Abstract
Context:
The Darning technique of inguinal hernia repair is a tissue-based technique with documented low recurrence rate in some parts of the world. Though practiced in our setting, little is documented on its outcome.
Aims:
The aim was to review the outcome of Darning technique of inguinal hernia repair in our setting.
Study Design:
A descriptive retrospective study.
Patients and Methods:
Clinical records of all patients who had inguinal hernia repair using the Darning technique between January 2007 and December 2011 in our institution were obtained. Details of sociodemographic data, intraoperative findings and postoperative complications were reviewed.
Statistical Analysis Used:
simple frequencies, proportions and cross-tabulations.
Results:
A total of 132 patients whose ages ranged from 15 to 84 years (mean = 49.4 years) with a male: female ratio of 12:1 were studied. Majority of the hernias were right sided (68.9%), mostly indirect (81.8%). The procedures were for emergencies in 17 (12.9%) cases whereas the rest (87.1%) were done electively. Most procedures, 110 (83.3%) were performed under local anesthesia. Surgical site infection was the most common complication occurring in six patients (4.5%), while four patients (3%) had chronic groin pain. At a mean follow-up period of 15 months there were two recurrences (1.5%) both occurring in patients with bilateral hernias (P = 0.001).
Conclusions:
The Darning technique of inguinal hernia repair is a safe and effective method for inguinal hernia repair in our setting.
Keywords: Darning, hernia, inguinal
INTRODUCTION
Inguinal hernia repair has undergone several modifications since the description of the Bassini technique.[1] The various techniques described are aimed at improving outcome, particularly recurrence rate. The underlying factor identified as a cause of recurrence in most of these methods of repair is the fraying and tearing of the fibers of the inguinal ligament due to the significant amount of tension associated with them.[2] Darning technique first introduced by Abrahamson and popularized by Moloney is considered to be a relatively tension free through tissue based method of repair. It entails approximation of the inguinal ligament to the conjoint tendon with monofilament nylon beginning from the pubic tubercle to the internal ring and back to the pubic tubercle without forcibly bringing the tissues together with the sutures forming a weave in the posterior wall of the inguinal canal.[3,4]
Studies evaluating the Darning technique have shown satisfactory outcomes in terms of recurrence and other postoperative complications. Some of these are comparable to Lichtenstein technique of inguinal hernia repair,[5,6] which is currently the gold standard of open inguinal hernia repair. In most parts of sub-Saharan Africa, studies on inguinal hernia repair using nonprosthetic methods are based on the less acceptable Bassini technique with very few reports on other tissue-based methods such as the Darning technique.[7] Although, the use of mesh for inguinal hernia repair is now gaining acceptance in our setting, nonprosthetic methods still find relevance in emergency presentations such as obstruction or strangulation, which are not uncommon modes of presentation,[8,9] and in many hospitals where the experience with mesh repair is limited. In such instances, tissue-based repair methods with acceptable recurrence rate will be ideal.
This study aims to present our experience with the use of the Darning technique for repair of inguinal hernia in a Nigerian tertiary hospital.
PATIENTS AND METHODS
The study is a retrospective descriptive study conducted in the Ife Hospital Unit of the Obafemi Awolowo University Teaching Hospitals Complex Ile-Ife, Osun state, Nigeria. The hospital is a tertiary health facility serving the largely agrarian semi-urban communities of adjoining parts of Osun, Ondo, Oyo and Ekiti states in South-West, Nigeria.
Records of all patients who had inguinal hernia repair between January 2007 and December 2011 were obtained using the operation registers and case files, and only those whose method of repair was stated in their records were reviewed. Those whose hernias were repaired using the Darning technique were then selected for further review. Details of their sociodemographic features (age, sex and occupation), hernia characteristics (hernia type and extent), operative details (method of anesthesia, lead surgeon and duration of operation) and postoperative outcome were obtained. Postoperative outcome measures included hematoma, surgical site infection, hydrocele, chronic groin pain and recurrence. Chronic groin pain was defined in this study as the documentation of groin pain in the patients’ follow-up records beyond 3 months after surgery. Information regarding these outcome measures was based on documentation in the case notes during follow-up clinic visits. Statistical analysis was performed using SPSS version 22. Data were expressed as frequencies and proportions with some of these presented as tables and charts. Cross-tabulations were done to compare the relationship between recurrence and other variables. Pearson's Chi-square test was done to determine the level of statistical significance while Fisher's test was used in its place when the cases in each cell were <5. Statistical significance was set at a P < 0.05.
