Abstract
Background:
There were several studies using either low dose Bupivacaine as unilateral selective spinal anesthesia (SSA) or low dose lidocaine SSA for ambulatory knee arthroscopy. There were many concerns about high failure rate, complications, and different times to home readiness discharges.
Aim of the Study:
The study aimed to: (1) Compare the clinical efficacy and side effects of two different techniques of SSA in subarachnoid block for ambulatory knee arthroscopy (2) evaluate the possibility of a shorter stay in post-anesthesia care unit (PACU) or eligibility for fast tracking anesthesia (bypassing PACU) after SSA and numbers of patient bypassed PACU (3) compare the time to ambulate and time to home readiness.
Patients and Methods:
Prospective, randomized and open study was conducted, including 50 outpatients undergoing knee arthroscopy. Patients allocated into two groups: Bupivacaine group (group B); was injected with 3 mg bupivacaine and 10 ug fentanyl intrathecally in lateral decubitus position and remained for 20 min then supine position. Lidocaine group (group L) was injected with 20 mg lidocaine, plus 25 ug fentanyl intrathecally and immediately keeps in the supine position after injection. The quality and durations of motor and sensory block were compared between groups. Sensory block assessed by pin brick method and motor block assessed by Bromage scale. Time spent in PACU, the time to ambulate, and times to home-readiness were compared. Number of patients bypassed PACU was recorded. Side effects as pain, nausea, vomiting, postdural puncture headache, transient neurological symptoms, retention of urine and pruritus were evaluated and compared after SSA.
Results:
Bupivacaine group provided unilateral spinal anesthesia with significantly longer duration of both motor and sensory blocks than bilateral spinal of lidocaine group P < 0.001 and P < 0.01 respectively. The upper dermatomal height of sensory block reached was T9 and T8 in groups B and L respectively. Group B showed more intense motor block than group L. There was no significant difference between both groups as regards postoperative side effects P > 0.05. Group L patients did not stay in PACU, and all patients bypassed it P < 0.001. Bupivacaine group patients showed significantly longer time to ambulate and time to home-readiness than lidocaine group P < 0.001 and P < 0.01 respectively.
Conclusion:
Both techniques of SSA were clinically efficient as subarachnoid block, and they had less postoperative side effects. Lidocaine spinal was more eligible for fast-tracking anesthesia than bupivacaine spinal with shorter time to ambulate and home-readiness time.
Keywords: Bupivacaine, fast-track, knee arthroscopy, lidocaine, selective spinal anesthesia
INTRODUCTION
There is a general agreement on the desired outcomes in ambulatory surgery which based on three essential goals; safe and effective anesthesia, minimal side effects and rapid recovery with discharge home as early as safely possible. Anesthetic drugs used should provide those goals and achieve faster onset, more rapid recovery and fewer side effects. All previous considerations meet together in application called fast-tracking anesthesia which used a combination of old and new drugs to provide rapid emergence from anesthesia and ensure full criteria of recovery room discharging and also ensure bypassing the acute recovery room and proceeding to step-down recovery holding area.[1] The modified Aldrete's score may not be adequate after ambulatory surgeries requiring either general or regional anesthesia because it failed to consider common side effects as pain, nausea, vomiting and ability to void. Therefore, new fast-track scoring system which included the modified Aldrete's score as well as an assessment of pain and emesis had been proposed.[2] Selective spinal anesthesia (SSA) was defined as “minimal doses of intrathecal agents are used, so that only the nerve roots supplying a specific area and only the modalities that need to be anesthetized are affected.”[3] SSA either unilateral or bilateral was used before with different local anesthetics and different adjuncts. Unilateral selective spinal with different doses of Bupivacaine was accused by high failure rate and delay of voiding. Bilateral selective spinal with different doses of lidocaine was accused by high transient neurological symptoms (TNS).[4] Knee arthroscopy is a common procedure which performed in ambulatory setting. Arthroscopic exploration of knee may last only 10 min up to 1 h, whereas operation of meniscus, capsules and ligaments, on synovial of the knee.[5] The aim of the current study was to compare between two techniques of SSA as regards the eligibility to meet the criteria of fast-track anesthesia in recovery profiles and time of home-readiness discharging as well as the clinical efficacy and side effects of both techniques as SSA in ambulatory knee arthroscopy.
