Abstract
Anti–N-methyl-D-aspartate (NMDA) receptor encephalitis is a rare panencephalitis that can present with severe cardiac dysrhythmias. We present a case of a 19-year-old woman with no significant medical history who presented with progressive changes in mental status and profound ictal asystole that necessitated the placement of an external temporary pacemaker. She was diagnosed with and treated for anti-NMDA receptor encephalitis, and she recovered after a prolonged and complicated hospitalization. We review the pathophysiology and management of anti-NMDA receptor encephalitis, as well as its cardiac manifestations.
Keywords: Anti-N-methyl-D-aspartate receptor encephalitis/complications/diagnosis/etiology/therapy; asystole; delirium, dementia, amnestic, cognitive disorders/immunology; disease progression; female; heart block; immunosuppressive agents/therapeutic use; immunotherapy/methods; ovarian neoplasms/complications; paraneoplastic syndromes, nervous system; syncope, vasovagal/etiology; teratoma/complications
The clinical entity of anti–N-methyl-d-aspartate (NMDA) receptor encephalitis was first described in 2007.1 Although more than 600 cases of anti-NMDA receptor encephalitis have been reported since that time, the entity remains before a definitive diagnosis can be reached.2 This malady is a rare, immunotherapy-responsive panencephalitis that typically presents with psychiatric manifestations and movement disorders, which can be fatal. Most patients are young women with ovarian teratomas, although there are reports of affected children and men who have no identifiable tumors. Rarely, ictal asystole occurs among epileptic patients. Case series suggest that anti-NMDA receptor encephalitis patients, in general, are at increased risk of cardiac dysrhythmia. After treatment of the encephalitis, dysrhythmias usually resolve and permanent pacing is not required.
Case Report
In December 2012, a 19-year-old woman with a history of migraine headaches presented at our emergency department (ED) after an apparent seizure. She stated that her last memory before her suspected seizure was of solving an extended problem on a classroom blackboard while preparing for final examinations. Her next memory was of awakening in the ED. While in the ED, she experienced a witnessed, generalized tonic-clonic seizure and was given intravenous lorazepam and phenytoin. An electrocardiogram was notable only for mild QT prolongation and sinus rhythm (Fig. 1). The results of routine laboratory examinations and magnetic resonance angiography of the brain were not helpful. Two weeks before her ED visit, the patient had reported constant headaches, accompanied by a burning sensation in her head that went down her nose and into her chest, lasting an hour at a time. These episodes had recurred a few times per week. She also had reported facial and hand tingling during these same episodes. After her discharge from the ED and her outpatient follow-up with neurology, she reported difficulty thinking, emotional lability (laughing, crying, and thoughts of impending doom), memory problems, and the intermittent hearing of music. Upon leaving the neurology clinic, she was prescribed levetiracetam and was scheduled for outpatient electroencephalography (EEG), in an effort to evaluate her seizure activity.
Fig. 1.
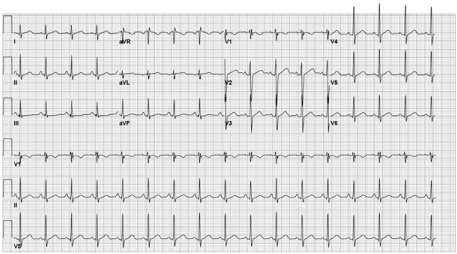
Patient's electrocardiogram on admission shows mild QT prolongation and sinus rhythm.
Two days after her outpatient neurology visit, she underwent an EEG that revealed status epilepticus, originating from the right mid-temporal region. She was then admitted to the hospital for evaluation of those seizures. She was afebrile on presentation, and her vital signs fell within normal limits. On neurologic examination, she was alert, oriented, and able to follow commands. She was laughing inappropriately during the examination and frequently used expletives toward her father, which was atypical behavior, according to him.
