1. Introduction
Transeptal access is an integral skill for interventional cardiologists for a multitude of cardiac interventions including, balloon mitral valvotomy a commonly performed procedure in India and south Asia. The procedure was first performed by Braunwald, Ross and Morrow and later refined by Brockenbrough and Mullins, whose names have been intricately linked with this procedure.1–3 The procedure, however, evokes considerable trepidation in many young interventionalists due its steep learning curve and potential catastrophic complications. However, the procedure is relatively simple in most patients, barring patients with extremely distorted anatomy like aneursymally dilated left/right atria where the anatomy of the interatrial septum is often grossly altered.
2. Equipment
The usual equipment required for transeptal access is a pre-shaped transeptal sheath with introducer and a pre-shaped transeptal needle. These sheaths and needles are available in both adult and pediatric sizes. The Mullins sheath is the most commonly used sheath for transeptal access (Fig. 1a). This is an 8 French 60 cm sheath that can be introduced over a 0.032 J-tipped guidewire. The needle most often used for atrial septal puncture is the stainless steel Brokenbrough needle (Medtronic Inc) (Fig. 1b). The needle is a hollow tube which is 18 gauge tapering to 21 gauge. The proximal end has a flange with an arrow that points towards the needle tip. The other needles available are the BRK, BRK-1, BRK-2 and BRK-XS needles which are marketed by St Judes Medical. The BRK is the standard needle with slight angulation between the tip and the shaft (19°) and is used for routine septal puncture. The BRK-1 needle has a greater angulation between the shaft and the tip (53°) and is preferred in cases with a very large right atrium. The larger angulation helps in sitting better on the septal wall. The needle is available in two lengths (71 or 89 cm).
Fig. 1.

a: Mullins sheath with dilator. b: Transeptal needles: The needle on the left is the Brockenbrough needle. The one in the middle is BRK needle from St Jude Medical while the needle on the right is the BRK1 needle.
3. Procedural technique
Following venous and arterial access from the right groin, the Mullins sheath is advanced over a 0.032″ Terumo guide wire into the superior vena cava. A pigtail catheter is placed in the aortic root in the non-coronary cusp which is the lower most part of the aortic root (Table 1). The Brockenbrough needle is then advanced into the Mullins sheath about 2–3 cms short of the tip (Fig. 2; Video 1). It is useful to keep a finger between the base of the Brockenbrough needle and the hub of the Mullins sheath to prevent inadvertent advancement of the needle (Fig. 3). While most operators attach a 2 or 5 ml syringe, preferably with a Luer lock, it is also possible to attach the needle to a pressure transducer. Care is taken that the patient is supine without any rotation of the spine because this distorts the orientation of the atrial septum.
Table 1.
Step by step guide to septal puncture.
| Step 1: Mullins sheath with Brockenbrough needle positioned in SVC. Pigtail catheter positioned in aorta at the level of the aortic valve |
| Step 2: Mullins sheath with needle withdrawn into the right atrium to lie 1–3 cm (half to one vertebra) below the level of the aortic catheter in the AP projection. |
| Step 3: Brockenbrough needle rotated to 4–5 o'clock position. Optimal position confirmed in AP, RAO and lateral/LAO projection. |
| Step 4: Left atrial entry by probing at fossa ovalis site or septal puncture performed by protruding the Brockenbrough needle through the Mullins sheath. Left atrial access confirmed by contrast injection and pressure monitoring. |
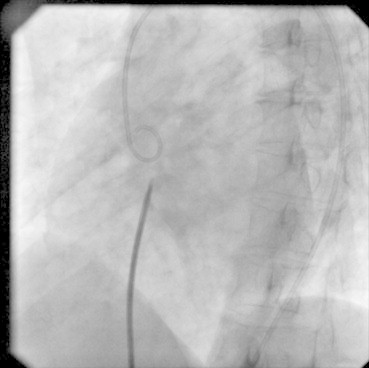
Fig. 2.

AP fluoroscopic view with a Mullins sheath and Brockenbrough needle in the SVC. Pigtail catheter is placed in the aorta with the loop of the pigtail resting in the non-coronary cusp.
Fig. 3.

Brockenbrough needle inserted into the Mullins sheath with the needle flange pointing at 3 o' clock position.
Supplementary video related to this article can be found at http://dx.doi.org/10.1016/j.ihj.2015.02.024.
