Abstract
Context:
Laryngoscopy and intubation cause an intense reflex increase in heart rate, blood pressure, due to an increased sympathoadrenal pressor response. Lignoocaine has shown blunting of pressor response to intubation. Dexmedetomidine has sympatholytic effects.
Aims:
To the best of our knowledge there is no study comparing the efficacy of lignocaine with two different doses of dexmedetomidine for attenuating the pressor response. With this idea, we planned to conduct the present study.
Materials and Methods:
After approval by the Hospital Ethics committee, 90 consenting adults aged 18-65 years of age of either sex of non-hypertensive ASA Grade I or II were randomly allocated into three groups. Group D1- IV Dexmedetomidine 0.5μg/kg over 10 minutes Group D2- IV Dexmedetomidine 1μg/kg over 10 minutes Group X- IV Lignocaine 1.5mg/kg in 10 ml normal saline
Statistical Analysis Used:
ANOVA and Student's t test used for analysis.
Results:
Dexmedetomidine 1µg/kg was more effective than 0.5µg/kg and lignocaine 1.5mg/kg in attenuating the pressor response.
Conclusions:
We conclude that dexmedetomidine 1μg/kg adequately attenuates the hemodynamic response to laryngoscopy and endotracheal intubation when compared with dexmedetomidine 0.5μg/kg and lignocaine 1.5mg/kg.
Keywords: Dexmedetomidine, Lignocaine, Pressor response, Hemodynamic response, Catecholamine release
INTRODUCTION
Most patients undergoing surgery with general anesthesia require laryngoscopy and intubation as mandatory procedures. Laryngoscopy and intubation cause an intense reflex increase in heart rate (HR), blood pressure, and serum concentration of catecholamines leading to hypertension, tachycardia and dysrhythmias, which are evoked by stimulation of laryngeal and tracheal tissues during the procedure.[1,2,3,4]
These changes due to an increased sympathoadrenal pressure response can lead to adversities like myocardial infarction, acute heart failure and cerebrovascular accidents in susceptible individuals.[5]
Therefore in recent times, attenuation of this pressure response to laryngoscopy and intubation has become one of the most researched topics in the field of anesthesiology.
Some of the ways for attenuation of this pressure response include: Limiting duration of laryngoscopy to 15 s, use of β blockers like esmolol, lignocaine, low dose opioids (5-10 μg/kg) of fentanyl and sufentanil or alfentanil 80-100 μg/kg, morphine 0.2 mg/kg.[6]
Lignocaine is an aminoethylamide and prototype of amide local anesthetic group.[7] Introduced in the year 1948, it is the most widely used local anesthetic.[8] In 1961, Bromage showed that its intravenous (IV) use blunted pressure response to intubation.[9] An IV dose of lignocaine 1.5 mg/kg given 3 min prior to intubation has shown near optimal results.[10]
Dexmedetomidine, a α2 adrenergic agonist, has anesthetic sparing, analgesic, sedative, anxiolytic and sympatholytic effects.[11] It decreases central nervous system sympathetic outflow in a dose-dependent manner and has analgesic effects best described as opioid sparing.[12] In view of the fact that dexmedetomidine has shown minimal side-effects, it is finding its way into every segment of anesthesia practice.[13]
To the best of our knowledge, there is no study comparing the efficacy of IV lignocaine with two different doses of dexmedetomidine for attenuating the pressure response. The appropriate dose of dexmedetomidine is also not well-established, especially in the Indian population subset.
With this idea, we planned to conduct the present study to compare two different doses of dexmedetomidine with lignocaine for attenuation of pressure response.
MATERIALS AND METHODS
Ethics
After approval by the Hospital Ethics Committee, 90 consenting adult patients aged 18–65 years of age of either sex of nonhypertensive American Society of Anesthesiologists Grade I or II undergoing elective surgery under general anesthesia with endotracheal intubation were included in this randomized study protocol. Randomization was done using a computer generated random number table. Allocation concealment was ensured with sealed opaque envelope. The study was conducted from December 2012 to June 2013.
Study design
A complete preanesthetic checkup of patients was performed prior to their scheduled allotment into the different study groups. A detailed history which includes information regarding exercise tolerance, comorbidities, allergy, past hospital admissions and surgical history or anesthesia exposure, addictions were obtained.
General physical examination and systemic examination was performed during this time. Patients with the following conditions were however excluded from our study, namely: History of cardiac and pulmonary disease, pregnancy, morbid obesity, allergy to the study drug, hypertensive patients, impaired kidney or liver function and anticipated difficult airway.
Lignocaine preparation used was XYLOCARD 2% 50 ml (Astra-Zeneca Pharmaceuticals, Bengaluru, India) and dexmedetomidine by the name of DEXTOMID 200 μg/2 ml (Neon Pharmaceuticals, Mumbai, India) for conducting this study.
After obtaining written and informed consent, patients were randomly allocated into one of the three groups.
Group D1 - Patients were given IV dexmedetomidine 0.5 μg/kg over 10 min as premedication before induction of general anesthesia
Group D2 - Patients were given IV dexmedetomidine 1 μg/kg over 10 min as premedication before induction of general anesthesia
Group X - Patients were given IV lignocaine 1.5 mg/kg in 10 ml normal saline, 3 min before laryngoscopy and intubation.
Monitoring
The following parameters were monitored during the intra-operative period:-
Heart rate and rhythm by three lead electrocardiogram
Noninvasive blood pressure
Oxygen saturation by pulse oxymeter
End-tidal concentration of carbon dioxide level by capnograph.
Anesthetic technique
On shifting the patient to the operation theater, all the monitoring devices were attached. An 18 G IV infusion line was started, and all patients were hydrated with approximately 8-10 ml/kg of normal saline before induction. Oxygen was administered by a Hudson face mask at the rate of 5 l/min. Patients were given injection midazolam 1 mg IV as premedication.