During the patient's hospitalization, her mental status waxed and waned. On day 2 of admission, she underwent a lumbar puncture, which revealed a normal opening pressure, no signs of viral or bacterial meningitis, a red blood cell count of less than 1 cell/mm3, a white blood cell count of 34 cells/mm3 (91% lymphocytes, 8% monocytes), and a protein level of 25 mg/dL. On day 3, she became increasingly agitated (screaming and singing) and was unable to complete sentences. She was progressively disoriented and unable to recognize family members. On day 6, she received a diagnosis when her cerebral spinal fluid tested positive for anti-NMDA receptor encephalitis, with a titer of 1:40. Pulse-dose steroid therapy was begun, as was plasmapheresis. Pelvic ultrasonography revealed a right ovarian dermoid cyst, and this was confirmed on magnetic resonance imaging of the pelvis as 1.6 × 1.7 cm in size.
On day 12 of admission, our cardiology department was consulted to investigate intermittent bradycardia and tachycardia. During examination of the patient, she became nonresponsive, with a 14-s period of no electrical activity on telemetry (Fig. 2); thereafter, return of sinus rhythm was noted, with recurrent prolonged pauses (4–12 s) (Fig. 3). The patient was urgently taken to the cardiac catheterization laboratory for placement of an active-fixation lead, with an externally placed temporary transvenous pacemaker. On day 13, she underwent an exploratory laparotomy and a right-ovarian cystectomy. Pathologic results confirmed a mature cystic teratoma. During a prolonged hospitalization, her anti-NMDA receptor encephalitis was treated with intravenous steroids, plasmapheresis, and resection of the suspected tumor. After 31 days, she no longer needed the pacemaker, so it was explanted. At a 5-month follow-up visit after her discharge from the hospital, the patient reported improvement in her cognitive and memory abilities, as evidenced by her capacity to perform as well in her college courses as she had before her illness.
Fig. 2.
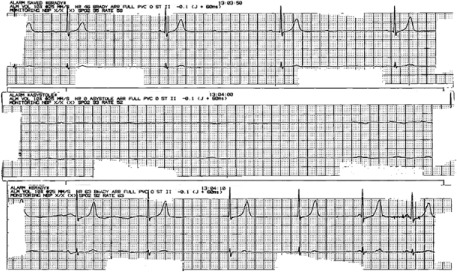
Telemetry recording of ictal asystole shows a 14-second pause.
Fig. 3.
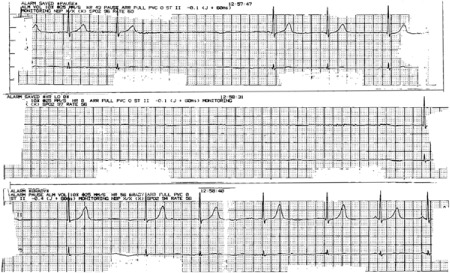
Telemetry recording shows repeated ictal asystole.
Discussion
Patients with anti-NMDA receptor encephalitis usually present with psychiatric symptoms that include psychosis, auditory and visual hallucinations, delusions, aggression, anxiety, obsessive-compulsive behaviors, depression, paranoia, insomnia, catatonia, mood lability, disinhibition, and hypersexuality.3 The anti-NMDA receptor antibodies are directed towards the NR1 subunit of the NMDA receptor.4 The NMDA receptors are important for synaptic transmission and remodeling, dendritic sprouting, and hippocampal long-term potentiation, all of which are considered to be crucial to memory. Antibodies to the receptor can cause neuronal death by means of excitotoxicity and apoptosis.5
A 2011 report6 noted the presence of ictal asystole during partial complex seizures in a case of anti-NMDA receptor encephalitis. Ictal asystole is a rare entity occurring in about 0.27% of epileptic patients (although it is probably underdiagnosed, given the necessity for continuous cardiac monitoring to obtain a proper diagnosis). In patients with intractable seizures in whom loop recorders were implanted, 21% were noted to have experienced periods of significant bradycardia.6 The bradycardia is thought to be secondary to the central nervous system's parasympathetic and sympathetic regulation of cardiac rhythm. The central regulation of the heart has been mapped to interconnections between the executive anterior cingulate cortex, the insular cortex, and the amygdala. The amygdala has reciprocal connections with the hypothalamus and brainstem, which eventually leads to their influence on the preganglionic sympathetic and parasympathetic neurons of the heart.7 In a series of 100 patients with anti-NMDA receptor encephalitis, 37 had cardiac arrhythmias (and 4 of those needed pacemakers).4 Prior case series6 suggest that anti-NMDA receptor encephalitis patients are at increased risk for cardiac dysrhythmias, in comparison with typical epileptic patients.
