Abstract
Background:
The anecdotal fear of using cautery for surgical incisions is still common in surgical practice despite recent evidences. The aim of this study is to compare the results of electrocautery and the scalpel in skin incisions.
Materials and Methods:
This is a prospective randomized double blind study conducted in the Department of Surgery, of a teaching hospital in Ibadan. Patients were randomized to have either scalpel or electrocautery incisions. The duration used in making the skin incision; the incisional blood loss and the ensuing length and depth of the wound were noted. Postoperative pain; duration of wound healing and the occurrence of surgical site infection were also noted.
Results:
There were 197 patients consisting of the scalpel group (n = 98) and the electrocautery group (n = 99). The ages ranged from 16 to 73 years. The demography, case distribution and body mass index were similar in both groups. The mode of presentation was predominantly elective. The incision time was shorter in the electrocautery group (P < 0.001). The blood loss was less with the diathermy compared to the scalpel (6.53 ± 3.84 ml vs. 18.16 ± 7.36 ml, P < 0.001). The cumulative numerical rating scale score for pain was 12.65 (standard deviation [SD] 8.06) and 17.12 (SD 9.49) in the diathermy and scalpel groups respectively (P < 0.001). There was no statistically significant difference in wound infection and wound closure (epithelialization time) (P = 0.206).
Conclusion:
The use of electrocautery in making skin incision is associated with reduced incision time, incisional blood loss, and postoperative pain.
Keywords: Diathermy, electrocautery, general surgery, surgical incision
INTRODUCTION
Despite the introduction of electrocautery (diathermy) about a century ago,[1,2] it is still used mostly for underlying dissection and hemostasis.[3] Skin incisions with electrocautery are not frequent because of the fear of deep burns; poor wound healing and excessive scarring.[4] These presumptions stem from experimental and clinical studies that yielded varied reports.[5,6,7]
Modern electrosurgical units capable of delivering pure sinusoidal currents have evolved a change in this concept. The advantages are rapid hemostasis, faster dissection, and a reduced overall operative blood loss.[4,8,9] Majority of studies had compared electrocautery and scalpel incision in terms of wound infection, postoperative pain, blood loss, duration of healing and postoperative wound complication in only selected groups of patients with the exclusion of patients with medical co-morbidities.[4,5,6,7,8,9,10,11] No study till date has focused on a heterogeneous population of general surgical cases in native Africans.
This study compared electrocautery and scalpel incisions in patients with varied general surgery conditions. The indices observed were the incision time, incisional blood loss, postoperative pain, wound healing and postoperative wound infection. The safety of diathermy in our environment was also considered.
MATERIALS AND METHODS
This prospective randomized clinical study was conducted in the Department of Surgery, of a teaching hospital in Ibadan Nigeria between March 2011 and February 2012. The hospital is a referral center located in South-western Nigeria. An approval was obtained from the hospital ethics committee.
All patients admitted through the accident and emergency department and surgical out-patient department for surgery were eligible for the study. Consenting patients for surgery were further categorized as being clean or clean contaminated.
All consenting patients within the inclusion criteria were consecutively enrolled in the study. Block randomization was used for allocation of patients into two groups (A and B). The whole process of generation and implementation of randomization was done by a surgeon who could not be blinded to which modality was to be used for making the incision. The patient and the assessor of the pain score (intern) were both blinded to which participant had scalpel or diathermy skin incision at surgery. All consenting patients within the inclusion criteria were consecutively enrolled in the study. Block randomization was used for allocation of patients into two groups (A and B). The whole process of generation and implementation of randomization was done by a surgeon who could not be blinded to which modality was to be used for making the incision. The patient and the assessor of the pain score (intern) were both blinded to which participant had scalpel or diathermy skin incision at surgery. All the surgeons were of consultant and senior registrar grade.
The exclusion criteria were patients <15 years, contaminated and dirty procedures and patients who could not comprehend the pain scoring index for assessing postoperative pain either due to an altered sensorium or communication barrier.
All consenting patients within the inclusion criteria were consecutively enrolled in the study.
The patient and the assessor of the pain score (intern) were both blinded to which participant had scalpel or diathermy skin incision at surgery.
