Abstract
Background:
Our aim was to demonstrate what women reported being counselled about weight gain in pregnancy, their perceptions of inappropriate gestational weight gain (GWG), and plans for weight gain in pregnancy.
Materials and Methods:
A cross-sectional survey of perceptions of prenatal attendees about inappropriate GWG was conducted at the prenatal clinic of a referral tertiary health facility in south western, Nigeria, between January 1, 2013 and June 30, 2013. Primary outcomes were the perceptions of women about risks involved with inappropriate weight gain and the proportion of women who self-reported being counselled at all on GWG, and had the right knowledge of risk(s) involved with inappropriate weight gain during pregnancy.
Results:
Of the 348 women who completed the survey, approximately four-fifths (82.8%) reported GWG being discussed at all by health care provider. Fewer women (29.3%) believed there were maternal risks with excess weight gain compared to inadequate weight gain (34.8%). With respect to perception of risks of inappropriate weight gain to infants, 23.65 and 18.4%, respectively, believed there were infant risks with excess and inadequate GWG. Overweight women [OR 0.39 (95% CI 0.16-0.98)] and those who received GWG information from more than one type of health care provider [OR 4.71 (95% CI 1.64-13.78)] had significant increased rate of correct knowledge of risks involved with inappropriate GWG.
Conclusion:
The lack of awareness of risks involved with inappropriate GWG by over half of respondents underscores the need for improvement in educational intervention on GWG in our environment.
Keywords: Knowledge, obesity, pregnancy, perception, weight gain
INTRODUCTION
Weight gain in pregnancy remains a matter of great concern for women and health care providers. This worry about weight exists because of the influence of inappropriate weight or gestational weight gain (GWG) on pregnancy outcome.1,2,3 The prevalence of obesity or overweight in pregnancy is rising,4 and is of international concern.5 Although obesity is a common nutritional problem among pregnant women particularly in the industrialised nations,6 the westernisation of lifestyles in developing nations may tilt the statistics on obesity in pregnancy to reaching proportions in this population.
Estimates of the prevalence of overweight or obesity among adults in Nigeria range from 26% through 74.3%.7,8,9,10 Studies indicate that overweight and obesity are more prevalent in women than men,8,9,10 and approximately 40% of reproductive-aged women are overweight or obese.3 In Nigeria, studies demonstrate prevalence ranging between 7.4% and 10.7% for obesity in pregnancy.11,12,13
Excessive or inadequate GWG has significant effects on maternal, foetal and neonatal outcomes, including long term maternal and childhood health risks in life.14,15,16,17,18,19,20,21,22,23,24 Data from observational studies conducted in Nigeria found significant risk of obstetric complications with obesity; comprising hypertensive disorders, diabetes mellitus, operative delivery, dystocia in labour, macrosomia, and birth asphyxia.12,13,25,26,27 Underweight or inadequate weight gain have the potential for increased risk of preterm birth, low birth weight, intrauterine growth restriction (IUGR) or small for gestational age (SGA).28,29
To promote weight-related antenatal interventions for improving pregnancy outcome in our obstetric population, this study sought to demonstrate what women reported being counselled about weight gain, their understandings and perception of the risks associated with inappropriate GWG and plans for weight gain in the index pregnancy. This research would provide necessary evidence for modification of practice and introduction of interventions to promoting healthy weight gain during pregnancy, as correct advice from care provider is more linked with optimal GWG.30
MATERIALS AND METHODS
This cross-sectional study was conducted among pregnant women who were receiving antenatal care at the Prenatal Outpatient Clinic of our hospital after an informed consent, between January 1, 2013 and June 30, 2013 using a validated self-administered questionnaire. The survey questions were developed based on the extensive review of recently published studies on women's perception or understanding of weight gain and associated risks during pregnancy.5,31,32,33 This study was approved by the Ethics and Research committee of Ekiti State University Teaching Hospital, Ado-Ekiti, Nigeria.
