Abstract
Background:
Childhood obesity has increased over the past two decades. Child obesity is likely to persist through adulthood and increases the risk of non-communicable diseases (NCDs) later in life. This study assessed knowledge and attitudes towards obesity among primary school children in Dar es Salaam, Tanzania.
Materials and Methods:
A cross-sectional study was conducted in randomly selected primary schools in Dar es Salaam. A structured questionnaire was used to assess the knowledge and attitudes. Anthropometric and blood pressure measurements were taken using standard procedures.
Results:
A total of 446 children were included in the analysis. The mean age of the participants was 11.1 ± 2.0 years. The mean body mass index (BMI), systolic blood pressure (SBP) and diastolic blood pressure (DBP) were 16.6 ± 4.0 kg/m2, 103.9 ± 10.3 mmHg and 65.6 ± 8.2 mmHg, respectively. Prevalence of obesity (defined as BMI >95th percentile for age and sex) was 5.2%. Half of the children (51.1%) had heard about obesity from teachers at school (20%), radio (19.4%) and books/newspaper (17.3%). Less than half (45.4%) had knowledge about the risk factors for childhood obesity and correctly defined obesity (44.6%). However, a good number of the children (72.1%) were aware that they can be affected by obesity. Majority of them had negative attitude towards obesity and various factors leading to or resulting from childhood obesity.
Conclusions:
Knowledge about childhood obesity among primary school children is moderate and have negative attitude towards obesity. Integrating educational programs early in primary schools may be an effective strategy to impact knowledge about obesity and other non-communicable diseases early in childhood.
Keywords: Attitudes, knowledge, obesity, primary school children, Tanzania
INTRODUCTION
Childhood obesity has been increasing over the past few decades and has become a public health concern in both developed and developing countries.1 Global estimates indicate that 43 million children were overweight and obese in the year 2010.2 More than one-fifth of overweight and obese children were from developing countries. Globally, the prevalence of overweight is expected to increase from 6.7% in 2010 to more than 9% in 2020 compared to the increase from 8.5% to 12.7% in Africa within the same span of time.2
There is limited data on childhood obesity in Tanzania.3,4 Mosha et al., reported the prevalence obesity of 5.6% and 6.3% among children aged 6-9 years in Dodoma and Dar es Salaam, respectively.4 Another study reported a prevalence of 5.3% from Dar es Salaam and Morogoro among children aged 6-15 years.3 However, none of these studies assessed knowledge or attitudes towards obesity among primary school children.
Many of the conducted studies have concentrated on knowledge, attitudes and perception of parents5,6,7 and healthcare workers8,9,10 about childhood obesity. There is minimal investigation of knowledge and attitudes towards obesity among school age children themselves.11,12 Understanding school children's knowledge, perception and attitudes towards childhood obesity may be the cornerstone to the success of preventive programs for childhood obesity.
Changes in the dietary habits from consumption of traditional foods to intakes of high energy but low nutrient dense foods, frequent snacking and outdoor food consumption coupled with a more sedentary lifestyle are implicated in fueling the increasing problem of childhood obesity.13 Childhood obesity may result from a complex interaction of genetic, social and environmental factors that may influence eating and physical activity behaviour.14,15
The increasing body of literature supporting that childhood obesity persists through adult life,16 makes it very imperative to study and understand factors associated with childhood obesity including knowledge and attitudes of children themselves towards obesity. This study assessed the knowledge and attitudes towards obesity among primary school children in Dar es Salaam, Tanzania
MATERIALS AND METHODS
This cross-sectional study was conducted among primary school children aged 6-17 years from nine primary schools in Dar es Salaam. Primary schools were randomly selected and included in the study while insuring equal representation of both public and private primary schools from both urban and rural settings of Dar es Salaam. Study questionnaires with both closed and open-ended questions were used to gather the required information from the participants.
Data collection procedures have already been described elsewhere.17 Briefly, data were collected through a structured interview using questionnaire. Collected information included sociodemographic characteristics of the family, knowledge about obesity and its risk factors, prevention of obesity as well as attitude towards obesity. Children were asked if they had ever heard about obesity and if they could correctly define obesity. Knowledge about risk factors for obesity included; low birth weight, obese parents, less sleeping time, consumption of sweets and soft drinks, watching TV/internet/video games, pocket money, high income of parents, eating out of home, using car to go to school.
