Abstract
Background:
Oil pulling or oil swishing therapy is a traditional procedure in which the practitioners rinse or swish oil in their mouth. It is supposed to cure oral and systemic diseases but the evidence is minimal. Oil pulling with sesame oil and sunflower oil was found to reduce plaque related gingivitis. Coconut oil is an easily available edible oil. It is unique because it contains predominantly medium chain fatty acids of which 45-50 percent is lauric acid. Lauric acid has proven anti inflammatory and antimicrobial effects. No studies have been done on the benefits of oil pulling using coconut oil to date. So a pilot study was planned to assess the effect of coconut oil pulling on plaque induced gingivitis.
Materials and Methods:
The aim of the study was to evaluate the effect of coconut oil pulling/oil swishing on plaque formation and plaque induced gingivitis. A prospective interventional study was carried out. 60 age matched adolescent boys and girls in the age-group of 16-18 years with plaque induced gingivitis were included in the study and oil pulling was included in their oral hygiene routine. The study period was 30 days. Plaque and gingival indices of the subjects were assessed at baseline days 1,7,15 and 30. The data was analyzed using paired t test.
Results:
A statistically significant decrease in the plaque and gingival indices was noticed from day 7 and the scores continued to decrease during the period of study.
Conclusion:
Oil pulling using coconut oil could be an effective adjuvant procedure in decreasing plaque formation and plaque induced gingivitis.
Keywords: Coconut oil, oil pulling, plaque induced gingivitis
INTRODUCTION
Oral health is of prime importance to all individuals. Oral hygiene habits are instilled in childhood itself irrespective of the nationality or geographic location of an individual. The most reliable and accepted method of oral hygiene maintenance the world over are mechanical methods of tooth cleaning but adjuvants for decreasing plaque formation and maintaining oral hygiene have been sought. Presently chemotherapeutic agents are used as adjuvant agents to reduce plaque formation but they have their own disadvantages.1
Kavala graha or Gandoosha2 are procedures recommended for oral hygiene maintenance in ayurveda. They are elaborately mentioned in the texts of Charaka Samhita and Sushrutha's Samhitha. It is described as a procedure in which an individual takes a comfortable amount of oil/medicated oil and holds it or swishes it in the mouth. When the oil turns thin and milky white it is spit out without swallowing.2
Dr. F. Karach popularised this procedure as oil pulling.3 He claimed that oil pulling can cure several illnesses including oral diseases, but his claims were not supported by evidence. Recent studies of oil pulling therapy using sunflower oil4 and sesame oil5 were found to decrease plaque induced gingivitis. Even though coconut oil is used for gargling among the people in coconut farming communities, no studies have been done on the benefits of oil pulling using coconut oil, to date.
Coconut oil is an edible oil and is consumed as a part of the staple diet in many tropical countries. Coconut oil is a highly desired and easily available oil in India. It is used in cooking and for its cosmetic properties. Coconut oil is different from most other dietary oils because the predominant composition of coconut oil is a medium chain fatty acid, whereas in the majority of other oils the basic building blocks are almost entirely long chain fatty acids. This influences the physical and chemical properties of the oil. Coconut oil contains 92% saturated acids, approximately 50% of which is lauric acid. Human breast milk is the only other naturally occurring substance with such a high concentration of lauric acid. Lauric acid has proven anti-inflammatory effects and antimicrobial effects.6,7,8
Therefore a study was conducted to assess the effect of coconut oil on plaque formation and plaque related gingivitis.
MATERIALS AND METHODS
The aim of the study was to evaluate the effect of coconut oil pulling/oil swishing on plaque formation and to evaluate the effect on plaque induced gingivitis. A prospective interventional study was carried out. A total of 60 age matched subjects in the age-group of 16-18 years with plaque induced gingivitis were included in the study. Informed consent was taken for their inclusion in the study. The use of systemic or topical antibiotics and the history of dental treatment in the past one month were set as exclusion criteria. All the subjects were recruited into a single group. There was no control group in the study. The study was designed to compare the baseline values and the post intervention values in a single group performing coconut oil pulling in addition to their oral hygiene routine.
