Abstract
Background:
Cervical cancer is the second most common cancer among women worldwide and is the leading cause of deaths in developing countries. Despite the strong evidence that cervical cancer screening results in decreased mortality from this disease, the uptake for cervical screening among Jamaican women remains low.
Aims:
This study was carried out to identify factors associated with Jamaican women's decisions to screen for cervical cancer.
Materials and Methods:
Cross-sectional descriptive study of 403 women aged 19 years and older from Portland, Jamaica. An interviewer-administered questionnaire assessed the women's cervical cancer screening history, as well as their knowledge, attitudes, and practices regarding the disease and screening.
Results:
Of the 403 women interviewed, 66% had a Papanicolaou (Pap) smear and only 16% had a Pap test within the past year. Significant predicators of uptake of screening were being married, age, parity, discussing cancer with health provider, perception of consequences of not having a Pap smear, and knowing a person with cervical cancer. Women who did not know where to go for a Pap smear were 85% less likely to have been screened (prevalence odds ratio (POR): 0.15, 95% confidence interval (CI): 0.04, 0.52).
Conclusions:
This study showed suboptimal uptake of cervical cancer screening among Jamaican women. Multipronged approaches are needed to address barriers to screening, as well as identify and support conditions that encourage women's use of reproductive health services, thereby reducing incidence and mortality rates from cervical cancer.
Keywords: Cervical cancer, Cervical screenings, Health systems, Jamaica, Pap smears
Introduction
Cervical cancer is a significant public health burden in most developing countries, where it is a major cause of mortality and morbidity among women.[1] Despite the availability of free Papanicolaou (Pap) smear screening, cervical cancer is the second leading cause of cancer-related deaths among women in Jamaica.[2] There is strong evidence that suggests that cervical cancer screening results in decreased mortality from this disease.[3,4,5,6] However, literature suggests that the uptake for cervical screening for Jamaican women remains low.[7,8,9,10] In fact, about 90% of Jamaican women who die from cervical cancer had never been screened.[11]
According to the World Health Organization (WHO), the highest burden of cervical cancer occurs in developing nations, where there is a lack of effective screening programs and low uptake of Pap smear or pelvic examination (WHO).[1] Countries in the Caribbean region with the highest cervical cancer mortality rates are Haiti (48.1 per 100,000), Barbados (16.5 per 100,000), and Jamaica (17.4 per 100,000).[2] The mortality rate for cervical cancer in Jamaica is 6.6 times more than that for Caucasian females in the USA, and 2.8 times more than that for African-American females.[9]
Cervical cancer is almost always caused by the human papillomavirus (HPV) infection.[3,12] There are many serotypes of the virus and many are spread by sexual transmission. While most HPV infections are transient and do not cause disease, persistent infections with certain “high risk” strains, such as HPV 16, 18, 31, 33, 34, 45, 52, and 58 are responsible for approximately 90% of all cervical cancer cases worldwide.[3,12,13]
Although cervical cancer screening programs are free of charge and widely available in the Jamaican public health sector, HPV deoxyribonucleic acid (DNA) testing is currently only available through private health services.[2] HPV prevalence studies conducted in Jamaica have found high HPV prevalence ranging from 54 to 87% and highest among women who were single, young (16-19 years), and had had more than three sexual partners in their lifetime.[14,15] Despite high prevalence rates of HPV infection among Jamaican women, Jamaica is currently one of a few Caribbean countries that does not have a national HPV vaccine immunization program.[2]
Known risk factors for cervical cancer include early coital debut, large number of pregnancies, unprotected sex, multiple sex partners, partners with other concurrent partners, sexually-transmitted infections, use of oral contraceptives, family history of cervical cancer, smoking, and immunosuppression including human immunodeficiency virus (HIV) infection.[16] Research shows that most Jamaican women have high risk factors for cervical cancer including high prevalence rates of sexually-transmitted infections including HPV,[14,15] early onset of sexual activities, high parity, inconsistent use of condoms, and partners with other concurrent partners.[9,10] Thus, it is crucial to increase the uptake of cervical cancer screening practices among these high risk women.
Cervical cancer can often be found early, and sometimes even prevented entirely, by having regular Pap smears. If detected early, cervical cancer is one of the most successfully treatable cancers.[16] Evidence shows that early detection through cervical Pap smears has had a significant impact on the incidence and mortality associated with this cancer in many developed nations including the United States, United Kingdom, and Australia.[3,4,5,6] This success has been attributed to greater access to healthcare, increased uptake of cervical screening, and increased awareness of screening practices among women in these developed nations.[3,4,5] On the other hand, screening activities in many developing nations including Jamaica have failed to reverse cervical cancer incidence and mortality due to low uptake and follow-up of screening.[7,8,9,10,17,18,19,20,21]
Cervical cancer burden is projected to increase significantly in the Caribbean region in spite of the availability of Pap screening in most Caribbean countries.[22] Prior research in Latin America and the Caribbean has shown several factors that are thought to affect the uptake of Pap tests. These factors include health system factors such as access to testing facilities and service delivery, and personal factors such as lower socioeconomic status, lack of knowledge about cervical cancer screening, low perceived risk of disease, fear of cervical cancer diagnosis, fear of pain, and embarrassment.[7,9,10,22,23] A study by Bessler et al.,[7] in Jamaica also found that annual visits to a healthcare provider and provider recommendation influenced uptake of cervical cancer screening.
The objectives of this study were to determine the prevalence of cervical cancer screening (Pap smear) and identify factors associated with the uptake of screening among women in the mostly rural parish of Portland, Jamaica. These findings could be used to inform public policy, develop and implement strategies to increase screening activities, thereby reducing incidence, morbidity, and mortality from the disease.