The standard approach to treatment, since Dalmau's report in 2007,1 is identification of a possible antibody-producing tumor. In young women, ovarian teratomas are often found in association with anti-NMDA receptor encephalitis. Acute therapy includes immunosuppression with high-dose pulse steroids, intravenous immunoglobulin, possible plasmapheresis, and increased immunosuppression with rituxan or alternative chemotherapeutic agents. Clinical improvement in mental status can take weeks to months. Some patients are left with residual neurocognitive deficits.8 Given the expectation that central nervous system seizure and autonomic dysregulation will improve when treatment is begun, we provided our patient with a temporary transvenous pacemaker.
Anti-NMDA receptor encephalitis is a recently characterized clinical syndrome that presents with profound psychiatric and neurologic symptoms that can be fatal. Clinical recognition of the syndrome and laboratory confirmation are crucial to timely diagnosis and treatment. Untreated autonomic instability can progress to death or permanent disability. Case reports suggest that cardiac dysrhythmias might be more frequent in this population than in typical seizure patients.
We have described the case of a young patient who received timely diagnosis and treatment of anti-NMDA receptor encephalitis characterized by severe autonomic instability and ictal asystole, which required temporary cardiac pacing. Her neurologic and cardiac symptoms eventually resolved.
Footnotes
From: Division of Cardiology, David Geffen School of Medicine at UCLA, Los Angeles, California 90095
References
- 1.Dalmau J, Tuzun E, Wu H, Masjuan J, Rossi JE, Voloschin A et al. Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol. 2007;61(1):25–36. doi: 10.1002/ana.21050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Irani SR, Vincent A. NMDA receptor antibody encephalitis. Curr Neurol Neurosci Rep. 2011;11(3):298–304. doi: 10.1007/s11910-011-0186-y. [DOI] [PubMed] [Google Scholar]
- 3.Chapman MR, Vause HE. Anti-NMDA receptor encephalitis: diagnosis, psychiatric presentation, and treatment. Am J Psychiatry. 2011;168(3):245–51. doi: 10.1176/appi.ajp.2010.10020181. [DOI] [PubMed] [Google Scholar]
- 4.Dalmau J, Gleichman AJ, Hughes EG, Rossi JE, Peng X, Lai M et al. Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol. 2008;7(12):1091–8. doi: 10.1016/S1474-4422(08)70224-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peery HE, Day GS, Dunn S, Fritzler MJ, Pruss H, De Souza C et al. Anti-NMDA receptor encephalitis. The disorder, the diagnosis and the immunobiology. Autoimmun Rev. 2012;11(12):863–72. doi: 10.1016/j.autrev.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 6.Lee M, Lawn N, Prentice D, Chan J. Anti-NMDA receptor encephalitis associated with ictal asystole. J Clin Neurosci. 2011;18(12):1716–8. doi: 10.1016/j.jocn.2011.03.024. [DOI] [PubMed] [Google Scholar]
- 7.Britton JW, Benarroch E. Seizures and syncope: anatomic basis and diagnostic considerations. Clin Auton Res. 2006;16(1):18–28. doi: 10.1007/s10286-006-0277-z. [DOI] [PubMed] [Google Scholar]
- 8.Titulaer MJ, McCracken L, Gabilondo I, Armangue T, Glaser C, Iizuka T et al. Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol. 2013;12(2):157–65. doi: 10.1016/S1474-4422(12)70310-1. [DOI] [PMC free article] [PubMed] [Google Scholar]