All hemodynamic data was measured on arrival in observed time (OT), before induction, before intubation, and at 1, 3, 5 min after intubation by an independent observer.
Anesthesia was induced with a sleep dose of thiopental sodium and fentanyl 2 μg/kg. After giving injection vecuronium bromide 0.1 mg/kg IV and ventilating the patient with N2O and O2 for 3 min, intubation was performed with cuffed oral endotracheal tube of appropriate size for airway management. Patients are having unanticipated difficult airways requiring multiple attempts (two or more) at intubation or laryngoscopy time of more than 15 s were excluded from the study.
Anesthesia was maintained with isoflurane and nitrous oxide in oxygen. The mechanical ventilator was set to achieve an end-tidal carbon dioxide of 35-40 mmHg. Additional doses of vecuronium bromide if necessary were administered to maintain surgical relaxation. During the maintenance of anesthesia, additional doses of injection fentanyl 1 μg/kg were administered according to hemodynamic variables.
Surgery was allowed to start only after 5 min of intubation. At the end of surgery neuromuscular blockade was reversed with injection neostigmine 0.04 mg/kg and injection glycopyrrolate 0.1 mg/kg. IV ondansetron was injected to patients 30 min before the end of the surgery. The tracheal tube was removed after adequate spontaneous ventilation established.
We had planned to treat hypotension and bradycardia by decreasing the inhalational agent concentration by 50% or by administering IV ephedrine 10 mg or IV atropine 0.5 mg respectively.
Statistics
The mean and standard deviations of HR, systolic blood pressure (SBP) and diastolic blood pressure (DBP) in each of the groups were analyzed by analysis of variance (ANOVA) and using the paired Student's t-test for intragroup analysis. P < 0.05 was considered as significant.
RESULTS
The values mentioned below corresponded to these instances in time:
On arrival in OT
Before the induction of anesthesia
After induction and just before intubation
1 min after intubation
3 min after intubation
Chart 1.
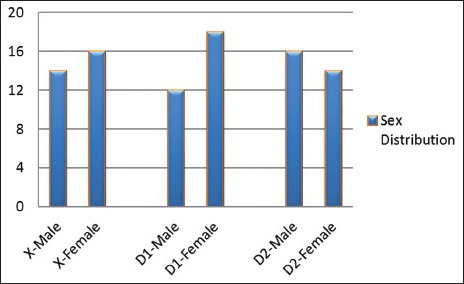
Sex distribution of the three groups
Chart 2.
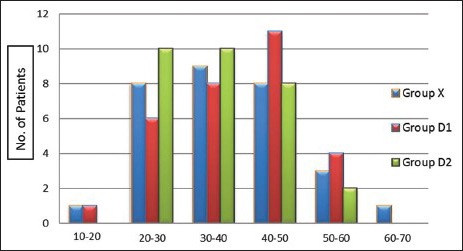
Age distribution in the three groups
According to Table 1, the difference between the three means was not found to be significant on application of ANOVA (0.194) when significance implies a P < 0.05 in case of HRa. A statistically significant difference between the three means was obtained in all the other HR readings, that is, HRb (0.011), HRc (0.001), HRd (0.001), HRe (0.000) and HRf (0.000) [Table 2].
Table 1.
HR at different times of patients belonging to the three groups
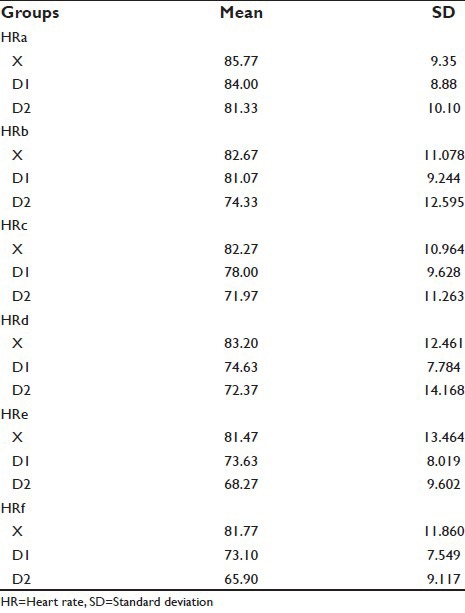
Table 2.
Comparison of HR in the lignocaine group at different instances of time taking HR on arrival in OT (HRa) as the standard by employing paired t-test
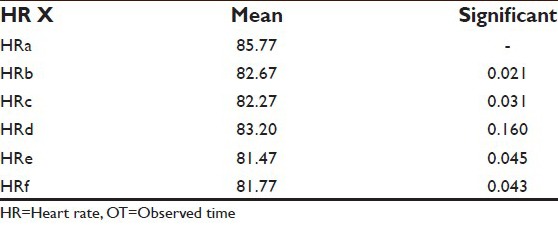
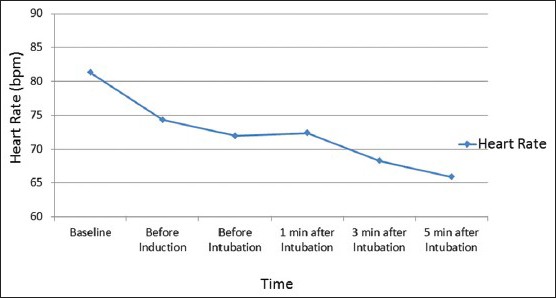
Besides the reading at 1 min after intubation that is, HRd (0.160), all other readings were shown to be statistically significant (P < 0.05) on applying paired t-test when compared with the reading on arrival in OT, that is, HRa.