A thorough history regarding the medical condition and the medication taken in the past 6 months was obtained from the subjects. The oral hygiene habits of all the subjects were recorded in detail. All the chosen subjects had a habit of brushing once or twice a day with toothbrush and paste. Six subjects had the habit of flossing once in the night along with brushing twice a day. The subjects were advised to routinely perform oil pulling with coconut oil every day in the morning in addition to their oral hygiene routine. Five subjects discontinued from the study as they could not tolerate the taste of the oil and three subjects discontinued from the study because of antibiotic usage during the period.
Modified Gingival Index9 and Plaque Index10 were used as the clinical measures to assess gingival inflammation and plaque formation respectively. The clinical examination was performed by two independent observers. All subjects were assessed around 4 hrs after performing oil pulling. Plaque and gingival indices were measured at baseline that is, and on days 1, 7, 15, 30 after the oil pulling routine was started. The final scores were statistically analyzed using the students paired t test. Interobserver agreement was measured using the kappa coefficient.
RESULTS
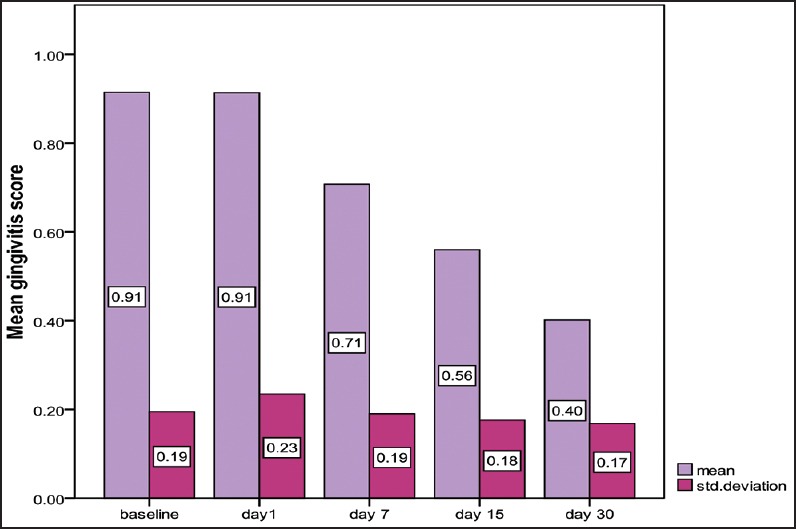
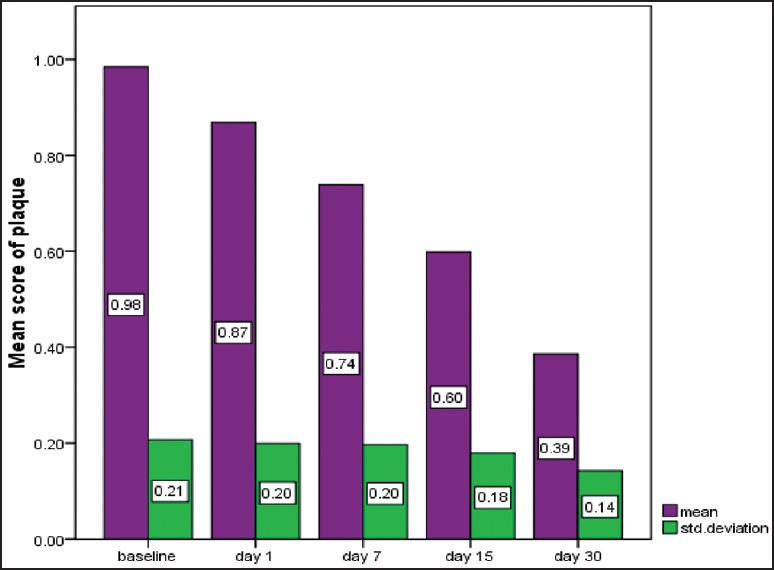
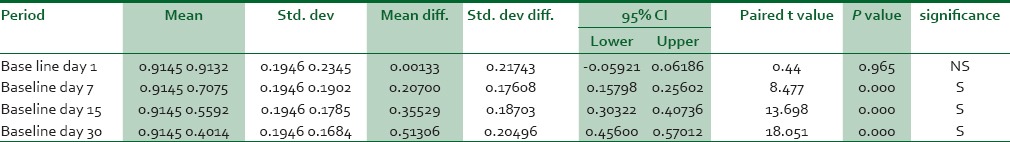
Reliability of clinical examination was tested for all the days of assessment and the interexaminer reliability was found to be substantial to good. The Kappa coefficient scores were in the range of 65-92 [Table 1a and b]. The mean gingival index was 0.91 and the plaque index was 1.19 at baseline. In comparison to the baseline values both the gingival and the plaque indices substantially reduced during the period of assessment. There was a steady decline in both the plaque index and the gingival index values from day 7. The average gingival index score on day 30 was down to 0.401 and the plaque index score was 0.385 [Figures 1 and 2]. Statistical analysis using the paired t test showed that the decrease was statistically significant [Tables 2 and 3].