RESULTS
A total of 404 patients had inguinal hernia repair during the study period. Of these, 257 patients whose methods of repair were stated in the records were reviewed. Darning technique was used in 132 cases (51.4%), Lichtenstein mesh repair was done in 85 cases (33%) while Bassini technique was employed in the remaining 40 cases (15.6%). Further analysis of the 132 patients who had Darning repair showed an age range of 15–84 years with a mean age of 49.4 years [Figure 1]. There were 122 males and ten females with a male: Female ratio of 12:1. Majority of the hernias were on the right side (91, 68.9%), left sided hernias were 35 (26.5%) while 6 cases (4.5%) were bilateral. Most of the hernias were inguinal (79, 59.8%), while 53 (40.2%) presented at the inguino-scrotal stage. Majority were primary hernia repairs 125 (94.7%) while there were 7 cases of recurrent hernia. One hundred and fifteen cases (87.1%) had reducible hernias while 17 cases (12.9%) presented with irreducible hernias requiring emergency operations.
Figure 1.
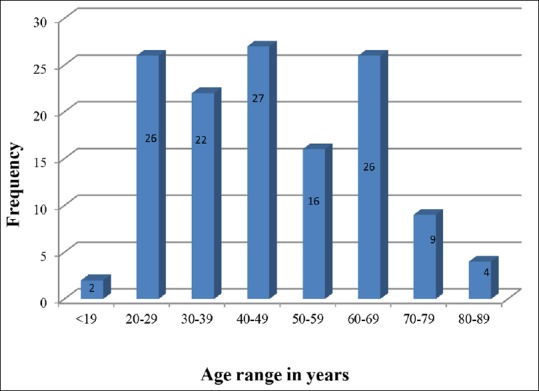
Age distribution
The type of hernia was characterized at surgery, revealing 108 indirect hernias (81.8%) while 22 were direct (16.7%), 2 patients (1.5%) had pantaloon hernia. Surgeries were performed by senior registrars and registrars as lead surgeons under the supervision of the unit consultant general surgeons in most cases (108, 81.8%) while 24 cases (18.2%) were performed by Consultant general surgeons. One hundred and ten patients (83.3%) were operated under local anesthesia, 15 patients (11.4%) had general anesthesia, while 7 patients (5.3%) had their hernias repaired under spinal anesthesia. The mean duration of operation was 68 min. Majority, 113 (85.6%) were done as day cases while 19 patients (14.6%) required hospital admission.
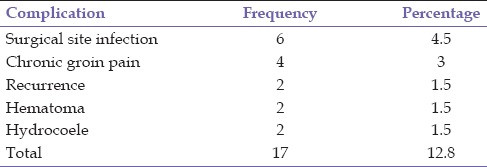
Regarding outcome, surgical site infection was the most common complication recorded, occurring in 6 patients (4.5%). These occurred both in emergency and elective cases with no statistically significant difference between the two (P > 0.05). Four patients had chronic groin pain (3%) while 2 patients (1.5%) had recurrences at a mean duration of follow-up of 15 months ranging from 2 weeks to 6 years [Table 1]. Both patients with recurrences had simultaneous repair of bilateral inguinal hernias. This association was found to be statistically significant (P = 0.001, odd ratio of 32 and confidence interval 12–85). One of the recurrences was unilateral while the other was bilateral. The surgeries were also performed by junior registrars in both instances, although this was not found not to be statistically significant. Preoperative straining, smoking, and obesity were not significantly associated with recurrence in this study. There was no peri-operative mortality.
Table 1.
Postoperative complications
DISCUSSION
The various techniques of inguinal hernia repair can be broadly classified into tissue-based and prosthetic methods. One major drawback of the tissue based repairs has been the amount of tension associated with most of them which is an important factor implicated in recurrence.[10] Though tissue based, the Darning technique is believed to have an advantage over many other nonprosthetic techniques being relatively tension free as the posterior wall is repaired without forcefully apposing the tissues. Rather, sutures are passed in a continuous fashion forming a weave in the posterior wall. This method of repair is more common in the United Kingdom and some other English speaking countries where most of the studies on this technique have been conducted.[11]
In sub-Saharan Africa, studies on inguinal hernia repair lack variety with regards to the techniques used. Except for a few mentions of the Darning technique,[12] most are based on the Bassini method of repair that is no longer recommended due to its relatively high recurrence rate. This fact was also observed by Yeboah in his review of inguinal hernia disease in Africa.[7] Our study thus highlights the practice of inguinal hernia surgery in a Nigerian teaching hospital using the Darning technique.