Materials and Methods
Study design and procedures
The Institutional Review Board of the University of Alabama at Birmingham, the Advisory Panel on Ethics and Medico-Legal Affairs in the Ministry of Health, Jamaica, and the North-East Regional Health Authority of Jamaica approved the study protocol prior to its implementation. A total of 403 women were enrolled, of which 252 were recruited from the community and 151 at health centers. No personal identifying information was collected in the anonymous questionnaire. All participants were given a full explanation of the methodology and purpose of the project and an assurance of confidentiality. No compensation was offered for participation.
A population survey study design was used. Participants completed an interviewer-administered questionnaire on knowledge, attitudes, and perceptions concerning cervical cancer and cervical cancer screening. The questionnaire was developed using the Health Belief Model as a guiding framework. The outcome variable of interest was a woman's history of having at least one lifetime Pap smear. Predictor variables of interest included:
Age,
Education,
Marital status,
Parity,
Average number of visits to a healthcare provider each year,
Knowledge about cervical cancer screening,
Risk factors for developing cervical cancer including history of smoking, sexually-transmitted infections, HPV diagnosis, age at coital debut, multiple lifetime partners, and oral contraceptive use, and
Barriers to screening including fear, cost, transportation, and embarrassment.
The study was conducted in the parish of Portland in the northeastern part of the island from May through August of 2005. Potential participants were defined as women aged 19 years and older regardless of past Pap smear testing history. Participants were recruited from various health centers throughout the parish, as well as in the general community. Participants were recruited from the following centers: Buff Bay Community Hospital, Cascade, Chepstowe, Hope Bay, Smatt Road Clinic (Port Antonio Health Department), Fellowship, Fairy Hill, and Manchioneal, in addition to the community at large. Residents recruited in the community were from different venues throughout the parish such as stores, schools, and other public places.
Cervical cancer screening in Portland, Jamaica
The standard test for early detection/prevention of cervical cancer in Jamaica is the Pap test. If performed routinely, it is highly effective at identifying changes in cervical cells that could later progress to cancer. Standard guidelines for Pap smear screening in Jamaica recommend that a woman be screened once per year beginning either at age 19 or after coital debut, depending on which event occurs first. If a woman has three consecutive normal smear results, screening frequency can be decreased to once every 3 years. Pap smear testing is not performed during pregnancy. Screening is routinely offered at a woman's 6-month postnatal visit. These recommendations are similar to the guidelines in many developed nations.
Healthcare in Portland, Jamaica is provided through both the private and public sectors. The Public Health Sector offers a variety of health services at little to no cost to the patient, whereas services are more costly in private facilities. There are a total of 16 functional public health centers throughout the parish. Seven of these centers are in the Western District, six in the Central District, and three in the East District. The largest facilities in terms of services offered and patients attending are the Port Antonio Health Department (Central District) and the Buff Bay Community Hospital (West District). One day each month is designated for Pap smear screening. Women may be screened during the remainder of the month if needed.
Statistical analysis
Absolute and relative frequencies (N and %) were obtained for the distributions of the selected variables for the two groups: Those who reported ever having a Pap smear test and those who did not. The general association statistic was used to determine differences in the distributions of selected variables by the two groups. Trend was assessed with the Mantel-Haenszel chi-square test. Odds ratios (ORs) and 95% confidence intervals (CIs) were generated as measures of association for all variables by the two groups. Both crude and adjusted measures of association were generated for all variables. All ORs and CIs were calculated from logistic regression equations. Missing values were excluded from the analysis. The analysis was conducted with Statistical Analysis Software (SAS), version 9.3 (SAS Institute Inc, Cary, NC). All reported P-values are two-tailed.
Multivariate logistic regression
Ever had a pap smear
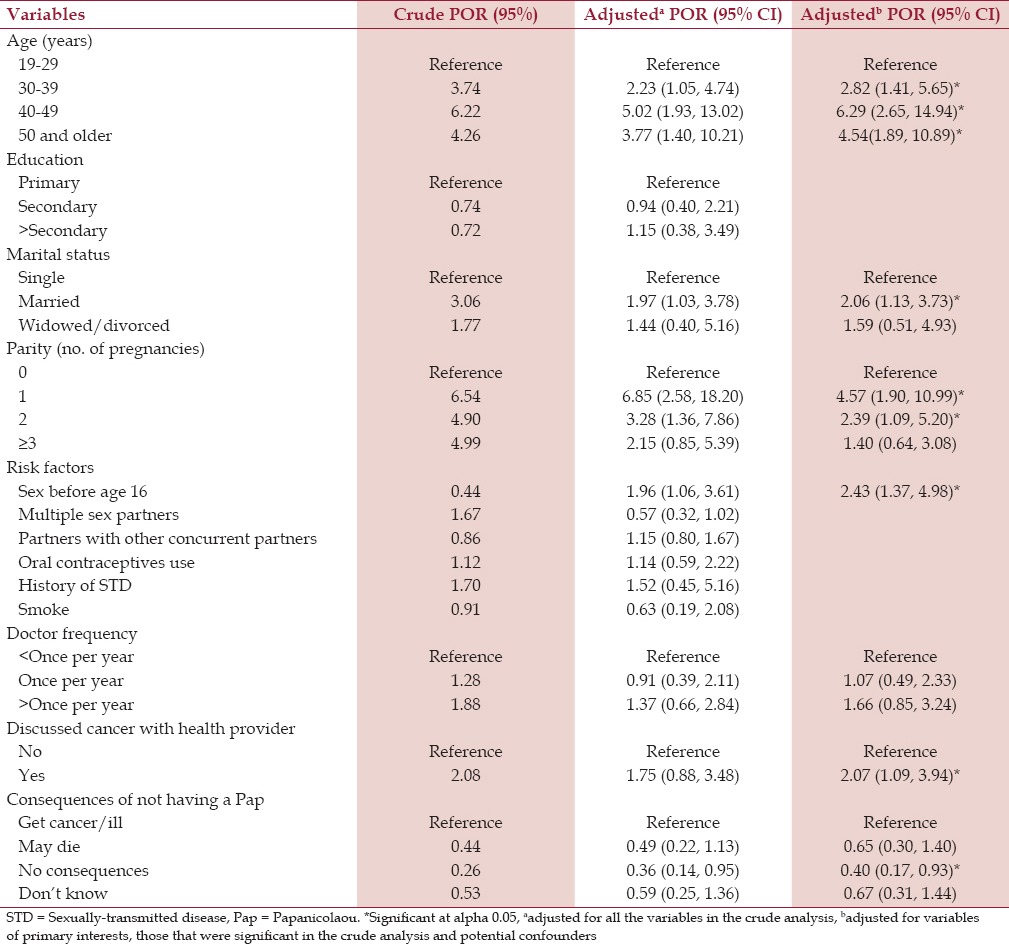
For the final adjusted model for Pap smear status [Table 1], all statistically significant variables from the primary analyses were entered into a logistic regression model. Backward stepwise logistic regression was performed. Variables with a statistical significance of P < 0.05 were retained. Variables that appeared to work as confounders were also retained.
