Abstract
Early or late post-implant placement complications are usually localized infectious/inflammatory processes and treated accordingly. If the healing process does not take place within a reasonable timeframe, the possibility of a pathologic process beyond localized infection/inflammation should be suspected. We describe a radiological/histopathological spectrum of bony lesions ranging from inflammatory to malignant lesions surrounding failed dental implants. Five cases of mandibular dental implant failure that clinically, radiologically and histopathologically appeared to be inflammatory processes are presented. The failure of the dental implants was immediate in two cases and late in the remaining three. The radiological features were essentially similar for all five, and they included radiolucent or mixed radiolucent–radiopaque lesions with poorly defined borders. Three lesions were limited to the area of the failed implant, while the other two extended to a large part of the mandible. The histopathological findings ranged from acute osteomyelitis and chronic osteomyelitis with features of a fibro-osseous-like lesion and occasional rimming of atypical osteoblasts to osteogenic sarcoma that was admixed with a component of osteomyelitis (diagnosis of the latter was achieved only after a series of biopsies). In-depth investigative procedures are imperative in order to establish an accurate diagnosis whenever the histopathological diagnosis is inconsistent with persisting clinical signs and symptoms in bone lesions associated with failed dental implants.
Keywords: Dental implant failure, Histopathology, Osteomyelitis, Osteogenic sarcoma
Introduction
Dental implants have become the most popular therapeutic technique for rehabilitation of edentulous alveolar ridges for the past two decades [1]. Pathological lesions that develop in the soft tissue adjacent to dental implants are usually of the inflammatory, plaque-induced type (i.e., peri-implant mucositis) [2, 3] and seldom of the reactive type (i.e., peripheral giant cell granuloma and pyogenic granuloma) [4, 5]. There have been less than twenty documented cases of primary squamous cell carcinoma that have developed in the soft tissues of the alveolar ridge surrounding dental implants, occasionally with a component involving the bone surrounding the implant or presenting as primary intraosseous squamous cell carcinoma adjacent to a dental implant [6]. Other types of malignancies that have been reported in close proximity to dental implants are anecdotal, and include one case each of plasmacytoma [7] and osteogenic sarcoma [8].
Implant failure can be arbitrarily classified into early (failure to achieve osseointegration) and late (failure to maintain established osseointegration during functional loading) [9, 10]. The etiology of early failure is assumed to include excessive surgical trauma, impaired healing, bacterial contamination and premature overloading, and that for late failure to include excessive occlusal stress and bacterial-induced peri-implant bone loss [9–11]. Clinical manifestation of early and late implant failure can be either symptomatic or asymptomatic (i.e., only affecting mobility) with or without radiological changes. The radiological change that is usually seen surrounding an implant failure is that of a peri-implant radiolucency, frequently with irregular contours [9, 10]. Untreated bacteria-induced peri-implantitis may eventually lead to deep bone invasion of the bacteria and cause true osteomyelitis, which is a rare complication relative to the large number of dental implants that are placed nowadays [12]. Acute and subsequent secondary chronic osteomyelitis in the context of implant failures has been reported in a small number of patients [10, 13–18]. Radiological features that are mainly associated with the chronic form of osteomyelitis consist of poorly-defined, moth-eaten, radiolucent bone loss admixed with radio-opaque areas, representing the formation of a bony sequestrum [12].
The present report describes a spectrum of lesions within the bone surrounding failed dental implants. The radiological and histopathological features of these lesions, ranging from inflammatory to malignant lesions, will be discussed.
Case Series
Between 2011 and 2012 four patients were referred to the Department of Oral and Maxillofacial Surgery (OMS) at the Chaim Sheba Medical Center, Tel Hashomer, for treatment of clinically diagnosed failure of dental implants. An additional patient was treated at Hadassah Medical Center, Jerusalem, and referred to OMS for consultation. Two patients presented with immediate implant failure and three with late failure.
