Abstract
Aim
To evaluate the preventative effect of intravenous 4 mg of dexamethasone and 8 mg oral dexamethasone on post-operative pain, swelling and trismus after the surgical extraction of mandibular third molars.
Materials and methods
A randomized clinical trial comprised of 200 patients (control group I intravenous and experimental group II orally) with impacted lower third molars, average age 20.8 years with no local or systemic problems, with bilateral impacted lower third molars, were operated under local anesthesia. Group I was given 4 mg IV and group II was given 8 mg orally of dexamethasone 1 h before procedure. The choice of which side to operate first and the amount of concentration of medication to use was made randomly and double-blindly. Post-operative pain was evaluated using a visual analog scale (VAS) and the degree of swelling was evaluated through facial reference points' variation. The presence of trismus was analyzed through measurement of the interincisal distance (IID). These assessments were obtained before the operation and 24 h, 48 h and 7th POD.
Results
No significant difference was found in facial swelling and trismus between IV 4 mg injection and oral 8 mg consumption after lower third molar surgery (student t test P > 0.05). The visual analogue scale scores for pain assessment showed no significant difference between IV injection and oral route of dexamethasone (student t test P > 0.05).
Conclusion
Patients can be administered 8 mg oral dexamethasone is as effective as 4 mg intra venous route without much difference in final outcome at any given point of time.
Keywords: Impacted mandibular third molar, Dexamethasone, Swelling, Pain, Trismus
1. Introduction
Surgical extraction of the mandibular third molar is one of the most common minor surgical procedure carried out in the Oral and Maxillofacial Field.1,2 It is afflicted by various forms of injury. Normally our body will respond to any type of injury in a peculiar & predictable manner which shows in the form of cardinal signs of inflammation. Being maxillofacial region is a highly vascularized and constituted by loose connective tissue of the liberation of exudates and subsequent resulting in swelling, trismus and pain still more.3 This result in more exaggerated response is predicted compared to other part of the body in of functional and structural form.
To control post-operative inflammation and symptoms associated, it is necessary to provide an adequate anti-inflammatory therapy intra and post-operative period. For several decades surgeons administered corticosteroids before or just after third molars' surgery to reduce inflammation and associated symptoms after oral surgical procedure. It is demonstrated that a better effect in the control of the swelling and trismus when using steroid anti-inflammatory drugs versus non steroidal anti-inflammatory drugs.4–6 One of such drug is administration of corticosteroids (CS), by the action of the anti-inflammatory effects of cortisone and Adrenocorticotropic Hormone (ACTH). The use of these CS in the treatment of Rheumatoid Arthritis (RA), the fact that increased its popularity among medical authorities which was reported by Hench et al (1950).7
Corticosteroids mechanism of action includes the inhibition of the enzyme Phospholipase A2 (PLA 2), which reduces the release of arachidonic acid in the cells of the inflamed focus. This will decrease prostaglandins' and leukotrienes synthesis, therefore reducing the accumulation of neutrophils, which explains, at least partly, the greatest power of corticosteroids compared to non steroidal anti-inflammatory drugs (NSAID'S).8
However, the clinical use of this type of drugs should be moderate, rational, for shorter period of time, and smaller dose because, according to endocrinology analyses, after the 5th day of use, the therapy has already begun to produce immunosuppression. In some patients it may take up to 9 months to return to normal levels when it is used for longer period. Some studies show the use of different doses but they don't compare them.8–11
Many patients will be apprehensive for receive IV medication. For them alternatively we can substitute enteric route. But the absorption may be delayed which might alters the action of the same.
Taking into account these facts, the purpose of the present study was to compare the effects of pre-operative administration of two different dosages (4 mg and 8 mg) and routes (intravenous and oral) of dexamethasone on post-operative pain, swelling and trismus after third molar surgery.
2. Materials and methods
A prospective, randomized, controlled, double blind, parallel group design study was conducted with the approbation of the Department of Oral and Maxillofacial Surgery over the period of two years from September, 2012 to September, 2014. The procedures were explained to the patients verbally and in writing, and informed consent was taken before enrollment. Those who were not ready or fail to report according to the set criteria, excluded from the study. The patients were randomly allocated to two groups i.e. control group I 4 mg intravenous administration and experimental group II 8 mg orally administration group.