A total of 197 patients was recruited into the study. In group A; 99 patients had diathermy skin incision while 98 patients in group B had conventional scalpel skin incision. Group A patients had a surgical incision made with force two valley lab diathermy machine in cutting mode, power of 5W and 515 kHz sinusoidal waveform while group B patients had surgical incision made with surgical blade. Prophylactic intravenous antibiotics were administered at induction of anesthesia. This was ceftriaxone alone or in combination with metronidazole when indicated. The prophylactic antibiotics were repeated for 72 h in clean-contaminated procedures. It was administered in the prophylactic setting for the clean procedures; hence it was not repeated in this cohort. The surgical incision in each case was made through skin, subcutaneous tissue, deep fascia, muscle ± aponeurosis and peritoneum or the proposed operation site. The length and depth of each incision were measured using a sterile flexible ruler and the incision time was defined as the start of the skin incision till the intended operation site was reached with complete hemostasis and incisional blood loss being the blood loss that occurred strictly during the period of skin incision and this was calculated as the differences between the dry and wet weight of the swabs (1 mg = 1 ml). No suction evacuation of blood was done while making the skin incision.
Postoperative analgesia was administered via the intravenous route using Tramadol hydrochloride for all patients on admission, and its oral form was used in day case surgery after an initial parenteral dose. The pain assessment was done by surgical interns at fixed times on postoperative days 1, 2 and 3 using the verbal, numerical rating scale to assess the level of pain. The day case respondents were called on the phone to assess their postoperative pain.
Postoperative wound assessment both for healing and surgical site infection were assessed concurrently on the first 5 postoperative days and then at appointed times depending on the site of surgery. The presence of a healing ridge with adequate tensile strength was used as an index of a healing wound while the Southampton grading system was used to denote the presence or absence of an infection. The peri-operative occurrence of any adverse reaction or event whilst using the electrocautery machine was noted at surgery.
The follow-up schedule included a review at the 4th, 8th and 12th week respectively postoperation. The findings from the patient's history, examination, body mass index (BMI), co-morbidities, laboratory reports, imaging reports, operative and postoperative course were all recorded in the pro-forma. Ethical approval was obtained for the study. Statistical data analysis was done using SPSS version 17 manufactured by IBM, Chicago.
Frequencies and proportions were used to summarize the variables while Chi-square and Student's t-test were used to test for association at 5% level of significance.
RESULTS
A total of 334 patients was eligible for inclusion in the study during the period. Of these, 137 patients were excluded from the study due to failure to meet the inclusion criteria. Thus, 197 patients were enrolled over the 1-year period.
Figure 1 shows a summary of patient's recruitment. There were no significant demographic differences between the two groups. We had a total of 88 male and 109 females with a male: Female ratio of 1:1.3. Their ages ranged from 16 to 73 years with a mean of 46 ± 14.9 years. Group A consisted of 99 patients (44 men and 55 women, mean age-46 years [standard deviation (SD)-13.91; range 16–73 years]) and group B included 98 patients (42 men and 56 women; mean age 45 years [SD-15.99; range 13–70 years]). In group A, 24 (24.2%) patients had medical co-morbidities while 27 (27.5%) patients in group B had associated medical co-morbidities. The mean overall weight was 68.71 kg (SD-16.56), while the BMI for groups A and B were 24.66 (SD-7.83) and 25.17 (SD-5.80) kg/m2 respectively which was not statistically significant.
Figure 1.