Patient #1
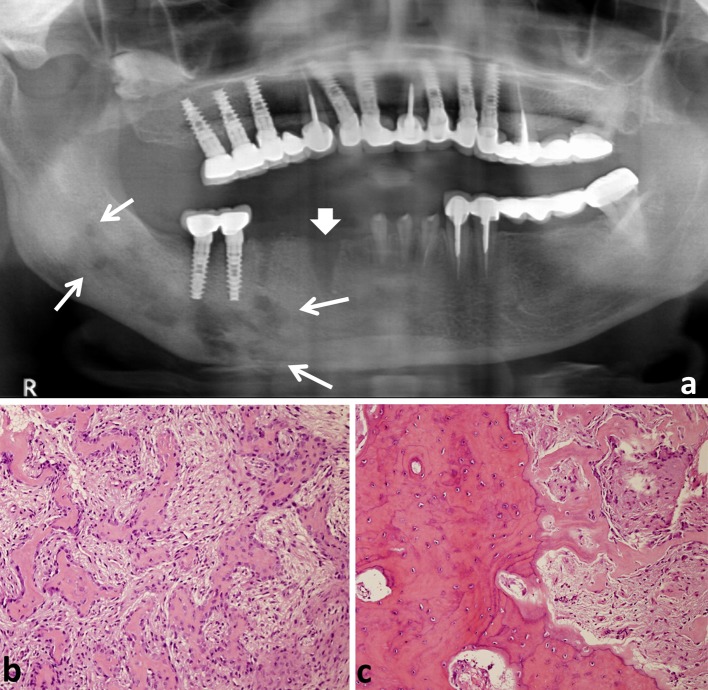
A 68-year-old female with a medical history of diabetes and hypercholesterolemia was referred to our OMS department due to vestibular edema and an inflammatory process in the area of a dental implant in the left mandibular premolar area that was placed several years ago. She received antibiotic treatment for 3 weeks, but the pain was not alleviated and a purulent exudate was present in the area of the implant. A panoramic X-ray revealed the absence of bony support around the implant that had replaced the mandibular second premolar (Fig. 1a). At surgery, the implant was removed, the area curetted, and a bony sequestrum was removed. Histopathological examination revealed fragments of non-vital bone surrounded by numerous bacterial colonies and acute and chronic inflammation (Fig. 1b). She was diagnosed as having chronic osteomyelitis with acute exacerbation and sequestrum formation. There was a slight improvement in the pain and swelling at the follow-up examination 2 months later.
Fig. 1.

a A crater-like, well-defined, radiolucent bony defect is seen surrounding the dental implant replacing the left mandibular second premolar. There are fine radio-opaque small structures in the distal area of the lesion. b Biopsy material shows necrotic bone and inflammatory infiltrate (HE, original magnification ×100)
Patient #2
A 58-year-old male with a medical history of hypertension was referred to our OMS department due to non-healing process in the edentulous area of the lower first molar. He had undergone extraction of the mandibular first and second molars with immediate implants in that area 10 months earlier. Two months after the procedure, the implant replacing the first molar was removed due to pain: there was no clinical evidence of osseointegration. He underwent two curettage procedures in that area during the ensuing 3 months, which were followed by artificial bone augmentation. Four months later, a panoramic X-ray revealed a mixed radiolucent–radiopaque lesion suspected as being osteomyelitis. An additional curettage procedure was performed and a biopsy was taken. The histopathological picture revealed a fragment of non-vital woven bone with many reversal lines, reminiscent of a Pagetoid pattern, and fibrotic bone marrow with chronic inflammation (Fig. 2). These features were compatible with chronic osteomyelitis. The follow-up radiological X-rays and lack of clinical symptoms 6 months later revealed that a healing process was ongoing.
Fig. 2.