PATIENTS AND METHODS
After approval by the ethics committee of our hospital, written informed consents were obtained from all patients. A prospective, randomized study was conducted during the years 2013–2014 in King Abdul-Aziz hospital in Kingdom of Saudi Arabia. Patients were scheduled for elective knee arthroscopy like arthroscopic exploration of knee last only 10 min up to 1 h, whereas operation of meniscus, capsules and ligaments, on synovial of the knee and longer operation for osteochondritis or severe osteomyelitis was excluded. The study enrolled 50 patients who were American Society of Anesthesiologists (ASA) physical status I and II, aged 18–60 years, and from both sexes. Exclusion criteria were unwilling patients, coagulopathies, cardiac diseases, hypertensive patients, neurological disorders, spinal deformity and patients with skin infection of the back at site of lumbar block. Patients received 10 mg of oral diazepam and prophylactic antibiotics. All patients were preloaded with 500 mL of 0.9% saline. Standard monitoring (electrocardiogram, noninvasive blood pressure and pulse oximetry) was used for all patients. Hypotension and bradycardia were defined as a decrease >20% of base-line of blood pressure or heart rate, and treated by ephedrine or atropine respectively. A tourniquet around the thigh, inflated 300–350 mmHg, was used in the operative extremity after anesthesia. Under all aseptic precautions, after infiltrating the skin with local anesthetic, subarachnoid block was performed with 25 Gauge, Quincke-Babcock spinal needle (Becton-Dickinson) as midline approach at L3–4 intervertebral space. Fifty patients were randomized by a computer generated random number table and by 1:1 ratio into two groups of 25 each. Group B (Bupivacaine group) or unilateral spinal group: Patients injected with 3 mg hyperbaric Bupivacaine (Astra Zeneca, USA) 0.5% (0.6 ml) plus fentanyl (Janssen Cilag, Belgium) 10 μg (0.2 ml) total volume was 0.8 ml. The study drug was injected by rate 0.4 ml/min (over 2 min). The specific gravity of the solution containing marcaine and fentanyl (3:1) was 1.026 at 20°C. Intrathecal injection was done on the lateral decubitus position on the operative limb. Patients remained on that position for 20 min then turned on supine position. The bevel of the needle was turned laterally towards the nerve roots involved. Group B patients came 30 min early to the operating room (OR) to avoid delaying OR time. Group L (lidocaine group) or bilateral spinal group: Patients received intrathecal injections with lidocaine (Hospira, USA) 2% 1 ml (20 mg) plus fentanyl 25 μg (0.5 ml) then completed to 3 ml by sterile water for injection. Patients injected on sitting a position over 10 s then immediately turn to the supine position. Lidocaine solution was hypobaric and had specific gravity 1.002. The direction of the bevel of the needle oriented caudally. In both groups; Sensory level and motor block were assessed by pinprick and modified Bromage scale (0 = full movement, 1 = movement of knee only, 2 = movement of ankles only, and 3 = no movement) respectively, every 5 min after lidocaine till establishing fixed sensory level (two consecutive assessment) and every 5 min till 30 min after Bupivacaine then at the end of surgery and in recovery room every 15 min till discharging home. The response to surgical stimulation was evaluated by ordinal scale (none, mild and severe), the rescue analgesia started from fentanyl 100 μg intravenous (I.V.) till turned to general anesthesia (GA) and it was considered failure of spinal anesthesia which recorded and excluded from the study. Acceptable operating condition was recorded from the surgeon as scale (excellent = 3, good = 2, fair = 1 and bad = 0) by same