reduce HIV sexual risk among youth. Children’s Hospital Los Angeles; Los Angeles, CA: 2010. [Google Scholar]
- Coyle K. All4You: Preventing HIV, other STD and pregnancy among young people in alternative education settings. ETR Associates; Scotts Valley, CA: 2011. [Google Scholar]
- Coyle K, Basen-Engquist K, Kirby D, Parcel G, Banspach S, Collins J, Harrist R. Safer choices: Reducing teen pregnancy, HIV, and STDs. Public Health Reports. 2001;116(Suppl 1):82–93. doi: 10.1093/phr/116.S1.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyle K, Marin B, Gardner C, Cummings J, Gomez C, Kirby D. Draw the line/respect the line: Setting limits to prevent HIV, STD and pregnancy, grade 7. ETR Associates; Scotts Valley, CA: 2003. [Google Scholar]
- Coyle KK, Fetro JV. Safer choices: Preventing HIV, other STDs and pregnancy, level 2. ETR Associates; Scotts Valley, CA: 2007. rev. [Google Scholar]
- Firpo-Triplett R, Fuller TR. General adaptation guidance: A guide to adapting evidence-based sexual health curricula. ETR Associates; Santa Cruz, CA: 2012. [Google Scholar]
- Hamilton BE, Martin JA, Ventura SJ. National Vital Statistics Report. 3. Vol. 62. National Center for Health Statistics; Hyattsville, MD: 2013. Births: Preliminary data for 2012; pp. 1–20. [PubMed] [Google Scholar]
- Hogben M, Leichliter JS. Social determinants and sexually transmitted disease disparities. Sexually Transmitted Diseases. 2008;35(12 Suppl):S13–18. doi: 10.1097/OLQ.0b013e31818d3cad. [DOI] [PubMed] [Google Scholar]
- Jemmott LS, Jemmott JB, McCaffree KA. Making a difference!: An abstinence approach to HIV/STDs and teen pregnancy prevention. Select Media; New York, NY: 2005. [Google Scholar]
- Jemmott LS, Jemmott JB, & McCaffree KA. Making proud choices!: A safer sex approach to HIV/STDs and teen pregnancy prevention. 3rd Select Media; New York, NY: 2006. [Google Scholar]
- Kirby D. Logic models: A useful tool for designing, strengthening and evaluating programs to reduce adolescent sexual risk-taking, pregnancy, HIV and other STDs. ETR Associates; Scotts Valley, CA: 2004. [Google Scholar]
- Kirby D. Emerging answers 2007: Research findings on programs to reduce teen pregnancy and sexually transmitted diseases. The National Campaign to Prevent Teen Pregnancy; Washington, DC: 2007. [Google Scholar]
- Kirby D, LePore G. Sexual risk and protective factors: Factors affecting teen sexual behavior, pregnancy, childbearing, and sexually transmitted disease: Which are important? Which can you change? ETR Associates; Scotts Valley, CA: 2007. [Google Scholar]
- Leigh WA, Coleman KD, amp; Andrews JA. Does place matter? Racial/ethnic differences in reproductive health outcomes of adolescents. Joint Center for Political and Economic Studies; Washington, DC: 2003. [Google Scholar]
- Lesesne CA, Lewis KM, Moore C, Fisher D, Green D, & Wandersman A. Promoting science-based approaches to teen pregnancy prevention using getting to outcomes (Unpublished manual) CDC Division of Reproductive Health; Atlanta, GA: 2011. [Google Scholar]
- Lesesne CA, Lewis KM, White CP, Green DC, Duffy JL, Wandersman A. Promoting science-based approaches to teen pregnancy prevention: Proactively engaging the three systems of the interactive systems framework. American Journal of Community Psychology. 2008;41:379–392. doi: 10.1007/s10464-008-9175-y. [DOI] [PubMed] [Google Scholar]
- Lewis KM, Lesesne CA, Zahniser C, Wilson MM, Desiderio G, Wandersman A, Green DC. Developing a prevention synthesis and translation system to promote science-based approaches to teen pregnancy, HIV and STI prevention. American Journal of Community Psychology. 2012;50(3):553–571. doi: 10.1007/s10464-012-9510-1. doi: 10.1007/s10464-012-9510-1. [DOI] [PubMed] [Google Scholar]
- Lezin N, Firpo-Triplett R, Fuller TR, & Wingood GM. Sisters, informing, healing, living, empowering (SiHLE) adaptation kit. ETR Associates; Santa Cruz, CA: 2012. [Google Scholar]
- Lezin N, Rolleri LA, Wilson MM, Fuller TR, Firpo-Triplett R, Barth RP, & Coyle K. Reducing the risk adaptation kit. ETR Associates; Scotts Valley, CA: 2011. [Google Scholar]