The general decline in the HR when compared with the baseline was observed. However, at 1 min after intubation a slight increment in HR was encountered. Maximum reduction in HR was seen 3 min after intubation [Table 3].
Table 3.
Comparison of HR in the dexmedetomidine 0.5 µg/kg group at different instances of time taking HR on arrival in OT (HRa) as the standard by employing paired t-test
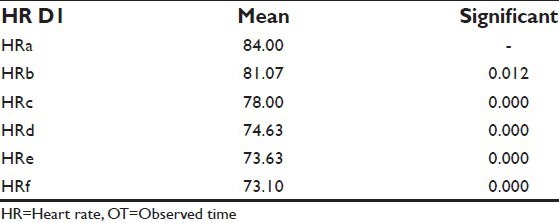
Readings as per Graph 1 were statistically significant (P < 0.05) on applying paired t test when compared with the reading on arrival in OT, that is, HRa.
Graph 1.
Comparison of heart rate in the lignocaine group at different time intervals
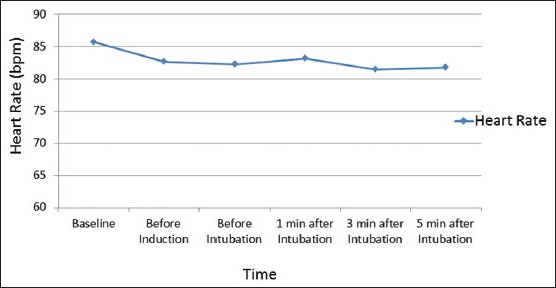
Graph 2 depicts the variation in the HR at different instances of time with the use of dexmedetomidine 0.5 μg/kg. A general decline in the HR when compared with the baseline was observed [Table 4].
Graph 2.
Comparison of heart rate in the dexmedetomidine 0.5 µg/kg group at different time intervals
Table 4.
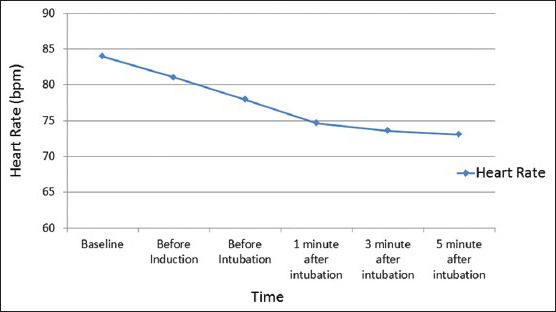
Comparison of HR in the dexmedetomidine 1 µg/kg group at different instances of time taking HR on arrival in OT (HRa) as the standard by employing paired t-test
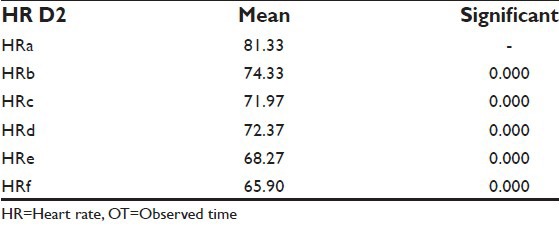
All readings were shown to be statistically significant (P < 0.05) on applying paired t-test when compared with the reading on arrival in OT, that is, HRa.
Graph 3 depicts the variation in the HR at different instances of time with the use of dexmedetomidine 1 μg/kg. The general decline in the HR when compared with the baseline was observed.
Graph 3.
Comparison of heart rate in the dexmedetomidine 1 µg/kg group at different time intervals
Graph 4 compares the HRs on employing lignocaine 1.5 mg/kg, dexmedetomidine 0.5 μg/kg, and dexmedetomidine 1 μg/kg respectively. Maximum reduction in HR was achieved in the group that was administered dexmedetomidine1 μg/kg.
Graph 4.
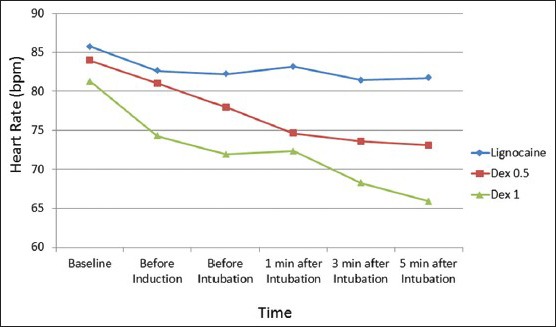
Comparison of heart rate in the three groups at different time instances
According to Table 5: In SBPa, SBPb, SBPc and SBPf the difference between the three means was found to be significant on application of ANOVA, taking P < 0.05. However, SBPd (0.403) and SBPe (0.021) were not significant on application of ANOVA [Table 6].
Table 5.
SBP at different times of patients belonging to the three groups
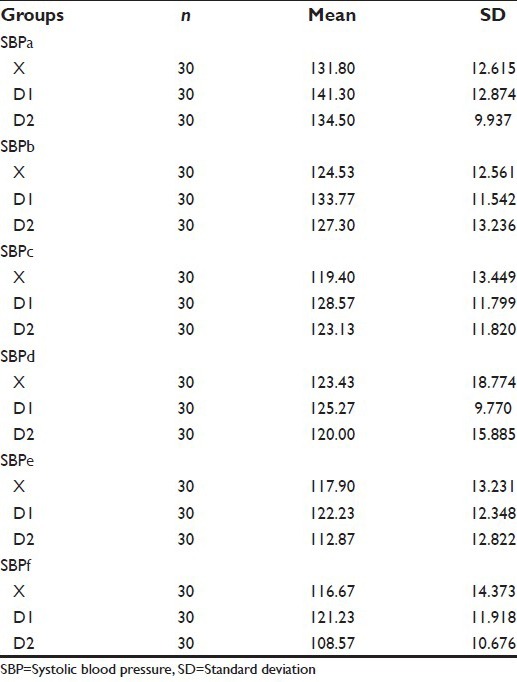
Table 6.