200 healthy patients (control group I 100 and experimental group II 100) with impacted lower third molars, with bilateral lower third molar in similar positions i.e. class II and position B (Pell and Gregory's classification)12 along with same degree of surgical difficulty (Pederson's Index) (Table 1), age between 19 and 34 years (mean 20.8 years). All the patients had no history of allergy to dexamethasone, amoxicillin, or acetaminophen, and had no use of other medicines one month before and during the study period. Prior to the surgical procedure, a detailed case history was taken and an oral examination was performed, including a panoramic radiograph and IOPA, to confirm the need for third molar removal. The choice of surgical procedure was randomly allocated for both control (group I) and experimental (group II) groups. The operating surgeon was not allowed to know the dosages used for the respective sides. The surgical procedure was performed after 1 h of the random choice of the determination of the side and dose of dexamethasone. . Both the patients and the surgeon were blinded to the use of corticosteroid. A third person not involved in the study was made incharge of dispensing the solution randomly and maintaining the record of solution dispensed to each patient. This record was not revealed to the investigators till the completion of study and obtaining results.
Table 1.
Type of lower third molar in similar positions.
| Type of LTM | Numbers |
|---|---|
| Horizontal LTM impaction | 104 |
| Distoangular LTM impaction | 30 |
| Mesioangular LTM impaction | 66 |
For standardization of the sample, we used the following clinical criteria: 1) Age between 19 and 34 years, 2) Bilateral impacted third molars (According to Pell and Gregory's classification), 3) Equivalent degree of surgical difficulty (Pederson's Index) comparing one side with the other, 4) Absence of any systemic disease.
All the patients made a mouthwash with chlorhexidine tablets 0.2% (Water dissolvable) before administration of local anesthesia (lidocaine 2% with epinephrine 1:200,000) at the area to be operated. Standard inferior alveolar nerve block and long buccal nerve block of surgical site was given and the surgical procedure is performed to remove the third molars under standard protocol.
In the post-operative period, an antibiotic (oral amoxicillin 500 mg, three times daily for three days) and 500 mg of acetaminophen three times daily every 8th hourly for 3 days was prescribed. The patients were also instructed to record the number of rescue drugs consumed by the seventh post-operative day.
The pain was evaluated in the post-operative period using a visual analog scale (VAS) of 10 point scale. Mouth opening was measured using the maximum mouth opening before the surgical procedure and evaluated at 24 h, 48 h and 7th day post-extraction.
The evaluation of the facial swelling was performed using a horizontal and vertical guide with a flexible ruler following control points as described by Neupert et al.11 The facial measures corresponded with: 1. Tragus of the Ear, 2. Mid point on the chin (soft tissue), 3. Lateral canthus of the eye and 4. Angle of the mandible (Figs. 1 and 2).
Fig. 1.

Measurement between points A and B.
Fig. 2.

Measurement between the points C and D.
The percentage of facial swelling was obtained from the difference of the measures made in the preoperative and post-operative periods, dividing the result by the value obtained in the preoperative period and multiplying it by one-hundred (100). The evaluation of the post-operative facial swelling was carried out at 24 h and 48 h and 7 days after the procedure. The established periods of time between the surgeries were determined previously 2 weeks.
The collected data were stored electronically and analyzed using the Statistical Analysis System (SAS) by means of descriptive statistic and the student t test and test of Wilcoxon of signalled ranks. The level of significance used in the statistical decisions was P < 0.05.
3. Results
Two Hundred (200) patients of both genders, between 19 and 34 years (mean 20.8 years) with impacted lower third molars comprised the sample of this study. Fig. 3 demonstrates the flow diagram for patient recruitment and selection. 200 patients were initially selected. However, five did not participate in the study follow-up period. The time of surgery using 4 mg IV of dexamethasone was 30.659 ± 3.76 and using 8 mg orally was 29.84 ± 5.54 without statistical differential among them (P = 0.3250) (Table 2).
Fig. 3.
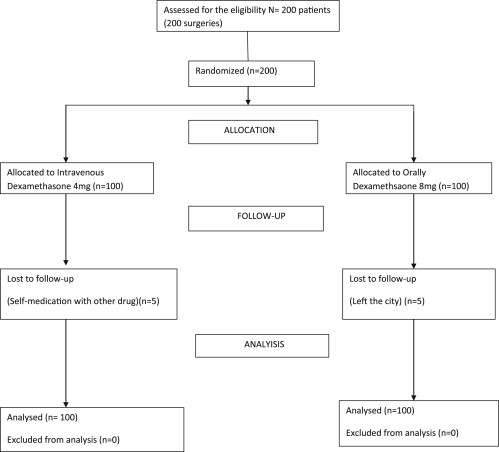
Flow chart diagram.