- Lezin N, Rolleri LA, Wilson MM, Taylor J, Fuller TR, Firpo-Triplett R, & Coyle K. Safer choices adaptation kit. ETR Associates; Scotts Valley, CA: 2011. [Google Scholar]
- Marin B, Coyle K, Cummings J, Gardner C, Gomez C, & Kirby D. Draw the line/respect the line: Setting limits to prevent HIV, STD and pregnancy, grade 8. ETR Associates; Scotts Valley, CA: 2003. [Google Scholar]
- Marin B, Coyle K, Gomez C, Jinich S, & Kirby D. Draw the line/respect the line:Setting limits to prevent HIV, STD and pregnancy, grade 6. ETR Associates; Scotts Valley, CA: 2003. [Google Scholar]
- Martin JA, Hamilton BE, Ventura SJ, Osterman MJK, Wilson EC, Matthews TJ. National Vital Statistics Reports. 1. Vol. 61. National Center for Health Statistics; Hyattsville, MD: 2012. Births: Final data for 2010; pp. 1–72. [PubMed] [Google Scholar]
- Mathews TJ, Sutton PD, Hamilton BE, Ventura SJ. State disparities in teenage birth rates in the U.S. National Center for Health Statistics Data Brief. Vol. 46. National Center for Health Statistics; Hyattsville, MD: 2010. pp. 1–8. [PubMed] [Google Scholar]
- McKleroy VS, Galbraith JS, Cummings B, Jones P, Harshbarger C, Collins C, ADAPT Team Adapting evidence-based behavioral interventions for new settings and target populations. AIDS Education and Prevention. 2006;18(Supplement A):59–73. doi: 10.1521/aeap.2006.18.supp.59. [DOI] [PubMed] [Google Scholar]
- Philliber S, Nolte K. Implementation science: Promoting science-based approaches to prevent teen pregnancy. Prevention Science. 2008;9(3):166–177. doi: 10.1007/s11121-008-0094-9. [DOI] [PubMed] [Google Scholar]
- Rolleri LA, Lezin N, Taylor J, Moore C, Wilson MM, Fuller TR, Firpo-Triplett R, & Coyle K. Reducing the risk adaptation kit. ETR Associates; Scotts Valley, CA: 2011. [Google Scholar]
- Lawrence J. Becoming a responsible teen adaptation kit. ETR Associates; Scotts Valley, CA: 2011. [Google Scholar]
- Rolleri LA, Wilson MM, Paluzzi PA, Sedivy VJ. Building capacity of state adolescent pregnancy prevention coalitions to implement science-based approaches. American Journal of Community Psychology. 2008;41:225–234. doi: 10.1007/s10464-008-9177-9. [DOI] [PubMed] [Google Scholar]
- Shrier L, Ancheta R, Goodman E, Chiou V, Lyden M, & Emans SJ. Safer sex intervention: An individualized intervention for high-risk adolescent girls. Sociometrics; Los Altos, CA: 2010. [DOI] [PubMed] [Google Scholar]
- Solomon J, Card JJ, Malow RM. Adapting efficacious interventions: Advancing translational research in HIV prevention. Evaluation and Health Professions. 2006;29(2):162–194. doi: 10.1177/0163278706287344. [DOI] [PubMed] [Google Scholar]
- St. Lawrence J. Becoming a responsible teen!: An HIV risk reduction program for adolescents. ETR Associates; Scotts Valley, CA: 2005. rev. [Google Scholar]
- Tortolero SR, Markham CM, Parcel GS, Peters RJ, Escobar-Chaves L, Basen-Enquist K, Lewis HL. Using intervention mapping to adapt an effective HIV, sexuality transmitted disease, and pregnancy prevention program for high-risk minority youth. Health Promotion Practice. 2005;6:286–298. doi: 10.1177/1524839904266472. [DOI] [PubMed] [Google Scholar]
- Ventura SJ, Abma JC, Mosher WD, Henshaw SK. National Vital Statistics Reports. Vol. 56. National Center for Health Statistics; Hyattsville, MD: 2008. Estimated pregnancy rates by outcome for the United States, 1990–2004; pp. 1–26. [PubMed] [Google Scholar]
- Viner RM, Ozer EM, Denny S, Marmot M, Resnick M, Fatusi A, Currie C. Adolescence and the social determinants of health. Lancet. 2012;379:1641–1652. doi: 10.1016/S0140-6736(12)60149-4. doi:10.1016/S0140-6736(12)60149-4. [DOI] [PubMed] [Google Scholar]
- Weinstock H, Berman S, Cates W., Jr. Sexually transmitted diseases among American youth: Incidence and prevalence estimates, 2000. Perspectives in Sexual and Reproductive Health. 2004;36(1):6–10. doi: 10.1363/psrh.36.6.04. [DOI] [PubMed] [Google Scholar]
- Wingood GM, DiClemente RJ. The ADAPT-ITT model: A novel method of adapting evidence-based HIV interventions. Acquired Immune Deficiency Syndrome. 2008;47(supplement 1):40–46. doi: 10.1097/QAI.0b013e3181605df1. [DOI] [PubMed] [Google Scholar]