Anthropometric measurements were conducted by trained research assistants while observing standard precautions.18 Body weight was measured using a self-calibrating precision digital scale (Omron, Japan) and height to the nearest 0.1 cm by a fixed Shorr measuring board (Shorr Productions, Olner, MD). Body Mass Index (BMI) was calculated as weight divided by height squared (kg/m2). Prevalence of obesity was defined using BMI percentiles for age and sex. Children with BMI ≥ 95th percentile for age and sex were considered obese and those with BMI between 85th and 95th percentile were classified as overweight.19,20
A standardised digital blood pressure measuring machine (Omron Digital HEM-907, Tokyo, Japan) was used to measure blood pressure in this population of primary school children. Blood pressure was measured on the left upper arm and in a seated position following at least 5-10 minutes of rest. An average of the three readings was used during analysis.
Descriptive statistics (means, standard deviations and frequencies) were used to describe the general characteristics of the participants. Prevalence of obesity by sociodemographic characteristics was assessed using chi-square (X2) test. Statistical analyses were performed using Statistical Package for Social Sciences (SPSS 15.0). In all analyses, two sided P ≤ 0.05 was considered statistically significant.
The study was approved by the Research Ethics Review Committee of Muhimbili University of Health and Allied Sciences. An informed consent to participate into the study was obtained from the parents/guardians of the selected children prior to the study.
RESULTS
Sociodemographic characteristics of the study population are presented in [Table 1]. About 53.14% (n = 237) of the total of 446 studied children were girls. The mean age of the children was 11.1 ± 2.0 years (11.3 ± 2.1 for boys and 11.1 ± 2.0 for girls). The mean BMI for girls (17.0 ± 4.0 kg/m2) was higher than that of boys (17.0 ± 4.0 kg/m2), and this difference was statistically significant (P = 0.002). Level of education of the mother was also difference for boys and girls (P = 0.014).
Table 1.
Sociodemographic characteristic of primary school children participating in the study
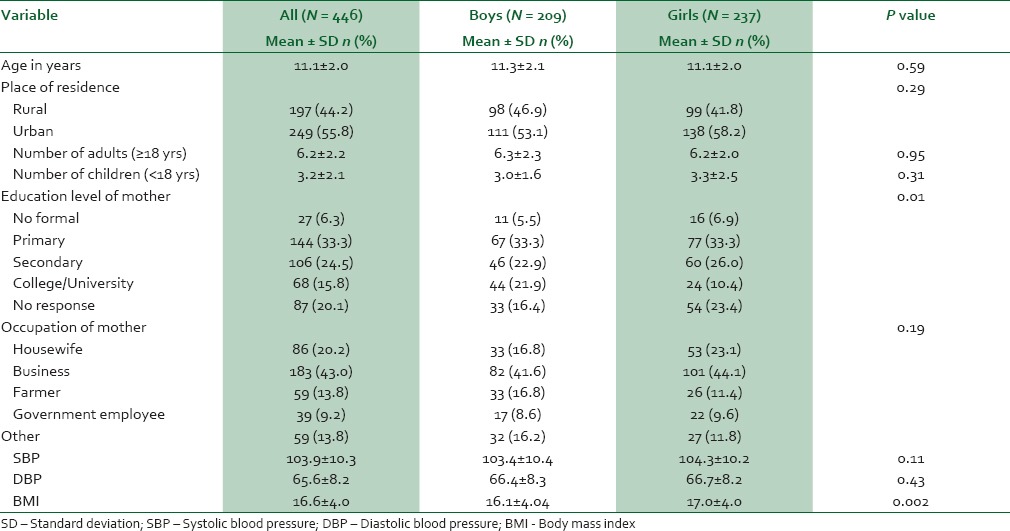
The overall prevalence of obesity in this population of school age children was 5.2%. Girls had higher prevalence (6.3%) compared to boys (3.8%). A similar trend was also observed for overweight. Prevalence of overweight was 13.1% for girls and 6.3% for boys. There was a statistically significant gender difference in the distribution of BMI in the population (P = 0.003). The level of knowledge and source of information regarding obesity are summarized in [Table 2]. More than half (51.1%) of the children had heard about obesity. Obese children had heard more about obesity than non-obese children (77.3% vs 47.0%) and this difference was statistically significant (P = 0.01). Source of information about obesity was mainly school teachers (20.3%), followed by radio (19.4%), books and newspapers (17.3%) and relatives/neighbours/friends (16.4%). Less than half of the children (44.6%) were able to correctly define obesity, 7.4% had moderate knowledge and 37.0% had poor or no knowledge about obesity. However, a good number of children (72.1%) were aware that they can be affected by obesity.
