Abstract
Background:
Cancer related fatigue (CRF) is a problem that is highly under reported, under recognized and thus, under treated. About 80% of patients receiving chemotherapy/radiotherapy experience CRF, making it the most common side effect of cancer treatment. Functional assessment of chronic illness therapy fatigue (FACIT-F) version-4 is a 13 item questionnaire that has been used to measure the level of fatigue of cancer patients during their daily activities over the past 7 days.
Materials and Methods:
92 patients of age 18 years and above attending the oncology Out Patient Department (OPD) of a regional cancer center were recruited in this study and were given FACIT-F questionnaire. The relevant sociodemographic parameters were obtained from the medical records of the patients. The internal consistency of the 13 items was measured using the Cronbach's alpha.
Results:
The Cronbach alpha coefficient for FACIT-F scale in our study was found to be 0.74. Kendall's coefficient of concordance was estimated to be 0.080. The correlation between Eastern Cooperative Oncology Group (ECOG) performance status and mean score of FACIT-F was studied, Pearson correlation coefficient was estimated to be 0.271 (P = 0.009).
Conclusions:
FACIT-F is a brief, simple, easy to administer and patient friendly tool to measure the fatigue in last 7 days. CRF should be given adequate attention from the beginning of the treatment to improve the quality of life of cancer patients.
Keywords: Cancer related fatigue, Cronbach's alpha, FACIT-F scale, quality of life
Introduction
The most common side effect of cancer treatment is fatigue. About 80% of patients receiving chemotherapy/radiotherapy experience cancer related fatigue (CRF). Also, sometimes fatigue may be only presenting symptom of cancer. The definition of CRF as given by National Comprehensive Cancer Network is “a distressing persistent, subjective sense of physical, emotional and/or cognitive tiredness or exhaustion related to cancer or cancer treatment that is not proportional to recent activity and interferes with usual functioning”.[1]
A patient may describe the symptoms as feeling very tired, worn out or lack of energy to get-up-and-go. There is an important demarcation between CRF and fatigue experienced by healthy people. CRF occurs even with very less activity and is not relieved by rest and/or sleep. CRF usually decreases after the completion of treatment of cancer; however, it may persist sometimes for months or years. Also, sometimes physician may misjudge CRF to be simply pain which might hamper adequate treatment of this complex symptom. CRF has a profound negative impact on the overall quality of life of cancer patients.[2] CRF assessment in outdoor patients and admitted patients may give conflicting results, CRF being more intense in hospitalized patients. The pathophysiology of CRF is less well understood. It is believed to be multifactorial; the cancer treatment itself being an important etiologic factor besides anaemia, infection, pain and psychosocial factors. Various validated tools are available for the measurement of fatigue; however, there is no gold standard. Functional assessment of chronic illness therapy fatigue scale (FACIT-F, Version-4) is a 13 item, easy to administer questionnaire that can reliably measure the level of fatigue of cancer patients during their daily activities over the past seven days.
Materials and Methods
All subjects participating in the study completed the FACIT-F questionnaire. By scoring convention, after appropriate reverse scoring of 11 items, lower scores on the FACIT-F subscale indicate greater levels of fatigue. Five point likert scale is used to measure the level of fatigue with zero indicating very much fatigued and four stands for not at all fatigued.[3] In this scale, point numbers seven and eight (“I have energy” and “I am able to do my usual activities”) are reversed scored. The score range from 0-52. A score of less than 30 indicates severe fatigue. The higher the score of less 30 indicates severe fatigue. The higher the score an FACIT-F scale, the better is the quality of life. A template for scoring can be downloaded from www.facit.org.
Patient recruitment
92 patients of age 18 years and above attending the oncology OPD from October 2013 to January 2014 who gave informed consent for participation in this questionnaire based study were recruited. The relevant sociodemographic parameters were obtained from the electronic medical records of the patients. The identity of the patients participating in the study and their responses were kept confidential. The subjects were required to return the filled questionnaire on the same day. The patients were not prompted the answers but in case of difficulty in understanding the question or the method of answering, the required explanations were given. In illiterate patients, the literate attendants were allowed to fill the questionnaires on behalf of the patients.
Statistical analysis
The internal consistency of the 13 items on the FACIT-F questionnaire was measured using the Cronbach's alpha. The correlation between the final score and various sociodemographic parameters were also determined by calculating Pearson correlation coefficient. All statistical calculations were performed using SPSS statistical software for windows version 20.0 (Armonk, New York, IBM Corp.).
