Abstract
Cardiac papillary fibroelastoma is a rare, benign tumor, arising predominantly from cardiac valves. This tumor can cause a variety of symptoms due to thromboembolism. We describe our single-center surgical experience with papillary fibroelastoma of the aortic valve.
From April 2004 through June 2013, 6,530 patients underwent cardiac surgery. Of those, 6,098 patients were included in the final analysis. Twenty-one patients (0.34%) underwent surgical resection of 30 papillary fibroelastomas of the aortic valve.
Most patients (67%) were incidentally diagnosed to have cardiac papillary fibroelastoma. The usual symptom was cerebral infarction (in 5 of 7 symptomatic patients). A rare presentation of papillary fibroelastoma in one patient was cardiac arrest caused by left main coronary artery ostial obstruction. Tumor size was not related to patient age (Pearson correlation coefficient, 0.34; P=0.13). Neither the number of tumors (1.43 ± 0.72 vs 1.43 ± 0.62) nor tumor size (8.14 ± 2.42 vs 8.07 ± 3.31 mm) was significantly different between symptomatic and asymptomatic patients. All lesions were resected by means of the simple shave technique. There were no operative or 30-day deaths. Follow-up echocardiograms showed no tumor recurrence (mean follow-up duration, 17 ± 14 mo).
We identified no significant relationship among tumor size, number of tumors, symptoms, or patient age. Because simple shave excision of the tumor can be safely achieved without evidence of tumor recurrence, we conclude that surgical resection can be reasonable in asymptomatic patients.
Keywords: Aortic valve/surgery, cardiac surgical procedures, chest pain/etiology, fibroma/complications/diagnosis/pathology/surgery, heart neoplasms/complications/surgery/ultrasonography, heart valve diseases/pathology, myocardial infarction/etiology, retrospective studies, treatment outcome
Primary cardiac tumors are rare, with an approximate prevalence of 0.02% in an autopsy study1 and 0.45% in an open-heart surgical study.2 Cardiac papillary fibroelastoma (CPF) is a benign endocardial papilloma. This lesion is the second most prevalent primary cardiac tumor2 and the most prevalent valvular tumor.3 The aortic valve (AV) is most often affected.4 Cardiac papillary fibroelastomas are frequently asymptomatic but can cause ischemic or thromboembolic symptoms. The typical clinical manifestations are cardiac or neurologic, including transient ischemic attack, stroke, angina, myocardial infarction, sudden death, heart failure, syncope, and blindness.4 Life-threatening events such as cardiac arrest and sudden death are rarely consequences of CPFs.5,6
In symptomatic patients, surgical resection of CPF is recommended, to prevent further ischemic or thromboembolic events. When these tumors are found incidentally during preoperative evaluation for cardiac surgery, their removal is reasonable, to prevent unexpected complications. When an incidental finding is the only potential indication for cardiac surgery, surgical intervention is a matter of debate.
This study, which focused on CPFs on the AV, describes the perioperative clinical characteristics of affected patients, characterizes the echocardiographic findings of CPFs, summarizes surgical treatment, and evaluates the midterm outcomes of CPF patients after surgical resection. In addition, we present a rare case in which a CPF obstructed the left main coronary artery (LMCA) ostium and caused cardiac arrest.
Patients and Methods
The data for this study were obtained retrospectively from the Bluhm Cardiovascular Institute's Clinical Trial Unit's Cardiovascular Research Database. Our use of this database was approved by the institutional review board at Northwestern University. Any subjects who refused participation in the project were not included in the analysis. From April 2004 through June 2013, 6,530 patients underwent cardiac surgery; of these, 6,098 were included in the study. Preoperative, operative, and postoperative variables were retrieved from the database, and echocardiographic reports, operative procedural notes, and histopathologic reports were reviewed. The clinical diagnosis of CPF was made by means of transthoracic echocardiography (TTE), transesophageal echocardiography (TEE), or both, and was confirmed by means of histopathologic review of the surgical specimen in all patients.