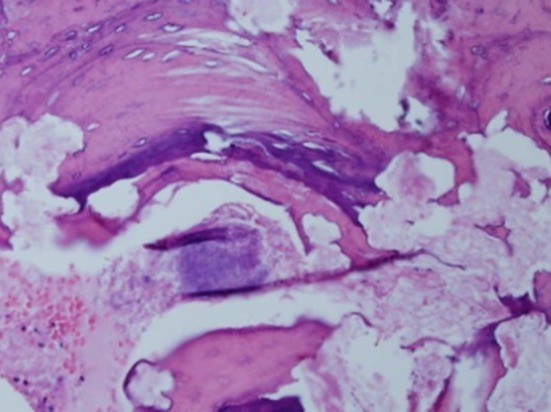
Fragments of non-vital bone (HE, original magnification ×200)
Patient #3
A 59-year-old female with a medical history of hypertension and asthma underwent the removal of a failing implant in the area of the right mandibular second premolar ~6 months before her referral to our OMS department. The decision to remove the implant was supported by the patient’s complaint of pain and swelling in that area that did not improve with long-term antibiotic treatment. The persistent swelling in the area of the removed implant had increased in size 2 weeks before she presented to our department. The clinical examination revealed firm and very tender right submandibular swelling and lingual and buccal cortical expansion in the body of the right mandible. The panoramic X-ray showed a poorly defined mixed radiolucent–radiopaque lesion extending from the right lower first premolar to the angle of the mandible that was suspected to be osteomyelitis (Fig. 3a). The area was curetted and a detached sequestrum was removed under general anesthesia. The microscopic examination revealed areas of granulation tissue and areas of hypercellular connective tissue associated with the formation of woven bone trabeculae mostly rimmed by plump osteoblasts. The latter areas were reminiscent of a fibro-osseous lesion (Figs. 3b, c). Another fragment was composed of necrotic bone, consistent with a sequestrum. 8 months after that surgical procedure, the patient still complained of pain, and a computerized tomographic (CT) scan confirmed features compatible with unresolved osteomyelitis. The patient started long-term treatment with doxycycline hydrochloride 100 mg once daily and she is being closely monitored.
Fig. 3.
a A mixed radiolucent–radiopaque, poorly defined lesion extending from the area of the mandibular first premolar to the angle of the mandible (arrows). The “socket” of the removed failing dental implant is still visible ~6 months after tooth extraction (thick arrow). b Irregular trabeculae of woven bone in a background of a cellular connective tissue, reminiscent of a fibro-osseous lesion (HE, original magnification ×200). c Woven bone forming on the existing bone (HE, original magnification ×200)
Patient #4
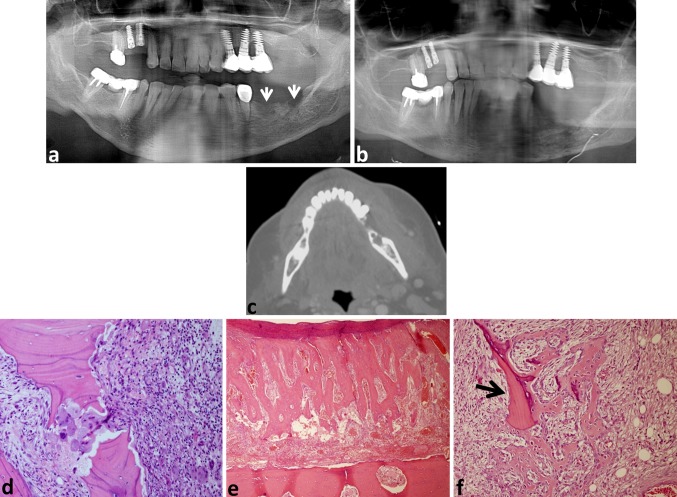
A 64-year-old female with a medical history of hypertension, diabetes and hypercholesterolemia was referred to our OMS department due to left submandibular and sublingual swelling and a cutaneous fistula with a purulent discharge. Two weeks earlier, she had undergone surgery for placing 2 dental implants in the area of a missing left mandibular second premolar and a first molar. The implants were removed 1 week later due to unbearable pain and swelling. A panoramic X-ray showed “sockets” of the removed implants (Fig. 4a). Another panoramic X-ray that was taken 2 weeks later showed a diffuse, poorly defined mixed radiolucent–radiopaque process occupying most of the left mandibular body (Fig. 4b). A CT scan highlighted the extensive buccal and lingual cortical bone loss associated with the soft tissue swelling (Fig. 4c). A biopsy was taken and showed residual bone with acute and some chronic inflammation similar to Patients #1 and #2, as well as multinucleated cells consistent with osteoclasts (Fig. 4d). She was diagnosed as having osteomyelitis, with the possibility of a secondary chronic subtype and underwent partial mandibulectomy with immediate plate reconstruction under general anesthesia. The microscopic examination of the specimen revealed that the cortical and trabecular