Table 1.
Crude and adjusted prevalence odds ratios (POR) with 95% confidence intervals (CIs) for the study population according to pap smear status (ever vs never had pap smear)
Had pap within the last year
For the final adjusted model, all statistically significant variables from the primary analyses were entered into a logistic regression model. Backward stepwise logistic regression was performed. Variables with a statistical significance of P < 0.05 were retained. Variables that appeared to work as confounders were also retained.
Results
Sociodemographic characteristics
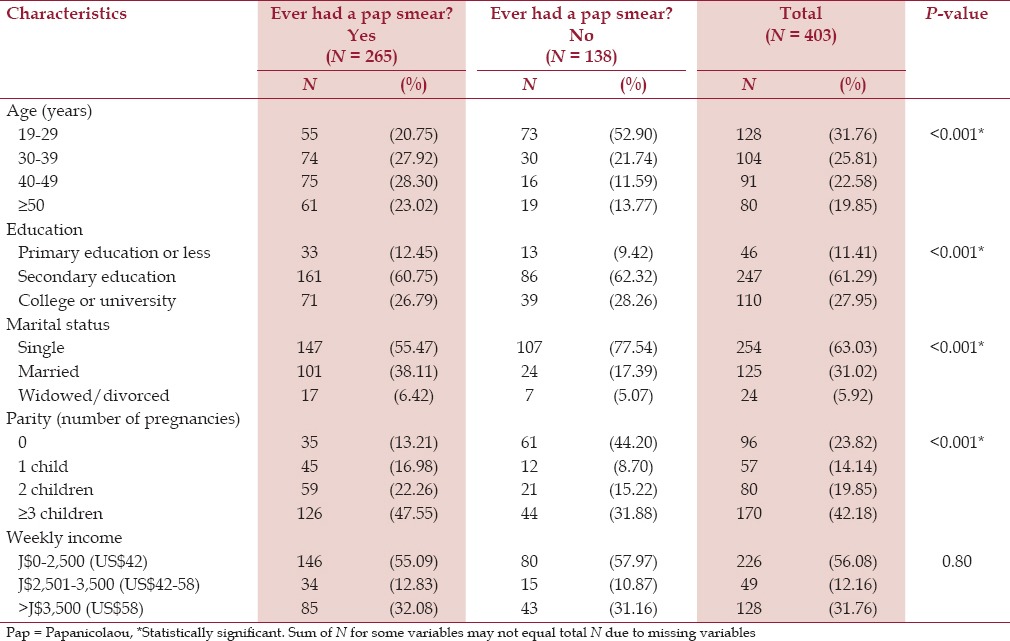
The sociodemographic characteristics of the study population are shown in Table 2. Approximately 66% (265 out of 403) of the study population had a Pap smear and only 16% had a Pap test within the past year. There were significant differences (P < 0.05) in the distribution of women by age. A little more than half (53%) of the women who had never had a Pap smear were in the youngest age group (19-29 years) compared to one-fifth of women (21%) who had ever had a Pap smear. More than three quarters (78%) of women had never had a Pap smear were single compared with 55% of women had ever had a Pap smear. There were also significant differences in the distributions of parity (P < 0.05). A little less than one-half (44%) of the participants who had never had a Pap smear had no children compared with 13% who had a Pap smear. Slightly greater than one-half (56%) of the women were of lower socioeconomic status, earning between 0 and J$2,500 weekly (US $41.67 at the time of the study).
Table 2.