Table 2.
Operation time for lower third molar surgery.
| Time(min) | Group I – intra venous | Group II – oral | P value |
|---|---|---|---|
| Range | 22–34 | 24–35 | 0.3250 |
| Mean | 30.659 | 29.84 | |
| SD | 3.76 | 5.54 |
It has no statistical differential between the used amount of anesthetic solution with both amounts of dexamethasone (P = 0.8550).
The 4 mg dexamethasone I.V. injection and 8 mg dexamethasone orally groups showed no significant differences in post-operative facial swelling after lower third molar surgery on days 1, 2, and 7 i.e. P > 0.05 (Table 3) (Figs. 4 and 5).
Table 3.
Mean and Standard Deviation (SD) of the studied measurement of swelling in relation with the evaluation time and dosage administered.
| Measures | Time |
4 mg iv |
8 mg Tab |
P value |
|---|---|---|---|---|
| Mean (SD1) | Mean (SD2) | |||
| Tragus – Mentalis | Pre-operative | 87.63 (4.89) | 90.19 (4.62) | P = 0.083 |
| 24 Hours post-operative | 89.26 (4.90) | 90.85 (4.56) | P = 0.502 | |
| 48 Hours post-operative | 90.19 (4.28) | 92.52 (5.11) | P = 0.631 | |
| 7th Post-operative day | 87.78 (4.86) | 90.37 (4.61) | P = 0.004 | |
| Angle – Outer canthus of the nose | Pre-operative | 77.63 (5.02) | 79.67 (7.74) | P = 0.093 |
| 24 Hours post-operative | 81.07 (4.27) | 81.19 (8.01) | P = 0.867 | |
| 48 Hours post-operative | 83.30 (4.61) | 81.30 (8.47) | P = 0.376 | |
| 7th Post-operative day | 77.68 (5.02) | 79.73 (7.74) | P = 0.003 |
Fig. 4.
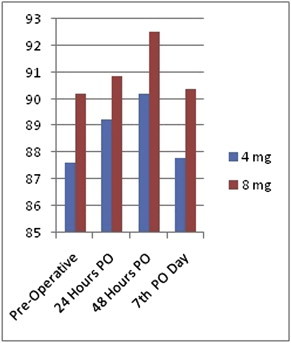
Tragus – Mentalis distance.
Fig. 5.
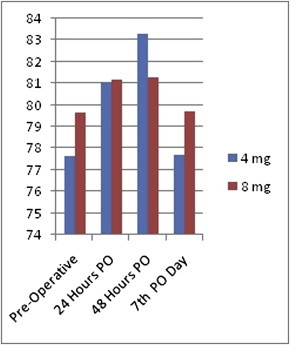
Angle – Ala of the nose distance.
No significant differences were observed in between the groups regarding maximum interincisal distance preoperatively and on post-operative days 1, 2, and 7 i.e P > 0.05 (Table 4) (Fig. 6).
Table 4.
Mean and Standard Deviation (SD) of the studied measurement of mouth opening in relation with the evaluation time and dosage administered.
| Measures | Time |
4 mg iv |
8 mg Tab |
P value |
|---|---|---|---|---|
| Mean (SD1) | Mean (SD2) | |||
| Inter incisal distance | Pre-operative | 44.64 (4.71) | 46.74 (5.67) | P = 0.089 |
| 24 Hours post-operative | 29.83 (4.71) | 30.39 (8.60) | P = 0.426 | |
| 48 Hours post-operative | 26.57 (3.42) | 33.54 (8.64) | P = 0.569 | |
| 7th Post-operative day | 44.29 (4.61) | 46.39 (5.48) | P = 0.002 |
Fig. 6.
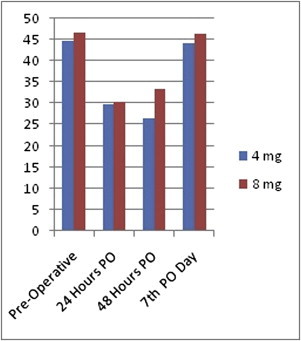
Inter incisal distance.
No statistically significant differences were found between protocols with regards to post-operative pain among the two groups (Table 5). And the total amount of acetaminophen consumption was not significantly different (Table 6).
Table 5.