Eligible participants for the study were women who had at least one prenatal visit after the first prenatal clinic registration visit, were able respond to the questions in the survey unaided, and had a viable singleton pregnancy at the time of survey completion. Women were excluded from the study if they had multiple gestations or evidence suggestive of intrauterine foetal death.
The correctness of the anthropometric information (gestational age, maternal weight, maternal height, and the number of prenatal visits) on the completed questionnaire was established using the clinical prenatal care records.
Outcome measures
Primary outcomes were the perceptions of women about risks involved with inappropriate weight gain and the proportion of women who self-reported being counselled at all on GWG, and had the right knowledge of risk(s) involved with inappropriate weight gain during pregnancy.
Based on the recent published study which found that 42.7% of prenatal attendees reported being counselled at all on weight gain in pregnancy,33 we calculated that 261 surveys would be the minimum required to estimate the proportion of women who were counselled on weight gain at all to within ± 6%.
Data analysis
Data analyses were performed using the statistical software package SPSS 17 (SPSS Inc., version 17.0, Chicago, IL, USA). We examined maternal plans for weight gain with respect to body mass index (BMI) category and perceived weight status. Univariate analysis was used to examine the unadjusted odds of women's knowledge of risks with inappropriate weight gain for each maternal variable in relation to a particular referent category. The independent effects of variables associated with right knowledge of risks involved with gestational weight at the P < 0.05 on univariate analysis were tested using multivariate logistic regression to evaluate the adjusted odds. Statistical significance level was set at a P-value less than 0.05.
RESULTS
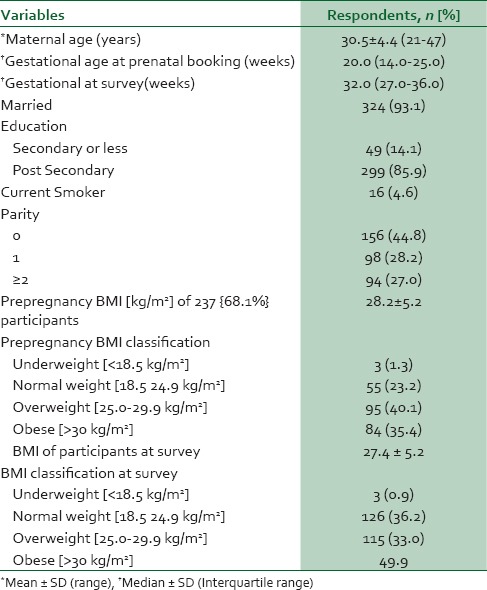
Of the women who were approached to participate in the survey between January and June 2013, 348 women were eligible for inclusion into the study analysis. The demographic and clinical characteristics of the study population are presented in Table 1.
Table 1.
Demographic characteristics of respondents
Approximately 82.8% of the women reported receiving counselling on GWG at all from their health care providers [Table 2]. Twenty-two percent of respondents (22.4%) reported that their health care provider had recommended that they should gain a specific range of weight (12-12.5 kg). About three-fifths (56.6%) of women reported being counselled that there were increased risks with excess gestational weight; however, a higher proportion (69.5%) of the women reported being counselled on the risks with inadequate GWG. Approximately a third (29.3%) and quarter (23.6%) of the women believed there were maternal and infant risks, respectively, with excess GWG. Nearly a third (34.8%) of the respondents believed that inadequate weight gain below the recommended range poses risk to maternal health while fewer women (18.4%) believed that infant risks are also increased. Almost all the women (98.9%) believed that weight measurement at each prenatal visit would be helpful in their plans for weight gain during pregnancy. Ninety percent (89.9%) of women thought that the provision of weight gain information at prenatal booking visit would help to maintain appropriate GWG. With respect to maternal perception of weight status at survey, nine out of every ten women (90.5%) perceived themselves to be normal weight; the weight perception of the remaining one-tenth was largely overweight (7.5%). Only 2% of the respondents reported self-perception of their weight status as underweight. None of the women perceived themselves to be obese in contrast to the obesity prevalence of 29.9% at survey.