The following is the supplementary video related to this article:
AP fluoroscopic view with a Mullins sheath and Brockenbrough needle in the SVC. Pigtail catheter is placed in the aorta with the loop of the pigtail resting in the non-coronary cusp.
The entire assembly of the Mullins sheath with the needle is then gradually withdrawn in the AP projection on fluoroscopy into the right atrium, taking care that the Brockenbrough needle points at 3 o' clock position. The assembly first descends from the superior vena cava into the right atrium and then along the thick part of the interatrial septum. The entire assembly is withdrawn slowly in one smooth maneuver until it reaches the level of the aortic valve (Fig. 4; Video 2). During this entire maneuver, care is taken that needle continues to point at 3 o' clock position. Then it is gradually withdrawn further below the level of the aortic valve, usually by 1–3 cms (half to one vertebral space), to lie along the interatrial septum at the expected position of the fossa ovalis (Fig. 5; Video 3). The needle is then rotated in a clockwise manner to around 4–5 o' clock position. At this point one can generally feel good transmitted pulsations on the entire assembly.
Fig. 4.
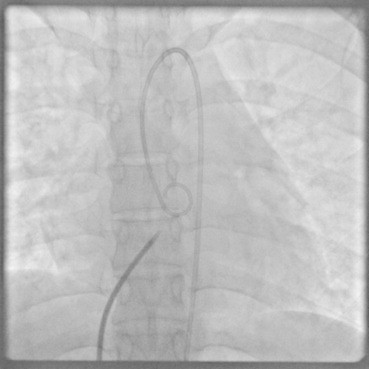
AP fluoroscopic view with the Mullins sheath and Brockenbrough needle now at the level of the aortic valve.
Fig. 5.
AP fluoroscopic view with the Mullins sheath and Brockenbrough needle positioned at the expected area of the fossa ovalis.
Supplementary video related to this article can be found at http://dx.doi.org/10.1016/j.ihj.2015.02.024.
The following are the supplementary video related to this article:
AP fluoroscopic view with the Mullins sheath and Brockenbrough needle now at the level of the aortic valve.
AP fluoroscopic view with the Mullins sheath and Brockenbrough needle positioned at the expected area of the fossa ovalis.
The position of the needle is then confirmed in at least two additional views – RAO and dead lateral. In 30° RAO the interatrial septum is generally seen en face. Therefore, the needle should look away from the operator (Fig. 6; Video 4) and not point to the left (posterior) or right (anterior). Additionally, it should be confirmed that the needle is lying posterior and inferior to the plane of the aorta. In the lateral view the needle should be facing posteriorly towards the spine (Fig. 7; Video 5) and should be between halfway from pigtail to spine to two-thirds between pigtail and spine. The needle should not be too low or else it may enter the coronary sinus. The position of the needle needs to be confirmed in all three views for a safe and optimal septal puncture. It is very important to recheck the position in other orthogonal views if the needle is manipulated in one view. When all the above criteria are met, gentle probing in this area may often permit left atrial entry through the stretched fossa ovalis without an actual need for needle puncture.
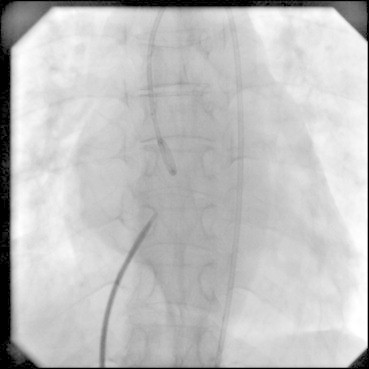
Fig. 6.

RAO projection with the Mullins sheath and Brockenbrough needle at the expected area of fossa ovalis. Note that the tip of the needle looks away from the operator.
Fig. 7.
Lateral projection at the same position as in Figs. 5 and 6. The needle looks posteriorly towards the spine.
Supplementary video related to this article can be found at http://dx.doi.org/10.1016/j.ihj.2015.02.024.
The following are the supplementary video related to this article:
RAO projection with the Mullins sheath and Brockenbrough needle at the expected area of fossa ovalis. Note that the tip of the needle looks away from the operator.
Lateral projection at the same position as in Figs. 5 and 6. The needle looks posteriorly towards the spine.