Results
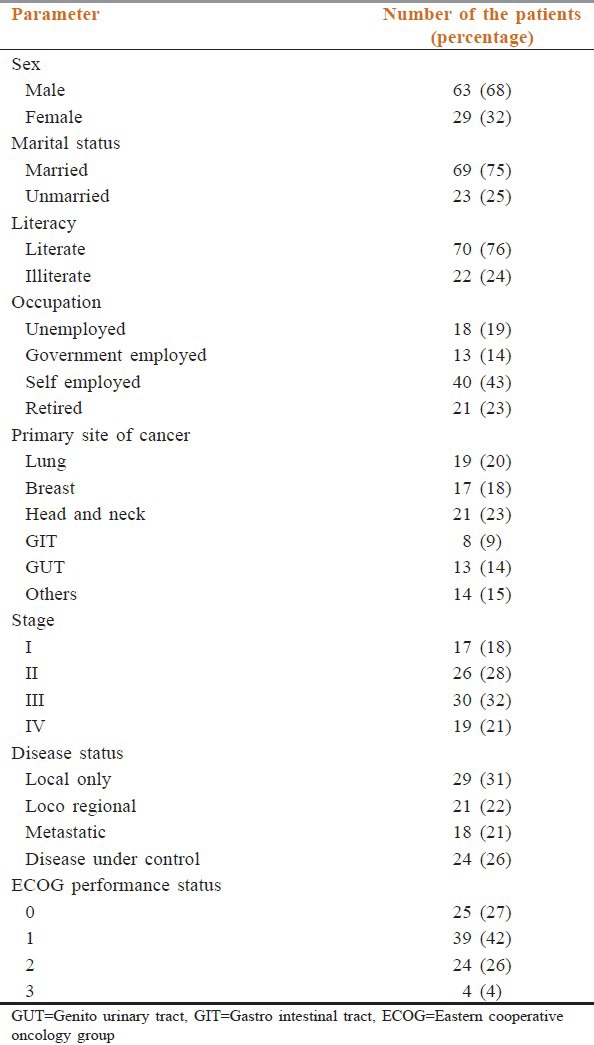
92 patients were found eligible and included in this study. These patients completed the FACIT-F questionnaire. The sociodemographic parameters of the patient cohort, is shown in [Table 1] 68.4% patients were male, 75% married while 76% were illiterate; 22.8% patients had primary of head and neck cancer while 20.6% were suffered from lung cancer, breast cancer suffers constituted 8.5% of the study group. Most of the patients were in advanced stage of diseased stage III (32.6%), stage IV (20.6%), whereas 26% patients had diseased under control at the time of entry in to the study.
Table 1.
Sociodemographic parameters of the patients (n=92)
The total score ranged from 13-46 with mean score of 36 (SD = 3.84). Twenty-one percent patients had score of <30 indicating severe fatigue, 96% of these patients had undergone cancer directed therapy (chemotherapy and radiotherapy), and 82% were in advanced stages of disease. The Cronbach's alpha coefficient for FACIT-F scale encompassing all the items in our study was found to be 0.74. Kendall's coefficient of concordance was estimated to be 0.080. Shows the individual item statistics. The corrected item total correlation ranged from 0.2–0.7 for all the items signifying the importance of each of them. There was only limited variation between the mean and SD values for the individual items that also reinforced the importance of each of the items and excluded the possibility of wide differences between the items. The value of ‘Cronbach's alpha if item deleted’ was found to be lesser than the value of original cronbach's alpha (0.74) for all items; thus, it can be inferred that all the items are essential for the scale and none of the items can be deleted. Analysis of variance (ANOVA) with Tukey's test for non additivity was applied and it revealed highly significant correlation (P ≤ 0.001) between items. Tukey›s estimate of power to which observations must be raised to achieve additivity was found to be 2.285. Hotelling's T squared test also revealed high significance value (P ≤ 0.001). The correlation between Eastern Cooperative Oncology Group (ECOG) performance status and mean score of FACIT-F was studied, Pearson correlation coefficient was estimated to be 0.271 (P = 0.009).