Table 2.
Patient perception of gestational weight gain
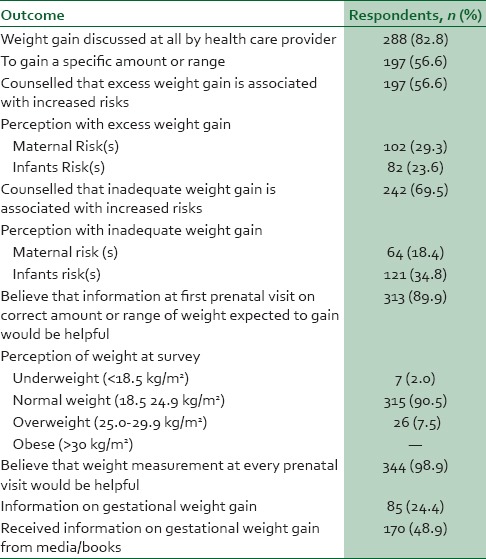
When enquired as to the sources of information on GWG, 40.2%, 22.7%, and 13.2% of respondents, respectively, stated nurses, dieticians, and doctors (obstetricians or family physicians), with 13.2% reporting that they received information from two or more aforementioned care providers. Approximately one-fifth (17.2%) of the respondents reported not ever receiving information on GWG at all from health care provider. Approximately one-quarter (24.4%) of the women stated that family and friends provided counselling on weight gain besides care provider and nearly one-half (48.9%) stated they acquired knowledge on weight gain from reading and internet.
Overall, 46.3% of women correctly reported risk(s) with inappropriate weight gain during pregnancy. The common reported maternal risks involved with excess weight gain were caesarean section, gestational diabetes, labour dystocia and hypertension (15.8%, 6.3%, 4.6%, and 4.0% respectively). Only 3(0.9%) women each reported haemorrhage and obesity as risks to themselves during pregnancy and longer term respectively. The frequently reported risk of excess GWG to infant was macrosomia (20.7%); with perinatal mortality and childhood obesity being reported by one (0.3%) and two (0.6) women respectively. Approximately 1 in 5 women (20.7%) reported foetal growth restriction as risk of inadequate weight gain. The reported rates of low birth weight and prematurity as risks associated with inadequate GWG were 12.4% and 1.4% respectively.
The relationship between BMI category (Prepregnancy and survey BMI), patients’ perception of own weight and their plans for weight gain during pregnancy were examined [Table 3]. Among the two hundred and thirty eight of the final study sample of 348 respondents who provided information (prepregnancy weight and height) for calculation of prepregnancy BMI, slightly higher than two-thirds (68.4%) were planning to maintain normal weight or gain within the recommended range; the BMI classification of respondents planning to maintain normal weight was underweight, normal weight, overweight and obese (33.3%, 72.4%, 61.1% and 75.0% respectively). Thirty percent (30.8%) of the sub-group with prepregnancy BMI were intending to gain excess weight (66.7%, 27.3%, 39.0%, 22.6%, respectively of underweight, normal weight, overweight and obese respondents) while only obese women (0.8%) were planning to lose weight.
Table 3.