Sociodemographic characteristics of the study population according to pap smear screening status
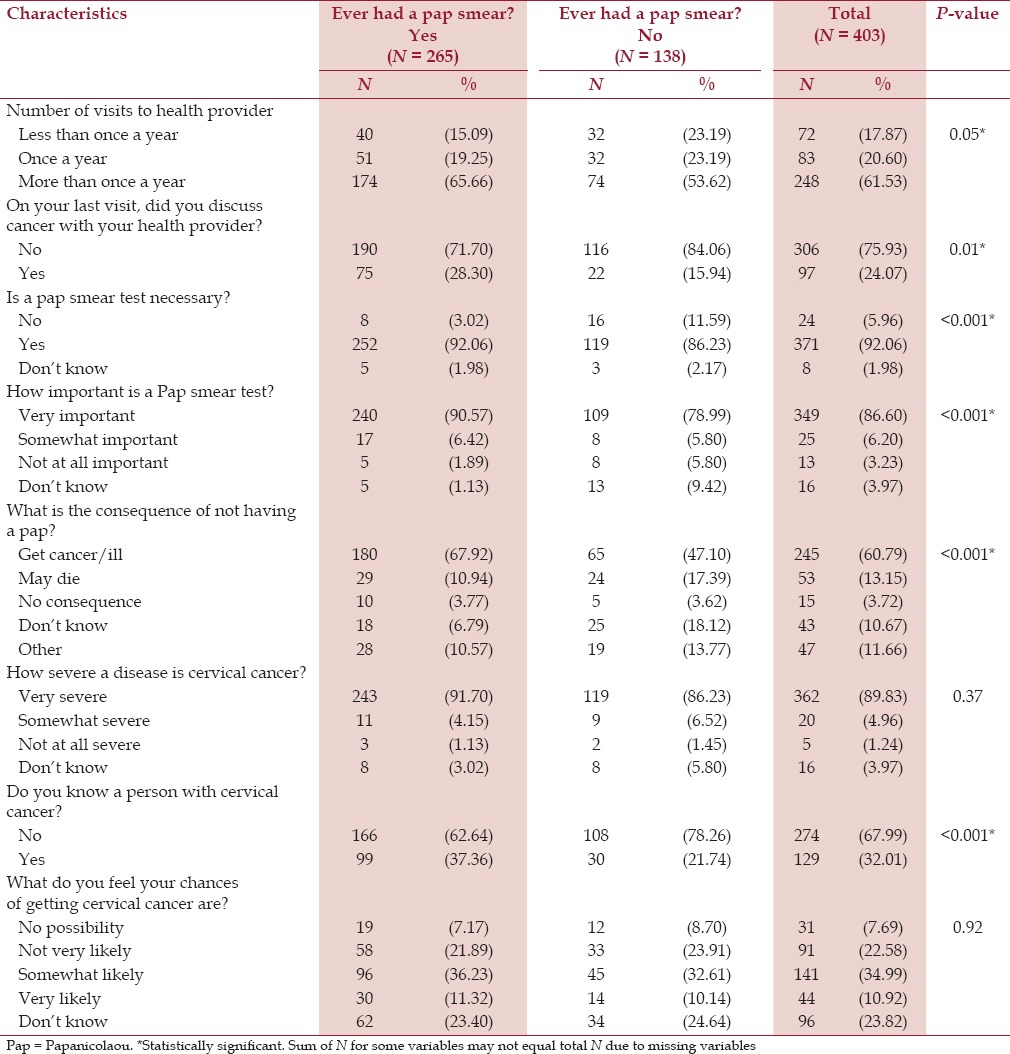
Knowledge, attitudes, and practices
Table 3 shows knowledge, attitudes, and practices about cervical cancer and Pap smear screening. About 66% of the women who had ever received a Pap smear had visited a healthcare provider more than once per year compared with 54% of women who had never had a Pap smear (P = 0.05). Slightly more than one-fourth (28%) of women who had ever had a Pap smear had discussed cancer with their healthcare provider compared with 16% who had never had a Pap smear (P < 0.05). A greater proportion of women who had ever had a Pap (95%) responded that a Pap smear test was necessary compared to 86% of women who had never had a Pap (P < 0.05). Among women who had ever had a Pap smear, 91% reported that a Pap smear was “very important” compared with 79% of women who had never had a Pap smear (P < 0.05). Compared with women who had never had a Pap smear (47%), a significantly greater proportion of women who had a Pap smear (68%) reported that “getting cancer or being ill” was a consequence of not having a Pap smear (P < 0.05). More than one-third (37%) of the women who ever had a Pap smear reported that they knew a person with cervical cancer compared with 22% of women who never had a Pap smear (P < 0.05).
Table 3.
Distribution of study population according to pap smear screening status by knowledge, attitudes, and practices
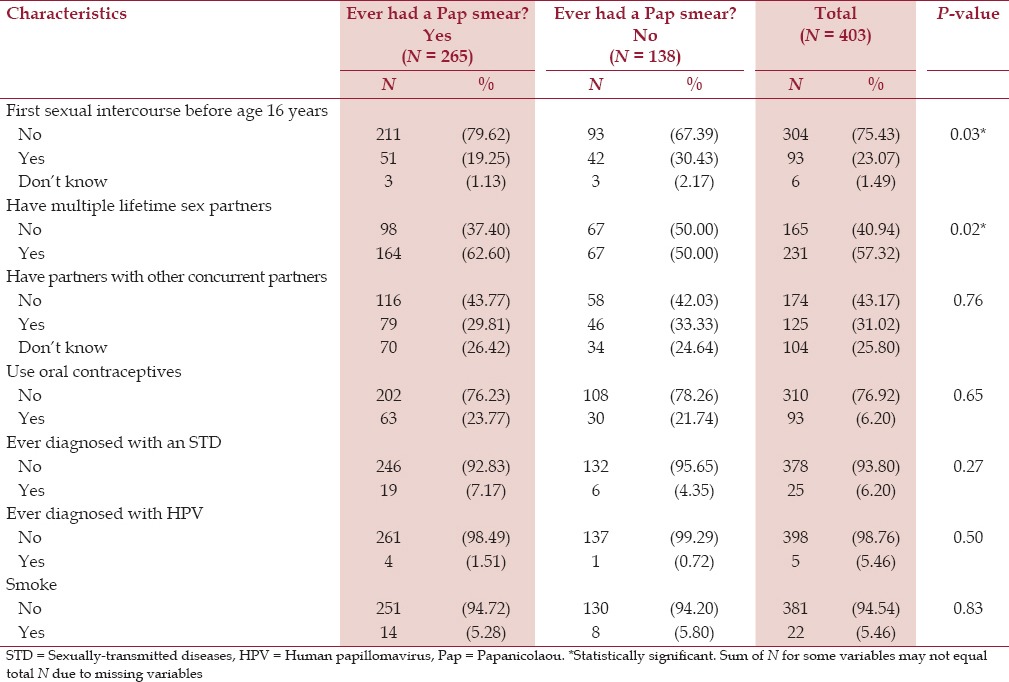
Cervical cancer risk factors
With regard to risk factors for cervical cancer, there was a significant difference (P < 0.05) in the distributions of women who reported having sex at a young age and having multiple sex partners [Table 4]. Almost one-third (30%) of the women who had never had a Pap (30%) reported that they had sex before age 16 compared to 19% of women who had ever had a Pap smear (P < 0.05). A significantly greater proportion of women who had ever had a Pap (63%) responded that they had multiple lifetime sex partners compared to one-half (50%) of women who had never had a Pap (P < 0.05). There were no significant differences in the distributions of other cervical cancer risk factor categories. However, about one-third (31%) of the sample reported that they had partners with other concurrent partners, 23% used oral contraceptives, 6% had a history of sexually-transmitted infections, and 5% smoked.