surgeon. The duration of sensory block judged as time from the block till first postoperative analgesia required by the patients. The duration of motor block by starting from the return to Bromage scale of 0–1. Tourniquet tolerance time was recorded and compared between groups (patients start to complain from Tourniquet). Intraoperative hypotension or bradycardia was reported and managed in both groups. Postoperative pain was assessed by visual analogue score from (0 = no pain and 10 = the worst pain imaginable) and postoperative analgesia was given according to it as pethidine 1 mg/kg I.V. or paracetamol 1 g I.V. The criteria to transfer to ambulatory surgical unit (ASU) were full recovery from motor block and sensory block not above T12, vital stability and no pain. If the mentioned criteria were fulfilled at the end of the operation after releasing of the tourniquet, the patient bypassed post-anesthesia care unit (PACU); it was fast-tracked. After SSA the PACU discharge was evaluated by using both the new fast-tracking scoring system (modified Aldrete's score plus pain and postoperative nausea and vomiting [PONV] assessment) and minimum score was 12/14 with no zero scores was required for the patients to be fast-tracked. Before transferring to ASU the patient had to be able to sit up, and patients with vertigo, somnolence or wanted to lie down, were kept in PACU even though their fast-tracking score was ≥12/14. Home – discharge criteria were: Vitally stable, oriented, no PONV, no or mild pain <4, no bleeding, ability to walk with crutches (if surgeon allowed ambulation), no headache and ability to void. Time in PACU and time to ambulate were recorded. Time to home-readiness was measured from the time of spinal block establishing. Number of patients bypassed PACU was recorded. Complications in PACU and ASU were assessed and recorded as pain, PONV, pruritus, postdural puncture headache (PDPH), urine retention and TNS. Pain was managed as mentioned. PONV was treated by ondansetron 4 mg I.V. Pruritus was assessed by (0 = no and 10 = the worst) and treated with 0.004–0.01 mg naloxone or diphenhydramine if needed. PDPH was followed up in surgical word if founded and we treated by bed rest for 24 h with no pillow and plenty of water or fluid up and caffeine tablets up to dural patch. TNS was asked as any pain referred to the back of the thigh or buttocks. PDPH and TNS were evaluated by telephone interviews after 24 h, 3 and 7 days and the patient was requested to come again to the hospital if needed for proper management. Retention of urine was assessed before leaving the recovery room. If the patients were unable to void and urinary retention occurred (full bladder on palpation, inability to micturate 8 h postoperatively with discomfort) these patients were advised to contact hospital and to insert urinary catheter. This occurrence was considered a failure of ambulatory anesthesia. Written instructions for the postoperative period at home including a contact place and person were given to the patients or their relative on home discharge.
Statistical analysis
The sample size of 25 patients per study group was calculated to detect >20% difference in time to home-readiness (184 min and 153 min) between both groups to achieve a power of 80% (α =0.05). The power value was evaluated with power and sample size package program. We compared the outcomes between the groups by calculating P value using Student's t-test, Chi-square and Fisher's exact tests. Continuous data were expressed as mean ± standard deviation while categorical data were expressed as numbers and percentage. A two-tailed P < 0.05 was considered statistically significant. SPSS package for Window (version 12) (SPSS Inc., Chicago, IL) was used.