Comparison of SBP in the lignocaine 1.5 mg/kg group at different instances of time taking SBP on arrival in OT (SBPa) as the standard by employing paired t-test
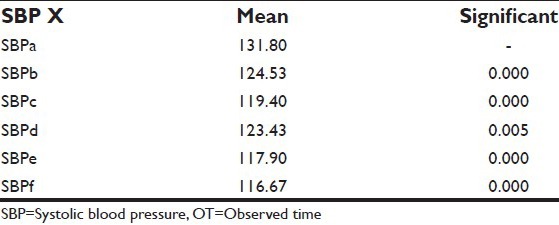
All readings were shown to be statistically significant (P < 0.05) on applying paired t-test when compared with the reading on arrival in OT, that is, SBPa.
Graph 5 depicts the variation in the SBP at different instances of time with the use of lignocaine 1.5 mg/kg. A general decline in the SBP when compared with the baseline was observed. However, a marginal increment in SBP was noted 1 min after intubation [Table 7].
Graph 5.
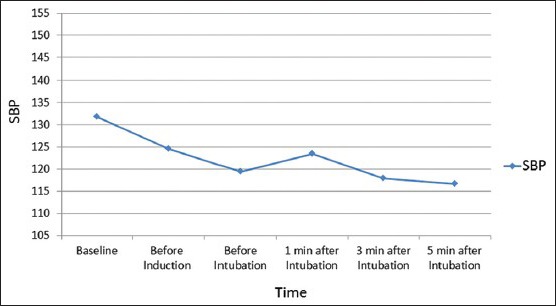
Comparison of systolic blood pressure in the lignocaine group at different time intervals
Table 7.
Comparison of SBP in the dexmedetomidine 0.5 µg/kg group at different instances of time taking SBP on arrival in OT (SBPa) as the standard by employing paired t-test
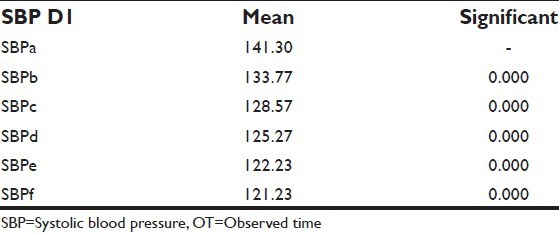
All readings were shown to be statistically significant (P < 0.05) on applying paired t-test when compared with the reading on arrival in OT, that is, SBPa. The SBP decreased after the patient received the study drug.
Graph 6 depicts the variation in the SBP at different instances of time with the use of dexmedetomidine 0.5 μg/kg. The general decline in the SBP when compared with the baseline was observed [Table 8].
Graph 6.
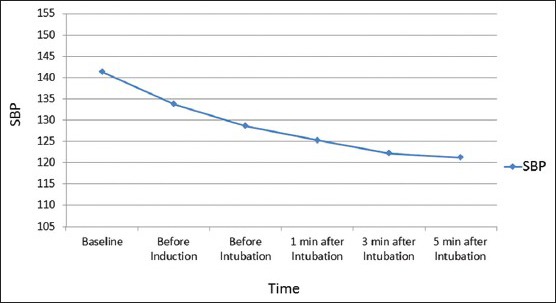
Comparison of systolic blood pressure in the dexmedetomidine 0.5 µg/kg group at different time intervals
Table 8.
Comparison of SBP in the dexmedetomidine 0.5 µg/kg group at different instances of time taking SBP on arrival in OT (SBPa) as the standard by employing paired t-test
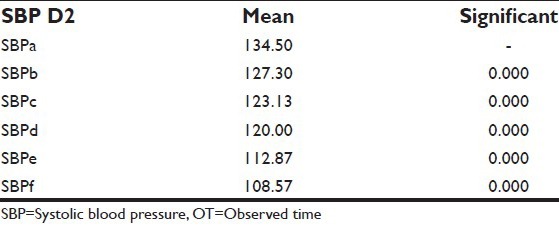
All readings were shown to be statistically significant (P < 0.05) on applying paired t-test when compared with the reading on arrival in OT, that is, SBPa.
Graph 7 depicts the variation in the SBP at different instances of time with the use of dexmedetomidine 1 μg/kg. The general decline in the SBP when compared with the baseline was observed.
Graph 7.
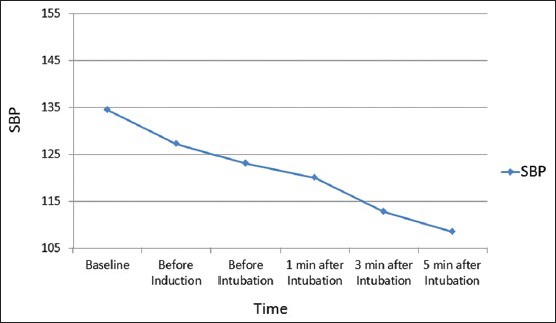
Comparison of systolic blood pressure in the dexmedetomidine 1 µg/kg group at different time intervals
As per Graph 8 On comparing all the three groups, maximum reduction in SBP was achieved in the group that was administered dexmedetomidine 1 μg/kg and was statistically significant.
Graph 8.