Once the septum is punctured, blood is gently aspirated followed by a small contrast injection to confirm left atrial opacification (Fig. 8; Videos 6, 7). This is further confirmed by measuring left atrial pressures and waveforms. If the needle is attached to a pressure transducer, then a flat line, which is observed when the needle abuts the atrial septum, gives way to a left atrial pressure trace (Fig. 9). The Mullins sheath is finally advanced into the left atrium over which subsequent catheter exchanges can be performed.
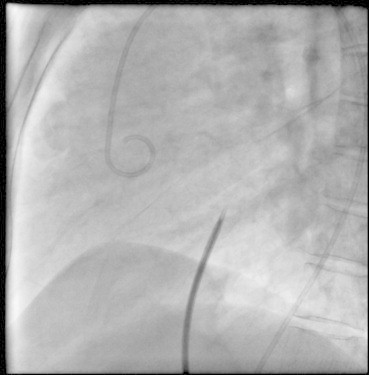
Fig. 8.

Radiographic contrast injection in the left atrium through the Mullins sheath.
Fig. 9.
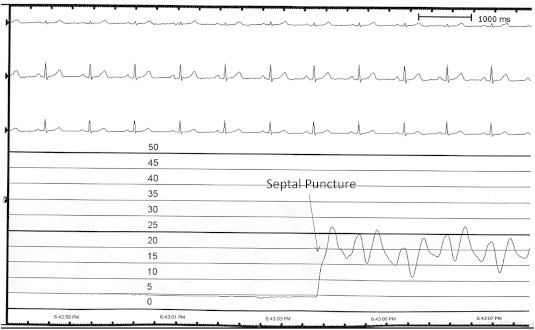
Hemodynamic trace obtained from the Mullins sheath at the fossa ovalis. The pressure recording is at 25 mm paper speed and on a 0–50 mmHg scale with each line representing 5 mmHg. The patient is in sinus rhythm. When the Mullins sheath reaches the fossa ovalis the pressure trace becomes a straight line as it abuts the septum. Once the septal puncture is performed the pressure trace and waveform of the left atrium is seen.
Supplementary video related to this article can be found at http://dx.doi.org/10.1016/j.ihj.2015.02.024.
The following are the supplementary video related to this article:
Septal puncture in lateral view.
Radiographic contrast injection in the left atrium through the Mullins sheath.
4. Variations in technique
While the above steps work in most cases, variations in anatomy require small modifications. The most frequently encountered problem is with giant left atria. In such circumstances, the left atrium hugs the borders of the heart and the position of the fossa ovalis is shifted more inferiorly. Therefore, when the needle is withdrawn into the right atrium from the SVC, it often hugs the lateral border of right atrium before it reaches the horizontal level of the aortic valve. The needle then needs to be much withdrawn further to reach the fossa ovalis. To maintain contact with the atrial septum the needle may require to be rotated even further to 6 o' clock position. It is often during this step that one may lose contact with septum and slip into the anterior or posterior atrial recesses. Inadvertent puncture in these areas can lead to cardiac tamponade. In difficult cases, one may need to increase the curvature of the Brockenbrough needle to retain contact with the septum or use BRK 1 needle.
Increasing confidence and competence in septal puncture has made use of cardiac imaging largely redundant in centers that perform these procedures in large volumes. Intra-cardiac echo could possibly guide septal puncture in aneursymal left atria. In difficult cases, a cheaper alternative of levo phase pulmonary angiography can demonstrate the left atrium.4
Many operators prefer to perform septal puncture in the LAO view. In this view the interatrial septum is profiled end-on and therefore differentiates the left and the right atria. However, the aorta overlaps the interatrial septum in this view (Fig. 10; Video 7). This must there be complimented with the RAO view to confirm posterior location of the needle.
Fig. 10.
LAO fluoroscopic view with the needle in the same position as in Figs. 5–7. Note the slight overlap of the Brockenbrough needle with the pigtail catheter in the aorta.
Rarely, a persistent left SVC may enlarge the coronary sinus pushing the atrial septum upwards. In such cases it is useful to delineate the margins of the coronary sinus with a contrast injection prior to septal puncture. Some operators like to keep a catheter in the CS to mark the posterior border of the left atrium.