Table 2.
Knowledge and source of information about obesity to primary school children
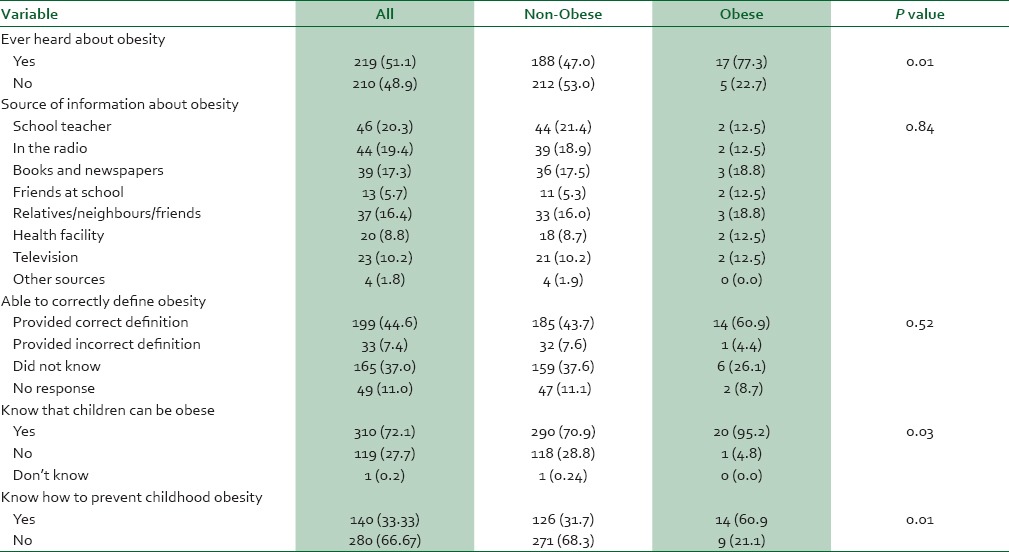
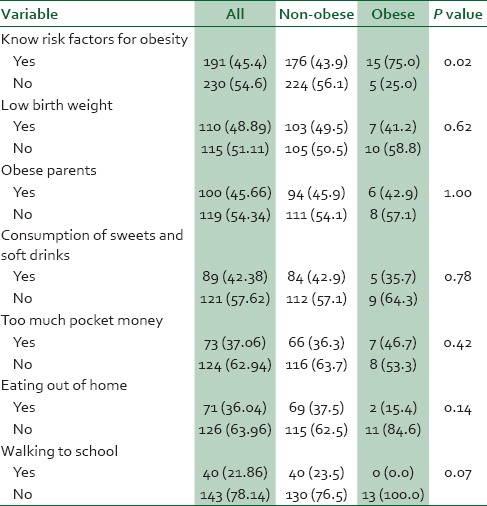
With regard to knowledge about risk factors for obesity [Table 3], less than half of the children (45.4%) had knowledge about the risk factors. Obese children had significantly higher knowledge about risk factors for obesity compared with non-obese children (75.0% vs 43.9%, and this difference in knowledge between obese and non-obese children about obesity risk factors was statistically significant (P = 0.02). With regard to prevention, only one-third were aware of the ways to prevent childhood obesity. Obese children seemed to know more than non-obese children (60.9% vs 31.7%).
Table 3.
