Abstract
A 46-year-old man with a history of paranoid schizophrenia was admitted with a recurrence of psychotic symptoms. Improvement was noted after the initiation of clozapine. After 2 weeks of clozapine therapy, chest pressure and abnormal cardiac biomarkers (in the presence of a normal coronary angiogram) raised suspicion of myocarditis. That diagnosis was confirmed by means of cardiac magnetic resonance imaging. Discontinuation of the clozapine led to resolution of the cardiac symptoms. Clozapine-induced myocarditis is rare and can be missed for lack of specific clinical findings. In order to prevent disease progression and a possibly fatal outcome, early recognition of the condition and prompt discontinuation of clozapine are necessary.
Keywords: Antipsychotic agents/adverse effects, cardiac magnetic resonance imaging, clozapine, myocarditis/chemically induced, schizophrenia/drug therapy
Myocarditis is a rare but potentially life-threatening sequela of the administration of clozapine, a highly effective 2nd-generation antipsychotic drug. Establishing an early diagnosis is crucial to improving outcomes. We describe the case of a middle-aged man who developed myocarditis after the initiation of clozapine therapy for paranoid schizophrenia. Our report focuses on the optimal diagnostic and therapeutic options for the management of clozapine-induced myocarditis.
Case Report
A 46-year-old man was admitted to the psychiatry unit with homicidal ideations and auditory hallucinations. His medical history was significant for hyperlipidemia and paranoid schizophrenia. There was no history of alcohol or tobacco use or of illicit-substance abuse (including cocaine). The patient had 3 previous admissions for delusional behavior despite his attempts at control with medications that included escitalopram, risperidone, and olanzapine.
For his presenting symptoms, the patient was started on haloperidol, with no response. Therefore, the regimen was changed to clozapine, at a dosage that was gradually increased to 150 mg twice daily, with progressive improvement in his symptoms. However, after 2 weeks of that therapy, the patient developed recurrent episodes, at rest, of intermittent, midsternal chest pressure, which was aggravated by lying flat. There was no associated dyspnea, fever, chills, cough, vomiting, or diarrhea. His blood pressure was 84/54 mmHg, his heart rate was 110 beats/min, and his oxygen saturation was normal on pulse oximetry. Auscultation revealed a loud S1 with no rubs, and normal breath sounds. A 12-lead electrocardiogram showed sinus tachycardia, a normal QTc interval, and no ST-segment abnormalities. Cardiac biomarkers included an initial serum cardiac troponin I level of 2.1 ng/mL (normal, <0.12 ng/mL), which subsequently peaked at 5 ng/mL.
In view of the possibility of acute coronary syndrome, the patient was admitted to the cardiac telemetry unit. Echocardiography revealed normal left ventricular (LV) size, normal systolic function (LV ejection fraction [LVEF], 0.60), and possible mild hypokinesis of the LV mid anterolateral wall. Coronary angiography showed normal coronary arteries. Therefore, myocarditis was suspected, and cardiac magnetic resonance imaging (CMR) was performed. Gadolinium-enhanced images showed a small area of late gadolinium enhancement in the anterolateral subepicardium (Fig. 1), which suggested nonischemic fibrosis or scar consistent with a diagnosis of myocarditis.
Fig. 1.
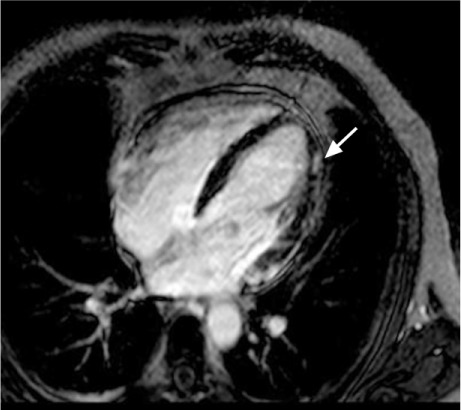
Gadolinium-enhanced cardiac magnetic resonance image shows a small area of late enhancement (arrow) within the anterolateral left ventricular epicardium, with sparing of the endocardium. This is nonischemic fibrosis or scar, consistent with focal myocarditis.