Additional variations in the venous anatomy may pose challenges such as right femoral vein/common iliac vein occlusion or inferior vena cava occlusion. Sepal puncture from the left groin is generally not very different from the right though addition of a larger curve to Brockenbrough needle may ease the procedure in some patients. Though the jugular approach uses the same landmarks, the operator should be sufficiently skilled to correct for the spatial changes vis a vis the groin approach.
Electrophysiologists who perform atrial septal puncture for radiofrequency ablation of atrial fibrillation generally prefer not to take arterial access since prolonged procedure time and continuous anticoagulation with heparin during the procedure leads to an increased incidence of groin hematomas. The coronary sinus serves as a useful landmark for septal puncture in these cases (Fig. 11a and b; Video 8). In the RAO projection, the needle should point posterior to the coronary sinus os while in the lateral and LAO view the needle should not be posterior to the coronary sinus catheter (Figs. 12, 13a and b; Videos 9 and 10). A catheter at the His bundle location can substitute as a anatomical landmark for the pigtail catheter at the level of the aortic valve to guide septal puncture. Electrophysiology procedures for atrial fibrillations require two sheaths in the left atrium. Instead of puncturing the septum a second time, most electrophysiologists simply probe the interatrial septum near the previous puncture site with the second long sheath (with the dilator) with a 0.032″ ordinary guide wire. In most instances, the guidewire can slip in by the side of the previous puncture.
Fig. 11.

a and b, AP and RAO fluoroscopic projection with a decapolar catheter positioned in the coronary sinus and the Mullins sheath with Brockenbrough needle at the fossa ovalis. Note that the needle is posterior to the os of the coronary sinus in the RAO view.
Fig. 12.
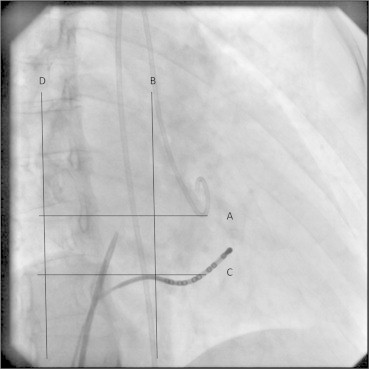
RAO projection in a patient who underwent concomitant mitral valvuloplasty and ablation of a left free wall pathway. Pigtail catheter in the aorta, decapolar catheter in the coronary sinus and Brocekenbrough needle at fossa ovalis. The needle lies approximately a centimeter below the aortic valve (line A) and posterior to both the aorta and the coronary sinus os (line B), which mark the anterior boundary of the interatrial septum. The puncture needle should not dip below coronary sinus os which also marks the anteroinferior margin of the interatrial septum (line C). The posterior margin of the left atrium is visible on the RAO projection (line D) though this overlaps with the pulmonary vein antrum and the right atrium. Septal puncture is best performed in the center of this “box” that is so formed. Entry into the left ventricle (LV) is most easily achieved if the entry is made in between lines B and D. The closer the needle is to line B, the puncture becomes more anterior and closer to the mitral annulus. This may impede easy LV entry; in difficult cases, a retro loop along the posterior wall of LA may facilitate LV entry. A high and anterior puncture risks entry into the aorta which may be catastrophic. A very posterior puncture is associated with the risk of pericardial tamponade; in some cases although the needle may enter the left atrium, it may have “stitched” the posterior walls of the right atrium and left atrium.
Fig. 13.
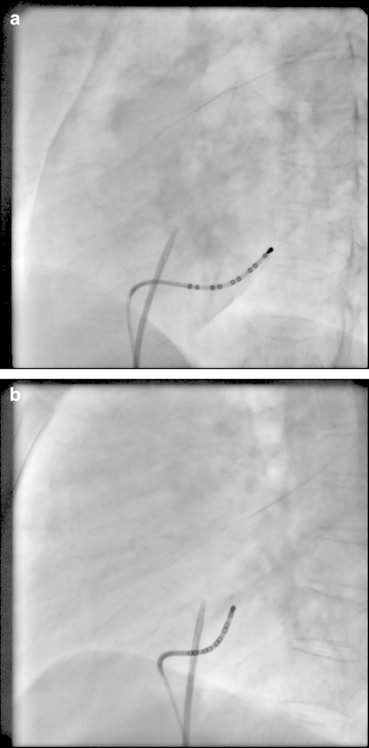
a and b, LAO and lateral fluoroscopic projections with the needle in the same position as Fig. 9.