bone were vital in most parts. There was extensive periosteal bone formation (Fig. 4e) with trabeculae of osteoid and woven bone that were partially rimmed by osteoblasts. Those cells showed some hyperchromatism and atypia. There was a background of moderately cellular connective tissue that also contained dispersed chronic inflammatory cells. All of those features were compatible with chronic osteomyelitis, although the presence of osteoid bone and the formation of new bone over local residual bone (Fig. 4f) together with the atypical osteoblasts raised the possibility of a low-grade osteosarcoma. The patient has been given long-term intravenous antibiotic treatment because the healing process was slow and compromised due to her general health status.
Fig. 4.
a The arrows point to the “sockets” of the removed implants. b 2 weeks later, the bone loss that was previously limited to the implant “sockets” now appears as a poorly defined, mixed radiolucent–radiopaque process occupying most of the left mandibular body. c A CT scan performed at the same time as (b) highlights the extensive buccal and lingual cortical bone loss. Soft tissue swelling corresponding to the destructive bony process can be observed. d Residual bone with resorption lacunae and inflammation (HE, original magnification ×200). e Remarkable periosteal bone formation. The mandibular bone is seen at the bottom of the field (HE, original magnification ×100). f Woven bone in a background of moderately cellular connective tissue. The woven bone is occasionally forming over remnants of residual trabeculae (arrow) (HE, original magnification ×200)
Patient #5
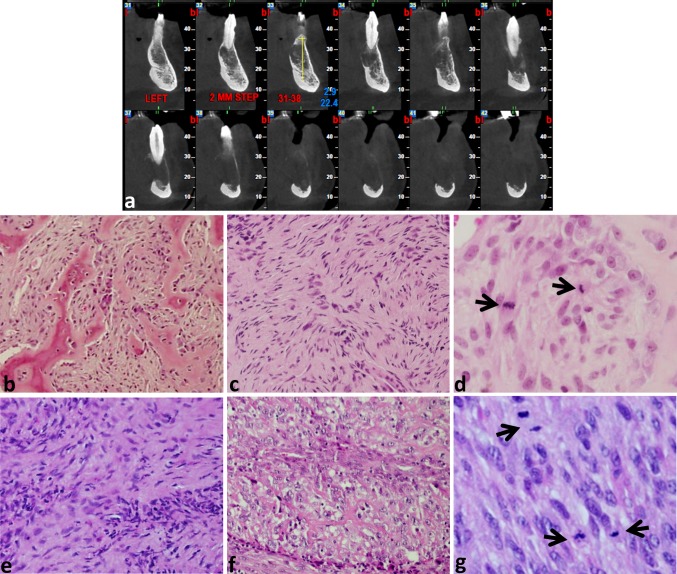
A 75-year-old female with a medical history of hypertension had undergone removal of a failing dental implant in the second molar of the left mandible. The implant had been placed 5 years previously, and the patient complained of recent-onset pain. The CT scan taken after removal of the implant showed an irregular bone loss with a poorly defined hypodense appearance. There was extensive thinning in some areas and almost complete destruction of the buccal and lingual cortices. There was also some lingual expansion between the second molar and the anterior area of the mandible (Fig. 5a). Two sequential biopsies were taken 1 month apart due to a poor healing process. The results of the biopsies were similar and showed tissue fragments composed of fine trabeculae of woven bone rimmed by epithelioid osteoblasts within a cellular stroma (Fig. 5b), similar to the histopathological findings in the biopsy taken from Patient #4 (Fig. 4f). Other areas were composed of connective tissue that was partially hyalinized with alternating cellular areas, often infiltrated by chronic inflammatory cells, including several multinucleated giant cells. The more cellular areas were composed of connective tissue with spindle cells that were arranged in short intersecting bundles. Some of the spindle cells had a plump nucleus with mild atypia (Fig. 5c). Mitotic figures were occasionally observed (Fig. 5d). The proliferation index among the stromal, non-inflammatory cells, as assessed by Ki-67, was ~4 %. Collectively, these findings were interpreted as representing a fibro-osseous lesion, but the possibility was raised that the biopsies were not representative of the entire nature of the lesion. The level of the patient’s pain intensified and the cortical expansion continued to increase during the next 5 months. A new biopsy (Fig. 5e) showed some features similar to those seen in the previous biopsies, however the material was now predominantly occupied by an infiltrating, hypercellular mass with mostly spindle-shaped atypical cells associated with osteoid formation (Fig. 5f). Necrotic areas were present, as were numerous mitotic figures, including atypical ones (Fig. 5g). Based on these findings, she was diagnosed as having high-grade osteogenic sarcoma for which she underwent treatment with palliative radiation that resulted in only partial response.