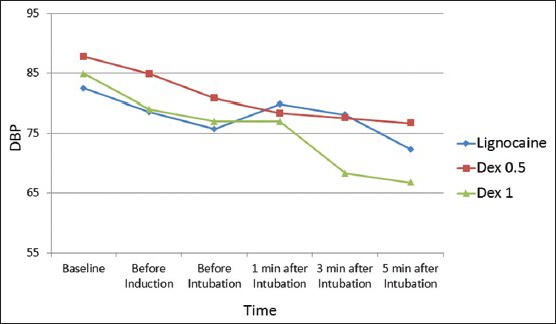
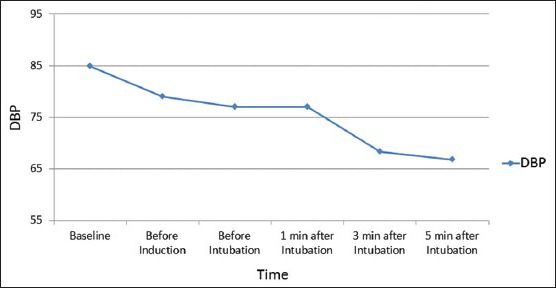
Comparison of diastolic blood pressure of the three groups at different time instances
According to Table 9. the difference between the three means was found to be not significant on application of ANOVA in DBPa (0.028), DBPc (0.095) and DBPd (0.581), taking P < 0.05 whereas, DBPb (0.008), DBPe (0.000) and DBPf (0.001) were found to be statistically significant [Table 10].
Table 9.
DBP at different times of patients belonging to the three groups
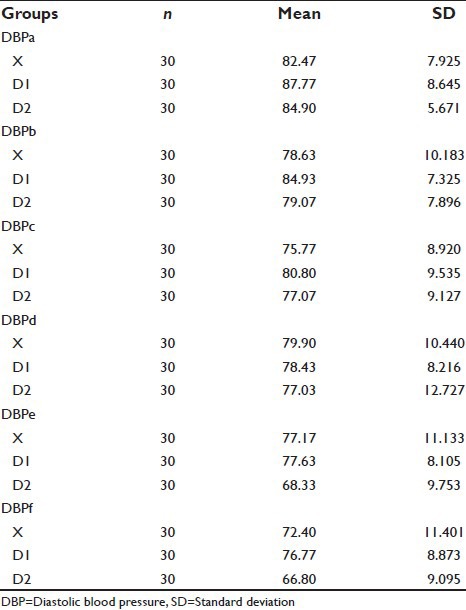
Table 10.
Comparison of DBP in the lignocaine 1.5 mg/kg group at different instances of time taking DBP on arrival in OT (DBPa) as the standard by employing paired t-test
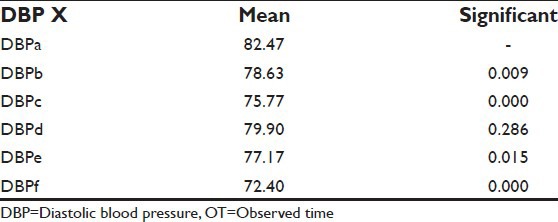
Besides the reading at 1 min after intubation, that is, DBPd (0.286), all other readings were shown to be statistically significant (P < 0.05) on applying paired t-test when compared with the reading on arrival in OT, that is, DBPa.
Graph 9 depicts the variation in the DBP at different instances of time with the use of lignocaine 1.5 mg/kg. A decline in the DBP when compared with the baseline was observed. However, at 1 and 3 min after intubation we noticed an increment in the DBP [Table 11].
Graph 9.
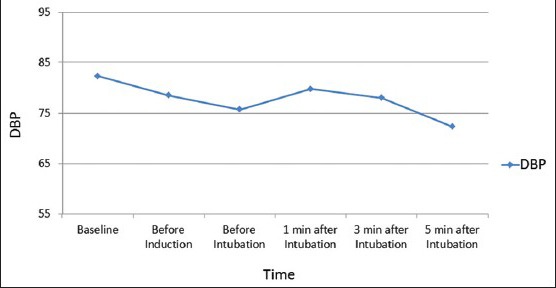
Comparison of diastolic blood pressure in the lignocaine group at different time intervals
Table 11.
Comparison of DBP in the dexmedetomidine 0.5 µg/kg group at different instances of time taking DBP on arrival in OT (DBPa) as the standard by employing paired t-test
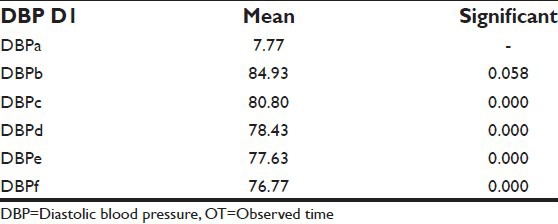
All readings were shown to be statistically significant (P < 0.05) on applying paired t-test when compared with the reading on arrival in OT, that is, DBPa.
Graph 10 depicts the variation in the DBP at different instances of time with the use of dexmedetomidine 0.5 μg/kg. The general decline in the DBP when compared with the baseline was observed [Table 12].
Graph 10.
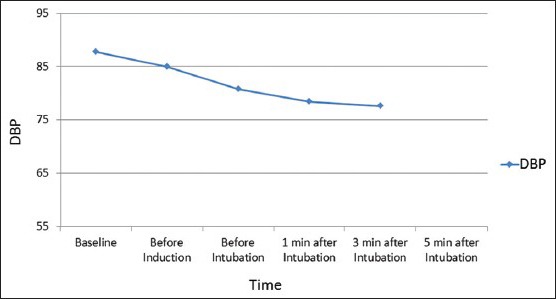
Comparison of diastolic blood pressure in the dexmedetomidine 0.5 µg/kg group at different time intervals
Table 12.
Comparison of DBP in the dexmedetomidine 1 µg/kg group at different instances of time taking DBP on arrival in OT (DBPa) as the standard by employing paired t-test
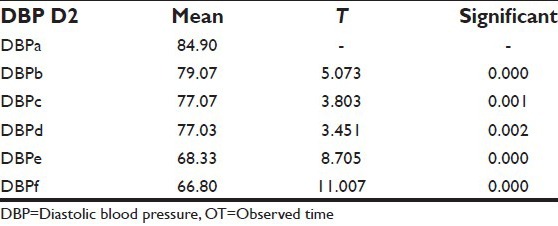
All readings were shown to be statistically significant (P < 0.05) on applying paired t-test when compared with the reading on arrival in OT that is DBPa.