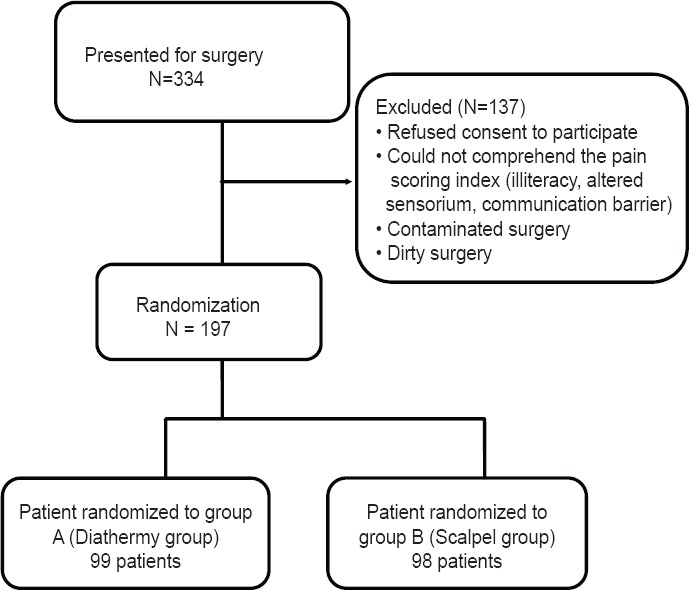
Summary of patients’ recruitment
Table 1 shows the patient characteristics. In the diathermy group; 83 patients underwent elective procedures, and 16 patients had emergency procedures whilst in the scalpel arm 88 patients underwent elective procedures, and 10 patients had emergency procedures. The distribution of surgical cases was similar in both groups. Table 2 shows the distribution of frequency of surgery and anatomic site for each group. A total of 164 (83.2%) patients presented for care via the surgery out-patient department while 33 (16.8%) patients were admitted through the accident and emergency department. The predominant mode of anesthesia was general anesthesia in 157 (79.8%) patients. Local anesthesia and spinal anesthesia were used in 27 (13.5%) and 15 (5.7%) respectively. Parenteral analgesia was administered in 94% of patients; while the rest had oral analgesia. Although there was no statistical difference between the length (P = 0.570) or depth (P = 0.952) of incision in both groups, the incision time (P = 0.001) and incisional blood loss (P = 0.011) were significantly higher in group B patients (who had scalpel incisions). The cumulative numerical rating scale score was lower in group A than in group B (12.65 ± 8.06 vs. 17.12 ± 9.49, P = 0.001).
Table 1.
Patient characteristics in the two groups (n=197)
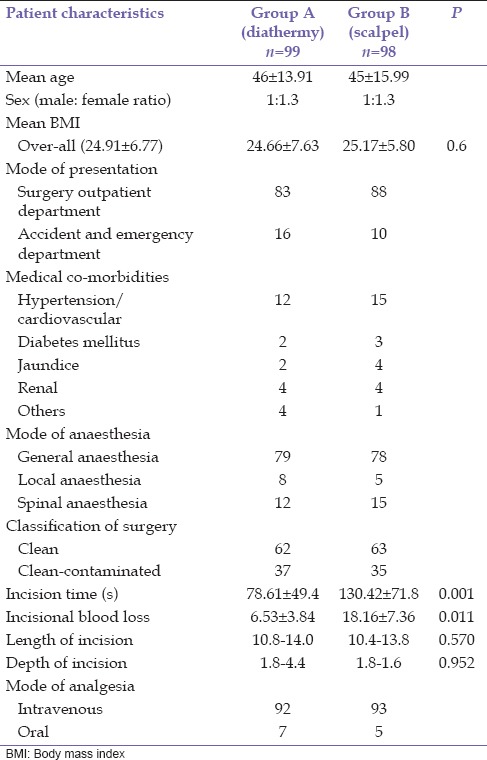
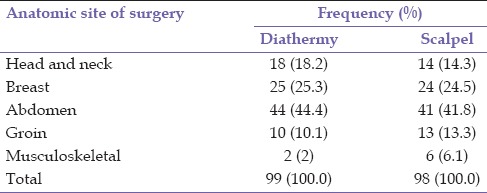
Table 2.
Distribution of anatomic sites for diathermy and scalpel
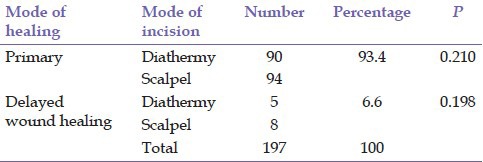
The wound healing time was comparable in both groups of patients with a delay in wound healing occurring in 5 (5.1%) patients in group A and 8 (8.1%) patients in group B. A total of 20 (10.4%) patients had wound infection with a similar prevalence in both groups (P = 0.206).
Table 3a and b shows the statistical analysis of the outcome variables.
Table 3a.