Table 4.
Distribution of study population according to pap smear status and cervical cancer risk factors
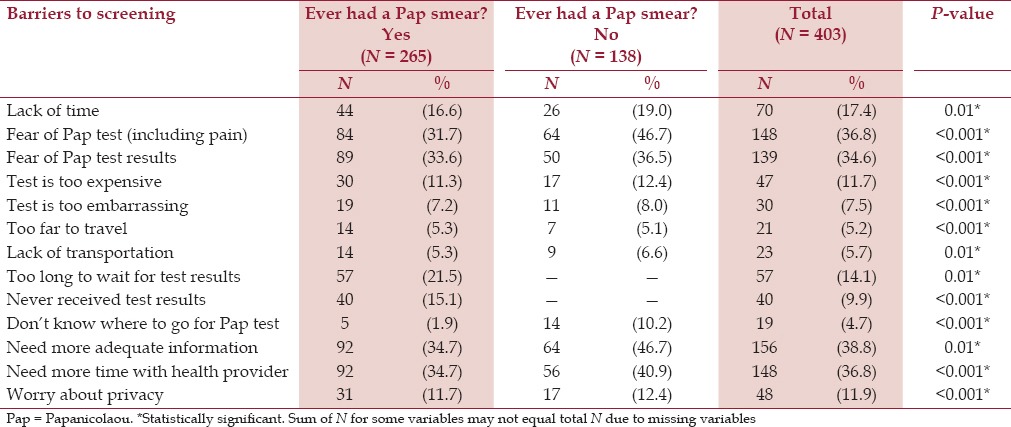
Perceived barriers
Logistic regression analysis revealed that women who reported that they did not know where to go for a Pap smear test were 85% less likely to have ever had a Pap smear (95% CI: 0.04, 0.52). Table 5 shows significant differences in the distributions of women who revealed that they feared the Pap test and needed more adequate information (P < 0.05). A greater proportion of the women who had never had a Pap smear reported that they feared the Pap test (47%), and that they needed more adequate information (47%). About 37% of the total study population reported that they needed more time with their health provider and 35% reported that they feared their health provider would find cervical cancer as the result of a Pap smear.
Table 5.
Distribution of study population according to pap smear screening status and perceived barriers to screening
In the final model [Table 1], women in the 30-39 years age group were almost three times more likely to have ever had a Pap smear compared to women in the youngest age group (19-29 years;95% CI: 1.41, 5.65). Women who were 40-49 years of age were 6.2 times more likely to have ever had a Pap smear compared to women in the 19-29 years age group (95% CI: 2.65, 14.94). Compared to the youngest age group (19-29 years), women 50 years and older were 4.5 times more likely to have had a Pap smear (95% CI: 1.89, 10.89).
Compared to single women, married women were two times more likely to have had a Pap smear (95% CI: 1.13, 3.73). Parity was also found to be associated with the uptake of Pap smear, as women with one child (OR: 4.57, 95% CI: 1.90, 10.99, P 0.5) and those with two children (OR: 2.39, 95% CI: 1.09, 5.20, P 0.5) were more likely to have ever had a Pap smear compared to women who did not have any children. Women who had early coital debut (sex before age 16) were 2.4 times more likely to have ever had a Pap smear compared to women who had sex after age 16 (95% CI: 1.37, 4.98).
Women who discussed cancer with their health providers were two times more likely to have ever had a Pap smear (95% CI: 1.09, 3.94). Compared with women who reported that “getting cancer or being ill” was consequence of not having a Pap smear, those who reported that there were “no consequences” of not having a Pap smear were 60% less likely to have ever had a Pap smear (95% CI: 0.17, 0.93).
Women who earned more than J$3,500 (US$58) weekly were three times more likely to have been screened for cervical cancer in the last year compared to women who earned J$0-2,500 (US$42) weekly (95% CI: 1.42, 6.39). Women who knew a person with cervical cancer were also more likely to have been screened for cervical cancer in the last year (prevalence odds ratio (POR): 2.53, 95% CI: 1.79, 7.03).
Discussion
About two-thirds (66%) of women in this study had been screened for cervical cancer, with 16% screened within the past year. This finding from the parish of Portland concurs with national data which showed that about one-third (34%) of females in Jamaica had never had a Pap smear.[24] This suboptimal uptake of cervical cancer screening is worrisome since the Caribbean has one of the highest cervical cancer rates and the Jamaican Ministry of Health provides Pap screenings for free or little cost.[2]
Some of the barriers to screening among the study population included lack of information (47%), fear of Pap test (47%), needing more time with health provider (41%), and fear of Pap test results (37%). These barriers to cervical cancer screening have also been documented in other studies done in Jamaica and other developing countries.[7,17,18,19,20,21,25,26] Certainly, there is a need to address these internal and health system barriers in order to increase the uptake of cervical cancer screening in Jamaica and other developing nations. Multipronged approaches including improving patient-provider communication and dispelling misconceptions and fears about Pap smear should be employed. Additionally, health systems should make Pap tests more accessible and available.