Graph 11 depicts the variation in the DBP at different instances of time with the use of dexmedetomidine 1 μg/kg. A general decline in the DBP when compared with the baseline was observed.
Graph 11.
Comparison of diastolic blood pressure in the dexmedetomidine 1 µg/kg group at different time intervals
On comparing all the three groups, maximum reduction in DBP was achieved in the group, which was administered dexmedetomidine 1 μg/kg and was statistically significant.
DISCUSSION
The hemodynamic response characterized by tachycardia and hypertension to manipulation in the area of the larynx, by means of laryngoscopy and intubation, is well-recognized. Stimulation of mechanoreceptors in the pharyngeal wall, epiglottis and vocal cords, is thought to be the cause for this hemodynamic response.
Shribman et al. found that laryngoscopy alone or followed by tracheal intubation increases arterial pressure and catecholamine levels while intubation significantly increases HR.[14] These changes were reported to be greatest 60 s after intubation of the trachea that lasts for 5-10 min. If no specific measures are taken to prevent this hemodynamic response, the HR can increase from 26% to 66% depending on the method of induction and the SBP can increase from 36% to 45%.[14,15]
Myocardial ischemia might occur during the induction-intubation sequence in patients with coronary artery disease. Intraoperative ischemia has been associated with a high rate of perioperative myocardial infarction.[16] Interventions like direct laryngoscopy involving severe sympathetic stimuli, prevention of tachycardia, hypertension and elevated total oxygen consumption due to sympathetic activity may prove beneficial in patients with limited cardiac reserve.[17]
Various studies have reviewed the effect of lignocaine to blunt the sympathoadrenal pressure response. Lev and Rosen in their study reviewed the use of prophylactic lignocaine as a preintubation medication.[10] A dose of 1.5 mg/kg intravenously 3 min prior to intubation was employed and was found to be optimal for attenuation of the sympathoadrenal pressure response to laryngoscopy and intubation without any overt harmful effects. We also administered lignocaine 1.5 mg/kg 3 min before intubation in our study and observed a general decline in HR, SBP, and DBP as is represented by the interpretation of Graphs 1, 5 and 9. The decrease in HR and blood pressure in our study might also be attributed to the use of anesthetic agents such as opioids (fentanyl) and inhalational agents.
Wilson et al. in their study stated that IV lignocaine is beneficial in preventing the hemodynamic changes to laryngoscopy and intubation.[18] Their results are reiterated by our study too in which we have described similar results. We noted the maximal decline of HR to be at 3 min after intubation [Graph 1], while the maximal decline in SBP and DBP is observed at 5 min postintubation [Graphs 5 and 9]. However this decline of HR and blood pressure can possibly be attributed to the combined effects of fentanyl and inhalational agents administered during the maintenance of anesthesia. From our statistical analysis we also infer from [Table 1] that though there is a general decline in HR after administration of lignocaine, but at the time interval corresponding to 1 min postintubation, we observed an increase in HR. This shows that the pressure response was incompletely abolished by lignocaine.
Malde and Sarode in their study concluded that on comparison of lignocaine in a dose of 1.5 mg/kg and fentanyl 2 μg/kg for suppression of hemodynamic response to endotracheal intubation, fentanyl was found to be relatively superior.[19] Lignocaine attenuated the rise in blood pressure while fentanyl prevented it totally. The rise persisted for 3 min in the lignocaine but 10 min in the control group. The fentanyl group also showed a significant decrease in SBP after administration, which came back to normal at 1-3 min following intubation. In our study we found that lignocaine sufficiently attenuated the above mentioned hemodynamic response, but this attenuation was not complete and a spike in SBP was observed 1 min postintubation [Graph 5]. We also we noticed 2 spikes at 1 min and 3 min intervals postintubation in the DBP recordings [Graph 9] which are in concordance with the above study. In our study we also did not encounter any side-effects like hypotension or bradycardia when lignocaine at a dose of 1.5 mg/kg was employed.
Recent studies however, have questioned lignocaine's efficacy. In studies by Singh et al.[20] van den Berg et al.[21] and Kindler et al.[22] IV lignocaine 1.5 mg/kg was ineffective in controlling the acute hemodynamic response following laryngoscopy and intubation. In a study conducted by Pathak et al.[23] it was shown that lignocaine 1.5 mg/kg was ineffective in blunting responses during laryngoscopy and tracheal intubation when compared with two different doses of alfentanil (15 μg/kg and 30 μg/kg). However in our study, we used fentanyl universally in all the three groups. From the interpretation of the results of our study we concluded that lignocaine attenuated but did not completely abolish the pressure response to laryngoscopy and intubation.
Alpha two adrenergic agonists decrease sympathetic tone and their preoperative use has been shown to blunt the hemodynamic responses to laryngoscopy and intubation.[24] They also reduce the need for anesthetics and therefore can be used as an adjunct to general anesthesia.[25] Dexmedetomidine is a highly selective and specific alpha two adrenergic agonist. Therefore, it is increasingly being used as an agent to attenuate the pressure response.
Sagiroglu et al. concluded that the overall control of hemodynamic responses to tracheal intubation were better with dexmedetomidine 1 μg/kg as compared to dexmedetomidine 0.5 μg/kg.[26] In our study we also compared similar doses of dexmedetomidine with lignocaine and we concluded that 1 μg/kg of dexmedetomidine significantly reduced the increase in HR associated with laryngoscopy and intubation when compared to 0.5 μg/kg of dexmedetomidine. We also infer that both doses of dexmedetomidine brought upon a greater decline in HR when individually compared with lignocaine. This is represented in Graphs 1–4.