Knowledge about risk factors for childhood obesity among primary school children
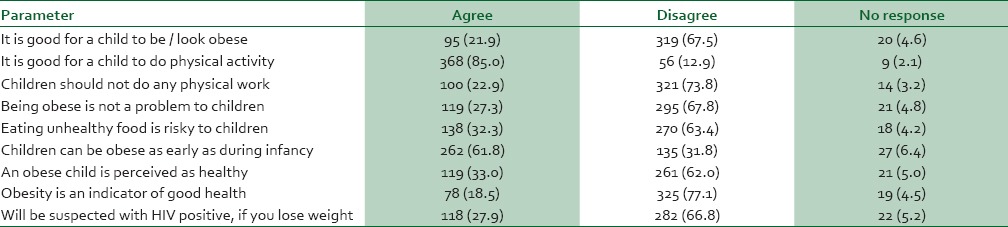
Most children had correct attitudes towards obesity during childhood [Table 4]. More than two-thirds (67.5%) of the children disagreed with a statement that “it is good for a child to be/look obese. Majority (85.0%) of the children agreed that children should do physical activities and (77.1%) disagreed with a statement that obesity is an indicator of good health.
Table 4.
Attitudes of primary school children towards obesity
DISCUSSION
The present study assessed the knowledge and attitudes towards obesity in a representative sample of primary school children in Dar es Salaam. The findings have shown that primary school children have good knowledge about obesity. The study has further revealed that this population of primary school children have appropriate/negative attitude towards obesity.
The prevalence of obesity in this population of primary school children was 5.2%, which is similar to reports from other studies conducted elsewhere in Tanzania,3,4 and low compared to prevalence reported from other parts.21,22,23 Despite the fact that prevalence of obesity in this population of primary school is low, overall, childhood obesity has increased dramatically since 1990s. In the US, prevalence of obesity among children aged 2-4 years increased from 13.05% in 1998 to 14.94% in 2010, while that of extreme obesity increased from 1.75% to 2.07% during the same time period.24 The recent global analysis of prevalence and trends of child overweight and obesity has shown that out of the 43 million children estimated to be overweight and obese, 35 million were from developing countries. The same analysis has shown that the worldwide prevalence of childhood overweight and obesity increased from 4.2% in 1990 to 6.7% in 2010 and is expected to reach 9.1% by 2020.25
Childhood obesity is determined by both genetic and environmental factors.26,27,28 With a dramatic increase in childhood overweight and obesity, knowledge and attitudes of the children themselves towards childhood obesity need to be placed on the frontline. Most studies have focussed on knowledge and perception of parents/caregivers,5,6,7 and health care professional9,10,29,30 about child obesity. The present study is among few that have focussed on assessment of knowledge about child obesity and perceptions about body weight among children.12,31,32,33 Findings of the present study have shown that half (51.1%) of the primary school children had heard about obesity with 44.6% having a good knowledge about obesity. Regardless of the difference in methodological approaches, the level of knowledge shown by children in this study is higher compared to that reported from a study conducted among adolescents in preparatory schools in Ismailia, Egypt, which reported that only 12.3% of the participants had good knowledge about child obesity and risk factors.25
In this study, obese children reported to have heard more about obesity, had higher knowledge about obesity and knew more about prevention of obesity than non-obese children. Another study conducted among children in southern Brazil found that obese children had higher knowledge in nutrition compared to the non-obese classmates.11 The explanation for such findings was that because of their condition, obese children are more likely to be interested and hence receive/seek information regarding obesity. Other studies, however, have not found any significant differences in the level of knowledge about nutrition between obese and non-obese children.34,35
Another interesting finding from our study was the appropriate attitudes of the study participants towards obesity. Majority of the children (77.1%) disagreed with a statement that “obesity is an indicator of good health”. Likewise, more than two-thirds (67.8%) of the children disagreed with a statement that “being obese is not a problem to a child”. Due to human immunodeficiency virus (HIV) pandemic, many people prefer to be obese or overweight so as not to look suspicious of having HIV/acquired immunodeficiency syndrome (AIDS). Two-thirds of the children in this study did not agree with a statement that “you will be suspected as being HIV positive if you lose weight”. Generally, children in this study had appropriate attitudes towards obesity. Other studies have also reported negative attitudes towards obesity among children.36,37 In a systematic review of the views of young children in the UK about obesity, body size, shape and weight, children expressed among other things that being overweight is seen as a social problem, where desirable bodies are not overweight and that overweight children are made to feel different and terrible.37
The main strengths of this study include anthropometric measurements (weight and height) that were measured as opposed to other studies which use self-reported weight and height and the use of a relatively easy to administer and understand questionnaire to collect the required information from children. The main limitation of this study is that sampled children were from Dar es Salaam region only; hence, these findings may not be generalisable to broader Tanzania. Also certain aspects to measure knowledge about obesity in children may have been missed.
