Abstract
Background:
Low serum vitamin D can cause myalgia, myositis, myopathy, and myonecrosis. Statin-induced myalgia is a major and common cause of statin intolerance. Low serum vitamin D and statins, additively or synergistically, cause myalgia, myositis, myopathy, and/or myonecrosis. Statin-induced myalgia in vitamin D deficient patients can often be resolved by vitamin D supplementation, normalizing serum vitamin D levels.
Aims:
In 74 men and 72 women (age 59 ± 14 years) intolerant to ≥2 statins because of myalgia, myositis, myopathy, or myonecrosis and found to have low (<32 ng/mL) serum vitamin D, we prospectively assessed whether vitamin D supplementation (vitamin D2: 50,000-100,000 units/week) to normalize serum vitamin D would allow successful rechallenge therapy with statins.
Materials and Methods:
Follow-up evaluation on vitamin D supplementation was done on 134 patients at 6 months (median 5.3), 103 patients at 12 months (median 12.2), and 82 patients at 24 months (median 24).
Results:
Median entry serum vitamin D (22 ng/mL, 23 ng/mL, and 23 ng/mL) rose at 6 months, 12 months, and 24 months follow-up to 53 ng/mL, 53 ng/mL, and 55 ng/mL, respectively, (P < .0001 for all) on vitamin D therapy (50,000-100,000 units/week). On vitamin D supplementation, serum vitamin D normalized at 6 months, 12 months, and 24 months follow-up in 90%, 86%, and 91% of the patients, respectively. On rechallenge with statins while on vitamin D supplementation, median low-density lipoprotein cholesterol (LDLC) fell from the study entry (167 mg/dL, 164 mg/dL, and 158 mg/dL) to 90 mg/dL, 91 mg/dL, and 84 mg/dL, respectively, (P < .0001 for all). On follow-up at median 6 months, 12 months, and 24 months on statins and vitamin D, 88%, 91%, and 95% of the previously statin-intolerant patients, respectively, were free of myalgia, myositis, myopathy, and/or myonecrosis.
Conclusions:
Statin intolerance because of myalgia, myositis, myopathy, or myonecrosis associated with low serum vitamin D can be safely resolved by vitamin D supplementation (50,000-100,000 units /week) in most cases (88-95%).
Keywords: Myalgia, myonecrosis, myopathy, myositis, rhabdomyolysis, statin intolerance, statin rechallenge, vitamin D deficiency, vitamin D supplementation
Introduction
Very low serum vitamin D without concomitant statins can cause reduced muscle function,[1,2] myalgia, myositis, and (rarely) rhabdomyolysis,[3,4] and levels <10 ng/mL can produce severe muscle weakness and pain.[5] Exercise-induced severe rhabdomyolysis in a subject with severe vitamin D deficiency (6 ng/mL) has been reported.[4] Vitamin D may improve muscle strength through a highly specific nuclear receptor in the muscle tissue.[6] Serum vitamin D is related to physical performance.[7]
Statin-induced myalgia[8] is a major cause of statin intolerance[9,10,11,12,13] and is common; it is reported in 27% of subjects treated with statins.[12] Statin therapy in community-dwelling older adults may exacerbate the decline in muscle performance and the falls associated with aging without a concomitant decrease in muscle mass, a reversible effect after cessation of statins.[14]
Statins, even in the absence of low serum vitamin D, can cause myalgia and myositis.[15] Atorvastatin has a moderate inhibitory effect on CYP3A4 activity.[16] Low vitamin D levels might reduce CYP3A4 activity, with resultant increase in the serum statin levels and subsequent statin myotoxicity.[17] Within this frame of reference, the development of statin intolerance is promoted by low serum vitamin D in statin users.[9,10,11] Most recent studies,[9,10,11,18,19,20,21,22,23,24] but not all,[25,26,27] have suggested that low vitamin D additively or synergistically interacts with statins to cause myalgia-myopathy.
Since myalgia; myositis; myopathy; and/or myonecrosis are the major causes of statin intolerance,[28] and the tripartite association of serum vitamin D deficiency; statins; myalgia; myositis; myopathy; and/or myonecrosis has physiologic plausibility,[1,2,4,6,7,29] resolution of vitamin D deficiency interacting with statins to produce myalgia; myositis; myopathy; and/or myonecrosis would have significant clinical importance, thereby allowing reinstitution of statins to optimize reduction of low-density lipoprotein cholesterol (LDLC) and prevent cardiovascular diseases.
Palamaner et al.[18] retrospectively studied a cohort of 1,160 subjects taking statins, of whom 276 (24%) developed statin-induced myalgia, myositis, myopathy, and/or myonecrosis (SIM). The lowest quartile of serum vitamin D was independently associated with 1.21 times the hazard of the highest quartile for developing SIM (P = .001). Vitamin D values ≤15 ng/mL had sensitivity of 89%, specificity of 83%, and likelihood ratio of 5.1 in predicting SIM. Palamaner et al.[18] noted that “…considering the temporality of events, with vitamin D deficient patients, without myalgia at statin initiation, subsequently developing myalgia after statin therapy adds validity to our hypothesis associating vitamin D with SIM and negates the possibility of reverse causation that prior cross-sectional studies in this topic were criticized for….”