In the study conducted by Sagiroglu et al.[26] the results of SBP, DBP and mean arterial pressure were significantly lower in the group given dexmedetomidine 1 μg/kg than the group given dexmedetomidine 0.5 μg/kg at 1 min after intubation. This is in agreement with our study results as represented in Tables 5 and 9, which show a statistically significant decline in systolic and DBPs in the group administered dexmedetomidine 1 μg/kg. We also observed a general decline in the systolic and DBPs in both the groups administered dexmedetomidine (0.5 μg/kg and 1 μg/kg) when compared to the pressures on arrival in the OT which were considered as baseline [Tables 5 and 9]. On comparing all the three groups, we concluded that dexmedetomidine 1 μg/kg brought upon a maximal reduction in systolic and DBPs at 1, 3 and 5 min post intubation [Graphs 11 and 12]. However among dexmedetomidine 0.5 μg/kg and lignocaine, we noticed a greater decline in both systolic and DBP in the lignocaine group as compared to dexmedetomidine 0.5 μg/kg group at 1, 3 and 5 min after intubation [Graphs 11 and 12].
Graph 12.
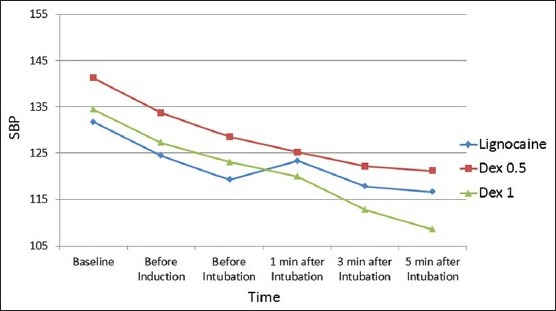
Comparison of systolic blood pressure of the three groups at different time instances
Laha et al.[27] in their study compared dexmedetomidine 1 μg/kg with control and concluded that dexmedetomidine effectively blunted the hemodynamic responses during laryngoscopy, and reduced anesthetic requirements. Our study also denotes similar findings and also provides comparison between two different doses of dexmedetomidine. From our study, we adequately establish that dexmedetomidine 1 μg/kg was comparatively superior to dexmedetomidine 0.5 μg/kg for attenuation of the pressure response to laryngoscopy and intubation.
Dexmedetomidine is finding its way into every segment of anesthesia practice and its safety and efficacy as an agent to attenuate the pressure response has been reasonably well established.
CONCLUSION
We conclude that dexmedetomidine in a dose of 1 μg/kg over 10 min before induction of anesthesia effectively attenuates the hemodynamic response to laryngoscopy and endotracheal intubation. Dexmedetomidine administered in a dose of 0.5 μg/kg over 10 min before induction of anesthesia was effective in blunting the tachycardic response to intubation but incompletely attenuated the increase in systolic and DBP. Further, lignocaine in a dose of 1.5 mg/kg given 3 min before laryngoscopy and intubation was more effective than dexmedetomidine 0.5 μg/kg in attenuating the increase in systolic and DBP at 3 min and 5 min after endotracheal intubation.
Dexmedetomidine 1 μg/kg was more effective than dexmedetomidine 0.5 μg/kg in attenuating the pressure response completely without any side effect. Dexmedetomidine 1 μg/kg has proved to maintain hemodynamic stability associated with intubation and hence may prove beneficial for cardiac patients where the stress response to laryngoscopy and intubation is highly undesirable.
In summary dexmedetomidine, a highly selective α2 adrenoreceptor agonist has many desirable clinical benefits that encourage its use in the perioperative period.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Colson P, Ryckwaert F, Coriat P. Renin-angiotensin system antagonist and anaesthesia. Anaesth Analg. 1949;96:261–3. [PubMed] [Google Scholar]
- 2.Matsukawa K, Ninomiya I, Nishiura N. Effects of anesthesia on cardiac and renal sympathetic nerve activities and plasma catecholamines. Am J Physiol. 1993;265:R792–7. doi: 10.1152/ajpregu.1993.265.4.R792. [DOI] [PubMed] [Google Scholar]
- 3.Kirvelä M, Scheinin M, Lindgren L. Haemodynamic and catecholamine responses to induction of anaesthesia and tracheal intubation in diabetic and nondiabetic uraemic patients. Br J Anaesth. 1995;74:60–5. doi: 10.1093/bja/74.1.60. [DOI] [PubMed] [Google Scholar]
- 4.Esler M. The sympathetic system and hypertension. Am J Hypertens. 2000;13:99S–105. doi: 10.1016/s0895-7061(00)00225-9. [DOI] [PubMed] [Google Scholar]
- 5.Foex P, Sear JW. The surgical hypertensive patient. Contin Educ Anaesth Crit Care Pain. 2004;4:139–43. [Google Scholar]
- 6.Saha U, Jayalakshmi TS. Pressor response in hypertension. Indian J Anaesth. 2003;47:443–9. [Google Scholar]
- 7.Catterall WA, Mackie K. Local Anesthetics. In: Brunton L, Chabner B, Knollman B, editors. Goodman and Gilman's The Pharmacological Basis of Therapeutics. 12th ed. New York: McGraw Hill Publishers; 2011. pp. 564–82. [Google Scholar]
- 8.Tripathi KD. Local anaesthetics. In: Tripathi KD, editor. Essentials of Medical Pharmacology. 6th ed. New Delhi: Jaypee Publishers; 2009. pp. 351–63. [Google Scholar]
