Abstract
Background:
Various sedative and analgesic techniques have been used during shock wave lithotripsy (SWL).
Aim:
This study aimed at evaluating the efficacy of ultrasound-guided unilateral transversus abdominis plane (TAP) block as an analgesic technique alternative during ureteric SWL.
Settings and Design:
Prospective randomized comparative study.
Materials and Methods:
Fifty patients scheduled for ureteric SWL were randomly allocated into two equal groups: Group (F) received 1.5 mcg/kg fentanyl intravenous and group (T) received unilateral TAP block with injection of 25 ml of bupivacaine 0.25% (62.5 mg).
Statistical Analysis:
Statistical analysis was performed using SPSS program version 19 and EP16 program.
Results:
The visual analog scale was significantly less in group (T) than in group (F) both intra-operatively (at 10, 20, 30, and 40 min) and postoperatively (at 10 min intervals in the postanesthesia care unit [PACU]) (P < 0.001). Rescue analgesia with pethidine during the procedure and in the PACU was less (P < 0.001) in the group (T) than group (F) with a median of 20 mg versus 55 mg, respectively. The higher sedation scores observed in group (F) at 15, 25, and 35 min during the procedure, and at 20 min during the PACU time were statistically highly significant (P < 0.001), but only significant at 10 min (P = 0.03) and 30 min (P = 0.007) during the PACU time. There was also highly significant decrease (P < 0.001) in the time of PACU stay in group (T) (38.2 ± 6.6 min) compared with group (F) (89.2 ± 13.39 min). We recorded 6 patients in group (F) (24%) who have developed respiratory depression (respiratory rate < 10 breaths/min) compared to 0% in group (T) (P = 0.022). In addition, in group (F) nausea was noted in 8 patients (32%) and vomiting in 6 patients (24%), which was statistically significant when compared to group (T) (0%) (P = 0.01 and 0.022, respectively).
Conclusion:
Ultrasound-guided unilateral TAP block is an effective alternative analgesic technique during ureteric SWL.
Keywords: Extracorporeal shock wave lithotripsy, local anesthetic, transversus abdominis plane block
INTRODUCTION
Extracorporeal shock wave lithotripsy (ESWL) was introduced into clinical practice in 1980 as a first-line therapy for the majority of urinary stones.[1] Pain experienced during ESWL is still poorly understood but is believed to be multifactorial. The superficial skin nociceptors and visceral nociceptors such as periosteal, pleural, peritoneal and/or musculoskeletal pain receptors are responsible for pain during ESWL.[2] Other contributing factors include individual variations, the site and size of stones and pressure of shock waves produced by different types of lithotripters.[3]
Different analgesic agents, including opioids[4,5] and local anesthetic agents,[6] as well as different analgesic techniques, such as general anesthesia, regional anesthesia, patient-controlled analgesia, and monitored anesthesia care have all been used to manage the pain during ESWL.[7] Fentanyl, a potent synthetic opioid, is commonly used during ESWL. The combination of fentanyl and other drugs like propofol has been proven as an effective intravenous (IV) analgesic technique but has significant side effects like respiratory depression, nausea, vomiting, and drowsiness.[8]
The ideal analgesic technique, offering pain-free treatment, free of adverse events, and cost-effective, remains to be established.[7] It has been proven in various literature that transversus abdominis plane (TAP) block provides good postoperative analgesia, when used in patients requiring abdominal wall incisions for total abdominal hysterectomy, lower segment caesarean section, prostatectomy, appendectomy, and laparoscopic surgeries.[9,10,11,12] Using ultrasound improves the success rate and accuracy of TAP block and prevents its complications.[13] Previous studies on cadavers and volunteers have elucidated the ability of the TAP block to produce block of the lower six thoracic and upper lumbar sensory afferents.[14,15]
The aim of our study was to evaluate the analgesic efficacy and safety of ultrasound-guided unilateral TAP block compared to IV fentanyl during ureteric SWL.