Fig. 5.
a A CT scan demonstrating irregular bone loss in the area of first left central incisor to the mid-body of the mandible. b Trabeculae of woven bone rimmed by osteoblasts within a cellular stroma (HE, original magnification ×200). c Spindle cells arranged in short intersecting bundles some of them show mild nuclear atypia (HE, original magnification ×200). d Mitotic figures (arrows) (HE, original magnification ×600). e Short intersecting bundles of spindle cells and foci of inflammatory infiltrate (HE, original magnification ×200). f Lace-like osteoid (HE, original magnification ×400). g Cellular area with several mitotic figures (arrows) (HE, original magnification ×600)
Discussion
The current series of failed dental implants, irrespective of their occurrence at an early or late stage, shared a clinical picture that pointed to the manifestation of an infectious/inflammatory process, characterized by signs of swelling, pain, fistula and purulent exudate. The radiological features were essentially similar, and included radiolucent or mixed radiolucent–radiopaque lesions with poorly defined borders. Some of them were limited to the area of the failed implant (Patients #1–3), while others were extensive and involved a large part of the mandible (Patients #4 and #5). The histopathological findings ranged from acute osteomyelitis and chronic osteomyelitis with features of a fibro-osseous-like lesion and occasional rimming of atypical osteoblasts, to osteogenic sarcoma that was admixed with a component of osteomyelitis.
The importance of the present study lies in raising awareness to the fact that what is clinically, radiologically and histopathologically diagnosed as a failed dental implant-related inflammatory process might conceal life-threatening conditions. Thus, in the event that the healing process is not progressing as expected, the possibility that the biopsy is not representative of the true nature of the lesion should be considered. Patient #5 clearly showed that a malignancy could be obscured by a florid inflammatory process at both clinical and radiological levels, and that the correct diagnosis could have been expedited had there been multiple representative biopsies from the extensive lesion.
Development of osteogenic sarcoma of the jawbones in association with dental implants has been reported in the English language literature in only one publication [8]. In that case, the osteogenic sarcoma developed in the premolar–molar area of the maxilla 11 months after the patient had received a titanium dental implant. At surgery, the tumor appeared to be directly associated with the dental implant.
In contrast with the exceedingly rare dental implant-related osteogenic sarcoma in the jawbones, development of an osteogenic sarcoma in association with orthopedic metal implants is well documented, albeit it also constitutes a rare event [19, 20]. The reported interval from implant placement to the development of malignancy ranged from 6 months to 30 years, with a mean of 9 years [19]. In our presented case, the osteogenic sarcoma was discovered 5 years after the placement of the implant.