Mean pain measurement by visual analogue pain scale in points.
| Groups | Number | Mean | SD | P value | |
|---|---|---|---|---|---|
| Preop-pain | Group A | 100 | 1.24 | 1.12 | 0.874 |
| Group B | 100 | 1.28 | 1.39 | ||
| IPO-pain | Group A | 100 | 1.54 | 1.23 | 0.754 |
| Group B | 100 | 1.46 | 1.31 | ||
| 2nd Day-pain | Group A | 100 | 1.7 | 1.42 | 0.0012 |
| Group B | 100 | 1.5 | 1.60 | ||
| 7th Day-pain | Group A | 100 | 1.7 | 1.17 | 0.000 |
| Group B | 100 | 1.4 | 1.5 |
Table 6.
Amount of consumption of analgesics among two routes and two doses using Wilcoxon test.
| Dexamethasone 4 mg intravenous median (D1–D3) | Dexamethasone 8 mg orally median (D1–D3) | P value | |
|---|---|---|---|
| Analgesic consumption (n) | 9 (5.26–12.00) | 8.5 (6.25–11.5) | 0.54 |
4. Discussion
Surgery of impacted third molars is one of the most frequent procedures in Oral and Maxillofacial Surgery2–4 and can lead to immediate post-operative pain and discomfort.2,6–8
The literature provides the number of studies on the analgesic and anti-inflammatory effects of different doses and routes of administration of dexamethasone.1,2,4–6,13–16,23 On the contrary basis, no comparative analysis were available regarding the pre-emptive effect of two routes of administration of dexamethasone on trismus, pain and swelling after lower third molar surgery. With our current knowledge, the present prospective study is the first to compare the effects of two routes intravenous versus orally-administered as a single dose pre-operatively 1 h before the surgical procedure.
Trismus is a direct sequel of the post-operative swelling, being able to compress the nervous structures and generate mild to severe pain.5 Dexamethasone was chosen for the study because it has shown to be a drug of safe administration and acts for longer period, if time and dosages are strictly followed. The employed antibiotic was amoxicillin and analgesic was acetaminophen, also another proven drug of safe administration and because of the fact that it doesn't modify platelet's aggregation, coagulation time or neutrophil's action.10
Many studies have demonstrated the safety of intravenous dexamethasone.17 Filho et al16 reported the administration of 8 mg dexamethasone was more effective than 4 mg dexamethasone. Many studies emphasize the effects of dexamethasone in dentoalveolar surgery in many types, dosages and times of administration. The current study compared the effects of 4 mg dexamethasone given by intravenous route 1 h before the procedure and orally 8 mg dexamethasone 1 h before the procedure in reducing post-operative swelling, pain and trismus in bilateral third molar surgery.
The inflammatory response and consequent post-operative complications associated with third molar extraction are influenced by factors such as surgical difficulty and patient characteristics. Thus, measures were adopted in an attempt to control the variability within and between patients. Although the Pell and Gregory classification has been questioned as an appropriate method for determining the complexity of third molar extractions,18,19 one well-controlled clinical trial found that the radiographic position for impacted teeth could be a good indicator of surgical difficulty and was associated with post-operative complications.14 In the present study, the patients were operated on by the same surgical team and had their teeth in the same radiographic position.
The duration of the surgery and number of rescue analgesics consumed by the patients were evaluated for the control of possible confounding factors that could influence responses regarding the three variables studied (swelling, pain and trismus) As no statistically significant differences were found between protocols (Tables 1 and 6), no multivariate analysis was performed. As reported in the past studies,9,11,20 the number of analgesics ingested seems not to be governed by the administration of corticosteroids.
Many previous studies regarding facial swelling14,21 illicit the dexamethasone can reduce facial swelling significantly, with many different regimes. The present study showed that facial swelling by facial measurements in both groups pre-operatively had no significant differences. The patients in both groups credibly swelled slightly in third molar surgery.
Trismus is also a common complication following third molar extraction and can have a negative impact on quality of life by hampering eating and speaking.22 Filho et al16 found the administration of 8 mg dexamethasone was more effective than 4 mg of dexamethasone to reduce the degree of trismus. In our study, we have used maximum interincisal distance to study trismus and found there were no significant differences on days 1,2 and 7 after lower third molar surgery among both the groups.