Discussion
About 75% of the cancer patients experience fatigue at least for limited duration.[4,5,6] CRF is not only experienced by patients with active disease[4,7] but also by the survivors.[8,9,10] CRF is an immense problem associated with pervasive disturbance in the quality of life of cancer patients.[11]
Comprehensive cancer care requires the proper control of symptoms as well besides the control of primary disease. Thus, the management of CRF deserves to be a part of treatment in at least 75% of the patients. Unfortunately, CRF is highly neglected both by the patients and the physician and thus, specific CRF directed therapeutic approaches are seldom offered. The CRF issue is highly unaddressed especially in the busy settings with inappropriate doctor patient ratio. There is an important role of social workers in such centers may help in reduction of CRF by the appropriate patient and relatives’ counseling. Even in today's advanced cancer treatment world, cancer pain continues to be under–treated despite the availability of highly effective therapy.[12,13] In this perspective, it is highly unlikely that symptom complex like CRF which is a newly recognized and poorly understood both in terms of pathophysiology and therapeutic options will be treated properly. CRF is under–described in the scientific literature; this should be considered as a major barrier to its improved management. There is an urgent need to train the oncologists to recognize and effectively treat this hidden problem which is a major deterrent to the quality of life of cancer patients.
Despite its very high prevalence among cancer patients, potential negative impact on patients’ activities, and the emotional well-being, research in fatigue is still underdeveloped and there are only a few studies available in the literature reporting on CRF among Indian population.[14] Severity of fatigue was more in chemotherapy and concurrent chemo-radiation group as compare to radiotherapy. Patients who received chemotherapy as their initial treatment were expected to report greater fatigue severity and disruptiveness than patients who received radiotherapy as their initial treatment.[15] Another important perspective of severity of CRF as reported by Stone et al., was its significant association with the depression sub-score of the Hospital Anxiety and Depression Scale, ECOG performance status and disease burden (P < 0.001).[16] Also, they reported higher median fatigue score in patients with lung cancer (41.5) as compared to breast (24) and prostate cancer (24.5). The emotional status and the family background have an important influence on CRF.
There is a threefold problem in the management of CRF. First one is patient related, patients usually do not complain of symptoms of fatigue even if it is severe.[1] This can be circumvented by taking proper history and encourage patients to share their psychosocial problem with the physician besides the physical complaints. Second level of required improvement in CRF management is physician related. The physician should be trained regarding the use of non-pharmacological therapies such as cognitive behavior therapy, graded exercise therapy, pacing besides the use of pharmacological management like antidepressants and psycho stimulants. In the western world, there is also a third problem which is system related; the insurance and reimbursement policies should be modified to cover the expenses of management of CRF and psychosocial problems of a cancer patient. This will constitute a holistic approach in the management of cancer patients covering all the aspects of symptoms complex of this dreaded disease.
FACIT-F scale is a validated scale available in at least 45 different languages. The Cronbach's alpha coefficient data in our patient cohort was 0.74 which validates the scale. Internal consistency reliabilities of the FACIT-F were uniformly high throughout the sample. CRF was correlated with overall qualities of life and ECOG performance status. The correlation between FACIT-F score and ECOG performance status was highly significant (P = 0.007). This could be explained in terms of fatigue worsening with increased need for bed rest, leading to reduced FACIT-F score and higher value of ECOG scale. However, no significant correlation was found with sociodemographic parameters like sex, age, stage, primary site of diseased, occupation, or marital status, thus, verifying the divergent validity of FACIT-F.
Conclusions
Though CRF is ill–managed, there is still a ray of hope that the situation surrounding CRF is reminiscent of cancer pain in the 1980s, which has improved gradually in last 30 years. FACIT-F is a brief, simple, easy to administer and patient friendly tool to measure the fatigue in last 7 days. CRF should be given adequate attention from the beginning of the treatment to improve the quality of life of cancer patients.
Acknowledgments
The authors would like to thank consultants in Department of Oncology Dr. Ajay Sharma, Dr. N Sharma, Dr. S L Jakhar, Dr. R Bothra and Dr. J Nangal. Also, they express gratitude to PG Students of the Department: Dr. Raj K Nirban, Dr. Sitaram, Dr. Daleep, Dr. Guman, Dr. Murali, Dr. Tanya, Dr. Rajesh, and Dr. R Purohit.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.NCCN Clinical Practice Guidelines in Oncology: Cancer-Related Fatigue. Version 1. National Comprehensive Cancer Network. 2014 ed. [Accessed 2014 Feb 10]. Available from: http://www.nccn.org/professionals/physician_gls/pdf/fatigue.pdf .