Linde et al.[23] reported that repletion of vitamin D in vitamin D deficient patients abated myalgias. Of 21 vitamin D deficient patients with intolerable statin-associated myalgias, 14 out of 15 rechallenged with statins were subsequently symptom-free, with one patient experiencing mild and tolerable symptoms, far exceeding the expected rates of acquired tolerability with no therapy (P = 0.01).
Resolution of statin-induced myalgias by correcting vitamin D deficiency has also been reported by Lee,[19] Fang,[20] and Bell.[20,21]
In our current study, we prospectively assessed 146 patients (not previously reported)[9,10,11] intolerant to ≥2 statins because of myalgia, myositis, myopathy, or myonecrosis and found to have low (<32 ng/mL) serum vitamin D. We assessed whether vitamin D supplementation, targeted to normalize serum vitamin D, would allow successful rechallenge therapy with statins in previously statin-intolerant patients.
Materials and Methods
The study conformed to the ethical guidelines of the Jewish Hospital Institutional Review Board for human research, following an approved protocol.
Statin-intolerant patients with low serum vitamin D (<32 ng/mL)
In the temporal order of their referral from Midwestern physicians (Ohio, Kentucky, Indiana, and West Virginia), we prospectively studied 223 hypercholesterolemic patients with statin intolerance (unable to tolerate ≥2 statins), who were found by us to have serum vitamin D <32 ng/mL, our laboratory lower normal limit (LNL). After experiencing myalgia, myositis, myopathy, and/or myonecrosis, all of the referred patients refused to take another statin unless steps were taken to explicate and treat[9,10,11] the pathoetiology of their statin intolerance.
We excluded those patients who had previously developed rhabdomyolysis during statin therapy and those who were taking corticosteroids at study entry, or who had comorbidities that would result in muscle or bone pain (diabetic sensory neuropathy, fibromyalgia, polymyalgia rheumatica, arthritis, peripheral vascular disease, sensory neuropathy, and hypothyroidism). Age was not used as either an inclusion or an exclusion criterion. After the above exclusions from the referred cohort of 223 patients, we prospectively studied 146 in the current analysis cohort.
Laboratory determinations
At the initial visit, after an overnight fast, blood was drawn for total serum 25-hudroxyvitamin D [25(OH)D] levels (vitamin D + vitamin D3), quantitated by two-dimensional high-performance liquid chromatography (2D-HPLC) with tandem mass spectrometry detection after protein precipitation.[30] The laboratory LNL for total 25(OH)D was 32 ng/mL.[30] Additional measures included plasma cholesterol, triglyceride, high-density lipoprotein cholesterol (HDLC); and LDLC; serum calcium; along with creatine phosphokinase (CPK); glucose; insulin; and renal, thyroid, and liver function tests. At each follow-up visit, fasting blood was obtained for lipid profile, serum calcium, CPK, glucose, renal, and liver function tests.
Vitamin D supplementation and prospective follow-up
After documentation of low entry serum 25(OH)D at study entry, the 146 statin-intolerant, vitamin D deficient patients were started on vitamin D2 by prescription,[31] with 58% given 50,000 units/week and 42% given 100,000 units/week, with the higher doses given more often to Caucasians and to men. After 3 weeks on the vitamin D supplementation and with the continuation of vitamin D, statin therapy was restarted, predominantly rosuvastatin with a dosage of 10-20 mg/day. The first follow-up visit was after 1-2 weeks on combined vitamin D and statin rechallenge. The patients were instructed not to take other supplemental vitamins. During follow-up, if intolerable muscle symptoms comparable to those which had previously caused intolerance to ≥2 statins occurred on the statin rechallenge, the patients were instructed to stop the statin rechallenge immediately.
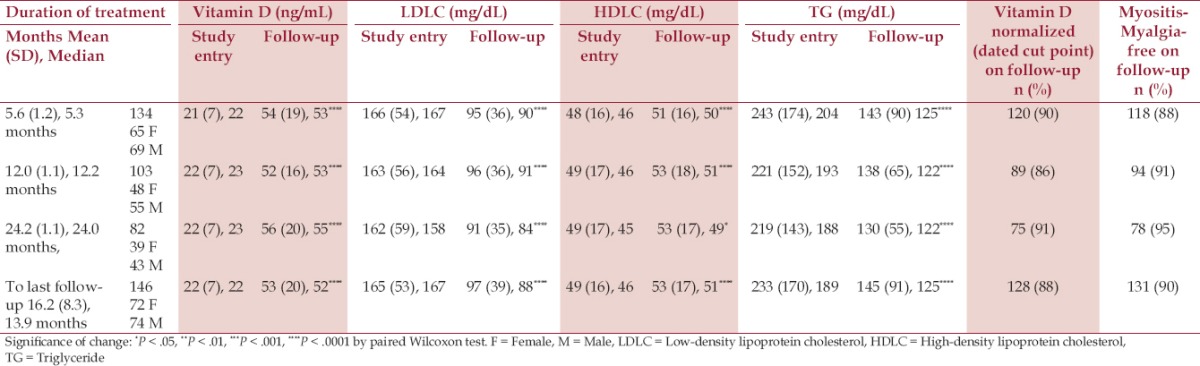
The patients were prospectively reassessed at 3-month intervals for 1 year and then at 4-month intervals thereafter [Table 1], with remeasurement of serum vitamin D and LDLC in each visit. The vitamin D dose[31] was adjusted to keep serum vitamin D in the middle of the normal range ~50-80 ng/mL, and the statin doses were adjusted to reduce LDLC below the Adult Treatment Panel (ATP) III guideline cut points.[32] Additional measures at each follow-up visit were serum calcium, CPK, renal, glucose, and liver function tests. At each follow-up visit, a detailed history was obtained for statin, prescription drug, and the amount of vitamin D supplementation.