CONCLUSION
To our knowledge, this is the first study to assessed knowledge and attitudes about obesity in a representative sample of primary school children in Tanzania. Our results have clearly indicated that children have good knowledge about obesity and negative attitudes towards obesity. These findings have significant implications in the prevention of obesity in Tanzania. It has been shown that obesity can start as early as in the first half of infancy.38,39 Thus, infancy and pre-school periods have been proposed to be the most critical periods for long term interventions to prevent obesity.40,41 Despite the fact that obesity in this population is low and that children have negative attitudes towards obesity, necessary measures need to be taken to maintain this low level of obesity.
ACKNOWLEDGEMENT
We acknowledge the parents who consented for their children participate in this study and head teachers of the primary schools where this study was conducted for their unlimited support during data collection.
Footnotes
Source of Support: Financial support to conduct the study was received from Muhimbili University of Health and Allied Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Karnik S, Kanekar A. Childhood obesity: A global public health crisis. Int J Prev Med. 2012;3:1–7. [PMC free article] [PubMed] [Google Scholar]
- 2.de Onis M, Blössner M. Prevalence and trends of overweight among preschool children in developing countries. Am J Clin Nutr. 2000;72:1032–9. doi: 10.1093/ajcn/72.4.1032. [DOI] [PubMed] [Google Scholar]
- 3.Chillo P, Lwakatare J, Janabi M, Matuja W, Greve G. Low prevalence of cardiovascular disease risk factors among primary school children in Tanzania: An opportunity for primordial prevention? Tanzania Med J. 2009;24:9–14. [Google Scholar]
- 4.Mosha TC, Fungo S. Prevalence of overweight and obesity among children aged 6-12 years in Dodoma and Kinondoni municipalities, Tanzania. Tanzan J Health Res. 2010;12:6–16. doi: 10.4314/thrb.v12i1.56202. [DOI] [PubMed] [Google Scholar]
- 5.Wan AM, Norazawati AK, Lee YY. Overweight and obesity among malay primary school children in Kota Bharu, Kelantan: Parental beliefs, attitudes and child feeding practices. Malays J Nutr. 2012;18:27–36. [PubMed] [Google Scholar]
- 6.Redsell SA, Atkinson P, Nathan D, Siriwardena AN, Swift JA, Glazebrook C. Parents’ beliefs about appropriate infant size, growth and feeding behaviour: Implications for the prevention of childhood obesity. BMC Public Health. 2010;10:711. doi: 10.1186/1471-2458-10-711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sealy YM. Parents’ perceptions of food availability: Implications for childhood obesity. Soc Work Health Care. 2010;49:565–80. doi: 10.1080/00981381003635353. [DOI] [PubMed] [Google Scholar]
- 8.Larsen L, Mandleco B, Williams M, Tiedeman M. Childhood obesity: Prevention practices of nurse practitioners. J Am Acad Nurse Pract. 2006;18:70–9. doi: 10.1111/j.1745-7599.2006.00105.x. [DOI] [PubMed] [Google Scholar]
- 9.Mazur A, Matusik P, Revert K, Nyankovskyy S, Socha P, Binkowska-Bury M, et al. Childhood obesity: Knowledge, attitudes, and practices of European pediatric care providers. Pediatrics. 2013;132:e100–8. doi: 10.1542/peds.2012-3239. [DOI] [PubMed] [Google Scholar]
- 10.Van Gerwen M, Franc C, Rosman S, Le Vaillant M, Pelletier-Fleury N. Primary care physicians knowledge, attitudes, beliefs and practices regarding childhood obesity: A systematic review. Obe Rev. 2009;10:227–36. doi: 10.1111/j.1467-789X.2008.00532.x. [DOI] [PubMed] [Google Scholar]