The etiopathological basis for a malignancy to be associated with orthopedic metal implants is speculative, and a number of possibilities have been suggested. Animal models revealed that elements, such as beryllium, cobalt, nickel and titanium, among other metals, possess carcinogenic properties [8, 19, 20]. Several studies have demonstrated that culturing osteoblasts on titanium substrates induces upregulation of selected genes involved in osseointegration [21, 22]. This can also be the basis for altered gene expression in conjunction with the evolution of a neoplastic process. Another suggestion is that the placement of an implant induces osteonecrosis, which is considered to be a risk factor for the development of a sarcoma [19]. It is, of course, not possible to ascribe direct cause and effect relationships between the use of dental implants and malignancy based on our single case of high-grade osteogenic sarcoma.
In summary, we present 5 cases of failed dental implants that clinically suggested infectious/inflammatory condition. 3 of these 5 lesions presented radiologically as a localized process in the vicinity of the implant, while the process was remarkably extensive and extended far beyond the region of the implant in the remaining two cases. The diagnosis of 3 lesions was histopathologically obvious and fully supported the clinical picture. However, the diagnosis of 2 lesions, especially the extensive ones, was obscured by the inflammatory process. Thus, whenever the histopathological diagnosis is in disagreement with persisting clinical signs and symptoms in spite of adequate treatment, further investigative procedures are imperative in order to establish an accurate diagnosis.
Acknowledgments
The authors thank Dr. Itzhak Neuman and Dr. Alex Mali from Hadassah Medical Center, Ein Kerem, Jerusalem, for the histopathological material in Case #5. The authors thank Ms. Esther Eshkol for editorial assistance. This study was partially supported by the Ed and Herb Stein Chair in Oral Pathology, Tel Aviv University.
References
- 1.Ng DY, Wong AY, Liston PN. Multidisciplinary approach to implants: a review. N Z Dent J. 2012;108:123–128. [PubMed] [Google Scholar]
- 2.Khammissa RA, Feller L, Meyerov R, Lemmer J. Peri-implant mucositis and peri-implantitis: clinical and histopathological characteristics and treatment. S Afr Dent J. 2012;67(122):124–126. [PubMed] [Google Scholar]
- 3.Armas J, Culshaw S, Savarrio L. Treatment of peri-implant diseases: a review of the literature and protocol proposal. Dent Update. 2013; 40:472–4, 476–8, 480. [DOI] [PubMed]
- 4.Dojcinovic I, Richter M, Lombardi T. Occurrence of a pyogenic granuloma in relation to a dental implant. J Oral Maxillofac Surg. 2010;68:1874–1876. doi: 10.1016/j.joms.2009.06.015. [DOI] [PubMed] [Google Scholar]
- 5.Peñarrocha-Diago MA, Cervera-Ballester J, Maestre-Ferrín L, Peñarrocha-Oltra D. Peripheral giant cell granuloma associated with dental implants: clinical case and literature review. J Oral Implantol. 2012;38(Spec):527–532. doi: 10.1563/AAID-JOI-D-11-00143. [DOI] [PubMed] [Google Scholar]
- 6.Pfammatter C, Lindenmuller IH, Lugli A, Filippi A, Kuhl S. Metastases and primary tumors around dental implants: a literature review and case report of peri-implant pulmonary metastasis. Quintessence Int. 2012;43:563–570. [PubMed] [Google Scholar]
- 7.Poggio CE. Plasmacytoma of the mandible associated with a dental implant failure: a clinical report. Clin Oral Implant Res. 2007;18:540–543. doi: 10.1111/j.1600-0501.2007.01361.x. [DOI] [PubMed] [Google Scholar]