This study also found that not knowing where to go for cervical cancer screening was negatively associated with ever having a Pap smear. This observation is in accordance with other studies,[25,27] and suggests that more information about the benefits as well as locations for Pap tests may need to be disseminated among women in this region. Additionally, health system changes are needed to integrate cervical cancer screening into primary health services in order to increase awareness of this invaluable preventive measure. Consequently, increased awareness of screening activities and locations will provide Jamaican women with more opportunities to participate in early detection activities.
In accordance with similar studies,[7,10,25,26,28,29] our study found age to be a significant factor in the uptake of cervical cancer screening. This study found that women in the youngest age group (19-29 years) were less likely to have ever had a Pap smear compared with women in the older age groups. The underuse of screening among the youngest age group might not pose a significant public health concern as they are less likely to develop cervical cancer compared to older women (aged 30-50 years).[30,31] However, it is essential to target this age group as most are sexually active. Given the high rates of infection with both high- and low-risk HPV genotypes among Jamaican women,[14,15] coupled with early coital debut and sexual risk behaviors,[9,10] there is a need to increase cervical cancer screening among these women.
Compared with married women, single women in this study were much less likely to have ever had a Pap smear. Marital status has been found to be a significant predicator of uptake of cervical cancer screening in other studies.[18,25,26,29,31,32,33,34] On one hand, spousal support has been found to be positively associated with cervical cancer screening.[18,26,29,31] For instance, studies that assessed cervical screening uptake among women in Malaysia[29] and Tanzania[18] found that women who received social support from their husbands were more likely to attend cervical screening. On the other hand, spouses have been found to hinder cervical cancer screening.[17,30,32] Women in Zimbabwe[17] and Kenya[30] reported that they did not seek cervical screening services because their husbands did not permit them. Therefore, effective interventions need to engage the community including men in promoting awareness of cervical cancer and prevention practices.
As anticipated, healthcare utilization among the study population was associated with uptake of cervical cancer screening. In accordance with a study by Bessler et al.,[7] this study found that Jamaican women who visited a health provider more than once per year were more likely to have ever had a Pap smear compared with women who did not. Conversely, lack of healthcare access has been attributed to low uptake of Pap screening.[17,32,35,36,37,38] For instance, a study among underserved Hispanic and African-American women in the United States found that women who did not have medical coverage were less likely to have been screened.[37] Therefore, it is crucial to increase access to healthcare in order to ensure cervical cancer screening.
Receiving relevant information regarding cervical cancer and Pap smear recommendation from health providers has been shown to positively affect initial receipt of a Pap smear.[7,28,29,36] This study found that women who discussed cancer with their health provider were two times more likely to have ever had a Pap smear. This observation might be due to the fact that these women are more responsive to providers who educate them about the disease and preventive measures. In addition to encouraging women to get Pap smears, these discussions are an excellent opportunity to address misconceptions or fears about the procedure.
This study also found that attitudes regarding consequences of not receiving a Pap smear were associated with screening uptake. Women who reported that there were “no consequences” of not having a Pap smear were less likely to have ever been screened. Given the increasing rates of morbidity and mortality due to cervical cancer among Jamaican women,[22,23] coupled with enormous cost of acute and supportive care for late-stage cervical cancer,[7] surely, not having a Pap test has dire consequences. Hence, there is a need to educate Jamaican women about the consequences of not having a Pap test. These messages should not scare women, but change their knowledge and attitudes about this preventive practice. Consequently, this could affect their decision to undergo Pap tests in the future and share the information with others.[19]
Studies have shown that peer support plays a crucial role in the uptake of cervical cancer screening.[27,39,40] In this study, we found that women who knew a person with cervical cancer were more likely to have been screened in the past year. This finding can be explained by greater access to information about the disease and preventive measures from individuals with cervical cancer. Other studies,[29,40] have also shown that women who knew a person who had a Pap test were more likely to have been screened. Therefore, screening programs should promote peer support in order to increase knowledge and uptake of cervical cancer screening.
This study also found a strong association between parity and the uptake of cervical cancer screening. Women with children were more likely to have ever been screened compared to those who did not have any offspring. This finding is reassuring since multiparity has been found to be associated with increased risk of cervical dysplasia and cancer.[16] The high chances of cervical cancer screening among women with children might be explained by greater interaction between healthcare providers and women who attend maternal and health clinics. Consequently, women with children have more opportunities to gain awareness of cervical cancer and screening through their more frequent contact with health providers.[26,29,31,37] Additionally, these women may be more responsive to reproductive healthcare due to their experience with obstetric or gynecological care.[26,31]
This study had several limitations. All participants were recruited from the parish of Portland in Jamaica. Thus, these findings may not be representative of the whole nation. Additionally, this study was limited by its cross-sectional design, use of self-report, and convenience sampling. Furthermore, there is a possibility of recall and social desirability biases due to the sensitive nature of this study. Despite these limitations, our findings have implications for healthcare services to ensure increased uptake of cervical cancer screening and dispel misconceptions about the Pap test.
Conclusion
This study is one of a few studies,[7,9,10] that has attempted to determine factors associated with the uptake of cervical cancer screening among Jamaican women. Our study findings give insight regarding suboptimal uptake of cervical cancer screening that can be addressed through multipronged approaches.
First, interventions should address misconceptions and fears about cervical cancer screening activities. These interventions should also identify and support conditions that encourage women's use of reproductive health services, thereby reducing the incidence and mortality rates from cervical cancer. Second, health system changes are needed and should include training health providers to:
Improve service delivery,
Improve accessibility and
Understand and address patient concerns.