Supplementary video related to this article can be found at http://dx.doi.org/10.1016/j.ihj.2015.02.024.
The following are the supplementary data related to this article:
LAO fluoroscopic view with the needle in the same position as in Figs. 5–7. Note the slight overlap of the Brockenbrough needle with the pigtail catheter in the aorta.
AP and RAO fluoroscopic projection with a decapolar catheter positioned in the coronary sinus and the Mullins sheath with Brockenbrough needle at the fossa ovalis. Note that the needle is posterior to the os of the coronary sinus in the RAO view.
AP and RAO fluoroscopic projection with a decapolar catheter positioned in the coronary sinus and the Mullins sheath with Brockenbrough needle at the fossa ovalis. Note that the needle is posterior to the os of the coronary sinus in the RAO view.
LAO and lateral fluoroscopic projections with the needle in the same position as Fig. 9.
LAO and lateral fluoroscopic projections with the needle in the same position as Fig. 9.
5. Complications
Major complications are encountered in <1% of transeptal procedures. Pericardial tamponade is the most frequent complication. Most commonly this results from punctures being attempted from non-standard sites. Careful attention to the procedure, confirming the puncture site in all three views can prevent this complication. Posterior punctures, including puncture of the pulmonary vein can lead to hemothorax. Other complications such as aortic puncture, systemic embolism, septal dissection and even death have also been reported.
6. Conclusions
Atrial septal puncture is a critical skill for interventional cardiologists in countries overwhelmed with rheumatic mitral stenosis. With the rapid growth in radiofrequency ablation for atrial fibrillation, there has been resurgence in interest even in the developed world. In experienced hands this is a safe procedure when done with due deligence even in the most demanding circumstances.
Conflicts of interest
The author has none to declare.
References
- 1.Ross J., Jr., Braunwald E., Morrow A.G. Left heart catheterization by the transeptal route: a description of the technique and its applications. Circulation. 1960;22:927–934. [Google Scholar]
- 2.Brockenbrough E.C., Braunwald E., Ross J., Jr. Transseptal left heart catheterization. A review of 450 studies and description of an improved technic. Circulation. 1962;25:15–21. doi: 10.1161/01.cir.25.1.15. [DOI] [PubMed] [Google Scholar]
- 3.Mullins C.E. Transseptal left heart catheterization: experience with a new technique in 520 pediatric and adult patients. Pediatr Cardiol. 1983;4:239–245. doi: 10.1007/BF02242264. [DOI] [PubMed] [Google Scholar]
- 4.Hung J.S. Atrial septal puncture technique in percutaneous transvenous mitral commissurotomy : mitral valvuloplasty using the lnoue balloon catheter technique. Cathet Cardiovasc Diagn. 1992;26:275–284. doi: 10.1002/ccd.1810260407. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
AP fluoroscopic view with a Mullins sheath and Brockenbrough needle in the SVC. Pigtail catheter is placed in the aorta with the loop of the pigtail resting in the non-coronary cusp.
AP fluoroscopic view with the Mullins sheath and Brockenbrough needle now at the level of the aortic valve.
AP fluoroscopic view with the Mullins sheath and Brockenbrough needle positioned at the expected area of the fossa ovalis.
RAO projection with the Mullins sheath and Brockenbrough needle at the expected area of fossa ovalis. Note that the tip of the needle looks away from the operator.
Lateral projection at the same position as in Figs. 5 and 6. The needle looks posteriorly towards the spine.
Septal puncture in lateral view.
Radiographic contrast injection in the left atrium through the Mullins sheath.
LAO fluoroscopic view with the needle in the same position as in Figs. 5–7. Note the slight overlap of the Brockenbrough needle with the pigtail catheter in the aorta.
AP and RAO fluoroscopic projection with a decapolar catheter positioned in the coronary sinus and the Mullins sheath with Brockenbrough needle at the fossa ovalis. Note that the needle is posterior to the os of the coronary sinus in the RAO view.
AP and RAO fluoroscopic projection with a decapolar catheter positioned in the coronary sinus and the Mullins sheath with Brockenbrough needle at the fossa ovalis. Note that the needle is posterior to the os of the coronary sinus in the RAO view.
LAO and lateral fluoroscopic projections with the needle in the same position as Fig. 9.
LAO and lateral fluoroscopic projections with the needle in the same position as Fig. 9.