Our findings with regards to sociodemographic features and hernia characteristics are consistent with what has been documented in previous studies.[13] We however observed a reduction in the number of cases presenting with complications, our record of 12.9% shows a reduction from what has been previously documented in studies in a similar setting where up to a quarter of hernias seen presented with complications.[9] This may be a reflection of improvement in availability and accessibility of health care facilities and also an improvement in public enlightenment. More still needs to be done however as the number of patients presenting with inguino-scrotal hernia (37%) still suggests delay in presentation.
In a largely agrarian population like ours where occupations with manual labor is common, both the development and progression of groin hernias will be common. We hope to engage in effective health communication interventions at community level in conjunction with our community health physicians to promote early presentation of abdominal hernias thereby reducing the incidence of complications in our patients.
There were 7 cases of recurrent hernia that had a repair in the study. These all had their primary hernia repaired in different centers by the Bassini method attesting to the high recurrence rate that may attend Bassini method. We repaired these cases by the Darning method due to the nonavailability of mesh in our center at the time corresponding to the first 2 years of this study. Other recurrent hernias seen in the later part of this study were repaired with prosthetic mesh that is the recommended technique in such instances.[14]
The Darning technique has been acclaimed to have the advantage of a short learning curve particularly when compared with other popular nonprosthetic methods of repair such as the Shouldice technique.[15] The fact that most of the cases were performed by resident doctors with majority of them carried out under local anesthesia is a testimony to this fact. The procedure can, therefore, be learned by those who perform hernia repair in many secondary level public healthcare facilities as well as those in private settings many of who continue to practice only the Bassini method.
Chronic groin pain is currently considered an important outcome measure following inguinal hernia repair particularly as it affects the quality of life. It is defined as any visual analog score above zero, which lasts for more than 3 months.[16] The 3% chronic groin pain rate recorded in this study compares well with the work of Courtney et al. who also reported a chronic groin pain rate of 3% in a population-based study of over 5,000 patients who had undergone inguinal hernia repair.[17]
A recurrence rate of 1.5% recorded compares with previous studies that recorded values in the range of 0.6–4%.[5,18,19] This is much lower than the 10% recurrence rate recorded following Bassini technique in some series and comparable to the 1% recurrence rate following Lichtenstein mesh repair.[2,6] A longer follow-up period may however reveal a higher recurrence rate than what we noted in this study. A statistically significant relationship between bilaterality and recurrence was quite notable in our study. It was found that patients with bilateral inguinal had a 32 fold risk of developing recurrence when compared with those unilateral hernias. It remains to be determined however whether this is directly related to the technique or unidentified patient-related factors. Patients with undetected bladder outlet obstruction or unidentified connective tissue disorders, for instance, may be predisposed to developing multiple hernias and if this is not taken into consideration prior to surgery may also account for recurrences. Thus, patients with bilateral hernias should be evaluated thoroughly for possible underlying factors that may predispose to recurrence. Such may also be considered for mesh repair as recommended by some authors.[20]
CONCLUSION
Inguinal hernia repair using the Darning technique is a safe and effective method of inguinal hernia repair. We recommend its adoption over the traditional Bassini repair for nonprosthetic repair of inguinal hernia in our setting. A prospective study comparing Darning with the standard Lichtenstein repair in our setting is also recommended.
ACKNOWLEDGMENTS
Our appreciations go to Prof. DO Akinola, Prof. OO Lawal, Prof. ARK Adesunsanmi, and Dr. OI Alatise whose patients were included in the study.
Footnotes
Source of Support: Nil
Conflicts of Interest: None declared.