- 11.Triches RM, Giugliani ER. Obesity, eating habits and nutritional knowledge among school children. Rev Saude Publica. 2005;39:541–7. doi: 10.1590/s0034-89102005000400004. [DOI] [PubMed] [Google Scholar]
- 12.Economos CD, Bakun PJ, Herzog JB, Dolan PR, Lynskey VM, Markow D, et al. Children's perceptions of weight, obesity, nutrition, physical activity and related health and socio-behavioural factors. Public Health Nutr. 2012;17:170–8. doi: 10.1017/S136898001200479X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adair LS, Popkin BM. Are child eating patterns being transformed globally? Obes Res. 2005;13:1281–99. doi: 10.1038/oby.2005.153. [DOI] [PubMed] [Google Scholar]
- 14.Bouchard C. Childhood obesity: Are genetic differences involved? Am J Clin Nutr. 2009;89:1494–501S. doi: 10.3945/ajcn.2009.27113C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gibbs BG, Forste R. Socioeconomic status, infant feeding practices and early childhood obesity. Pediatr Obes. 2014;9:135–46. doi: 10.1111/j.2047-6310.2013.00155.x. [DOI] [PubMed] [Google Scholar]
- 16.Rooney BL, Mathiason MA, Schauberger CW. Predictors of obesity in childhood, adolescence, and adulthood in a birth cohort. Matern Child Health J. 2011;15:1166–75. doi: 10.1007/s10995-010-0689-1. [DOI] [PubMed] [Google Scholar]
- 17.Muhihi AJ, Mpembeni RN, Njelekela MA, Anaeli A, Chillo O, Kubhoja S, et al. Prevalence and determinants of obesity among primary school children in Dar es Salaam, Tanzania. Arch Public Health. 2013;71:26. doi: 10.1186/0778-7367-71-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cogill B. Anthropometric Indicators Measurement Guide. Vol. 360. Washington: Food and Nutrition Technical Assistance (FANTA) Project, FHI; 2003. [Google Scholar]
- 19.Asayama K, Ozeki T, Sugihara S, Ito K, Okada T, Tamai H, et al. Criteria for medical intervention in obese children: A new definition of “obesity disease” in Japanese children. Pediatr Int. 2003;45:642–6. doi: 10.1046/j.1442-200x.2003.01795.x. [DOI] [PubMed] [Google Scholar]
- 20.Olden CL, Flegal KM. Changes in terminology for childhood overweight and obesity. Natl Heal Stat Rep. 2010;25:1–5. [PubMed] [Google Scholar]
- 21.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999-2002. JAMA. 2004;291:2847–50. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 22.Lobstein T, Frelut ML. Prevalence of overweight among children in Europe. Obes Rev. 2003;4:195–200. doi: 10.1046/j.1467-789x.2003.00116.x. [DOI] [PubMed] [Google Scholar]
- 23.Taleb S, Agli A. Obesity of the child: Role of the socio-economic factors, parental obesity, food behavior and physical activity in schoolchildren in a city of east Algeria. Cah Nutr Diet. 2009;44:198–206. [Google Scholar]
- 24.Pan L, Blanck HH, Sherry B, Dalenius K, Grummer-Strawn LM. Trends in the prevalence of extreme obesity among US preschool-aged children living in low-income families, 1998-2010. JAMA. 2012;308:2563–5. doi: 10.1001/jama.2012.108099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.de Onis M, Blössner M, Borghi E. Global prevalence and trends of overweight and obesity among preschool children. Am J Clin Nutr. 2010;92:1257–64. doi: 10.3945/ajcn.2010.29786. [DOI] [PubMed] [Google Scholar]
- 26.Monasta L, Batty GD, Cattaneo A, Lutje V, Ronfani L, Van Lenthe FJ, et al. Early-life determinants of overweight and obesity: A review of systematic reviews. Obes Rev. 2010;11:695–708. doi: 10.1111/j.1467-789X.2010.00735.x. [DOI] [PubMed] [Google Scholar]