MATERIALS AND METHODS
After approval of the hospital's “Clinical Research Ethics Committee,” a written informed consent was obtained from all patients enrolled in the study. This prospective randomized comparative study was performed over 11 months (from October 2013 to August 2014) at the Department of Urology in Dr. Soliman Fakeeh Hospital, Jeddah, Saudi Arabia. Fifty patients of American Society of Anesthesiologists (ASA) physical status I and II, aged 18–65 years old, of both gender, with single radiopaque ureteric stone scheduled for elective SWL, were included in this study. Exclusion criteria were patient's refusal, body mass index (BMI) <20 kg/m2 or more than 30 kg/m2, coagulopathy and significant systemic or metabolic diseases. Patients with a history of substance abuse, psychiatric problems or allergy to any of the medications to be used in the study were also excluded.
On arrival to the lithotripsy unit, routine preoperative evaluation was performed, and the procedure was explained to all patients. Before premedication, each patient was instructed on the use of a standard 10 cm visual analogue scale (VAS) with “0” as no pain and “10” as the worst pain imaginable. Patients were advised not to move during the procedure and to ask for analgesia for intolerable pain or discomfort. Baseline measurements of heart rate (HR), mean arterial pressure (MAP), respiratory rate (RR), and room air oxygen saturation (SaO2) were obtained using an electrocardiogram, a “Dinamap” automated blood pressure monitor, and a pulse oximeter, respectively.
After insertion of an IV cannula, paracetamol 1 g (Perfalgan™, Bristol-Myer's Squibb) was infused to cover the pain of visceral origin. Afterward, Ringer's lactate infusion (10 ml/kg/h) was started, oxygen mask (6 L/min) was applied and IV midazolam (0.05 mg/kg) was given as a premedication.
Patients were randomly divided into two groups: Group (F) (n = 25) received fentanyl 1.5 mcg/kg IV immediately prior to the procedure, and group (T) (n = 25) received unilateral TAP block (described later). Intra- and post-operative data were recorded by a physician blinded to the study groups.
In group (T), the unilateral TAP block was performed in a supine position 10 min prior to the procedure. Using portable ultrasound device (SonoSite™, Bothell, WA, USA), a linear 6–13 MHz ultrasound transducer was placed at the level of the anterior axillary line between the 12th rib and the iliac crest of the same side of the ureteric stone. The puncture area and the ultrasound probe were prepared in a sterile manner. Using the in-plane technique with a skin entry at 1–2 cm away from the transducer, the skin was infiltrated with 1 ml lidocaine 1% and an 18-gauge Tuohy needle was advanced into the plane between the internal oblique muscle and the transversus abdominis muscle (TAM). Once the needle tip position was confirmed by injecting 2 ml of normal saline 0.9% and observing a hypoechoic pocket between the two muscles, 25 ml of bupivacaine 0.25% (62.5 mg) was injected slowly after negative aspiration. The drug was seen spreading in the TAP in a hypoechoic dark oval shape. Decreased sensation in the appropriate dermatomal levels of the same side of the procedure was confirmed by pinprick.
Shockwave lithotripsy was performed by SWL machine (Lithoskop™; combined X-ray/shock wave C-arm system, Siemens, Germany). The shock wave emitter was applied on the abdomen of the patients at the same side of the stone. Hemodynamic (HR and MAP) and respiratory (RR and SaO2) variables and VAS scores were recorded at 5 min intervals intra-operatively and 10 min intervals in the postanesthesia care unit (PACU).
Patients who developed pain intra-operatively or in the PACU and with a VAS of more than (3) received 0.25 mg/kg IV pethidine, to be repeated on demand. The total amount of pethidine given to patients as rescue analgesia was recorded.