REFERENCES
- 1.Bekker J, Keeman JN, Simons MP, Aufenacker TJ. A brief history of the inguinal hernia operation in adults. Ned Tijdschr Geneeskd. 2007;151:924–31. [PubMed] [Google Scholar]
- 2.Zsolt B, Csíky M. Recurrence rate in Bassini operation after five years. Magy Seb. 2001;54:307–8. [PubMed] [Google Scholar]
- 3.Abrahamson J. Hernias. In: Zinner MJ, editor. Maingot's Abdominal Operations. 10th ed. Conneticut: Appleton and Lange; 1997. pp. 479–580. [Google Scholar]
- 4.Moloney GE. Darning inguinal hernias. Arch Surg. 1972;104:129–30. doi: 10.1001/archsurg.1972.04180020009001. [DOI] [PubMed] [Google Scholar]
- 5.Farooq O, Batool Z, Bashir-ur-Rehman Prolene Darn: Safe and effective method for primary inguinal hernia repair. J Coll Physicians Surg Pak. 2005;15:358–61. [PubMed] [Google Scholar]
- 6.EU Hernia Trialists Collaboration. Laparoscopic compared with open methods of groin hernia repair: Systematic review of randomized controlled trials. Br J Surg. 2000;87:860–7. doi: 10.1046/j.1365-2168.2000.01540.x. [DOI] [PubMed] [Google Scholar]
- 7.Ohene-Yeboah M, Abantanga FA. Inguinal hernia disease in Africa: A common but neglected surgical condition. West Afr J Med. 2011;30:77–83. [PubMed] [Google Scholar]
- 8.Mbah N. Morbidity and mortality associated with inguinal hernia in Northwestern Nigeria. West Afr J Med. 2007;26:288–92. doi: 10.4314/wajm.v26i4.28329. [DOI] [PubMed] [Google Scholar]
- 9.Adesunkanmi AR, Agbakwuru EA, Badmus TA. Obstructed abdominal hernia at the Wesley Guild Hospital, Nigeria. East Afr Med J. 2000;77:31–3. doi: 10.4314/eamj.v77i1.46371. [DOI] [PubMed] [Google Scholar]
- 10.Abrahamson J. Etiology and pathophysiology of primary and recurrent groin hernia formation. Surg Clin North Am. 1998;78:953–72. doi: 10.1016/S0039-6109(05)70364-9. vi. [DOI] [PubMed] [Google Scholar]
- 11.Morgan M, Reynolds A, Swan AV, Beech R, Devlin HB. Are current techniques of inguinal hernia repair optimal? A survey in the United Kingdom. Ann R Coll Surg Engl. 1991;73:341–5. [PMC free article] [PubMed] [Google Scholar]
- 12.Agbakwuru EA, Olabanji JK, Alatise OI, Katung IA, Onakpoya UU. Single versus two layer suturing for wound closure after inguinal hernia repair. Niger J Clin Pract. 2009;12:162–4. [PubMed] [Google Scholar]
- 13.Arowolo OA, Agbakwuru EA, Adisa AO, Lawal OO, Ibrahim MH, Afolabi AI. Evaluation of tension-free mesh inguinal hernia repair in Nigeria: A preliminary report. West Afr J Med. 2011;30:110–3. [PubMed] [Google Scholar]
- 14.Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J, et al. European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia. 2009;13:343–403. doi: 10.1007/s10029-009-0529-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thapar V, Rao P, Deshpande A, Sanghavi B, Supe AN. Shouldice's herniorrhaphy versus Moloney's darn herniorrhaphy in young patients (a prospective randomised study) J Postgrad Med. 2000;46:9–12. [PubMed] [Google Scholar]
- 16.Classification of chronic pain. Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the International Association for the Study of Pain, Subcommittee on Taxonomy. Pain Suppl. 1986;3:S1–226. [PubMed] [Google Scholar]
- 17.Courtney CA, Duffy K, Serpell MG, O’Dwyer PJ. Outcome of patients with severe chronic pain following repair of groin hernia. Br J Surg. 2002;89:1310–4. doi: 10.1046/j.1365-2168.2002.02206.x. [DOI] [PubMed] [Google Scholar]
- 18.El-Bakry AA. Plication darn for the repair of inguinal hernia. A university hospital experience. Saudi Med J. 2002;23:1347–9. [PubMed] [Google Scholar]
- 19.Koukourou A, Lyon W, Rice J, Wattchow DA. Prospective randomized trial of polypropylene mesh compared with nylon darn in inguinal hernia repair. Br J Surg. 2001;88:931–4. doi: 10.1046/j.0007-1323.2001.01818.x. [DOI] [PubMed] [Google Scholar]
- 20.Amid PK, Shulman AG, Lichtenstein IL. Simultaneous repair of bilateral inguinal hernias under local anesthesia. Ann Surg. 1996;223:249–52. doi: 10.1097/00000658-199603000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]