Suspecting clozapine-induced myocarditis, we discontinued clozapine and replaced it with fluphenazine, a first-generation antipsychotic. Because of the predisposition of myocarditis to cardiac arrhythmias, we monitored the patient with cardiac telemetry and initiated a regimen of angiotensin-converting-enzyme inhibitor and β-blocker therapy. After 48 hours of monitoring, the patient's cardiac condition remained stable, at which point he was transferred back to the psychiatry unit and was subsequently discharged from the hospital. He was doing well when he returned for an outpatient visit, 6 weeks after discharge.
Discussion
Our patient had clozapine-induced myocarditis. Clozapine is a highly effective 2nd-generation antipsychotic agent used in the treatment of schizophrenia and other refractory psychotic disorders. Among patients taking clozapine, the incidence of clozapine-induced myocarditis is approximately 1%, and most cases occur within the first 2 months of treatment.1 Among affected patients, the commonly observed findings of peripheral eosinophilia, and of eosinophilic inclusions within endomyocardial biopsy samples, have led to the suggestion that clozapine-induced myocarditis is an immunoglobulin E-mediated hypersensitivity reaction.2 However, these findings are not reliable. Other investigators, on the basis of higher noradrenaline levels noted in patients treated with clozapine, have proposed that increased plasma noradrenaline levels are the probable mechanism of cardiac dysfunction.3 Nonetheless, the definitive mechanisms by which clozapine causes cardiotoxicity remain unclear. The clinical features are often nonspecific and can include chest discomfort, tachycardia, hypotension, arrhythmias, and signs of heart failure. Although electrocardiographic findings and serum cardiac biomarkers are abnormal when muscle damage from myocarditis is significant, these discoveries are nondiagnostic.
Two-dimensional echocardiography might provide a clue to the presence of myocarditis by revealing regional wall-motion abnormalities that do not match coronary vascular territories. However, in the presence of less extensive disease, echocardiography might be unhelpful.
The diagnostic imaging method of choice for myocarditis is CMR. The characteristic finding in myocarditis is a focal enhancement of the myocardium that correlates extremely well with a histologic finding of active myocarditis.4 With the use of T2-weighted imaging protocols, myocarditis can be diagnosed with a sensitivity of 84% and a specificity of 74%.5 The sensitivity can be further increased, to greater than 90%, with the use of gadolinium-based contrast agents.6 The criteria for diagnosis of myocarditis by CMR include at least 2 of the following indicators of inflammation: 1) increased regional or global myocardial signaling intensity in T2-weighted images; 2) increased early gadolinium-enhanced T1-weighted images in the global myocardium; and 3) at least one focal lesion that shows nonischemic regional distribution of late gadolinium enhancement.7 Cardiac magnetic resonance is useful in follow-up, because it enables monitoring for signs of resolution and changes in LVEF.4 Magnetic resonance imaging can also play a role in distinguishing myocarditis from myocardial infarction, which has a similar clinical presentation. In myocarditis, the infiltrates are characteristically located in the mid wall and the subendocardium is spared, whereas in myocardial infarction, the subendocardium typically is involved first.
The current gold standard for the diagnosis of myocarditis is endomyocardial biopsy. Although the absence of a biopsy-proven diagnosis is a limitation in our patient's case, endomyocardial biopsy—as a “blind” invasive procedure—has both inherent risks and limitations. It can be insensitive to the presence of focal myocarditis. The earliest location of myocardial inflammatory changes (as shown by CMR) is in the lateral wall of the LV, which standard biopsy techniques can easily miss.4 Consequently, endomyocardial biopsy is not universally recommended in the diagnosis of myocarditis.8 Yet imaging methods can be used to guide targeted sampling of myocardial lesions. Such measures might improve the diagnostic yield by providing the true incidence of clozapine-induced myocarditis, which is likely to be higher than the incidence currently reported.