- 27.Popkin BM, Gordon-Larsen P. The nutrition transition: Worldwide obesity dynamics and their determinants. Int J Obes Relat Metab Disord. 2004;28:S2–9. doi: 10.1038/sj.ijo.0802804. [DOI] [PubMed] [Google Scholar]
- 28.Singh GK, Kogan MD, Van Dyck PC, Siahpush M. Racial/ethnic, socioeconomic, and behavioral determinants of childhood and adolescent obesity in the United States: Analyzing independent and joint associations. Ann Epidemiol. 2008;18:682–95. doi: 10.1016/j.annepidem.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 29.Nauta C, Byrne C, Wesley Y. School nurses and childhood obesity: An investigation of knowledge and practice among school nurses as they relate to childhood obesity. Issues Compr Pediatr Nurs. 2009;32:16–30. doi: 10.1080/01460860802610186. [DOI] [PubMed] [Google Scholar]
- 30.Jelalian E, Boergers J, Alday CS, Frank R. Survey of physician attitudes and practices related to pediatric obesity. Clin Pediatr (Phila) 2003;42:235–45. doi: 10.1177/000992280304200307. [DOI] [PubMed] [Google Scholar]
- 31.Mosleh A, Mohammed H, Dalia E. Assessment of knowledge, attitude and practice of adolescents towards obesity in the preparatory schools in Ismailia city - Egypt. Egypt J Community Med. 2011;29 [Google Scholar]
- 32.Lee S, Ahn HS. Relation of obesity-related attitudes, knowledge, and eating behaviors with body weight and body shape satisfaction in 5th-grade Korean children. Nutr Res Pract. 2007;1:126–30. doi: 10.4162/nrp.2007.1.2.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Maximova K, McGrath JJ, Barnett T, O’Loughlin J, Paradis G, Lambert M. Do you see what I see. Weight status misperception and exposure to obesity among children and adolescents? Int J Obes (Lond) 2008;32:1008–15. doi: 10.1038/ijo.2008.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reinehr T, Kersting DM, Chahda C, Wollenhaupt A, Andler W. Nutritional knowledge of obese compared to non obese children. Nutr Res. 2003;23:645–9. doi: 10.1097/00005176-200109000-00026. [DOI] [PubMed] [Google Scholar]
- 35.Thakur N, D’Amico F. Relationship of nutrition knowledge and obesity in adolescence. Fam Med. 1999;31:122–7. [PubMed] [Google Scholar]
- 36.Wardle J, Volz C, Golding C. Social variation in attitudes to obesity in children. Int J Obes Relat Metab Disord. 1995;19:562–9. [PubMed] [Google Scholar]
- 37.Rees R, Oliver K, Woodman J, Thomas J. The views of young children in the UK about obesity, body size, shape and weight: A systematic review. BMC Public Health. 2011;11:188. doi: 10.1186/1471-2458-11-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McCormick DP, Sarpong K, Jordan L, Ray LA, Jain S. Infant obesity: Are we ready to make this diagnosis? J Pediatr. 2010;157:15–9. doi: 10.1016/j.jpeds.2010.01.028. [DOI] [PubMed] [Google Scholar]
- 39.van Dijk CE, Innis SM. Growth-curve standards and the assessment of early excess weight gain in infancy. Pediatrics. 2009;123:102–8. doi: 10.1542/peds.2007-3382. [DOI] [PubMed] [Google Scholar]
- 40.Bruce KD, Hanson MA. The developmental origins, mechanisms, and implications of metabolic syndrome. J Nutr. 2010;140:648–52. doi: 10.3945/jn.109.111179. [DOI] [PubMed] [Google Scholar]
- 41.Desai M, Beall M, Ross MG. Developmental origins of obesity: Programmed adipogenesis. Curr Diab Rep. 2013;13:27–33. doi: 10.1007/s11892-012-0344-x. [DOI] [PMC free article] [PubMed] [Google Scholar]