Patients’ intentions of or plans for gestational weight gain (GWG)
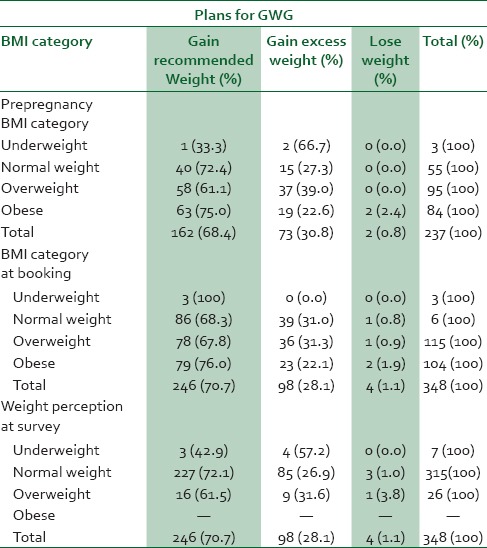
With respect to BMI category at prenatal booking visit and maternally perceived weight status at survey completion, approximately 70%, 28%, and 1% of the final study population, respectively, were planning to maintain normal weight, gain excessive weight and lose weight. Among women who plan to maintain normal gestational weight, their distribution was 100.0%, 68.3%, 67.8% and 76.0% of underweight women, normal weight women, overweight women and obese women respectively. The distribution of the respondents planning to gain excess weight across the strata of BMI at booking was 31.0%, 31.3% and 22.1% of normal weight women, overweight women and obese women respectively. The proportion of women who planned to lose weight in relationship to the BMI status at prenatal booking visit shows slightly rising trend with increasing maternal weight status (0.0%, 0.8%, 0.9% and 0.9% respectively for underweight women, normal weight women, overweight women and obese women).
Based on maternally perceived weight status, 57.2%, 26.9 and 31.6% of underweight women, normal weight women and overweight women respectively were planning to gain excess weight. Conversely, a higher proportion of normal weight women (72.1%) and overweight women (61.5%) and smaller proportion of underweight women planned to maintain weight gain within recommended range. Only a small percentage of normal weight (1.1%) and overweight women (3.8%) planned to lose weight.
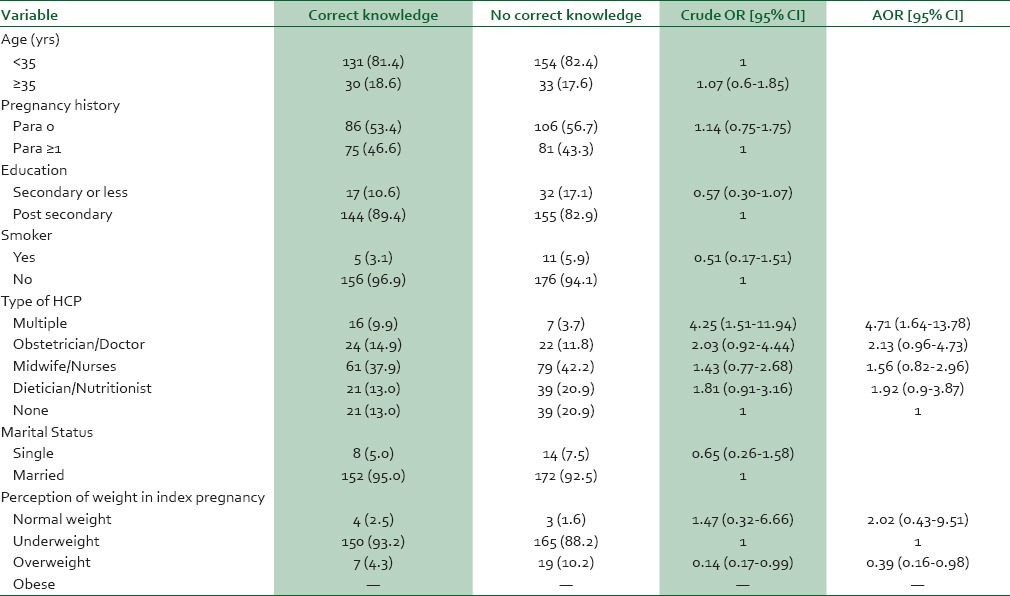
The relationships of maternal demographics, type of health care provider and weight perception to right/correct report of risks with inappropriate GWG are shown in Table 4. On univariate analysis, correct report of risks associated with inappropriate weight gain was significantly associated with having information on weight gain provided by multiple health care providers (Crude OR 4.25; 95% CI, 1.51-11.94) and perceived weight status being overweight (Crude OR 0.41; 95% CI, 0.17-0.99). Multivariate analysis with type of health care provider and perceived weight status in the regression model further showed that information on weight gain from multiple health care providers (AOR 4.71; 95% CI, 1.64-13.48) was associated with correct report of risk with inappropriate weight gain compared to women who received no information on weight from health care provider. Also, maternally perceived overweight status (AOR 0.39, 95% CI, 0.16-0.98) was significantly associated with poor report of risks with inappropriate weight gain compared to women who perceived their weight status as normal weight.