Statistical Analysis
Differences in data between symptomatic and asymptomatic patients were compared by means of the 2-sample Student t test or Mann-Whitney U test. The χ2 test was used for comparisons of qualitative data. Correlation was evaluated by means of the Pearson correlation. P <0.05 was considered statistically significant, and there were no multiplicity adjustments. For statistical analysis of the findings, we used SPSS Statistics version 22 (IBM Corporation; Armonk, NY).
Results
Twenty-seven patients were diagnosed with CPF of the AV preoperatively or intraoperatively, by means of TTE or TEE. Of those 27 patients, 21 (78%) were histopathologically confirmed to have CPF. The prevalence of CPF of the AV in the entire study group was 0.34%. There were 30 lesions in the 21 patients.
Preoperative Findings. Table I shows the preoperative findings. The mean age of the patients at the time of surgical resection was 63 ± 14 years (range, 29–80 yr). Most patients were female (67%). The chief CPF-related symptoms were cerebral infarction in 5 patients (24%) and angina in 2 patients (10%). One patient with angina presented with cardiac arrest. The lesion was incidentally discovered in 14 patients (67%). Table II shows the baseline characteristics of the 7 symptomatic CPFs in comparison with the 14 asymptomatic (incidentally found) CPFs. Clinical presentations in the asymptomatic patients were dyspnea caused by valvular heart disease (in 6 patients), chest pain caused by coronary