Table 1.
Vitamin D supplementation in 146 hypercholesterolemic, vitamin D deficient patients previously statin-intolerent because of myalgia, myositis, myopathy, or myonecrosis. Prospective follow-up at 6 months, 12 months, and 24 months [mean (SD), median exhibited]
Evaluation for and definitions of myalgia, myopathy, myositis, myonecrosis, and rhabdomyolysis
At the initial visit and at every follow-up visit, the patients were interviewed and assessed by the principal investigators. Muscle symptom definitions of both the 2014 National Lipid Association's Statin Muscle Safety Expert Panel[33] and the National Heart, Lung, and Blood Institute[34] were used. Myalgia was defined as muscle discomfort including aches, soreness, stiffness, tenderness, or cramps with a normal CPK level. Myopathy was defined as muscle weakness, with or without CPK elevation. Myositis was defined as muscle inflammation while myonecrosis was defined as symptomatic muscle discomfort with elevated CPK (compared to baseline), mild (3-10-fold elevation in CPK), moderate (10-50-fold), and severe (≥50-fold). Clinical rhabdomyolysis included myonecrosis with myoglobinuria or acute renal failure.
The distinction between myalgic patients and nonmyalgic patients is necessarily imprecise, based on subjective reports[33,34] and CPK levels. However, CPK levels, particularly when they are less than 10 times the laboratory upper normal limit (UNL),[35,36,37] do not regularly facilitate distinction between myalgia-myositis and nonmyalgia-myositis.
Adherence to the vitamin D supplementation (50,000-100,000 units/week)[31] and adherence to the prescribed statin rechallenge dose were reviewed by the investigators at each follow-up visit. The major statin rechallenge was rosuvastatin with a dosage of 10-20 mg/day, but the choice of the specific statin for rechallenge was governed in part by the statin that was paid for by the patients' medical insurance plans.
Statistical methods
All statistical analyses were performed using SAS (version 9.3) (Statistical Analysis Systems, Cary, North Carolina). The sample size calculations were based on our recent study[10] of 38 vitamin D deficient, statin-intolerant patients with myalgia, myositis, myopathy, and/or myonecrosis, 35 (92%) of whom successfully resumed statins without myalgia, myositis, myopathy, and/or myonecrosis after 50,000 units of vitamin D/week supplementation for 3 months. To demonstrate that ≥80% of the previously statin-intolerant patients would recover statin tolerance after vitamin D supplementation, at least 75 vitamin D deficient, statin-using patients with myalgia, myositis, myopathy, and/or myonecrosis would be needed for significance alpha = .05, with power 0.8.
Responses to vitamin D supplementation and reinstation of statins were assessed in patients at 6 months, 12 months, and 24 months, and at the last of the three follow-up visits [Table 1]. Significance of the changes on vitamin D supplementation treatment was tested using nonparametric paired Wilcoxon tests [Table 1].
Stepwise logistic regression [significant level entering (SLE) = .15, significant level staying (SLS) = .05)] was run with response (muscle symptoms, no muscle symptoms) on statin and vitamin D supplementation at the last follow-up as the dependent variable and the following explanatory variables: Age, race, sex, entry serum 25(OH)D, levels at the last follow-up, change in CPK and vitamin D, and duration of vitamin D supplementation.
Results
Before beginning our study, all the patients had experienced myalgia, myositis, myopathy, or myonecrosis[33] but (by selection) not rhabdomyolysis on ≥2 statins, predominantly simvastatin, atorvastatin, or lovastatin, which led to their referral to our center.