Table 4.
Predictors of patient correct knowledge of risk{s} with inappropriate weight gain
DISCUSSION
In this present study on maternal perspectives on GWG, approximately four-fifths (82.8%) reported being counselled on GWG at all, with one-fifth (22.4%) being counselled to gain a specific amount or range of weight during pregnancy. Compared to a recent study by McDonald et al.,32 the proportion of women (28.5%) who recalled being counselled to gain specific amount of weight is slightly higher than that of this present study. Other GWG studies based on revised IOM recommendations have consistently found higher rates of women being counselled correctly to gain an amount or range of weight.30,37
Phelan et al., found that over one-third of women were not counselled by health professionals about appropriate weight gain pregnancy.38 In our setting, health professionals’ advice about specific or range of weight gain may be limited by their awareness of the well-documented IOM guidelines. As BMI classification in our obstetric practice is based on weight-for-height at first antenatal consultation, irrespective of gestational age; care providers’ awareness of IOM guidelines which encourage weight gain based on pre-pregnancy BMI ranges may limit counselling women about the traditional average maternal weight of 12-12.5 kg which does not depend on maternal BMI ranges. The perception by the majority of women that ‘weight measurement at every antenatal consultation (98.9%)’ and ‘health professionals’ provision of information on the correct, specific amount or range of weight expected to gain in pregnancy at first antenatal consultation would be helpful suggest that absence of advice on the recommended weight gain may be associated with the reported lack of information on expected GWG health provider advise.
Despite the awareness of adverse obstetric outcomes with inappropriate GWG by nearly a half of our respondents, approximately a fifth (22.1%) to two-fifths (39.0%) of respondents who were overweight or obese based on pre-pregnancy BMI, first antenatal consultation's BMI or self-reported perceived weight status planned to gain weight in excess of the specific amount or range. These findings are consistent with a previous study from Canada which found that overweight or obese women planned to gain weight above guidelines.32 Additionally, the classification of approximately two-thirds (63.2%) of women as ‘inappropriate weight status (underweight, overweight, and obese)’ among women who considered themselves normal weight (n = 315) at first antenatal consultation underscores the importance of provider objective assessment of maternal weight status and advice on appropriate weight gain in pregnancy.
Our study also found that less than or approximately one-third of the women believed there are maternal or infant risks associated with inappropriate GWG (inadequate or excess weight gain) despite over half of the respondents reported being counselled by care providers that there were risks with inappropriate weight gain. This study also demonstrates that a higher proportion of women believed that there were risks with excess weight gains to themselves compared to their infants. Conversely, the proportion of women who perceived infant risks with inadequate weight gain is greater than those perceiving maternal risks with inadequate weight gain. The concern about caesarean section and foetal growth restriction, most frequent reported consequences of excessive and inadequate weight gain, respectively, may explain these findings. These findings are consistent with two prior studies by McDonald et al.31,32
We found that ‘receiving information on GWG from multiple health care professionals (AOR 4.71; 95% CI, 1.64-13.48), and “self-perceived weight status as overweight’ (AOR 0.39, 95% CI, 0.16-0.98) to be independent predictors of right knowledge of risk(s) with inappropriate GWG. We could not compare our findings with previous research as none has previously described the factors associated with correct report of risks involved with inappropriate weight gain. The strong relationship of advice on GWG from multiple health professionals suggests that the quality of counselling may strongly influence patients’ knowledge on weight gain in pregnancy.
Although our study was conducted using self-administered questionnaire, the anthropometric information given by women was validated using the prenatal clinical records. The median prenatal visit (four visits) in this study shows that many women had opportunities for counselling on GWG during the period of prenatal care. By enquiring on maternal self-perception of weight at prenatal booking visit, we could adequately counsel women whose weight perception differs from objective weight status as perceived weight status would influence plans for weight gain.