- 8.McGuff HS, Heim-Hall J, Holsinger C, Jones AA, O’Dell DS, Hafemaister AC. Maxillary osteosarcoma associated with a dental implant. Report of a case and review of the literature regarding implant-related sarcomas. J Am Dent Assoc. 2008;139:1052–1059. doi: 10.14219/jada.archive.2008.0307. [DOI] [PubMed] [Google Scholar]
- 9.Esposito M, Thomsen P, Ericson LE, Lekholm U. Histopathological observations on early implant failures. Int J Oral Maxillofac Implant. 1999;14:798–810. [PubMed] [Google Scholar]
- 10.Esposito M, Thompsen P, Ericson LE, Sennerby L, Lekholm U. Histopathologic observations on late implant failures. Clin Implant Dent Relat Res. 2000;2:18–32. doi: 10.1111/j.1708-8208.2000.tb00103.x. [DOI] [PubMed] [Google Scholar]
- 11.Wiskott HW, Dubrez B, Scherrer SS, Belser UC. Reversible and irreversible peri-implant lesions: report and etiopathogenetic analysis of 7 cases. J Oral Implantol. 2004;30:255–266. doi: 10.1563/1548-1336(2004)30<255:RAIPLR>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 12.Zimmerli W. Osteomyelitis therapy–antibiotic therapy. In: Baltensperger MM, Eyrich GK, editors. Osteomyelitis of the jaws. Berlin: Springer; 2009. pp. 179–190. [Google Scholar]
- 13.Kesting MR, Thurmuller P, Ebsen M, Wolff KD. Severe osteomyelitis following immediate placement of a dental implant. Int J Oral Maxillofac Implant. 2008;23:137–142. [PubMed] [Google Scholar]
- 14.O’Sullivan D, King P, Jagger D. Osteomyelitis and pathological mandibular fracture related to a late implant failure: a clinical report. J Prosthet Dent. 2006;95:106–110. doi: 10.1016/j.prosdent.2005.10.014. [DOI] [PubMed] [Google Scholar]
- 15.Piattelli A, Cosci F, Scarano A, Trisi P. Localized chronic suppurative bone infection as a sequel of peri-implantitis in a hydroxyapatite-coated dental implant. Biomaterials. 1995;16:917–920. doi: 10.1016/0142-9612(95)93116-U. [DOI] [PubMed] [Google Scholar]
- 16.Piattelli A, Scarano A, Piattelli M. Abscess formation around the apex of a maxillary root from implant: clinical and microscopical aspects. A case report. J Periodontol. 1995;66:899–903. doi: 10.1902/jop.1995.66.10.899. [DOI] [PubMed] [Google Scholar]
- 17.Rokadiya S, Malden NJ. An implant periapical lesion leading to acute osteomyelitis with isolation of Staphylococcus aureus. Br Dent J. 2008;205:489–491. doi: 10.1038/sj.bdj.2008.935. [DOI] [PubMed] [Google Scholar]
- 18.Sussman HI, Moss SS. Localized osteomyelitis secondary to endodontic-implant pathosis. A case report. J Periodontol. 1993;64:306–310. doi: 10.1902/jop.1993.64.4.306. [DOI] [PubMed] [Google Scholar]
- 19.Keel SB, Jaffe KA, Nielsen GP, Rosenberg AE. Orthopaedic implant-related sarcoma: a study of twelve cases. Mod Pathol. 2001;14:969–977. doi: 10.1038/modpathol.3880420. [DOI] [PubMed] [Google Scholar]
- 20.Adams JE, Jaffe KA, Lemons JE, Siegal GP. Prosthetic implant associated sarcoma: a case report emphasizing surface evaluation and spectroscopic trace metal analysis. Ann Diagn Pathol. 2003;7:34–46. doi: 10.1053/adpa.2003.50006. [DOI] [PubMed] [Google Scholar]
- 21.Ogawa T, Nishimura I. Genes differentially expressed in titanium implant healing. J Dent Res. 2006;85:566–570. doi: 10.1177/154405910608500617. [DOI] [PubMed] [Google Scholar]
- 22.Takeuchi K, Saruwatari L, Nakamura HK, Yang JM, Ogawa T. Enhanced intrinsic biomechanical properties of osteoblastic mineralized tissue on roughened titanium surface. J Biomed Mater Res A. 2005;72:296–305. doi: 10.1002/jbm.a.30227. [DOI] [PubMed] [Google Scholar]