Table 1a.
Kappa scores for modified gingival index
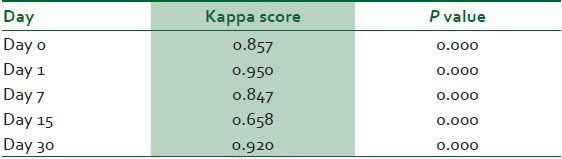
Table 1b.
Kappa scores for plaque index
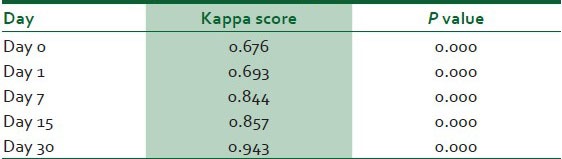
Figure 1.
Shows the mean and standard deviation of plaque index scores
Figure 2.
Shows the mean and standard deviation of gingival index scores
Table 2.
Comparison of plaque index scores between baseline, 7, 15, and 30 days
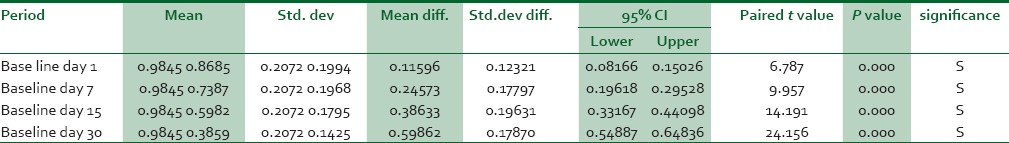
Table 3.
Comparison of gingival index scores between baseline, 15, 30 and 45 days
DISCUSSION
The primary cause of gingival inflammation is plaque. Dental plaque is defined clinically as a structured, resilient substance that adheres to intraoral hard surfaces and is composed of bacteria in a matrix of salivary glycoprotein and extracellular polysaccharides. Plaque induced gingivitis is the result of an interaction between plaque and the tissues and the inflammatory response of the host. It is associated with the subtle microbial alterations as the plaque matures.11,12
Oral hygiene measures using chemo mechanical procedures reduce the incidence of plaque related diseases by decreasing the plaque accumulation. Our study aimed at checking the effectiveness of oil pulling with coconut oil as an adjuvant to brushing, in decreasing the plaque accumulation and plaque induced gingivitis. Plaque Index by Sillness and Loe10 and Modified Gingival Index9 were used for clinical assessment in the study as they are the most widely used indices in trials for therapeutic agents.13 Oil pulling with sunflower oil was found to significantly reduce plaque index and gingival index after 45 days.4 Asokan et al., found oil pulling therapy with sesame oil was equally effective as chlorhexidine in decreasing plaque induced gingivitis.5 In our study also there was a significant decrease in the plaque and the gingival index at the end of 30 days.
There are various hypotheses on the mechanisms by which oil pulling may act in decreasing the plaque and gingival index. In oil pulling, as the oil is swished in the mouth the mechanical shear forces exerted on the oil leads to its emulsification and the surface area of the oil is greatly increased. The oil film thus formed on the surface of the teeth and the gingiva can reduce plaque adhesion and bacterial co aggregation.5
It was also proposed that the alkalis in the saliva can react with the oil leading to saponification and formation of a soap like substance [Figure 3] which can reduce the adhesion of plaque.5,14 Coconut oil has a high saponification value and is one of the most commonly used oil in making soaps. The soaps produced with coconut oil can lather well and have an increased cleansing action.15 The lauric acid in the coconut oil can easily react with sodium hydroxide in saliva during oil pulling to form sodium laureate, the main constituent of soap16 which might be responsible for the cleansing action and decreased plaque accumulation.