RESULTS
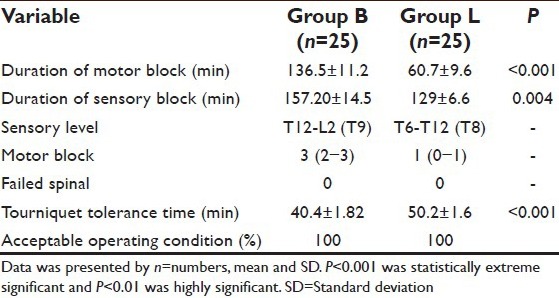
There were no significant differences between both groups as regards the demographic data and duration of surgery P > 0.05 [Table 1]. Duration of motor and sensory blocks was significantly longer in bupivacaine group than lidocaine group 136.5 ± 11.2 and 157.2 ± 14.5 min versus 60.7 ± 9.6 and 129 ± 6.6 min (P < 0.001 and P < 0.01) respectively. Bupivacaine group had more intense motor block than lidocaine group (2–3 vs. 0–1) on Bromage scale. The highest sensory level in group B was T9 versus T8 in the lidocaine group. There was no failed spinal in both groups. There was not any bradycardia or hypotension in patients of both groups. Group L showed longer tourniquet tolerance time than Bupivacaine group (50.2 ± 1.6 min vs. 40.4 ± 1.82 min) respectively (P < 0.001). There was acceptable operating condition 100% in both groups [Table 2]. There was no rescue analgesia intraoperatively in both groups.
Table 1.
Demographic data
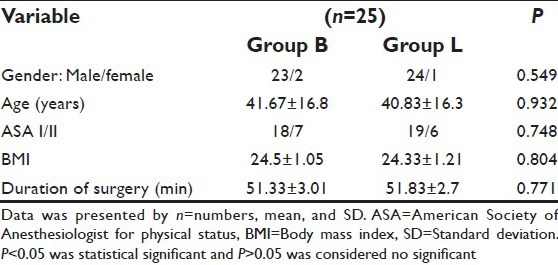
Table 2.
Clinical efficacy of subarachnoid block
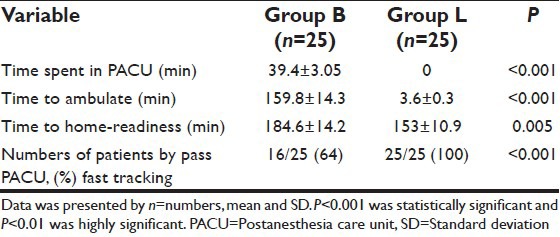
Both groups had low pain score postoperatively (2–3) 1 versus (2.1–3) 0.9 P > 0.05. There were 2 patients in each group suffered from PONV. Group B showed urine retention 2/25 (8%). Lidocaine group showed more Pruritus than Bupivacaine group (7/25 vs. 5/25). None of the patients developed TNS till 7 days postoperatively. Three patients developed PDPH (2 in group B and one in group L) after 7–10 days [Table 3]. There were 9 patients in group B stayed in PACU for 39.4 ± 3.05 min and none of the patients of group L stayed in it (P < 0.001). Patients in group L showed extremely and highly significant shorter ambulation and home-readiness times than patients in group B (3.6 ± 0.3 min and 153 ± 10.9 min vs. 159.8 ± 14.3 min and 184.6 ± 14.2 min) P < 0.001 and P < 0.01 respectively. All patients in group L bypassed PACU by 100% and patients in group B bypassed PACU by 64% (P < 0.001) [Table 4].
Table 3.
Postoperative side effects of SSA
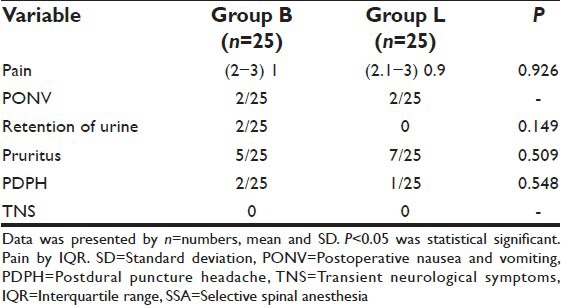
Table 4.