Distribution of frequency of wound infection in anatomic sites
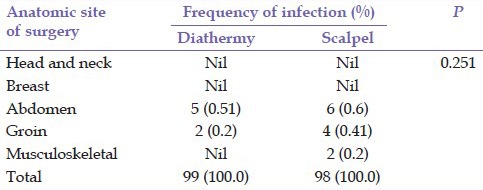
Table 3b.
The mode of healing in relation to the mode of incision
DISCUSSION
Several studies have shown that diathermy is increasingly being used for making skin incisions, securing hemostasis, dissecting tissue planes and cutting.[4,6,7,12] It facilitates hemostasis, reduces overall intraoperative time and lastly produce a wound that heals similarly as one created by the scalpel.[4] Despite these advantages; its use by surgeons for skin incisions in centers in developing countries including ours is still sub-optimal. We can allude to the paucity of studies involving a heterogeneous group of patients in this part of the world as the cause along with the old belief that electrocautery causes electric burns when used to make skin incisions, thus increasing the amount of devitalized tissue within the wound.
Mastectomy for breast carcinoma (25%) accounted for the highest proportion of procedures performed in both groups. This is consistent with the increased awareness and hospital presentation with subsequent management of the disease. Herniorrhaphy for groin hernias and thyroidectomy for simple multinodular goiter followed thereafter for both groups respectively. This is in slight contrast to a previous study[3] which had more of open cholecystectomy for cholelithiasis (16.2%) followed by herniorrhaphy for groin hernia (14.7%). This can be explained by the sub-specialty of the surgical divisions and also regional variations in the epidemiology of the disease.
Slightly over a quarter (28.6%) of our patients had co-morbidities, with hypertension ranking highest; comparable with other authors.[13,14,15] Our study along with various other studies showed a significantly shorter incision time in the diathermy group compared with the scalpel group. This is in contrast to the review by a previous studym,[16] which suggested no added advantage with diathermy skin incision in terms of the incision time. The reduced incisional blood loss in the diathermy group is in concordance with the findings in a similar study.[10] There was only a slight difference in volume. The mean blood loss in the diathermy group was 1.53 ± 3.84 ml whilst theirs[10] was 1.43 ± 0.201 ml. This is due to the coagulative effect of diathermy on the micro-circulation of the area immediately adjoining the area of the incision.
In accordance with previous studies,[4] our results suggested a significantly reduced postoperative pain in the diathermy group. This is due to the thermal effect of diathermy on the sensory nerve fibers with the subsequent disruption of transmission of nerve impulses. Cell vaporization caused by the application of a pure sinusoidal current leads to immediate tissue and nerve necrosis without significantly affecting adjoining structures. Consequently, there is total or partial injury to the cutaneous nerves in the area of the surgical wound with a reduced postoperative pain profile in patients who had diathermy skin incisions.[17] We however did not compare the postoperative pain with the various sites of surgery because the varied anatomic sites, along with the various amounts of underlying tissue dissection and inherent class of surgery may all affect the pain assessment score. This is a one of the limitations of this study.
Although our wound infection rate compared favorably with an initial study,[6] it was higher when compared with 5% in a more recent study.[10] The conclusion was that it was not statistically significant. The overall outcome in this study in terms of early and late wound complications is comparable with other similar studies.[12,17]
The mean duration for complete wound healing was similar for both groups. This is similar to initial studies.[3] There was no adverse effect noted during the course of our study attributable to the use of diathermy.
CONCLUSION
The use of diathermy for skin incisions in our local population is associated with reduced incisional blood loss, incisional time, and postoperative pain. It has no effect on wound closure (epithelialization) and is not associated with any delay in wound healing. It has been adjudged safely in this study if deployed in the proper way and manner with little or no side effect.
Footnotes
Source of Support: Nil
Conflicts of Interest: None declared.