Figure 3.
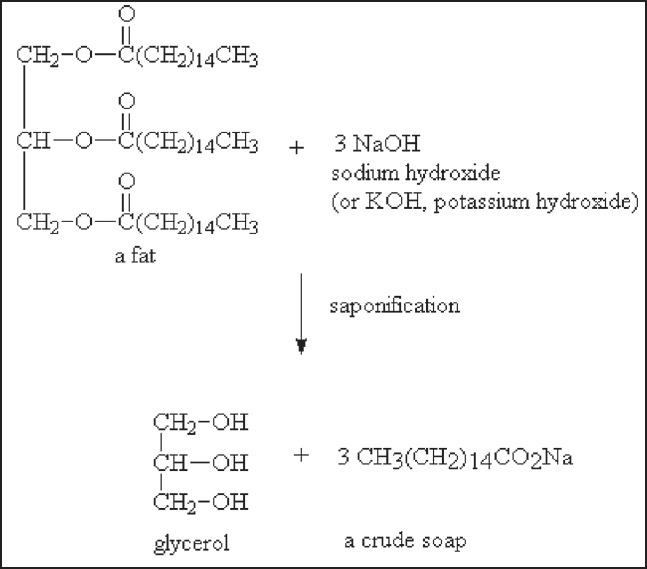
Saponification reaction
The significant reduction in gingivitis can be attributed to decreased plaque accumulation and the anti-inflammatory, emollient effect of coconut oil. In animal studies coconut oil was found to be an effective burn wound healing agent and this was attributed to its anti-inflammatory and antiseptic properties.17 Coconut oil showed moderate anti-inflammatory effects on ethyl phenylpropiolate induced ear edema in rats, and carrageenin and arachidonic acid-induced paw edema.18 It was found be effective and safe when used as an emollient and moisturiser.19
There are many commercially available mouthwashes. Chlorhexidine containing mouthwashes have been found to be the most effective among them. Listerine (phenol compound) and Meridol (an amine/stannous fluoride mouthwash) were found to be less efficacious than Chlorhexidine in controlling plaque induced gingivitis. (Listerine) and (Meridol). After 3 weeks of rinsing, plaque indices remained the lowest in the chlorhexidine group, while subjects using Listerine or Meridol the score were similar but significantly lower than that of individuals rinsing with the placebo solution. The antimicrobial potential of chlorhexidine was found to be the highest followed by Meridol.20 In our study there was a 50% decrease in the plaque and gingival index scores in 4 weeks which is comparable to the decrease produced by chlorhexidine.
Chlorhexidine on long term use alters taste sensation and produces brown staining on the teeth which is very difficult to remove. The mucous membranes and the tongue can also be affected and may be related to the precipitation of chromogenic dietary factors on to the teeth and mucous membranes.21 Staining is also associated with the of long term use of Phenol compound and stannous fluoride containing mouth washes.22 In the present study there were no reported alterations in the taste or noticeable staining from coconut oil at the end of 4 weeks.
As an antimicrobial agent, chlorhexidine is effective against both gram positive and gram negative bacteria. Its antibacterial action is due to an increase in cellular membrane permeability followed by coagulation of the cytoplasmic macromolecules.23,24,25 It has also been shown that chlorhexidine can reduce the adherence of Porphyromonas gingivalis to epithelial cells.26 Pure-culture studies of 10 oral bacteria (eight genera) showed that Actinomyces naeslundii, Veillonella dispar, Prevotella nigrescens, and the streptococci were highly susceptible to CHX, while Lactobacillus rhamnosus, Fusobacterium nucleatum, were less susceptible.27
Studies show that coconut oil also has substantial antimicrobial activity. This is attributed to the presence of monolaurin in coconut oil. It is shown to have significant antimicrobial activity against Escherichia vulneris, Enterobcater spp., Helicobacter pylori, Staphylococcus aureus, Candida spp., including C. albicans, C. glabrata, C. tropicalis, C. parapsilosis, C. stellatoidea and C. krusei7,28 Studies also show that coconut oil is affective against S. mutans and C. albicans in an in vitro oral biofilm model.29 The antimicrobial potency of coconut oil was not tested in our study. Further studies with a have been planned to check the antimicrobial potential of coconut oil. The fact that a control group with a proven chemotherapeutic agent was not used is the major the limitation of our study.