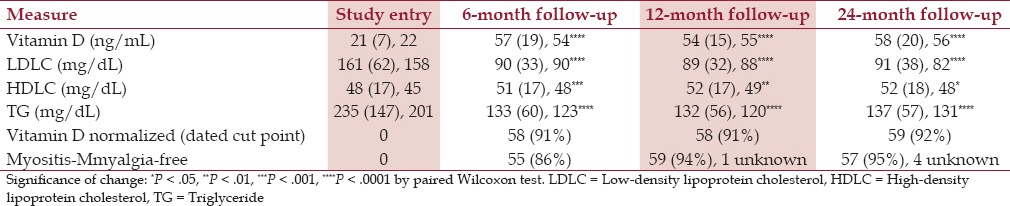
Of the 146 patients, there were 74 men and 72 women with the mean ± standard deviation (SD) age being 59 ± 14 years; 134 patients had follow-up at 6 months (median 5.3 months), 103 at 12 months (median 12.2 months), and 82 at 24 months (median 24.0 months) [Table 1]. Of the 146 patients, 64 had all three follow-up visits, at ~6 months, 12 months, and 24 months [Table 2].
Table 2.
Vitamin D supplementation in 64 (30 women, 34 men) hypercholesterolemic, vitamin D deficient patients previously statin-intolerent because of myalgia, myositis, myopathy, or myonecrosis. Prospective followup at 6 months, 12 months, and 24 months [mean (SD), median exhibited]. The 64 patients had all three follow-up visits at 6 months, 12 months, and 24 months
At the 6-month follow-up visit, the median vitamin D supplementation dose was 50,000 units/week, 50,000-<70,000 units/week in 43% of patients and 70,000-100,000 units/week in 39% of patients. At the 12-month follow-up visit, the median vitamin D supplementation dose was 50,000 units/week, 50,000-<70,000 units/week in 41% of patients and 70,000-100,000 units/week in 36% of patients. At the 24-month follow-up visit, the median vitamin D supplementation dose was 50,000 units/week, 50,000-<70,000 units/week in 38% of patients and 70-100,000 units/week in 37% of patients.
In the three follow-up time windows, median entry serum vitamin D (22 ng/mL, 23 ng/mL, and 23 ng/mL) rose on vitamin D therapy to 53 ng/mL, 53 ng/mL, and 55 ng/mL, respectively, (P < .0001) [Table 1]. In the 64 patients with all three follow-up visits (6 months, 12 months, and 24 months), serum vitamin D rose from 22 ng/mL at pretreatment entry to 54 ng/mL, 55 ng/mL, and 56 ng/mL at 6 months, 12 months, and 24 months, respectively, [Table 2].
Vitamin D normalized on therapy at the three follow-up periods in 90% (5.3 months), 86% (12.2 months), and 91% of patients (24.0 months) [Table 1]. In the 64 patients with all three follow-up visits, vitamin D normalized in 91%, 91%, and 92% of patients at 6-month, 12-month, and 24-month follow-up visits, respectively, [Table 2].
Median LDLC in the time windows fell from 167 mg/dL, 164 mg/dL, and 158 mg/dL at pretreatment study entry to 90 mg/dL, 91 mg/dL, and 84 mg/dL, respectively, (P < .0001 for all) [Table 1]. Mean HDLC rose from 46 mg/dL, 46 mg/dL, and 45 mg/dL to 50 mg/dL, 51 mg/dL, and 49 mg/dL, respectively, (P < .0001, <.0001, <.05) and triglyceride fell from 204 mg/dL, 193 mg/dL, and 188 mg/dL to 125 mg/dL, 122 mg/dL, and 122 mg/dL, respectively, (P < .0001 for all) [Table 1]. In the 64 patients with all three follow-up visits, median LDLC fell from 158 mg/dL at entry to median levels of 90 mg/dL, 88 mg/dL, and 82 mg/dL on follow-up (P < .0001 for all) [Table 2].
During the three follow-up visits, 3% of patients (4 patients) had CPK 3-<10 times the UNL, the other 97% had CPK <3*UNL, and no patient had CPK ≥10*UNL.
At the 6-month follow-up, 16 (12%) patients had myalgia-myositis (all with CPK <3 times the laboratory UNL) and stopped the statin rechallenge while 118 (88%) remained free of muscle symptoms [Table 1]. At the 12-month follow-up, nine (9%) patients had myalgia-myositis and stopped the statin rechallenge, one of whom had mild myonecrosis [CPK 3-<10*UNL] and eight with CPK <3*UNL while 94 (91%) remained free of myalgia-myositis [Table 1]. At the 24-month follow-up, four (5%) patients had myalgia-myositis and stopped the statin rechallenge (three had CPK<3*UNL, and one had CPK 3-<10*UNL) while 78 (95%) remained symptom-free. At the last of the follow-ups, 15 (10%) patients had myalgia-myositis and stopped the statin rechallenge (13 had CPK<3*UNL, two had CPK 3-<10*UNL) while 131 (90%) were symptom-free [Table 1].
At all the three follow-up periods of the 16 (12%), nine (9%), and four (5%) patients who stopped the statin rechallenge because of myalgia-myositis, none had moderate or severe myonecrosis and rhabdomyolysis.
By stepwise selection, the only significant predictor for muscle symptoms at the last follow-up was the serum vitamin D level. For each one unit increase in serum vitamin D, the odds ratio (OR) (muscle symptoms/symptom-free) was 0.96 with the 95% confidence intervals being 0.933-0.996. The area under the curve (AUC) for this logistic regression model was 0.719.