Third, policy makers should consider integrating cervical cancer screening activities with primary health services and accord the disease the same priorities as those of HIV and childhood immunizations.
Footnotes
Source of Support: Minority Health International Research Training (MHIRT) grant # T37-MD001448 from the National Center on Minority Health and Health Disparities, National Institutes of Health, USA and the Ministry of Health, Jamaica.
Conflict of Interest: None declared.
References
- 1.Human papillomavirus (HPV) and cervical cancer. World Health Organization. 2014. [Accessed July 1, 2014]. at http://www.who.int/mediacentre/factsheets/fs380/en/
- 2.Situational analysis of cervical cancer prevention and control in the Caribbean. Pan American Health Organization. 2013. [Accessed August 15, 2014]. at http://www.who.int/mediacentre/factsheets/fs380/en/
- 3.Scarinci IC, Garcia FA, Kobetz E, Partridge EE, Brandt HM, Bell MC, et al. Cervical cancer prevention. Cancer. 2010;116:2531–42. doi: 10.1002/cncr.25065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peto J, Gilham C, Fletcher O, Matthews FE. The cervical cancer epidemic that screening has prevented in the UK. Lancet. 2004;364:249–56. doi: 10.1016/S0140-6736(04)16674-9. [DOI] [PubMed] [Google Scholar]
- 5.Taylor R, Morrell S, Mamoon H, Wain G, Ross J. Decline in cervical cancer incidence and mortality in New South Wales in relation to control activities (Australia) Cancer Causes Control. 2006;17:299–306. doi: 10.1007/s10552-005-0515-z. [DOI] [PubMed] [Google Scholar]
- 6.Aminisani N, Armstrong B, Egger S, Canfell K. Impact of organised cervical screening on cervical cancer incidence and mortality in migrant women in Australia. BMC Cancer. 2012;12:491. doi: 10.1186/1471-2407-12-491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bessler P, Aung M, Jolly P. Factors affecting uptake of cervical cancer screening among clinic attendees in Trelawny, Jamaica. Cancer Control. 2007;14:396–404. doi: 10.1177/107327480701400410. [DOI] [PubMed] [Google Scholar]
- 8.Jeong S, Saroha E, Knight J, Roofe M, Jolly PE. Determinants of adequate follow-up of an abnormal Papanicolaou result among Jamaican women in Portland, Jamaica. Cancer Epidemiol. 2011;35:211–6. doi: 10.1016/j.canep.2010.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bourne PA, Kerr-Campbell MD, McGrowder DA, Beckford OW. Perception of women on cancer screening and sexual behavior in a rural area, Jamaica: Is there a public health problem? N Am J Med Sci. 2010;2:174–81. doi: 10.4297/najms.2010.2174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bourne PA, Charles CA, Francis CG, South-Bourne N, Peters R. Perception, attitude and practices of women towards pelvic examination and Pap smear in Jamaica. N Am J Med Sci. 2010;2:478–86. doi: 10.4297/najms.2010.2478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fletcher H. Screening for cervical cancer in Jamaica. Caribb Health. 1999;2:9–11. [PubMed] [Google Scholar]
- 12.Cervical Cancer. Medline Plus. 2014. [Accessed June 15, 2014]. at http://www.nlm.nih.gov/medlineplus/cervicalcancer.html .
- 13.de Sanjose S, Quint W, Alemany L, Geraets DT, Klaustermeier JE, Lloveras B, et al. Human papillomavirus genotype attribution in invasive cervical cancer: A retrospective cross-sectional worldwide study. Lancet Oncol. 2010;11:1048–56. doi: 10.1016/S1470-2045(10)70230-8. [DOI] [PubMed] [Google Scholar]
- 14.Lewis-Bell K, Luciani S, Unger E, Hariri S, McFarlane S, Steinau M, et al. Genital human papillomaviruses among women of reproductive age in Jamaica. Rev Panam Salud Publica. 2013;33:159–65. doi: 10.1590/s1020-49892013000300001. [DOI] [PubMed] [Google Scholar]
- 15.Watt A, Garwood D, Jackson M, Younger N, Ragin C, Smikle M, et al. High-risk and multiple human papillomavirus (HPV) infections in cancer-free Jamaican women. Infect Agents Cancer. 2009;4:1–11. doi: 10.1186/1750-9378-4-S1-S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.What are the risk factors for cervical cancer? American Cancer Society. 2014. [Accessed June 15, 2014]. at http://www.cancer.org/cancer/cervicalcancer/moreinformation/cervicalcancerpreventionandearlydetection/cervicalcancerprevention-and-early-detection-cervical-cancer-riskfactors .