Despite the aforementioned strengths, our study has a number of limitations. This survey could not assess the information women acquired on amount or range of weight expected to gain based on the 2009 IOM guidelines, but this was not the primary outcome of this study. Recall bias in remembering prepregnancy weight may limit our findings. The lack of information on the number of health talks (a potential confounder on perceptions and knowledge of participants) received by each participants may limit the interpretation of our findings. As shown in Table 3, we chose to explore plans for GWG in current pregnancy by asking participants to check ‘Excessive weight gain’, ‘Excessive weight loss’, or ‘Maintain steady weight gain’, because this would reveal insight about the need for educational intervention based on the new weight gain guidelines in our country. However, this would be a common weakness of any study evaluating the information women received on weight gain in most countries that are yet to adopt the new pregnancy weight gain guidelines.
In conclusion, there were lower rates of perception of maternal and infant risks associated with inappropriate GWG (ranging from approximately 23-34%) despite the reported rate of counselling on risks involved with inappropriate weight gain by approximately two-thirds of the women in our study. Furthermore, a sizeable proportion of women who were considered overweight or obese based on pre-pregnancy, first antenatal consultation's BMI or self-reported perceived weight status planned to gain weight in excess of the specific amount or range. These findings may assist in strengthening the knowledge of women on all aspects of weight gain in pregnancy.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Andreto LM, de Souza AI, Figueiroa JN, Cabral-Filho JE. Factors associated with excessive gestational weight gain among patients in prenatal care at a public hospital in Recife, Pernambuco, Brazil. Cad Saude Publica. 2006;22:2401–9. doi: 10.1590/s0102-311x2006001100014. [DOI] [PubMed] [Google Scholar]
- 2.Costa BM, Maldi PC, Gil MF, Paulinelli RR. Determinant factors of excessive weight gain in eutrophic pregnant women. Femina. 2006;34:823–8. [Google Scholar]
- 3.Ramachendran J, Bradford J, McLean M. Maternal obesity and pregnancy complications: A review. Aust N Z J Obstet Gynaecol. 2008;48:228–35. doi: 10.1111/j.1479-828X.2008.00860.x. [DOI] [PubMed] [Google Scholar]
- 4.Davies GA, Maxwell C, McLeod L, Gagnon R, Basso M, Bos H, et al. Society of Obstetricians and Gynaecologists of Canada. Obesity in pregnancy. J Obstet Gynaecol Can. 2010;32:165–73. doi: 10.1016/S1701-2163(16)34432-2. [DOI] [PubMed] [Google Scholar]
- 5.Furber CM, McGowan L, Bower P, Kontopantelis E, Quenby S, Lavender T. Antenatal interventions for reducing weight in obese women for improving pregnancy outcome. Cochrane Database Syst Rev. 2013;1:CD009334. doi: 10.1002/14651858.CD009334.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wolfe HM, Gross TL. Obesity in pregnancy. Clin Obstet Gynecol. 1994;37:596–604. doi: 10.1097/00003081-199409000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Sola AO, Steven AO, Kayode JA, Olayinka AO. Underweight, overweight and obesity in adults Nigerians living in rural and urban communities of Benue State. Ann Afr Med. 2011;10:139–43. doi: 10.4103/1596-3519.82081. [DOI] [PubMed] [Google Scholar]