Sedation was assessed at 5 min intervals during the procedure and at 10-min intervals in the PACU using the Ramsay sedation score as follows:
1 = Anxious or agitated,
2 = Co-operative, oriented, and tranquil,
3 = Responds to commands only,
4 = Brisk response to a light glabellar tap or to a verbal stimulus,
5 = Sluggish response to a light glabellar tap or to a verbal stimulus,
6 = No response to stimulus.[16]
The incidence of nausea and/or vomiting from the onset of the procedure until discharge from the PACU was recorded. Ondansetron 4 mg IV was given as a rescue antiemetic. All patients were closely observed for symptoms and signs of local anesthetic toxicity (e.g. light-headedness, circumoral numbness, tongue paresthesia, arrhythmia, muscle twitches and convulsions) as well as the side effects of opioids, such as bradycardia (HR < 50 beats/min), hypotension (MAP < 20% of baseline), bradypnea (RR < 10 breaths/min), hypoxia (SaO2 < 93%), and pruritus.
After completion of the procedure, the total number of shockwaves, their power and the total duration of the procedure were also recorded and considered for statistical analysis. Afterward, patients were transferred to the PACU. Criteria for discharge from the PACU include full consciousness, hemodynamic stability, ability to walk to the bathroom and void and absence of significant pain, nausea and/or vomiting. The length of PACU stay was recorded.
Sample size was calculated according to the following data: Confidence interval 95%, power of test 80%, ratio of unexposed to exposed 1:1, risk of decreased RR in fentanyl group 35% compared to 1% in TAP block group. Hence, the sample size was 50 patients, 25 in each group.
Statistical analysis was performed using SPSS program version 19 (Armonk, NY: IBM Corp.) and EP16 program. Demographic data and side of the stones were analyzed using Student's t-test for numerical data and Chi-square test for categorical data. Perioperative variables and VAS during the procedure and in the time of PACU were analyzed using Student's t-test or Mann–Whitney U-test as appropriate. Sedation scores during the procedure and in the PACU time and the perioperative side effects were analyzed using Fisher's exact test and Chi-square test as appropriate. Data are presented as mean ± standard deviation, median, numbers, and frequencies as appropriate. P < 0.05 was considered statistically significant and < 0.001 was highly significant.
RESULTS
From 56 consecutive patients scheduled for ureteric SWL during the study period, 6 patients were excluded. Three patients were excluded from group (F); two were shifted to general anesthesia due to patients’ irritability and one had required ureteric stent insertion. Three patients were also excluded from group (T); TAP block failed completely in one patient, and the other two patients underwent ureteroscopic lithotripsy due to stone impaction. Finally, 50 patients were enrolled in the study, 25 in each group and were considered for analysis [Figure 1].
Figure 1.
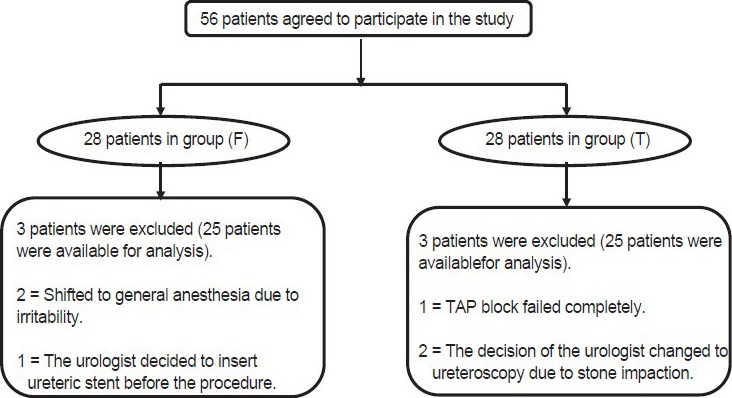
Flow chart of the study
Demographic data of the patients (sex, age, weight, height, BMI, and ASA classification), and side of the stones were comparable and no statistically significant differences were observed between the two groups [Table 1].
Table 1.
Demographic data of patients and the side of stones

There were also no significant differences between the two groups regarding duration of SWL, number of shock waves, and the maximum power of shock waves needed to crush the stones [Table 2].
Table 2.