artery disease (2 patients), palpitations caused by atrial fibrillation (1 patient), and no symptoms (5 patients). Two of the asymptomatic CPFs were found on intraoperative TEE during coronary artery bypass grafting; the others were incidentally found during TTE or TEE screening for renal transplantation, investigation of abnormal electrocardiographic (ECG) results, and paroxysmal atrial fibrillation.
TABLE I.
Characteristics and Findings in the 21 Patients with Aortic Valve Tumors
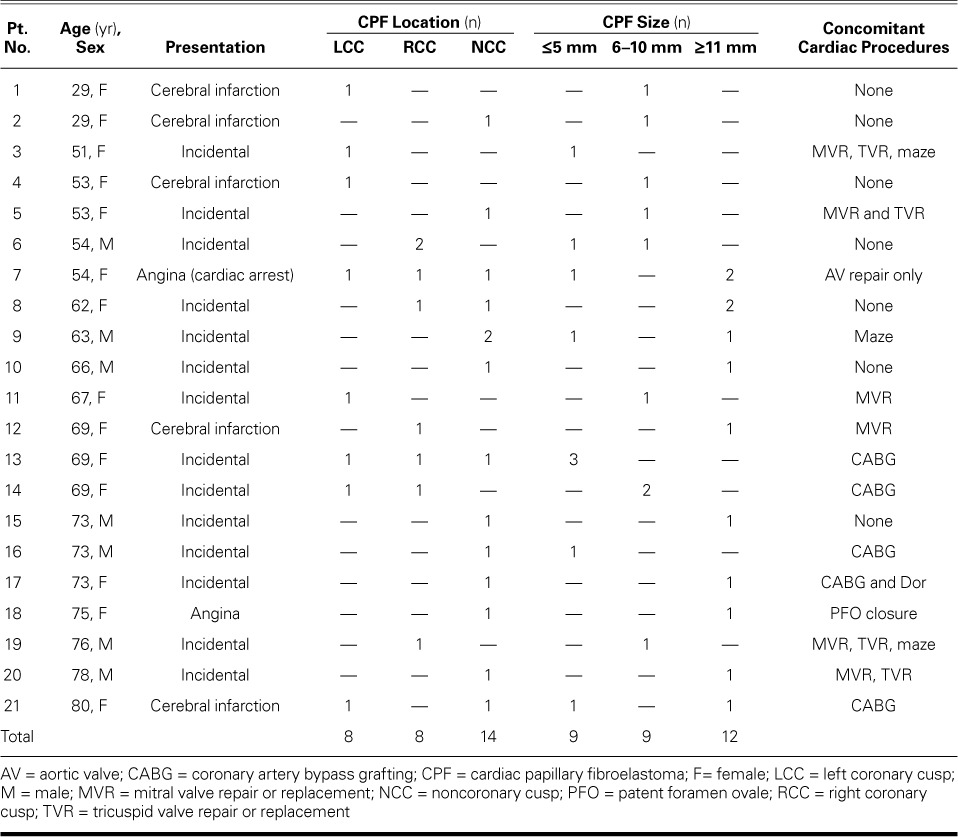
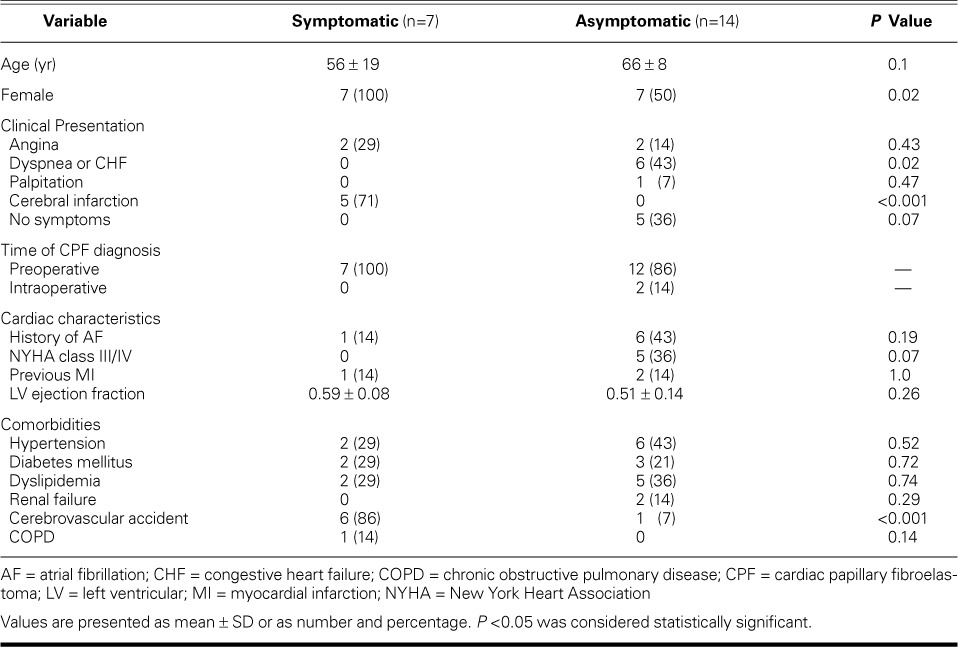
TABLE II.
Baseline Characteristics of the 21 Patients with CPF, in Accordance with Symptom Status
Echocardiographic and Intraoperative Findings. Table I shows the echocardiographic and intraoperative findings. The noncoronary cusp of the AV was involved most often. Solitary lesions were found in 14 patients, 2 or 3 lesions (in multiple cusps) in 5 patients, and 2 lesions (in one cusp) in 2 patients. The mean number of lesions was 1.43 ± 0.72 in tumor-related symptomatic patients and 1.43 ± 0.62 in asymptomatic patients (P=0.86, Mann-Whitney U test).
Lesion size (range, 3–13 mm) was measured during preoperative or intraoperative echocardiography; Table I shows the maximal diameters. Lesion size was not correlated with patient age (Pearson correlation coefficient, 0.34; P=0.13) (Fig. 1). The mean lesion size was 8.14 ± 2.42 mm in symptomatic patients and 8.07 ± 3.31 mm in asymptomatic patients (P=0.96, Student t test).
Fig. 1.