Safety
No patients developed hypercalcemia and nephrolithiasis. There were no consistent abnormal alterations in serum calcium, renal, glucose, or liver function tests during the study period.
At 6-month follow-up, 2% (3/134) of the patients had serum vitamin D levels ≥100 ng/mL (the laboratory UNL), 0% (0/103) at 12-month follow up, and 2% (2/82) at 24-month follow-up. These patients were asymptomatic at these high serum vitamin D levels and when their vitamin D supplementation was halved, their serum vitamin D level fell below the laboratory UNL of 100 ng/mL.
Discussion
Unless myonecrosis or clinical rhabdomyolysis[33] are present, myalgia, myopathy, and myositis in statin-muscle intolerant patients is necessarily subjective. Within this frame of reference, before entering the current study, all the patients had experienced myalgia, myositis, myopathy, or myonecrosis on ≥2 statins, severe enough so that they refused to begin any new statin therapy without evaluation of their statin intolerance.
In most studies, low serum vitamin D is associated with statin intolerance[9,10,11,14,18,19,20,21,22] and vitamin D supplementation appears to reverse statin intolerance,[19,20,21,23] including our three previous reports.[9,10,11] In the current study, among the 146 statin-intolerant patients found to have low serum vitamin D, most of them (88% at 6 months, 91% at 12 months, and 95% at 24 months) tolerated statins without myalgia, myositis, myopathy, and/or myonecrosis after repletion of serum vitamin D with vitamin D supplementation therapy (median 50,000 units/week). By logistic regression, the only significant predictor for muscle symptoms at the last follow-up was serum vitamin D level at that time, consistent with our hypothesis that statin intolerance because of myalgia, myositis, myopathy, and/or myonecrosis was associated with low serum vitamin D and could largely be resolved by vitamin D supplementation. Furthermore, vitamin D supplementation was safe and well tolerated.
What are the potential mechanisms that account for the effectiveness of vitamin D supplementation on statin-induced myalgia and myositis? Muscle cells have vitamin D receptors, and low levels of plasma vitamin D can be associated with proximal muscle weakness, hypotonia, prolonged time to peak contraction and relaxation, and generalized musculoskeletal pain.[15,28,38] Supplementation with vitamin D may enhance the skeletal muscle function through morphological adaptations and enhanced calcium availability during cross-bridge cycling.[39] Vitamin D and the vitamin D receptor in the skeletal muscle influence it via both genomic and nongenomic mechanisms.[40,41] The skeletal muscle contains vitamin D receptors that modulate transcription factors in muscle cells, which in turn mediate cell proliferation and differentiation into mature type II muscle fibers.[42] Vitamin D is responsible for transportation of calcium into sarcoplasmic reticulum, necessary for sarcomeric muscular contraction,[43] and plays an important function in muscle contractility and myogenesis.[44] Since vitamin D is an inducer of CYP3A4 and CYP2C9, vitamin D supplementation should reduce myopathic side effects by increasing the metabolism of statins, thereby reducing statin-induced muscle toxicity.[45] Simvastatin, atorvastatin, and lovastatin are metabolized primarily by CYP3A4, fluvastatin by CYP2C9, and pravastatin and rosuvastatin are not appreciably metabolized by CYP enzymes.[45] Rosuvastatin, the statin rechallenge used in the present study, appears to cause less myalgia than other statins,[46] in part, because it is not metabolized by CYP3A4. Pitavastatin is marginally metabolized by CYP2C9 and to a lesser degree by CYP2C8.[45]
The strength of the current study was that 88-95% of patients previously intolerant to two or more statins were, after repletion of serum vitamin D, able to tolerate rechallenge with statins with concomitant excellent lowering of LDLC to ATP suggested levels.[32] The second strength of the current study, adding to previous experience,[9,10,11,14,18,19,20,21,22,23] is the large number of patients with extended follow-up, reemphasizing the effectiveness of vitamin D supplementation in myalgia, myositis, myopathy, and/or myonecrosis statin-intolerant patients with low pretreatment vitamin D. An optimal, gold-standard study of patients intolerant to ≥2 statins and having low pretreatment vitamin D would be double-blind, incorporating four intervention groups using a single statin at a fixed dose. Group 1 would be given placebos for both statin and vitamin D, group 2 placebo for statin and active vitamin D supplementation, group 3 active statin and placebo vitamin D, and group 4 both active statin and active vitamin D. This study would require a large cohort of patients and would be very difficult to select as, based on our experience, patients intolerant of ≥2 statins will not agree to participate in a blinded study where half of the patients would be given a statin.
The major limitation of our current study and most previous reports,[19,20,21,23] including our three previous studies,[9,10,11] is that they were not double-blind and the endpoints (absence of myalgia, myositis, myopathy, and/or myonecrosis) were subjective. However, the patients of the current study who were intolerant of two or more statins because of myalgia-myopathy were referred to our center because of their refusal to ever take another statin, failing explication of a potential etiology and a simple, inexpensive, and safe intervention that would allow them to tolerate statins without incapacitating muscle symptoms. A second limitation of our current study was that ≥1 statin, predominantly rosuvastatin, not metabolized by CYP3A4 and rarely associated with myalgia-myositis[46] was used for rechallenge after vitamin D supplementation. However, Fung et al.[47] have reported that the response to multiple statins on rechallenge did not differ between the statins.