Perioperative variables
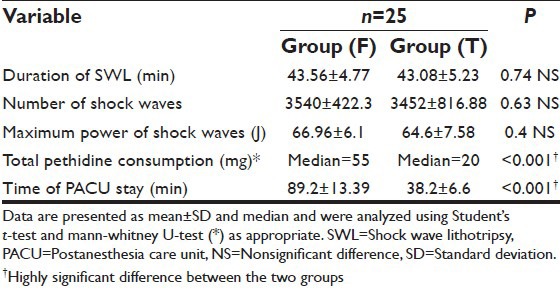
Rescue analgesia in the form of pethidine 0.25 mg/kg was administered in both groups. Statistical analysis showed highly significant decrease (P < 0.001) in the total amount of pethidine used during the procedure and in the PACU time in group (T) (median = 20 mg) compared to group (F) (median = 55 mg) [Table 2].
There was a highly significant decrease (P < 0.001) in the time of PACU stay in group (T) (38.2 ± 6.6 min) compared to group (F) (89.2 ± 13.39 min) [Table 2].
Visual analog scale scores showed a highly significant decrease in group (T) than group (F) at 10, 20, 30, and 40 min during the procedure [Figure 2], and at 10 min intervals in the PACU (P < 0.001) [Figure 3].
Figure 2.
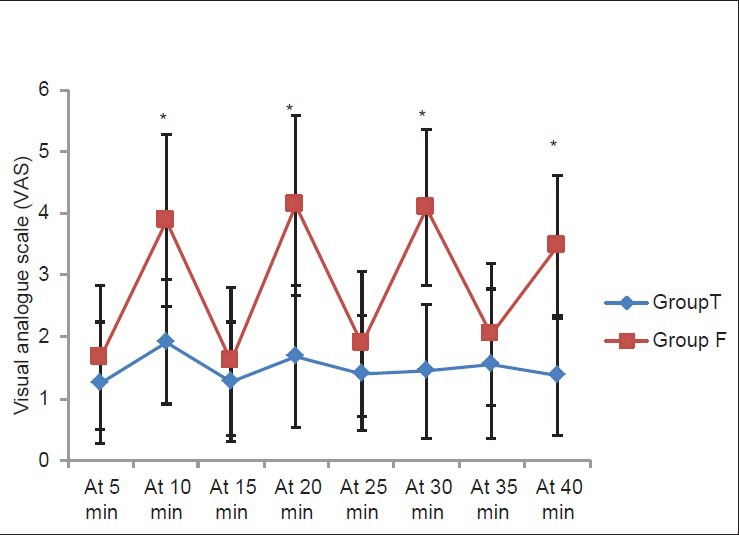
Visual analog scale values during shock wave lithotripsy. Data are presented as mean ± standard deviation. *P<0.001 = Highly significant compared to group (T)
Figure 3.
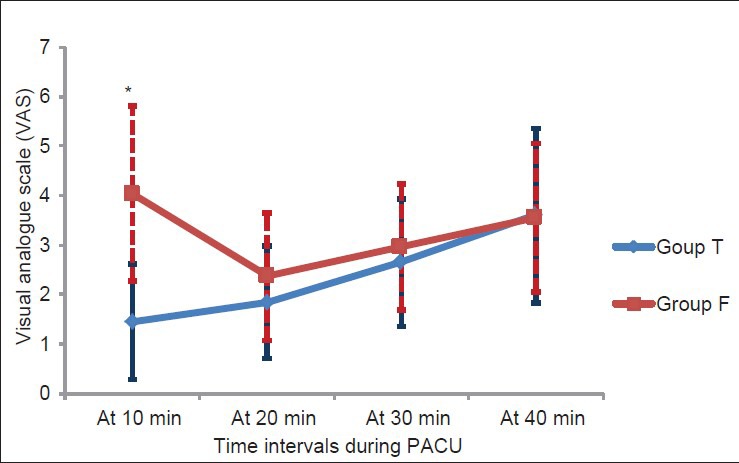
Visual analog scale values during postanesthesia care unit time. Data are presented as mean ± standard deviation. *P<0.001 = Highly significant compared to group (T)
Sedation scores showed highly significant increase in group (F) compared to group (T) at 15, 25, and 35 min during the procedure [Table 3] and at 20 min during the PACU time (P < 0.001) [Table 4], while there was a significant increase in sedation scores in group (F) than those in group (T) at 10 min (P = 0.03) and 30 min (P = 0.007) during the PACU time [Table 4].