The real contribution of corticosteroids to the control of pain is not yet fully clarified. The reduction in swelling may be accompanied by a reduction in pain. However, corticosteroids alone do not seem to have a clinically significant analgesic effect.1,9,15,20 Dionne et al20 found that dexamethasone 4 mg administered intravenously and orally 1 h before and 12 h after third molar extraction, respectively, led to a reduction in the thromboxane TXB; however, the reduction in the amount of the prostaglandin PGE 2, which is the main mediator responsible for the response to peripheral pain, was not controlled properly. In the present study, the patients were instructed to use acetaminophen 500 mg three times daily in the post-operative period for 3 days and to prolong use if needed. In both protocols (dexamethasone intravenous and oral), the patients consumed approximately the same number of rescue drugs, with a mean consumption of about 9 tablets up until the third post-operative day. As reported in previous studies2,11,20,23 the number of analgesics consumed seems not to be influenced by the administration of corticosteroids.
Regarding the perception of pain, a numerical rating scale was employed in the early post-operative period. Although patients scored less pain at all post-operative evaluation times following surgeries in which dexamethasone intravenous and consumption, no statistically significant differences were found between the two routes of dexamethasone (Table 5). Based on the number of analgesic tablets consumed in the post-operative period and the self-reported pain it was concluded that no differences were found between two routes of dexamethasone.
In 2005, Tiwana et al12 reported that the administration of IV corticosteroids before third molar surgery offers a beneficial effect on health-related quality of life, we agreed with this, because having less swelling and pain the patient can return to his/her normal life.
5. Conclusion
There is evidence that there would be good control over pain swelling, and mouth opening with use of dexamethasone in either form. But we found that there is no significant difference between two doses of administration of the dosage of 4 mg of dexamethasone IV or 8 mg oral form. Patients can be administered oral form with dose of 8 mg safely and more effectively which as effective as that of IV form. It is especially useful in patients who are got more apprehension about needle prick.
Conflicts of interest
All authors have none to declare.
References
- 1.Alexander R.E., Throndoson R.R. A review of perioperative corticosteroid use in dentoalveolar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:406–415. doi: 10.1067/moe.2000.109778. [DOI] [PubMed] [Google Scholar]
- 2.Kim K., Brar P., Jakubowski J., Kaltman S., Lopez E. The use of corticosteroids and nonsteroidal anti-inflammatory medication for the management of pain and inflammation after third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:630–640. doi: 10.1016/j.tripleo.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 3.Bodnar J. Corticosteroids and oral surgery. Anesth Prog. 2001;48:130–132. [PMC free article] [PubMed] [Google Scholar]
- 4.Baxendale B.R., Vater M., Lavery K.M. Dexamethasone reduces pain and swelling following extraction of third molar teeth. Anesthesia. 1993;48:961–964. doi: 10.1111/j.1365-2044.1993.tb07474.x. [DOI] [PubMed] [Google Scholar]
- 5.Klongnoi B., Kaewpradub P., Boonsiriseth K., Wongsirichat N. Effect of single dose preoperative intramuscular dexamethasone injection on lower impacted third molar surgery. Int J Oral Maxillofac Surg. 2012;41:376–379. doi: 10.1016/j.ijom.2011.12.014. [DOI] [PubMed] [Google Scholar]
- 6.Markiewicz M.R., Brady M.F., Ding E.L., Dodson T.B. Corticosteroids reduce postoperative morbidity after third molar surgery: a systematic review and meta-analysis. J Oral Maxillofac Surg. 2008;66:1881–1894. doi: 10.1016/j.joms.2008.04.022. [DOI] [PubMed] [Google Scholar]
- 7.Hench P.S., Kendall E.C., Slocumb C.H., Polley H.F. Effects of cortisone acetate and pituitary ACTH on rheumatoid arthritis, rheumatic fever and certain other conditions. Arch Med Interna. 1950 Apr;85:545–666. doi: 10.1001/archinte.1950.00230100002001. [DOI] [PubMed] [Google Scholar]