- 8.Wahab KW, Sani MU, Yusuf BO, Gbadamosi M, Gadamosi A, Yandutse MI. Prevalence and determinants of obesity - a cross-sectional study of an adult Northern Nigerian population. Int Arch Med. 2011;4:10. doi: 10.1186/1755-7682-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Olatunbosun ST, Kaufman JS, Bella AF. Prevalence of obesity and overweight in urban adult Nigerians. Obes Rev. 2011;12:233–41. doi: 10.1111/j.1467-789X.2010.00801.x. [DOI] [PubMed] [Google Scholar]
- 10.Adedoyin RA, Mbada CE, Balogun MO, Adebayo RA, Martins T, Ismail S. Obesity prevalence in adult residents of Ile-Ife, Nigeria. Nig Q J Hosp Med. 2009;19:100–5. [PubMed] [Google Scholar]
- 11.Chigbu C, Aja L. Obesity in pregnancy in southeast Nigeria. Ann Med Health Sci Res. 2011;1:135–40. [PMC free article] [PubMed] [Google Scholar]
- 12.Ezeanochie MC, Ande AB, Olagbuji BN. Maternal obesity in early pregnancy and subsequent pregnancy outcome in a Nigerian population. Afr J Reprod Health. 2011;15:55–9. [PubMed] [Google Scholar]
- 13.Jeremiah I, Nyeche S, Akani C, Akani N. Pregnancy outcome among obese parturients at the University of Port Harcourt Teaching Hospital. J Med Med Sci. 2011;2:1152–6. [Google Scholar]
- 14.Crane JM, White J, Murphy P, Burrage L, Hutchens D. The effect of gestational weight gain by body mass index on maternal and neonatal outcomes. J Obstet Gynaecol Can. 2009;31:28–35. doi: 10.1016/s1701-2163(16)34050-6. [DOI] [PubMed] [Google Scholar]
- 15.Salihu HM, De La Cruz C, Rahman S, August EM. Does maternal obesity cause preeclampsia. A systematic review of the evidence? Minerva Ginecol. 2012;64:259–80. [PubMed] [Google Scholar]
- 16.May R. Prepregnancy weight, inappropriate gestational weight gain, and smoking: Relationships to birth weight. Am J Hum Biol. 2007;19:305–10. doi: 10.1002/ajhb.20572. [DOI] [PubMed] [Google Scholar]
- 17.Sebire NJ, Jolly M, Harris JP, Wadsworth J, Joffe M, Beard RW, et al. Maternal obesity and pregnancy outcome: A study of 287,213 pregnancies in London. Int J Obes Relat Metab Disord. 2001;25:1175–82. doi: 10.1038/sj.ijo.0801670. [DOI] [PubMed] [Google Scholar]
- 18.Meyer BJ, Stewart FM, Brown EA, Cooney J, Nilsson S, Olivecrona G, et al. Maternal obesity is associated with the formation of small dense LDL and hypoadiponectinemia in the third trimester. J Clin Endocrinol Metab. 2013;98:643–52. doi: 10.1210/jc.2012-3481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Allman-Farinelli MA. Obesity and venous thrombosis: A review. Semin Thromb Hemost. 2011;37:903–7. doi: 10.1055/s-0031-1297369. [DOI] [PubMed] [Google Scholar]
- 20.Fyfe EM, Thompson JM, Anderson NH, Groom KM, McCowan LM. Maternal obesity and postpartum haemorrhage after vaginal and caesarean delivery among nulliparous women at term: A retrospective cohort study. BMC Pregnancy Childbirth. 2012;12:112. doi: 10.1186/1471-2393-12-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gardosi J, Madurasinghe V, Williams M, Malik A, Francis A. Maternal and fetal risk factors for stillbirth: Population based study. BMJ. 2013;346:f108. doi: 10.1136/bmj.f108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stothard KJ, Tennant PW, Bell R, Rankin J. Maternal overweight and obesity and the risk of congenital anomalies: A systematic review and meta-analysis. JAMA. 2009;301:636–50. doi: 10.1001/jama.2009.113. [DOI] [PubMed] [Google Scholar]
- 23.Mann JR, McDermott SW, Hardin J, Pan C, Zhang Z. Pre-pregnancy body mass index, weight change during pregnancy, and risk of intellectual disability in children. BJOG. 2013;120:309–19. doi: 10.1111/1471-0528.12052. [DOI] [PubMed] [Google Scholar]