- 2.Cella D, Peterman A, Passik S, Jacobsen P, Breitbart W. Progress toward guidelines for the management of fatigue. Oncology (Williston Park) 1998;12:369–77. [PubMed] [Google Scholar]
- 3.Webster K, Cella D, Yost K. The functional assessment of chronic illness therapy (FACIT) measurement system: Properties, applications, and interpretation. Health Qual Life Outcomes. 2003;1:1–7. doi: 10.1186/1477-7525-1-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vogelzang NJ, Breitbart W, Cella D, Curt GA, Groopman JE, Horning SJ, et al. Patient, caregiver, and oncologist perceptions of cancer-related fatigue: Results of a tripart assessment survey. The Fatigue Coalition. Semin Hematol. 1997;34(3 Suppl 2):4–12. [PubMed] [Google Scholar]
- 5.Portenoy RK, Thaler HT, Kornblith AB, Lepore JM, Friedlander-Klar H, Coyle N, et al. Symptom prevalence, characteristics, and distress in a cancer population. Qual Life Res. 1994;3:183–9. doi: 10.1007/BF00435383. [DOI] [PubMed] [Google Scholar]
- 6.Ventafridda V, De Conno F, Ripamonti C, Gamba A, Tamburini M. Quality-of-life assessment during a palliative care program. Ann Oncol. 1990;1:415–20. doi: 10.1093/oxfordjournals.annonc.a057794. [DOI] [PubMed] [Google Scholar]
- 7.Dunlop GM. A study of the relative frequency and importance of gastrointestinal symptoms and weakness in patients with far-advanced cancer: Student paper. Palliat Med. 1989;4:37–43. [Google Scholar]
- 8.Joly F, Henry-Amar M, Arveux P, Reman O, Tanguy A, Peny AM, et al. Late psychosocial sequelae in Hodgkin's disease survivors: A French population-based case-control study. J Clin Oncol. 1996;14:2444–53. doi: 10.1200/JCO.1996.14.9.2444. [DOI] [PubMed] [Google Scholar]
- 9.Berglund G, Bolund C, Fornander T, Rutqvist LE, Sjödén PO. Late effects of adjuvant chemotherapy and postoperative radiotherapy on quality of life among breast cancer patients. Eur J Cancer. 1991;27:1075–81. doi: 10.1016/0277-5379(91)90295-o. [DOI] [PubMed] [Google Scholar]
- 10.Okuyama T, Akechi T, Kugaya A, Okamura H, Imoto S, Nakano T, et al. Factors correlated with fatigue in disease-free breast cancer patients: Application of the Cancer Fatigue Scale. Support Care Cancer. 2000;8:215–22. doi: 10.1007/s005200050288. [DOI] [PubMed] [Google Scholar]
- 11.Portenoy RK. Cancer-related fatigue: An immense problem. Oncologist. 2000;5:350–2. doi: 10.1634/theoncologist.5-5-350. [DOI] [PubMed] [Google Scholar]
- 12.Bernabei R, Gambassi G, Lapane K, Landi F, Gatsonis C, Dunlop R, et al. Management of pain in elderly patients with cancer. SAGE Study Group. Systematic Assessment of Geriatric Drug Use via Epidemiology. JAMA. 1998;279:1877–82. doi: 10.1001/jama.279.23.1877. [DOI] [PubMed] [Google Scholar]
- 13.Pargeon KL, Hailey BJ. Barriers to effective cancer pain management: A review of the literature. J Pain Symptom Manage. 1999;18:358–68. doi: 10.1016/s0885-3924(99)00097-4. [DOI] [PubMed] [Google Scholar]
- 14.Karthikeyan G, Jumnani D, Prabhu R, Manoor UK, Supe SS. Prevalence of fatigue among cancer patients receiving various anticancer therapies and its impact on quality of Life: A cross-sectional study. Indian J Palliat Care. 2012;18:165–75. doi: 10.4103/0973-1075.105686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schmidt ME, Chang-Claude J, Vrieling A, Heinz J, Flesch-Janys D, Steindorf K. Fatigue and quality of life in breast cancer survivors: Temporal courses and long-term pattern. J Cancer Surviv. 2012;6:11–9. doi: 10.1007/s11764-011-0197-3. [DOI] [PubMed] [Google Scholar]
- 16.Stone P, Richards M, A’Hern R, Hardy J. A study to investigate the prevalence, severity and correlates of fatigue among patients with cancer in comparison with a control group of volunteers without cancer. Ann Oncol. 2000;11:561–7. doi: 10.1023/a:1008331230608. [DOI] [PubMed] [Google Scholar]