Table 3.
RSS during SWL
Table 4.
RSS in the PACU
There were no reported cases of bradycardia (HR < 50 beats/min), hypotension (MAP < 20% of baseline), hypoxia (SaO2 < 93%) or signs of local anesthetic toxicity in both groups [Table 5].
Table 5.
Perioperative side effects
Six patients in group (F) (24%) developed respiratory depression (RR < 10 breaths/min) without hypoxia compared to 0% in group (T) (P = 0.022) [Table 5].
Although one patient in group (F) (4%) complained of mild pruritus, it was statistically insignificant when compared to group (T) (0%) [Table 5].
Eight patients have had nausea (32%) and 6 have had vomiting (24%) in group (F), which was statistically significant when compared to group (T) (0%) (P = 0.01 and 0.022, respectively) [Table 5].
DISCUSSION
In the present study, we found that ultrasound-guided unilateral TAP block compared to IV fentanyl-was a very good analgesic technique for ureteric SWL as it provided a very good analgesia during the procedure with significantly lower doses of rescue analgesia, lower sedation scores and shorter times to discharge from the PACU without significant side effects.
The clinical efficacy of TAP block has been proven in many clinical trials of adults undergoing abdominal operations. It has also been used for postoperative analgesia following renal transplantation, reconstruction flaps of the anterior abdominal wall and inguinal lymphadenectomy.[9,10,11,13,17,18] McDonnell's et al. injected iopamidol contrast, and then, using computerized tomography and magnetic resonance imaging, studied the spread of the contrast within the TAP into three volunteers. They found that the contrast spread from the superior margin of the iliac crest up to the costal margin and extended posteriorly till the quadratus lumborum muscle.[14] A cadaveric study was done by Tran et al. in which 20 ml of aniline blue dye was injected into the TAP in the mid-axillary line. They noticed spread of the dye between the iliac crest, the costal margin and the lateral border of the rectus abdominis sheet.[15]
Although TAP block has been always used as a part of multimodal analgesia in combination with other drugs,[10] we used it in our study as the sole analgesic technique during ureteric SWL in which the shock wave emitter was applied to the ipsilateral anterior abdominal wall. The newer versions of SWL machines have reduced the amount of analgesia and sedation required during the procedure because of their lower shock wave output energy which is less painful than it used to be.[19] Rickford et al. presented a prospective randomized study to evaluate the use of general, epidural, and spinal anesthesia during ESWL. They found that general anesthesia has the advantages of being rapid and reliable, but resulted in postoperative nausea, vomiting, and sore throat. Epidural anesthesia consumed more time than spinal anesthesia and more supplementary drugs like fentanyl and midazolam. Spinal anesthesia showed a high incidence of postspinal headache. But both epidural and spinal anesthesia conferred awake and cooperative patients.[20]
In our study, we found that ultrasound-guided TAP block was an easy, rapid, and reliable analgesic technique with no significant side effects. Patients were awake and cooperative during the procedure, and they were early ambulated and discharged from the PACU. Ali and El Ghoneimy presented a comparative study between dexmedetomidine and fentanyl as adjuvant to propofol in children undergoing ESWL. They found that the RR values in the propofol/fentanyl group were significantly lower than the baseline throughout the procedure compared to the propofol/dexmedetomidine group and were significantly lower than the propofol/dexmedetomidine group at all-time intervals during the procedure.[21] These results are similar to the results obtained in our study. There was a significant decrease in the RR values in the fentanyl group (although without hypoxia) and was managed conservatively. In addition, nausea and vomiting was significant in the fentanyl group in comparison to the TAP block group; yet all patients responded to IV ondansetron 4 mg.