Overall, in our initial three reports[9,10,11] and in the current study, we have provided supplemental vitamin D to 402 statin-intolerant patients with low serum vitamin D at entry, of whom 352 (88%) were subsequently able to tolerate rechallenge with statins with excellent tolerability and the LDLC lowering to targeted levels.[32] Even given the placebo effect and the primarily subjective nature of myalgia, myositis, myopathy, and/or myonecrosis, it is very unlikely that 88-95% of statin-intolerant patients, as in the current report, were able take statin rechallenge without any muscle symptoms once serum vitamin D was normalized.
Conclusion
Statin intolerance because of myalgia, myositis, myopathy, or myonecrosis in vitamin D deficient patients can, in most cases (88%-95%), be safely resolved by vitamin D supplementation (50,000-100,000 units/week).
Footnotes
Source of Support: Supported in part by the Lipoprotein Research Fund of the Jewish Hospital of Cincinnati, Ohio.
Conflict of Interest: None declared.
References
- 1.Erkal MZ, Wilde J, Bilgin Y, Akinci A, Demir E, Bödeker RH, et al. High prevalence of vitamin D deficiency, secondary hyperparathyroidism and generalized bone pain in Turkish immigrants in Germany: Identification of risk factors. Osteoporos Int. 2006;17:1133–40. doi: 10.1007/s00198-006-0069-2. [DOI] [PubMed] [Google Scholar]
- 2.Shinchuk LM, Holick MF. Vitamin d and rehabilitation: Improving functional outcomes. Nutr Clin Pract. 2007;22:297–304. doi: 10.1177/0115426507022003297. [DOI] [PubMed] [Google Scholar]
- 3.Glerup H, Mikkelsen K, Poulsen L, Hass E, Overbeck S, Andersen H, et al. Hypovitaminosis D myopathy without biochemical signs of osteomalacic bone involvement. Calcif Tissue Int. 2000;66:419–24. doi: 10.1007/s002230010085. [DOI] [PubMed] [Google Scholar]
- 4.Glueck CJ, Conrad B. Severe vitamin d deficiency, myopathy, and rhabdomyolysis. N Am J Med Sci. 2013;5:494–5. doi: 10.4103/1947-2714.117325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rasheed K, Sethi P, Bixby E. Severe vitamin d deficiency induced myopathy associated with rhabydomyolysis. N Am J Med Sci. 2013;5:334–6. doi: 10.4103/1947-2714.112491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bischoff-Ferrari HA, Dietrich T, Orav EJ, Hu FB, Zhang Y, Karlson EW, et al. Higher 25-hydroxyvitamin D concentrations are associated with better lower-extremity function in both active and inactive persons aged > or =60 y. Am J Clin Nutr. 2004;80:752–8. doi: 10.1093/ajcn/80.3.752. [DOI] [PubMed] [Google Scholar]
- 7.Bunout D, Barrera G, Leiva L, Gattas V, de la Maza MP, Avendaño M, et al. Effects of vitamin D supplementation and exercise training on physical performance in Chilean vitamin D deficient elderly subjects. Exp Gerontol. 2006;41:746–52. doi: 10.1016/j.exger.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 8.Joy TR, Hegele RA. Narrative review: Statin-related myopathy. Ann Intern Med. 2009;150:858–68. doi: 10.7326/0003-4819-150-12-200906160-00009. [DOI] [PubMed] [Google Scholar]
- 9.Glueck CJ, Abuchaibe C, Wang P. Symptomatic myositis-myalgia in hypercholesterolemic statin-treated patients with concurrent vitamin D deficiency leading to statin intolerance may reflect a reversible interaction between vitamin D deficiency and statins on skeletal muscle. Med Hypotheses. 2011;77:658–61. doi: 10.1016/j.mehy.2011.07.007. [DOI] [PubMed] [Google Scholar]
- 10.Ahmed W, Khan N, Glueck CJ, Pandey S, Wang P, Goldenberg N, et al. Low serum 25 (OH) vitamin D levels (<32 ng/mL) are associated with reversible myositis-myalgia in statin-treated patients. Transl Res. 2009;153:11–6. doi: 10.1016/j.trsl.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 11.Glueck CJ, Budhani SB, Masineni SS, Abuchaibe C, Khan N, Wang P, et al. Vitamin D deficiency, myositis-myalgia, and reversible statin intolerance. Curr Med Res Opin. 2011;27:1683–90. doi: 10.1185/03007995.2011.598144. [DOI] [PubMed] [Google Scholar]
- 12.Vandenberg BF, Robinson J. Management of the patient with statin intolerance. Curr Atheroscler Rep. 2010;12:48–57. doi: 10.1007/s11883-009-0077-8. [DOI] [PubMed] [Google Scholar]