- 9.Bromage PR, Robson JG. Concentrations of lignocaine in the blood after intravenous, intramuscular epidural and endotracheal administration. Anaesthesia. 1961;16:461–78. doi: 10.1111/j.1365-2044.1961.tb13426.x. [DOI] [PubMed] [Google Scholar]
- 10.Lev R, Rosen P. Prophylactic lidocaine use preintubation: A review. J Emerg Med. 1994;12:499–506. doi: 10.1016/0736-4679(94)90347-6. [DOI] [PubMed] [Google Scholar]
- 11.Panzer O, Moitra V, Robert N. Pharmacology of sedative analgesics agents. Dexmedetomidine, remifentanil, ketamine: Volatile anesthetics and the role of peripheral Mu antagonists. Anesthesiol Clin. 2011;2:587–605. doi: 10.1016/j.anclin.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 12.Gertler R, Brown HC, Mitchell DH, Silvius EN. Dexmedetomidine: A novel sedative-analgesic agent. Proc (Bayl Univ Med Cent) 2001;14:13–21. doi: 10.1080/08998280.2001.11927725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dogru K, Arik T, Yildiz K, Bicer C, Madenoglu H, Boyaci A. The effectiveness of intramuscular dexmedetomidine on hemodynamic responses during tracheal intubation and anesthesia induction of hypertensive patients: A randomized, double-blind, placebo-controlled study. Curr Ther Res Clin Exp. 2007;68:292–302. doi: 10.1016/j.curtheres.2007.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shribman AJ, Smith G, Achola KJ. Cardiovascular and catecholamine responses to laryngoscopy with and without tracheal intubation. Br J Anaesth. 1987;59:295–9. doi: 10.1093/bja/59.3.295. [DOI] [PubMed] [Google Scholar]
- 15.Helfman SM, Gold MI, DeLisser EA, Herrington CA. Which drug prevents tachycardia and hypertension associated with tracheal intubation: Lidocaine, fentanyl, or esmolol? Anesth Analg. 1991;72:482–6. doi: 10.1213/00000539-199104000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Chraemmer-Jørgensen B, Høilund-Carlsen PF, Marving J, Christensen V. Lack of effect of intravenous lidocaine on hemodynamic responses to rapid sequence induction of general anesthesia: A double-blind controlled clinical trial. Anesth Analg. 1986;65:1037–41. [PubMed] [Google Scholar]
- 17.Mikawa K, Obara H, Kusunoki M. Effect of nicardipine on the cardiovascular response to tracheal intubation. Br J Anaesth. 1990;64:240–2. doi: 10.1093/bja/64.2.240. [DOI] [PubMed] [Google Scholar]
- 18.Wilson IG, Meiklejohn BH, Smith G. Intravenous lignocaine and sympathoadrenal responses to laryngoscopy and intubation. The effect of varying time of injection. Anaesthesia. 1991;46:177–80. doi: 10.1111/j.1365-2044.1991.tb09403.x. [DOI] [PubMed] [Google Scholar]
- 19.Malde AD, Sarode V. Attenuation of the hemodynamic response to endotracheal intubation: fentanyl vs lignocaine. Int J Anaesth. 2007;12:1. [Google Scholar]
- 20.Singh SP, Quadir A, Malhotra P. Comparison of esmolol and labetalol, in low doses, for attenuation of sympathomimetic response to laryngoscopy and intubation. Saudi J Anaesth. 2010;4:163–8. doi: 10.4103/1658-354X.71573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van den Berg AA, Savva D, Honjol NM. Attenuation of the haemodynamic responses to noxious stimuli in patients undergoing cataract surgery. A comparison of magnesium sulphate, esmolol, lignocaine, nitroglycerine and placebo given i.v. with induction of anaesthesia. Eur J Anaesthesiol. 1997;14:134–47. doi: 10.1046/j.1365-2346.1997.00069.x. [DOI] [PubMed] [Google Scholar]
- 22.Kindler CH, Schumacher PG, Schneider MC, Urwyler A. Effects of intravenous lidocaine and/or esmolol on hemodynamic responses to laryngoscopy and intubation: A double-blind, controlled clinical trial. J Clin Anesth. 1996;8:491–6. doi: 10.1016/0952-8180(96)00109-2. [DOI] [PubMed] [Google Scholar]
- 23.Pathak D, Slater RM, Ping SS, From RP. Effects of alfentanil and lidocaine on the hemodynamic responses to laryngoscopy and tracheal intubation. J Clin Anesth. 1990;2:81–5. doi: 10.1016/0952-8180(90)90058-b. [DOI] [PubMed] [Google Scholar]
- 24.Aantaa R, Jalonen J. Perioperative use of alpha2-adrenoceptor agonists and the cardiac patient. Eur J Anaesthesiol. 2006;23:361–72. doi: 10.1017/S0265021506000378. [DOI] [PubMed] [Google Scholar]
- 25.Scheinin B, Lindgren L, Randell T, Scheinin H, Scheinin M. Dexmedetomidine attenuates sympathoadrenal responses to tracheal intubation and reduces the need for thiopentone and peroperative fentanyl. Br J Anaesth. 1992;68:126–31. doi: 10.1093/bja/68.2.126. [DOI] [PubMed] [Google Scholar]
- 26.Sagiroglu AE, Celik M, Orhon Z, Yüzer S, Sen B. Different doses of Dexmedetomidine on controlling hemodynamic responses to tracheal intubation. Int J Anaesth. 2010;27:2. [Google Scholar]
- 27.Laha A, Ghosh S, Sarkar S. Attenuation of sympathoadrenal responses and anesthetic requirement by dexmedetomidine. Anesth Essays Res. 2013;7:65–70. doi: 10.4103/0259-1162.113996. [DOI] [PMC free article] [PubMed] [Google Scholar]