- 17.Mupepi SC, Sampselle CM, Johnson TR. Knowledge, attitudes, and demographic factors influencing cervical cancer screening behavior of Zimbabwean women. J Women's Health. 2011;20:943–52. doi: 10.1089/jwh.2010.2062. [DOI] [PubMed] [Google Scholar]
- 18.Lyimo FS, Beran TN. Demographic, knowledge, attitudinal, and accessibility factors associated with uptake of cervical cancer screening among women in a rural district of Tanzania: Three public policy implications. BMC Public Health. 2014;12:22. doi: 10.1186/1471-2458-12-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bayer AM, Nussbaum L, Cabrera L, Paz-Soldan VA. Missed opportunities for health education on pap smears in Peru. Health Educ Behav. 2011;38:198–209. doi: 10.1177/1090198110379580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ibekwe CM1, Hoque ME, Ntuli-Ngcobo B. Perceived benefits of cervical cancer screening among women attending Mahalapye District Hospital, Botswana. Asian Pac J Cancer Prev. 2010;11:1021–7. [PubMed] [Google Scholar]
- 21.Hoque M, Hoque E, Kader SB. Evaluation of cervical cancer screening program at a rural community of South Africa. East Afr J Public Health. 2008;5:111–6. [PubMed] [Google Scholar]
- 22.Villa LL. Cervical Cancer in Latin America and the Caribbean: The problem and the way to solutions. Cancer Epidemiol Biomarkers Prev. 2012;21:1409–13. doi: 10.1158/1055-9965.EPI-12-0147. [DOI] [PubMed] [Google Scholar]
- 23.Luciani S, Andrus JK. A Pan American Health Organization strategy for cervical cancer prevention and control in Latin America and the Caribbean. Reprod Health Matter. 2008;16:59–66. doi: 10.1016/S0968-8080(08)32405-7. [DOI] [PubMed] [Google Scholar]
- 24.Wilks R, Younger N, Tulloch-Reid M, McFarlane S, Francis D. Jamaica Health and Lifestyle Survey 2007-8. 2008. [Accessed May 7, 2014]. at http://www.mona.uwi.edu/reports/health/JHLSII_final_may09.pdf . [PubMed]
- 25.Were E, Nyaberi Z, Buziba N. Perceptions of risk and barriers to cervical cancer screening at Moi Teaching and Referral Hospital (MTRH), Eldoret, Kenya. Afr Health Sci. 2011;11:58–64. [PMC free article] [PubMed] [Google Scholar]
- 26.Nene B, Jayant K, Arrossi S, Shastri S, Budukh A, Hingmire S, et al. Determinants of women's participation in cervical cancer screening trail, Maharashtra, India. Bull World Health Organ. 2007;85:264–72. doi: 10.2471/BLT.06.031195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Byrd T, Peterson S, Chavez R, Heckert A. Cervical cancer screening beliefs among young Hispanic women. Prev Med. 2004;38:192–7. doi: 10.1016/j.ypmed.2003.09.017. [DOI] [PubMed] [Google Scholar]
- 28.Osingada CP, Ninsiima G, Chalo RN, Muliira JK, Ngabirano T. Determinants of uptake of cervical cancer screening services at a no-cost reproductive health clinic managed by nurse-midwives. Cancer Nurs. 2014 doi: 10.1097/NCC.0000000000000156. [DOI] [PubMed] [Google Scholar]
- 29.Gan DE, Dahlui M. Cervical screening uptake and its predictors among rural women in Malaysia. Singapore Med J. 2013;54:163–8. doi: 10.11622/smedj.2013047. [DOI] [PubMed] [Google Scholar]
- 30.Bingham A, Bishop A, Coffey P, Winkler J, Bradley J, Dzuba I, et al. Factors affecting utilization of cervical cancer prevention services in low-resource settings. Salud Public Mex. 2003;45:408–16. doi: 10.1590/s0036-36342003000900015. [DOI] [PubMed] [Google Scholar]
- 31.Swaddiwudhipong W, Chaovakiratipong C, Nguntra P, Mahasakpan P, Tatip Y, Boonmak C. A mobile unit: An effective service for cervical cancer screening among rural Thai women. Int J Epidemiol. 1999;28:35–9. doi: 10.1093/ije/28.1.35. [DOI] [PubMed] [Google Scholar]
- 32.Byrd T, Chavez R, Wilson K. Barriers and facilitators of cervical cancer screening among Hispanic women. Ethn Dis. 2007;17:129–34. [PubMed] [Google Scholar]
- 33.Suzu C, Elizabeth A, Adejumo A. Husbands' knowledge, attitude and behavioral disposition to wives screening for cervical cancer in Ibadan. Afr J Psychol Stud Soc Issues. 2014;17:167–76. [Google Scholar]
- 34.Williams M, Amoateng P. Knowledge and beliefs about cervical cancer screening among men in Kumasi, Ghana. Ghana Med J. 2012;46:147–51. [PMC free article] [PubMed] [Google Scholar]
- 35.Leyden WA, Manos MM, Geiger AM, Weinmann S, Mouchawar J, Bischoff K, et al. Cervical cancer in women with comprehensive health care access: Attributable factors in the screening process. J Natl Cancer Inst. 2005;97:675–83. doi: 10.1093/jnci/dji115. [DOI] [PubMed] [Google Scholar]
- 36.Nuño T1, Castle PE, Harris R, Estrada A, García F. Yuma Project Technical Team. Breast and cervical cancer screening utilization among hispanic women living near the united states-Mexico border. J Women's Health. 2011;20:685–93. doi: 10.1089/jwh.2010.2205. [DOI] [PubMed] [Google Scholar]
- 37.Bazargan M, Bazargan SH, Farooq M, Baker RS. Correlates of cervical cancer screening among underserved Hispanic and African-American women. Prev Med. 2004;39:465–73. doi: 10.1016/j.ypmed.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 38.Ackerson K, Gretebeck K. Factors influencing cancer screening practices of underserved women. J Am Acad Nurs Pract. 2007;19:591–601. doi: 10.1111/j.1745-7599.2007.00268.x. [DOI] [PubMed] [Google Scholar]
- 39.Agurto I, Arrossi S, White S, Coffey P, Dzuba I, Bingham A, et al. Involving the community in cervical cancer prevention programs. Int J Gynecol Obstet. 2005;89:S38–45. doi: 10.1016/j.ijgo.2005.01.015. [DOI] [PubMed] [Google Scholar]
- 40.Logan L, Mcllfatrick S. Exploring women's knowledge, experiences and perceptions of cervical cancer screening in an area of social deprivation. Eur J Cancer Care. 2011;20:720–7. doi: 10.1111/j.1365-2354.2011.01254.x. [DOI] [PubMed] [Google Scholar]