Graph shows the relationship between size of the cardiac papillary fibroelastoma and patient age (Pearson correlation coefficient, 0.34; P=0.13). P <0.05 was considered statistically significant.
Surgical Considerations. All 30 lesions were removed by means of simple shave excision. In 7 patients, CPF resection was the only reason for surgery (Table I).
Two 29-year-old women presented with recent cerebral infarction caused by CPF of the AV. These CPFs were safely resected through upper hemisternotomies by means of minimally invasive approaches.
Postoperative Findings. There were no operative or 30-day deaths, and no in-hospital thromboembolic events were detected. Outpatient echocardiograms, obtained in 8 patients after a mean duration of 17 ± 14 months (range, 2–48 mo), revealed no tumor recurrence.
A Presentation with Cardiac Arrest
A 54-year-old woman with a 2-week history of chest pain presented at the emergency department with chest pain that had occurred during an outpatient stress test. Her medical history included type 1 diabetes mellitus, hypertension, and hyperlipidemia. During the stress test, an ECG had shown deep ST-segment depressions in leads II, III, and aVF, and ST-segment elevation in lead aVR. Upon the patient's arrival at the emergency department, her chest pain had resolved and the ECG patterns had returned to baseline. However, during evaluation, she sustained a cardiac arrest and was resuscitated. When questioned, the patient reported a previous diagnosis of several masses on her AV. She was scheduled for emergency surgery.
The preoperative differential diagnoses were vegetation, thrombus, and dissection of the coronary ostia, as well as CPFs attached to the AV. Intraoperative TEE showed several highly mobile masses on the patient's AV. She underwent a median sternotomy and was placed on cardiopulmonary bypass (CPB) with antegrade and retrograde administration of cardioplegic solution. An oblique aortotomy was performed. Three separate papillomatous lesions were discovered. Two of the lesions were on the aortic leaflets, one each on the left coronary cusp (LCC) and noncoronary cusp, and were approximately 1 cm in diameter. The 3rd lesion was smaller and was found on the right coronary cusp. The mass on the free edge of the LCC was intermittently obstructing the LMCA orifice (Fig. 2). The patient's aorta was free of disease. There was no thrombus. Each lesion was carefully removed in its entirety. After the patient was weaned from CPB, her ventricular function was normal, compared with a preoperative left ventricular ejection fraction of 0.35 when the mass had intermittently obstructed the LMCA. Histopathologic analysis revealed benign papillary tumors, consistent with CPFs. The patient had an uneventful recovery.
Fig. 2.

Patient 7. Intraoperative photograph shows a cardiac papillary fibroelastoma on the free edge of the left coronary cusp.
Discussion
This study describes 30 CPFs of the AV, observed in 21 patients. All tumors were resected without sequelae. First, we analyzed the perioperative clinical characteristics of the patients. Clinically, CPFs are found only when they cause a symptom or when echocardiography is performed. The true prevalence of CPF is unknown, although advances in echocardiographic technology during the last few decades have resulted in its detection in an increasing number of patients. The true ratio of symptomatic to asymptomatic events is also unknown. This study showed that tumors were found incidentally, preoperatively or intraoperatively, in 67% of our CPF patients. The lesion can cause symptoms due to thromboembolization of the tumor itself or to the thrombus produced on the tumor surface; however, it is unclear whether thromboembolization is more likely to originate from a thrombus formed on the tumor or in a part of the CPF itself. Symptoms usually occur only when the tumor or thrombus is large enough to cause them and embolizes to a key location, such as the heart or the brain. In this study, all the tumor-related symptoms were cardiac or neurologic. Most previous studies have shown that CPFs tend to be found in men;4 however, some case series have shown a female predominance,7,8 as does our study.
Second, we have described the echocardiographic findings of CPFs. Our results are mostly consistent with those in the medical literature. Most tumors were solitary, and all were smaller than 20 mm in diameter.