- 13.Zhang H, Plutzky J, Skentzos S, Morrison F, Mar P, Shubina M, et al. Discontinuation of statins in routine care settings: A cohort study. Ann Intern Med. 2013;158:526–34. doi: 10.7326/0003-4819-158-7-201304020-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Scott D, Blizzard L, Fell J, Jones G. Statin therapy, muscle function and falls risk in community-dwelling older adults. QJM. 2009;102:625–33. doi: 10.1093/qjmed/hcp093. [DOI] [PubMed] [Google Scholar]
- 15.Gupta A, Thompson PD. The relationship of vitamin D deficiency to statin myopathy. Atherosclerosis. 2011;215:23–9. doi: 10.1016/j.atherosclerosis.2010.11.039. [DOI] [PubMed] [Google Scholar]
- 16.Tirkkonen T, Heikkila P, Vahlberg T, Huupponen R, Laine K. Epidemiology of CYP3A4-mediated clopidogrel drug-drug interactions and their clinical consequences. Cardiovasc Ther. 2013;31:344–51. doi: 10.1111/1755-5922.12028. [DOI] [PubMed] [Google Scholar]
- 17.Perez-Castrillon JL, Abad Manteca L, Vega G, Del Pino Montes J, de Luis D, Duenas Laita A. Vitamin d levels and lipid response to atorvastatin. Int J Endocrinol. 2010;2010:320721. doi: 10.1155/2010/320721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Palamaner Subash Shantha G, Ramos J, Thomas-Hemak L, Pancholy SB. Association of vitamin D and incident statin induced myalgia--a retrospective cohort study. PLoS One. 2014;9:e88877. doi: 10.1371/journal.pone.0088877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee P, Greenfield JR, Campbell LV. Vitamin D insufficiency - A novel mechanism of statin-induced myalgia? Clin Endocrinol (Oxf) 2009;71:154–5. doi: 10.1111/j.1365-2265.2008.03448.x. [DOI] [PubMed] [Google Scholar]
- 20.Fang S, Wu J. Resolution of statin-induced myalgias by correcting vitamin D deficiency. South Med J. 2011;104:380. doi: 10.1097/SMJ.0b013e318213d123. [DOI] [PubMed] [Google Scholar]
- 21.Bell DS. Resolution of statin-induced myalgias by correcting vitamin D deficiency. South Med J. 2010;103:690–2. doi: 10.1097/SMJ.0b013e3181e21088. [DOI] [PubMed] [Google Scholar]
- 22.Mergenhagen K, Ott M, Heckman K, Rubin LM, Kellick K. Low vitamin D as a risk factor for the development of myalgia in patients taking high-dose simvastatin: A retrospective review. Clin Ther. 2014;36:770–7. doi: 10.1016/j.clinthera.2014.02.023. [DOI] [PubMed] [Google Scholar]
- 23.Linde R, Peng L, Desai M, Feldman D. The role of vitamin D and SLCO1B1*5 gene polymorphism in statin-associated myalgias. Dermatoendocrinol. 2010;2:77–84. doi: 10.4161/derm.2.2.13509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Morioka TY, Lee AJ, Bertisch S, Buettner C. Vitamin D status modifies the association between statin use and musculoskeletal pain: A population based study. Atherosclerosis. 2015;238:77–82. doi: 10.1016/j.atherosclerosis.2014.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kurnik D, Hochman I, Vesterman-Landes J, Kenig T, Katzir I, Lomnicky Y, et al. Muscle pain and serum creatine kinase are not associated with low serum 25(OH) vitamin D levels in patients receiving statins. Clin Endocrinol (Oxf) 2012;77:36–41. doi: 10.1111/j.1365-2265.2011.04321.x. [DOI] [PubMed] [Google Scholar]
- 26.Riphagen IJ, van der Veer E, Muskiet FA, DeJongste MJ. Myopathy during statin therapy in the daily practice of an outpatient cardiology clinic: Prevalence, predictors and relation with vitamin D. Curr Med Res Opin. 2012;28:1247–52. doi: 10.1185/03007995.2012.702102. [DOI] [PubMed] [Google Scholar]
- 27.Eisen A, Lev E, Iakobishvilli Z, Porter A, Brosh D, Hasdai D, et al. Low plasma vitamin D levels and muscle-related adverse effects in statin users. Isr Med Assoc J. 2014;16:42–5. [PubMed] [Google Scholar]
- 28.Thompson PD, Clarkson P, Karas RH. Statin-associated myopathy. JAMA. 2003;289:1681–90. doi: 10.1001/jama.289.13.1681. [DOI] [PubMed] [Google Scholar]
- 29.Lips P. Vitamin D physiology. Prog Biophys Mol Biol. 2006;92:4–8. doi: 10.1016/j.pbiomolbio.2006.02.016. [DOI] [PubMed] [Google Scholar]
- 30.Tsugawa N, Suhara Y, Kamao M, Okano T. Determination of 25-hydroxyvitamin D in human plasma using high-performance liquid chromatography - tandem mass spectrometry. Anal Chem. 2005;77:3001–7. doi: 10.1021/ac048249c. [DOI] [PubMed] [Google Scholar]