CONCLUSION
Oil pulling has been proven to be an effective method in reducing plaque formation and plaque induced gingivitis. This preliminary study shows that coconut oil is an easily usable, safe and cost effective agent with minimal side effects which can be used as an adjuvant in oral hygiene maintenance. More studies on the antimicrobial potency of coconut oil on microorganisms causing oral diseases is required to authenticate the use of coconut oil as an effective oral antimicrobial agent. Further studies on coconut oil with a large number of subjects and comparative studies using various chemotherapeutic agents can improve the quality of evidence.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Mandel ID. Chemotherapeutic agents for controlling plaque and gingivitis. J Clin Periodontol. 1998;15:488–98. doi: 10.1111/j.1600-051x.1988.tb01020.x. [DOI] [PubMed] [Google Scholar]
- 2.Sooryavanshi S, Mardikar BR. Prevention and treatment of diseases of mouth by gandoosha and kavala. Anc Sci Life. 1994;13:266–70. [PMC free article] [PubMed] [Google Scholar]
- 3.Bruce Fife MD. Health Colorado Springs: Wise publications Co. 1st edition. 2000. The healing miracle of coconut oil. Piccadilly Books Ltd; pp. 1–46. [Google Scholar]
- 4.Amith HV, Ankola AV, Nagesh L. Effect of oil pulling on plaque and gingivitis. J Oral Health Community Dent. 2007;1:12–8. [Google Scholar]
- 5.Asokan S, Emmadi P, Chamundeswari R. Effect of oil pulling on plaque induced gingivitis: A randomized, controlled, triple-blind study. Indian J Dent Res. 2009;20:47–51. doi: 10.4103/0970-9290.49067. [DOI] [PubMed] [Google Scholar]
- 6.DebMandal M, Mandal S. Coconut (Cocos nucifera L: Arecaceae): In health promotion and disease prevention. Asian Pac J Trop Med. 2011;4:241–7. doi: 10.1016/S1995-7645(11)60078-3. [DOI] [PubMed] [Google Scholar]
- 7.Ogbolu DO, Oni AA, Daini OA, Oloko AP. In vitro antimicrobial properties of coconut oil on Candida species in Ibadan, Nigeria. J Med Food. 2007;10:384–7. doi: 10.1089/jmf.2006.1209. [DOI] [PubMed] [Google Scholar]
- 8.Pehowick DJ, Gomes AV, Barnes JA. Fatty acid composition and possible health effects of coconut constituents. West Indian Med J. 2000;49:128–33. [PubMed] [Google Scholar]
- 9.Lobene RR, Weatherford T, Ross NM, Lamm RA, Menaker L. A modified gingival index for use in clinical trials. Clin Prev Dent. 1986;8:3–6. [PubMed] [Google Scholar]
- 10.Löe H. The Gingival Index, the Plaque Index and the Retention Index Systems. J Periodontol. 1967;38:610–6. doi: 10.1902/jop.1967.38.6.610. [DOI] [PubMed] [Google Scholar]
- 11.Newman MG, Takei HH, Klokkervold PR. Carranza's Clinical Periodontology. 10th edition. Elsevier; 2006. p. 241. [Google Scholar]
- 12.Marsh PD. Dental plaque: Biological significance of a biofilm and community life-style. J Clin Periodontol. 2005;32:7–15. doi: 10.1111/j.1600-051X.2005.00790.x. [DOI] [PubMed] [Google Scholar]
- 13.Ciancio SG. Current status of indices of gingivitis. J Clin Periodontol. 1986;13:375–8. doi: 10.1111/j.1600-051x.1986.tb01476.x. [DOI] [PubMed] [Google Scholar]
- 14.Ambika S. Kartik Offsets Printers. 7th edition. 2001. Fundamentals of biochemistry for medical students; pp. 50–4. [Google Scholar]