To our knowledge, no investigators have reported long-term echocardiographic follow-up information for medically treated patients with CPF. The natural history of this type of tumor is largely unknown. Several authors have suggested that CPF tends to grow slowly over time.9–11 However, in our study, tumor size was not significantly correlated with patient age.
Third, we have described the surgical treatment of CPF of the AV, including the cases of the two 29-year-old women who presented with cerebral infarction. In symptomatic patients, surgical resection should be performed, to prevent further ischemic or thromboembolic events. Simple shave excision was safely achieved in all our patients. When CPF is found incidentally during preoperative cardiac evaluation, removal is reasonable, to prevent unexpected thromboembolic events perioperatively. When the incidental finding of tumors is the only indication for cardiac surgery, the choice of appropriate treatment—surgical or medical—is a matter of debate. Oral anticoagulation can be the treatment of choice if the tumor is not mobile or if valve replacement is strongly expected at the time of tumor resection. In the cases of 25 medically treated CPF patients, Gowda and colleagues4 reported tumor-related death in 12 of them. We recommend surgical treatment for patients in whom CPF is found incidentally.
Fourth, we have evaluated midterm outcomes after the surgical resection of CPF. The operative and 30-day survival rates in our patients were 100%, and we observed no tumor recurrence during follow-up evaluations.
Anastacio and colleagues7 reported a rare instance of CPF recurrence in a patient whose history of Hodgkin lymphoma had necessitated chest radiation. Cardiac papillary fibroelastomas were initially resected from the patient's right atrium and pulmonary valve. Three months later, a new 1 × 0.7-cm lesion was found and was resected from the patient's AV. Histopathologic results confirmed the diagnosis of CPF.
Cardiac papillary fibroelastomas are generally acquired and slow-growing; however, their cause is unknown. Kurup and colleagues8 reported on 12 autopsy cases and pointed out the relationships between CPF and previous cardiac surgery or radiation to the chest. In our study, 3 patients (14%) had undergone open-heart surgery, but none had a history of radiation therapy.
Fifth, we have reported a rare case of cardiac arrest from LMCA ostial obstruction caused by a CPF. Cardiac papillary fibroelastomas can cause a wide variety of embolic manifestations, and it is well known that they can cause acute coronary syndrome.12,13 The patient presented with severe coronary ischemia and progressed to cardiac arrest, for which she was resuscitated. Multiple highly mobile CPFs were found on all the coronary cusps, notably the approximately 1-cm mass on the LCC that intermittently occluded the LMCA ostium. To our knowledge, this is the first report of survival after cardiac arrest caused by CPF.
The friability, mobility, and location of CPFs should be evaluated in order to help the physician decide the indication and timing of surgery. The patient's clinical history might indicate tumor friability, and an echocardiogram might reveal mobility and location. Early surgery is recommended if the CPF is symptomatic, fairly mobile, or close to the coronary ostia.
Limitations of our study include its retrospective and single-center nature, although follow-up was prospective. The surgical procedures were performed by multiple surgeons. Cardiac papillary fibroelastoma was suspected only when echocardiography was performed, so the true prevalence and natural history of this tumor in our patients is unknown. The small number of patients was the most important limitation of this study.
Because simple shave excision of CPFs can be safely achieved, we conclude that surgical resection can be reasonable in asymptomatic patients.