Outcomes of clozapine-induced myocarditis are poor, with mortality rates as high as 50%.9 Early recognition of the condition—and prompt discontinuation of the offending agent—are crucial. Lower patient exposures to clozapine are associated with lower mortality rates. Rechallenging patients with clozapine is associated with high mortality rates (although this conclusion arises from an isolated case series10).
Footnotes
From: Department of Internal Medicine (Dr. Hatton) and Heart and Vascular Center (Drs. Bhat and Gandhi), MetroHealth Campus of Case Western Reserve University, Cleveland, Ohio 44109
Dr. Bhat is now at Cardiovascular Consultants, Ltd., Phoenix, Arizona.
References
- 1.Haas SJ, Hill R, Krum H, Liew D, Tonkin A, Demos L et al. Clozapine-associated myocarditis: a review of 116 cases of suspected myocarditis associated with the use of clozapine in Australia during 1993–2003. Drug Saf. 2007;30(1):47–57. doi: 10.2165/00002018-200730010-00005. [DOI] [PubMed] [Google Scholar]
- 2.Kilian JG, Kerr K, Lawrence C, Celermajer DS. Myocarditis and cardiomyopathy associated with clozapine. Lancet. 1999;354(9193):1841–5. doi: 10.1016/s0140-6736(99)10385-4. [DOI] [PubMed] [Google Scholar]
- 3.Elman I, Goldstein DS, Eisenhofer G, Folio J, Malhotra AK, Adler CM et al. Mechanism of peripheral noradrenergic stimulation by clozapine. Neuropsychopharmacology. 1999;20(1):29–34. doi: 10.1016/S0893-133X(98)00047-5. [DOI] [PubMed] [Google Scholar]
- 4.Mahrholdt H, Goedecke C, Wagner A, Meinhardt G, Athanasiadis A, Vogelsberg H et al. Cardiovascular magnetic resonance assessment of human myocarditis: a comparison to histology and molecular pathology. Circulation. 2004;109(10):1250–8. doi: 10.1161/01.CIR.0000118493.13323.81. [DOI] [PubMed] [Google Scholar]
- 5.Abdel-Aty H, Boye P, Zagrosek A, Wassmuth R, Kumar A, Messroghli D et al. Diagnostic performance of cardiovascular magnetic resonance in patients with suspected acute myocarditis: comparison of different approaches. J Am Coll Cardiol. 2005;45(11):1815–22. doi: 10.1016/j.jacc.2004.11.069. [DOI] [PubMed] [Google Scholar]
- 6.Liu PP, Yan AT. Cardiovascular magnetic resonance for the diagnosis of acute myocarditis: prospects for detecting myocardial inflammation. J Am Coll Cardiol. 2005;45(11):1823–5. doi: 10.1016/j.jacc.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 7.Friedrich MG, Sechtem U, Schulz-Menger J, Holmvang G, Alakija P, Cooper LT et al. Cardiovascular magnetic resonance in myocarditis: a JACC white paper. J Am Coll Cardiol. 2009;53(17):1475–87. doi: 10.1016/j.jacc.2009.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cooper LT, Baughman KL, Feldman AM, Frustaci A, Jessup M, Kuhl U et al. The role of endomyocardial biopsy in the management of cardiovascular disease: a scientific statement from the American Heart Association, the American College of Cardiology, and the European Society of Cardiology. Endorsed by the Heart Failure Society of America and the Heart Failure Association of the European Society of Cardiology. J Am Coll Cardiol. 2007;50(19):1914–31. doi: 10.1016/j.jacc.2007.09.008. [DOI] [PubMed] [Google Scholar]
- 9.Hagg S, Spigset O, Bate A, Soderstrom TG. Myocarditis related to clozapine treatment. J Clin Psychopharmacol. 2001;21(4):382–8. doi: 10.1097/00004714-200108000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Manu P, Sarpal D, Muir O, Kane JM, Correll CU. When can patients with potentially life-threatening adverse effects be rechallenged with clozapine? A systematic review of the published literature. Schizophr Res. 2012;134(2–3):180–6. doi: 10.1016/j.schres.2011.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]