- 31.Kennel KA, Drake MT, Hurley DL. Vitamin D deficiency in adults: When to test and how to treat. Mayo Clin Proc. 2010;85:752–8. doi: 10.4065/mcp.2010.0138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Grundy SM, Cleeman JI, Merz CN, Brewer HB, Jr, Clark LT, Hunninghake DB, et al. Coordinating Committee of the National Cholesterol Education Program. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110:227–39. doi: 10.1161/01.CIR.0000133317.49796.0E. [DOI] [PubMed] [Google Scholar]
- 33.Rosenson RS, Baker SK, Jacobson TA, Kopecky SL, Parker BA. The National Lipid Association's Muscle Safety Expert Panel. An assessment by the statin muscle safety task force: 2014 update. J Clin Lipidol. 2014;8(Suppl):S58–71. doi: 10.1016/j.jacl.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 34.Nichols GA, Koro CE. Does statin therapy initiation increase the risk for myopathy. An observational study of 32,225 diabetic and nondiabetic patients? Clin Ther. 2007;29:1761–70. doi: 10.1016/j.clinthera.2007.08.022. [DOI] [PubMed] [Google Scholar]
- 35.Draeger A, Monastyrskaya K, Mohaupt M, Hoppeler H, Savolainen H, Allemann C, et al. Statin therapy induces ultrastructural damage in skeletal muscle in patients without myalgia. J Pathol. 2006;210:94–102. doi: 10.1002/path.2018. [DOI] [PubMed] [Google Scholar]
- 36.Sniderman AD. Is there value in liver function test and creatine phosphokinase monitoring with statin use? Am J Cardiol. 2004;94:30F–4F. doi: 10.1016/j.amjcard.2004.07.052. [DOI] [PubMed] [Google Scholar]
- 37.Glueck CJ, Rawal B, Khan NA, Yeramaneni S, Goldenberg N, Wang P. Should high creatine kinase discourage the initiation or continuance of statins for the treatment of hypercholesterolemia? Metabolism. 2009;58:233–8. doi: 10.1016/j.metabol.2008.09.019. [DOI] [PubMed] [Google Scholar]
- 38.Harari M, Dramsdahl E, Shany S, Baumfeld Y, Ingber A, Novack V, et al. Increased vitamin D serum levels correlate with clinical improvement of rheumatic diseases after Dead Sea climatotherapy. Isr Med Assoc J. 2011;13:212–5. [PubMed] [Google Scholar]
- 39.Todd JJ, Pourshahidi LK, McSorley EM, Madigan SM, Magee PJ. Vitamin D: Recent Advances and Implications for Athletes. Sports Med. 2015;45:213–29. doi: 10.1007/s40279-014-0266-7. [DOI] [PubMed] [Google Scholar]
- 40.Hamilton B. Vitamin D and human skeletal muscle. Scand J Med Sci Sports. 2010;20:182–90. doi: 10.1111/j.1600-0838.2009.01016.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nguyen TM, Lieberherr M, Fritsch J, Guillozo H, Alvarez ML, Fitouri Z, et al. The rapid effects of 1,25-dihydroxyvitamin D3 require the vitamin D receptor and influence 24-hydroxylase activity: Studies in human skin fibroblasts bearing vitamin D receptor mutations. J Biol Chem. 2004;279:7591–7. doi: 10.1074/jbc.M309517200. [DOI] [PubMed] [Google Scholar]
- 42.Simpson RU, Thomas GA, Arnold AJ. Identification of 1,25-dihydroxyvitamin D3 receptors and activities in muscle. J Biol Chem. 1985;260:8882–91. [PubMed] [Google Scholar]
- 43.Pfeifer M, Begerow B, Minne HW. Vitamin D and muscle function. Osteoporos Int. 2002;13:187–94. doi: 10.1007/s001980200012. [DOI] [PubMed] [Google Scholar]
- 44.Boland RL. VDR activation of intracellular signaling pathways in skeletal muscle. Mol Cell Endocrinol. 2011;347:11–6. doi: 10.1016/j.mce.2011.05.021. [DOI] [PubMed] [Google Scholar]
- 45.Bhattacharyya S, Bhattacharyya K, Maitra A. Possible mechanisms of interaction between statins and vitamin D. QJM. 2012;105:487–91. doi: 10.1093/qjmed/hcs001. [DOI] [PubMed] [Google Scholar]
- 46.Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM, Jr, Kastelein JJ, et al. JUPITER Study Group. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359:2195–207. doi: 10.1056/NEJMoa0807646. [DOI] [PubMed] [Google Scholar]
- 47.Fung EC, Crook MA. Statin myopathy: A lipid clinic experience on the tolerability of statin rechallenge. Cardiovasc Ther. 2012;30:e212–8. doi: 10.1111/j.1755-5922.2011.00267.x. [DOI] [PubMed] [Google Scholar]