- 15.Alsberg CL, Taylor AE. The Fats and Oils - A General Overview (Fats and Oils Studies No.1) Stanford University Press; 1928. p. 86. [Google Scholar]
- 16.Pavia DL, Lampman GM, Kriz GS, Engel RG. Brooks/Cole Laboratotory series for organic chemistry. 2nd edition. 2004. Introduction to Organic Laboratory Techniques: A Small Scale Approach; pp. 252–65. [Google Scholar]
- 17.Srivastava P, Durgaprasad S. Burn wound healing property of Cocos nucifera: An appraisal. Indian J Pharmacol. 2008;40:144–6. doi: 10.4103/0253-7613.43159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Intahphuak S, Khonsung P, Panthong A. Anti-inflammatory, analgesic, and antipyretic activities of virgin coconut oil. Pharm Biol. 2010;48:151–7. doi: 10.3109/13880200903062614. [DOI] [PubMed] [Google Scholar]
- 19.Agero AL, Verallo-Rowell VM. A randomized double-blind controlled trial comparing extra virgin coconut oil with mineral oil as a moisturizer for mild to moderate xerosis. Dermatitis. 2004;15:109–16. doi: 10.2310/6620.2004.04006. [DOI] [PubMed] [Google Scholar]
- 20.Brecx M, Brownsfone E, MacDonald L, Gelskey S, Cheang M. Efficacy of Listerine®, Meridol® and chlorhexidine mouthrinses as supplements to regular tooth-cleaning measures. J Clin Periodontol. 1992;19:202–7. doi: 10.1111/j.1600-051x.1992.tb00640.x. [DOI] [PubMed] [Google Scholar]
- 21.Leard A, Addy M. The propensity of different brands of tea and coffee to cause staining associated with chlorhexidine. J Clin Periodontol. 1997;24:115–8. doi: 10.1111/j.1600-051x.1997.tb00476.x. [DOI] [PubMed] [Google Scholar]
- 22.Brecx M, Macdonald LL, Legary K, Cheang M, Forgay MG. Long-term Effects of Meridol® and chlorhexidine mouthrinses on plaque, gingivitis, staining, and bacterial vitality. J Dent Res. 1993;72:1194–7. doi: 10.1177/00220345930720080601. [DOI] [PubMed] [Google Scholar]
- 23.Hennessy T. Some antibacterial properties of chlorhexidine. J Periodont Res. 1973;8:61–7. doi: 10.1111/j.1600-0765.1973.tb02166.x. [DOI] [PubMed] [Google Scholar]
- 24.Emisilon CG. Susceptibility of various microorganisms to chlorhexidine. Scand J Dent Res. 1977;85:255–65. doi: 10.1111/j.1600-0722.1977.tb00561.x. [DOI] [PubMed] [Google Scholar]
- 25.Budtz-Jorgensen E, Löe H. Chlorhexidine as a denture disinfectant in the treatment of denture stomatitis. Scand J Dent Res. 1972;80:457–64. doi: 10.1111/j.1600-0722.1972.tb00314.x. [DOI] [PubMed] [Google Scholar]
- 26.Grenier D. Effect of chlorhexidine on the adherence properties of Porphyromonas gingivalis. J Clin Periodontol. 1996;23:140–2. doi: 10.1111/j.1600-051x.1996.tb00547.x. [DOI] [PubMed] [Google Scholar]
- 27.McBain AJ, Bartolo RG, Catrenich CE, Charbonneau D, Ledder RG, Gilbert P. Effects of a chlorhexidine gluconate-containing mouthwash on the vitality and antimicrobial susceptibility of in vitro oral bacterial ecosystems. Appl Environ Microbiol. 2003;69:4770–6. doi: 10.1128/AEM.69.8.4770-4776.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Verallo-Rowell VM, Dillague KM, Syah-Tjundawan BS. Novel antibacterial and emollient effects of coconut and virgin olive oils in adult atopic dermatitis. Dermatitis. 2008;19:308–15. [PubMed] [Google Scholar]
- 29.Thaweboon S, Nakaparksin J, Thaweboon B. Effect of oilpulling on oral microorganisms in biofilm models. Asia J Public Health. 2011;2:62–6. [Google Scholar]