- 24.Rooney BL, Schauberger CW, Mathiason MA. Impact of perinatal weight change on long term obesity and obesity-related illnesses. Obstet Gynecol. 2005;106:1349–56. doi: 10.1097/01.AOG.0000185480.09068.4a. [DOI] [PubMed] [Google Scholar]
- 25.Obi SN, Obute EA. Pregnancy outcome in obese Nigerian. Trop J Obstet Gynaecol. 2004;21:32–5. [Google Scholar]
- 26.Olayemi OO, Umuerri CO, Aimakhu CO. Obstetric performance of Nigerian obese parturients. Trop J Obstet Gynaecol. 2002;19:17–20. [Google Scholar]
- 27.Adesina K, Aderibigbe S, Fawole A, Ijaiya M, Olarinoye A. Pregnancy outcome of the obese in Ilorin. Obstet Med. 2011;4:160–3. doi: 10.1258/om.2011.100081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Panaretto K, Lee H, Mitchel M, Larkins S, Manessis V, Buettner P, et al. Risk factors for preterm, low birth weight and small for gestational age birth in urban Aboriginal and Torres strait Islander women in Townsville. Aust N Z J Public Health. 2006;30:163–70. doi: 10.1111/j.1467-842x.2006.tb00111.x. [DOI] [PubMed] [Google Scholar]
- 29.Ferraz EM, Gray RH, Cunha TM. Determinants of preterm delivery and intrauterine growth retardation in north-east Brazil. Int J Epidemiol. 1990;19:101–8. doi: 10.1093/ije/19.1.101. [DOI] [PubMed] [Google Scholar]
- 30.Cogswell ME, Scanlon KS, Fein SB, Schieve LA. Medically advised, mother's personal target, and actual weight gain during pregnancy. Obstet Gynecol. 1999;94:616–22. doi: 10.1016/s0029-7844(99)00375-0. [DOI] [PubMed] [Google Scholar]
- 31.McDonald SD, Pullenayegum E, Bracken K, Chen AM, McDonald H, Malott A, et al. Comparison of midwifery, family medicine and obstetric patients’ understanding of weight gain during pregnancy: A minority of women report correct counselling. J Obstet Gynaecol Can. 2012;34:129–35. doi: 10.1016/S1701-2163(16)35155-6. [DOI] [PubMed] [Google Scholar]
- 32.McDonald SD, Pullenayegum E, Taylor VH, Lutsiv O, Bracken K, Good C, et al. Despite 2009 guidelines, few women reported being counselled correctly about weight gain in pregnancy. Am J Obstet Gynecol. 2011;205:333e.1–6. doi: 10.1016/j.ajog.2011.05.039. [DOI] [PubMed] [Google Scholar]
- 33.Herring SJ, Henry TQ, Klotz AA, Foster GD, Whitaker RC. Perceptions of low-income African-American mothers about excessive gestational weight gain. Matern Child Health J. 2012;16:1837–43. doi: 10.1007/s10995-011-0930-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Baker PN, editor. Obstetrics by Ten Teachers. 18th ed. London: Bookpower/ELST; 2006. p. 48. [Google Scholar]
- 35.Cunningham FG, Leveno KJ, Bloom SL, Hauth JC, Rouse DJ, Sponge CT, editors. Williams Obstetrics. 23rd ed. New York: Mc GrawHill companies Inc.; 2010. p. 200. [Google Scholar]
- 36.Weight gain during pregnancy: Re-examining the guidelines. Washington: The National Academies Press; 2009. Institute of Medicine. [Google Scholar]
- 37.Olson CM, Strawderman MS. Modifiable behavioural factors in a biopsychosocial model predicting adequate and excessive gestational weight gain. J Am Diet Assoc. 2003;103:48–54. doi: 10.1053/jada.2003.50001. [DOI] [PubMed] [Google Scholar]
- 38.Phelan S, Phipps MG, Abrams B, Darroch F, Schaffner A, Wing RR. Practitioner advice and gestational weight gain. J Womens Health (Larchmt) 2011;20:585–91. doi: 10.1089/jwh.2010.2316. [DOI] [PMC free article] [PubMed] [Google Scholar]