- 8.Montgomery M.T., Hogg J.P., Roberts D.L., Redding S.W. The use of glucocorticosteroids to lessen the inflammatory sequelae following third molar surgery. J Oral Maxillofac Surg. 1990 Feb;48:179–187. doi: 10.1016/s0278-2391(10)80207-1. [DOI] [PubMed] [Google Scholar]
- 9.Beirne O.R., Hollander B. The effect of methylprednisolone on pain, trismus, and swelling after removal of third molars. Oral Surg Oral Med Oral Pathol. 1986 Feb;61:134–138. doi: 10.1016/0030-4220(86)90173-8. [DOI] [PubMed] [Google Scholar]
- 10.Esen E., Taşar F., Akhan O. Determination of the anti-inflammatory effects of methylprednisolone on pain, swelling, trismus after third molar surgery. J Oral Maxillofac Surg. 1999;57:1201–1206. doi: 10.1016/s0278-2391(99)90486-x. [DOI] [PubMed] [Google Scholar]
- 11.Ustin Y., Erdogan O., Esen E., Karsli E.D. Comparison of the effects of 2 doses of methylprednisolone sodium succinate to reduce postoperative edema after removal of impacted third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:535–539. doi: 10.1016/S1079210403004645. [DOI] [PubMed] [Google Scholar]
- 12.Pell G.J., Gregory B.T. Impacted mandibular third molars: classification and modified techniques for removal. Dent Dig. 1933;39:330–338. [Google Scholar]
- 13.Boonsiriseth K., Klongnoi B., Sirintawt N., Saengsirinavin C., Wongsirichat N. Comparative study of the effect of dexamethasone injection and consumption in lower third molar surgery. Int J Oral Maxillofac Surg. 2012 Feb;41:244–247. doi: 10.1016/j.ijom.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 14.Graziani F., D'Aiuto F., Arduino P.G., Tonelli M., Gabriele M. Perioperative dexamethasone reduces post-surgical sequelae of wisdom tooth removal. A spilt-mouth randomized double-masked clinical trial. Int J Oral Maxillofac Surg. 2006;35:241–246. doi: 10.1016/j.ijom.2005.07.010. [DOI] [PubMed] [Google Scholar]
- 15.Grossi G.B., Maiorana C., Garramone R.A. Effect of submucosal injection of dexamethasone on postoperative discomfort after third molar surgery. A prospective study. J Oral Maxillofac Surg. 2007;65:2218–2226. doi: 10.1016/j.joms.2006.11.036. [DOI] [PubMed] [Google Scholar]
- 16.Laureano Filho J.R., Maurette P.E., Allais M., Cotinho M., Fernandes C. Clinical comparative study of the effectiveness of two dosages of dexamethasone to control postoperative swelling, trismus and pain after the surgical extraction of mandibular impacted third molars. Med Oral Pathol Oral Cir Buccal. 2008;96:535–539. [PubMed] [Google Scholar]
- 17.Tiwana P.S., Foy S.P., Shugars D.A. The impact of intravenous corticosteroids with third molar surgery in patients at high risk for delayed health-related quality of life and clinical recovery. J Oral Maxillofac Surg. 2005 Jan;63:55–62. doi: 10.1016/j.joms.2004.01.029. [DOI] [PubMed] [Google Scholar]
- 18.Garcia A.G., Sampedro F.G., Rey J.G., Vila P.G., Martin M.S. Pell-Gregory classification is unreliable as a predictor of difficulty in extracting impacted lower third molars. Br J Oral Maxillofac Surg. 2000;38:585–587. doi: 10.1054/bjom.2000.0535. [DOI] [PubMed] [Google Scholar]
- 19.Neupert E.A., 3rd, Lee J.W., Philput C.B., Gordon J.R. Evaluation of dexamethasone for reduction of postsurgical sequelae of third molar removal. J Oral Maxillofac Surg. 1992 Nov;50:1177–1182. doi: 10.1016/0278-2391(92)90149-t. [DOI] [PubMed] [Google Scholar]
- 20.Dionne R.A., Gordon S.M., Rowan J., Kent A., Brahim J.S. Dexamethasone suppresses peripheral prostanoid levels without analgesia in a clinical model of acute inflammation. J Oral Maxillofac Surg. 2003 Sep;61:997–1003. doi: 10.1016/s0278-2391(03)00310-0. [DOI] [PubMed] [Google Scholar]
- 21.Markovic A., Todorovic L.J. Effectiveness of dexamethasone and low-power laser in minimizing oedema after third molar surgery: a clinical trial. Int J Oral Maxillofac Surg. 2007;36:226–229. doi: 10.1016/j.ijom.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 22.Shugars D.A., Gentile M.A., Ahmad N. Assessment of oral health-related quality of life before and after third molar surgery. J Oral Maxillofac Surg. 2006;64:1721–1730. doi: 10.1016/j.joms.2006.03.052. [DOI] [PubMed] [Google Scholar]
- 23.Alcantara C.E.P., Falci S.G.M., Oliveira-Ferreira F., Santos C.R.R., Pinheiro M.L.P. Pre-emptive effect of dexamethasone and methylprednisolone on pain, swelling, and trismus after third molar surgery: a split-mouth randomized triple –blind clinical trial. Int J Oral Maxillofac Surg. 2014;43:93–98. doi: 10.1016/j.ijom.2013.05.016. [DOI] [PubMed] [Google Scholar]