Footnotes
From: Division of Cardiac Surgery, Bluhm Cardiovascular Institute, Northwestern University Feinberg School of Medicine and Northwestern Memorial Hospital, Chicago, Illinois 60611
References
- 1.Reynen K. Frequency of primary tumors of the heart. Am J Cardiol. 1996;77(1):107. doi: 10.1016/s0002-9149(97)89149-7. [DOI] [PubMed] [Google Scholar]
- 2.Steger CM, Hager T, Ruttmann E. Primary cardiac tumors: a single-center 41-year experience. ISRN Cardiol. 2012;2012:906109. doi: 10.5402/2012/906109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Edwards FH, Hale D, Cohen A, Thompson L, Pezzella AT, Virmani R. Primary cardiac valve tumors. Ann Thorac Surg. 1991;52(5):1127–31. doi: 10.1016/0003-4975(91)91293-5. [DOI] [PubMed] [Google Scholar]
- 4.Gowda RM, Khan IA, Nair CK, Mehta NJ, Vasavada BC, Sacchi TJ. Cardiac papillary fibroelastoma: a comprehensive analysis of 725 cases. Am Heart J. 2003;146(3):404–10. doi: 10.1016/S0002-8703(03)00249-7. [DOI] [PubMed] [Google Scholar]
- 5.Her AY, Kim YH, Heo JW, Yie K, Lee S. Papillary fibroelastoma of the aortic valve with atypical chest pain: late presentation with acute myocardial infarction and cardiac arrest. J Card Surg. 2012;27(3):327–30. doi: 10.1111/j.1540-8191.2011.01385.x. [DOI] [PubMed] [Google Scholar]
- 6.Bussani R, Silvestri F. Images in cardiovascular medicine. Sudden death in a woman with fibroelastoma of the aortic valve chronically occluding the right coronary ostium. Circulation. 1999;100(21):2204. doi: 10.1161/01.cir.100.21.2204. [DOI] [PubMed] [Google Scholar]
- 7.Anastacio MM, Moon MR, Damiano RJ, Jr, Pasque MK, Maniar HS, Lawton JS. Surgical experience with cardiac papillary fibroelastoma over a 15-year period. Ann Thorac Surg. 2012;94(2):537–41. doi: 10.1016/j.athoracsur.2012.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kurup AN, Tazelaar HD, Edwards WD, Burke AP, Virmani R., Klarich KW, Orszulak TA. Iatrogenic cardiac papillary fibroelastoma: a study of 12 cases (1990 to 2000) Hum Pathol. 2002;33(12):1165–9. doi: 10.1053/hupa.2002.130105. [DOI] [PubMed] [Google Scholar]
- 9.Levinsky L, Srinivasan V, Gingell RL, Fisher JE, Pieroni DR, Choh JH, Subramanian S. Papillary fibroelastoma of aortic and mitral valves following myectomy for idiopathic hypertrophic subaortic stenosis. Thorac Cardiovasc Surg. 1981;29(3):187–91. doi: 10.1055/s-2007-1023474. [DOI] [PubMed] [Google Scholar]
- 10.Cesena FH, Pereira AN, Dallan LA, Aiello VD, Mansur AJ. Papillary fibroelastoma of the mitral valve 12 years after mitral valve commissurotomy. South Med J. 1999;92(10):1023–8. doi: 10.1097/00007611-199910000-00017. [DOI] [PubMed] [Google Scholar]
- 11.Joffe II, Jacobs LE, Owen AN, Ioli A, Kotler MN. Rapid development of a papillary fibroelastoma with associated thrombus: the role of transthoracic and transesophageal echocardiography. Echocardiography. 1997;14(3):287–92. doi: 10.1111/j.1540-8175.1997.tb00724.x. [DOI] [PubMed] [Google Scholar]
- 12.Raju V, Srinivasan M, Padmanaban C, Soundararajan S, Kuppanna PJ. Left main coronary artery embolus: unusual presentation of papillary fibroelastoma of the aortic valve. Tex Heart Inst J. 2010;37(3):365–7. [PMC free article] [PubMed] [Google Scholar]
- 13.Erdoes G, Stalder M, Basciani R, Gugger M, Carrel T, Eberle B. An uncommon cause of coronary artery ostial obstruction: papillary fibroelastoma. Echocardiography. 2010;27(3):337–40. doi: 10.1111/j.1540-8175.2009.01087.x. [DOI] [PubMed] [Google Scholar]