Regarding sedation scores, there was a highly significant increase in the mean values in group (F) compared to group (T) at 15, 25, and 35 min during SWL and at 20 min during the PACU time.
The strong analgesic effect of ultrasound-guided TAP block is due to block of the lower six thoracic and upper lumbar sensory afferents,[14,15] where the anterior rami of the lower six thoracic nerves and the first lumbar nerve provide sensory supply to the skin, muscles and parietal peritoneum of the anterior abdominal wall. The ilio-hypogastric, ilio-inguinal, intercostal, and subcostal nerves pass through the plane between the internal oblique and TAMs to provide sensory supply to the abdominal wall.[14,18] To our knowledge, this is the first study which evaluated the efficacy and safety of ultrasound-guided unilateral TAP block for ureteric SWL.
Limitations to the technique described in our study (i.e. ultrasound-guided TAP block) include being restricted to ureteric stones in which the shock wave emitter would be applied to the ipsilateral anterior abdominal wall and not renal stones where the emitter would be applied posterior to the mid-axillary line. Second, our study was extended only till the end of PACU time. Further studies on a larger number of patients are required for long-term follow-up.
CONCLUSION
Ultrasound-guided unilateral TAP block is an effective alternative analgesic technique for ureteric SWL as it provides an optimal analgesic condition, less rescue analgesia, less intra-and postprocedural sedation, early ambulation, and early discharge from PACU with no significant side effects.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Chaussy C, Brendel W, Schmiedt E. Extracorporeally induced destruction of kidney stones by shock waves. Lancet. 1980;2:1265–8. doi: 10.1016/s0140-6736(80)92335-1. [DOI] [PubMed] [Google Scholar]
- 2.Weber A, Koehrmann KU, Denig N, Michel MS, Alken P. What are the parameters for predictive selection of patients requiring anesthesia for extracorporeal shockwave lithotripsy? Eur Urol. 1998;34:85–92. doi: 10.1159/000019690. [DOI] [PubMed] [Google Scholar]
- 3.Basar H, Yilmaz E, Ozcan S, Buyukkocak U, Sari F, Apan A, et al. Four analgesic techniques for shockwave lithotripsy: Eutectic mixture local anesthetic is a good alternative. J Endourol. 2003;17:3–6. doi: 10.1089/089277903321196706. [DOI] [PubMed] [Google Scholar]
- 4.Burmeister MA, Brauer P, Wintruff M, Graefen M, Blanc I, Standl TG. A comparison of anaesthetic techniques for shock wave lithotripsy: The use of a remifentanil infusion alone compared to intermittent fentanyl boluses combined with a low dose propofol infusion. Anaesthesia. 2002;57:877–81. doi: 10.1046/j.1365-2044.2002.02820.x. [DOI] [PubMed] [Google Scholar]
- 5.Beloeil H, Corsia G, Coriat P, Riou B. Remifentanil compared with sufentanil during extra-corporeal shock wave lithotripsy with spontaneous ventilation: A double-blind, randomized study. Br J Anaesth. 2002;89:567–70. doi: 10.1093/bja/aef202. [DOI] [PubMed] [Google Scholar]