REFERENCES
- 1.Wicker P. Electrosurgery - Part I. The history of diathermy. NATNEWS. 1990;27:6–7. [PubMed] [Google Scholar]
- 2.Memon MA. Surgical diathermy. Br J Hosp Med. 1994;52:403–8. [PubMed] [Google Scholar]
- 3.Shamim M. Diathermy vs. scalpel skin incisions in general surgery: Double-blind, randomized, clinical trial. World J Surg. 2009;33:1594–9. doi: 10.1007/s00268-009-0064-9. [DOI] [PubMed] [Google Scholar]
- 4.Kearns SR, Connolly EM, McNally S, McNamara DA, Deasy J. Randomized clinical trial of diathermy versus scalpel incision in elective midline laparotomy. Br J Surg. 2001;88:41–4. doi: 10.1046/j.1365-2168.2001.01625.x. [DOI] [PubMed] [Google Scholar]
- 5.Soballe PW, Nimbkar NV, Hayward I, Nielsen TB, Drucker WR. Electric cautery lowers the contamination threshold for infection of laparotomies. Am J Surg. 1998;175:263–6. doi: 10.1016/s0002-9610(98)00020-8. [DOI] [PubMed] [Google Scholar]
- 6.Groot G, Chappell EW. Electrocautery used to create incisions does not increase wound infection rates. Am J Surg. 1994;167:601–3. doi: 10.1016/0002-9610(94)90106-6. [DOI] [PubMed] [Google Scholar]
- 7.Hussain SA, Hussain S. Incisions with knife or diathermy and postoperative pain. Br J Surg. 1988;75:1179–80. doi: 10.1002/bjs.1800751211. [DOI] [PubMed] [Google Scholar]
- 8.Chalya PL, Mchembe MD, Mabula JB, Gilyoma JM. Diathermy versus scalpel incision in elective midline laparotomy: A prospective randomized controlled clinical study. East and Cent. Afr J Surg. 2013;18:71–7. [Google Scholar]
- 9.Kumar V, Tewari M, Shukla HS. A comparative study of scalpel and surgical diathermy incision in elective operations of head and neck cancer. Indian J Cancer. 2011;48:216–9. doi: 10.4103/0019-509X.82904. [DOI] [PubMed] [Google Scholar]
- 10.Arsalan S, Muhammad F, Athar AS, Sohail R. Elective midline laparotomy; comparison of diathermy and scalpel incisions. Prof Med J. 2011;18:106–11. [Google Scholar]
- 11.Ozdogan M, Yilmaz KB, Ozaslan C, Gurer A, Gulbahar O, Ersoy E. Scalpel versus electrocautery dissection: The effect on wound complication and pro inflammatory cytokines levels in wound fluid. Turk J Med Sci. 2008;38:111–6. [Google Scholar]
- 12.Franchi M, Ghezzi F, Benedetti-Panici PL, Melpignano M, Fallo L, Tateo S, et al. A multicentre collaborative study on the use of cold scalpel and electrocautery for midline abdominal incision. Am J Surg. 2001;181:128–32. doi: 10.1016/s0002-9610(00)00561-4. [DOI] [PubMed] [Google Scholar]
- 13.Maggio C, Bonzano A, Conte E, Libertucci D, Panarelli M, Bobbio M, et al. Preoperative evaluation in non-cardiac surgery: Cardiac risk assessment. Qual Assur Health Care. 1992;4:217–24. doi: 10.1093/oxfordjournals.intqhc.a036722. [DOI] [PubMed] [Google Scholar]
- 14.Wolfsthal SD. Is blood pressure control necessary before surgery? Med Clin North Am. 1993;77:349–63. doi: 10.1016/s0025-7125(16)30256-5. [DOI] [PubMed] [Google Scholar]
- 15.Dixon AR, Watkin DF. Electrosurgical skin incision versus conventional scalpel: A prospective trial. J R Coll Surg Edinb. 1990;35:299–301. [PubMed] [Google Scholar]
- 16.Telfer JR, Canning G, Galloway DJ. Comparative study of abdominal incision techniques. Br J Surg. 1993;80:233–5. doi: 10.1002/bjs.1800800238. [DOI] [PubMed] [Google Scholar]
- 17.Chrysos E, Athanasakis E, Antonakakis S, Xynos E, Zoras O. A prospective study comparing diathermy and scalpel incisions in tension-free inguinal hernioplasty. Am Surg. 2005;71:326–9. doi: 10.1177/000313480507100410. [DOI] [PubMed] [Google Scholar]