- 6.Demir E, Kilciler M, Bedir S, Erten K, Ozgok Y. Comparing two local anesthesia techniques for extracorporeal shock wave lithotripsy. Urology. 2007;69:625–8. doi: 10.1016/j.urology.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 7.Gupta NP, Kumar A. Analgesia for pain control during extracorporeal shock wave lithotripsy: Current status. Indian J Urol. 2008;24:155–8. doi: 10.4103/0970-1591.40607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gesztesi Z, Rego MM, White PF. The comparative effectiveness of fentanyl and its newer analogs during extracorporeal shock wave lithotripsy under monitored anesthesia care. Anesth Analg. 2000;90:567–70. doi: 10.1097/00000539-200003000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Carney J, McDonnell JG, Ochana A, Bhinder R, Laffey JG. The transversus abdominis plane block provides effective postoperative analgesia in patients undergoing total abdominal hysterectomy. Anesth Analg. 2008;107:2056–60. doi: 10.1213/ane.0b013e3181871313. [DOI] [PubMed] [Google Scholar]
- 10.McDonnell JG, O’Donnell B, Curley G, Heffernan A, Power C, Laffey JG. The analgesic efficacy of transversus abdominis plane block after abdominal surgery: A prospective randomized controlled trial. Anesth Analg. 2007;104:193–7. doi: 10.1213/01.ane.0000250223.49963.0f. [DOI] [PubMed] [Google Scholar]
- 11.Elkassabany N, Ahmed M, Malkowicz SB, Heitjan DF, Isserman JA, Ochroch EA. Comparison between the analgesic efficacy of transversus abdominis plane (TAP) block and placebo in open retropubic radical prostatectomy: A prospective, randomized, double-blinded study. J Clin Anesth. 2013;25:459–65. doi: 10.1016/j.jclinane.2013.04.009. [DOI] [PubMed] [Google Scholar]
- 12.Mukhtar K, Singh S. Transversus abdominis plane block for laparoscopic surgery. Br J Anaesth. 2009;102:143–4. doi: 10.1093/bja/aen338. [DOI] [PubMed] [Google Scholar]
- 13.Jankovic Z. Transversus abdominutesis plane block: The holy grail of anaesthesia for (lower) abdominutesal surgery. Periodicum Biologorum. 2009;111:203–8. [Google Scholar]
- 14.McDonnell JG, O’Donnell BD, Farrell T, Gough N, Tuite D, Power C, et al. Transversus abdominis plane block: A cadaveric and radiological evaluation. Reg Anesth Pain Med. 2007;32:399–404. doi: 10.1016/j.rapm.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 15.Tran TM, Ivanusic JJ, Hebbard P, Barrington MJ. Determination of spread of injectate after ultrasound-guided transversus abdominis plane block: A cadaveric study. Br J Anaesth. 2009;102:123–7. doi: 10.1093/bja/aen344. [DOI] [PubMed] [Google Scholar]
- 16.Consales G, Chelazzi C, Rinaldi S, De Gaudio AR. Bispectral Index compared to Ramsay score for sedation monitoring in intensive care units. Minerva Anestesiol. 2006;72:329–36. [PubMed] [Google Scholar]
- 17.French JL, McCullough J, Bachra P, Bedforth NM. Transversus abdominis plane block for analgesia after caesarean section in a patient with an intracranial lesion. Int J Obstet Anesth. 2009;18:52–4. doi: 10.1016/j.ijoa.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 18.Rozen WM, Tran TM, Ashton MW, Barrington MJ, Ivanusic JJ, Taylor GI. Refining the course of the thoracolumbar nerves: A new understanding of the innervation of the anterior abdominal wall. Clin Anat. 2008;21:325–33. doi: 10.1002/ca.20621. [DOI] [PubMed] [Google Scholar]
- 19.Chow GK, Streem SB. Extracorporeal lithotripsy. Update on technology. Urol Clin North Am. 2000;27:315–22. doi: 10.1016/s0094-0143(05)70260-3. [DOI] [PubMed] [Google Scholar]
- 20.Rickford JK, Speedy HM, Tytler JA, Lim M. Comparative evaluation of general, epidural and spinal anaesthesia for extracorporeal shockwave lithotripsy. Ann R Coll Surg Engl. 1988;70:69–73. [PMC free article] [PubMed] [Google Scholar]
- 21.Ali AR, El Ghoneimy MN. Dexmedetomidine versus fentanyl as adjuvant to propofol: Comparative study in children undergoing extracorporeal shock wave lithotripsy. Eur J Anaesthesiol. 2010;27:1058–64. doi: 10.1097/EJA.0b013e32833e6e2d. [DOI] [PubMed] [Google Scholar]