Recovery profile
DISCUSSION
The current study aimed to evaluate two different techniques of SSA in ambulatory knee arthroscopy which was a short procedure requiring short ambulatory anesthesia. In our study, the duration of knee arthroscopy was 51 min (mean), and we excluded any prolonged operation such as osteochondritis or osteomyelitis which required longer duration. The golden roles of ambulatory anesthesia were to provide safe and effective anesthesia, minimal postoperative side effects and safe, rapid, and early home discharging. The conventional spinal anesthesia was unsuitable for ambulatory anesthesia because it was not fulfilling the previous criteria, and there were residual motor block and delayed voiding. Fast-tracking anesthesia not only covered all criteria roles of ambulatory anesthesia but also provided saving of the cost and more rapid home discharging.[1] The aim of the current study was to evaluate that SSA effective as fast-tracking anesthesia. In the present study, we provided two different types of SSA. They were different in anesthetic agent (dose and type), baricity, and technique. They were similar as low-dose, low volume and slow rate of injection. SSA had been defined as “the practice of employing minimal doses of intrathecal agents, so the only nerve roots supplying specific area and only the modalities that required to be anesthetized are affected.”[4] In the current study we used the concept of SSA in two different techniques. We compared between unilateral and bilateral), (hypobaric and hyperbaric) and (low dose Bupivacaine and low-dose lidocaine) SSA. Patients of group B received Bupivacaine by low dose 3 mg plus fentanyl 10 μg injected slowly (0.4 ml/min) intrathecally in lateral decubitus position on operating limb that maintained for 20 min after injection. This technique provided unilateral spinal anesthesia which selectively blocks the operating limb only with a sensory level up to T9 and intense motor block on modified Bromage scale (2–3). Duration of motor and sensory blocks was sufficient to cover the duration of surgery and postoperative period 136 min of motor block and 157 min of sensory block. In group L; the duration of sensory (129 min) and motor (60 min) blocks were sufficient for both intraoperative and postoperative times. That block achieved acceptable operating condition by 100%. None of the patients received any rescue analgesia intraoperatively, and these matched with Korhonen.[5] There was no failed spinal anesthesia as block but 2 patients could not achieve unilateral spinal but bilateral spinal with agreement of Casati et al. who concluded inability to control the direction of the flow of the local anesthetic during the injection by different used spinal needles.[6] In our study, there was no event of hypotension or bradycardia that ensured the hemodynamic stability of SSA due to good selection of patients without any medical or cardiac diseases, low doses of adjuvant as fentanyl from 10 to 25 ug, selective block of sensory more than motor block, low doses of lidocaine and bupivacaine, preload fluid and finally there was not sympathectomy as conventional spinal anesthesia.[4,5] Hyperbaric bupivacaine had specific gravity 1.026 when injected very slowly preventing turbulence flow. A cerebrospinal fluid surrogate can be under layered without turbulence which was very important for unilateral block so any change in patient's position will affect spread of block so we kept the patients in decubitus position for at least 20 min.[4] The duration of sensory and motor block were suitable for ambulatory anesthesia in Bupivacaine group and matched with previous studies.[5] In the current study, we used low-dose lidocaine 20 mg plus fentanyl 25 μg as hypobaric solution. Its specific gravity was 1.002. The hypobaric solution was injected intrathecally in sitting a position and by fast rate over 20 s then patients were immediately laid down. The sensory level was T8 and little motor block (0–1) on modified Bromage scale. That block either sensory or motor was acceptable for the procedure by 100%. The spinal block was bilateral and efficient as none of the patients needed to rescue analgesia that matched with the study of Buckenmaier et al.[7] The duration of motor and sensory blocks by small lidocaine or bupivacaine dose was suitable for the concept of ambulatory anesthesia. Both groups tolerated to tourniquet because S1 segment was blocked by both techniques. The unilateral block of S1 resolved earlier than bilateral block that was matched with the previous study.[5] In the present study, we chose fentanyl as adjunct to local anesthetics to improve intraoperative analgesia and the quality of anesthesia without prolonged or delayed discharging time which matched with previous studies.[8] In the present study, we evaluated postoperative side effects of both techniques and how they matched with the concept of ambulatory and fast-tracking anesthesia. Both groups showed low pain scores postoperative which needed only paracetamol upon discharging home. The cause of low pain score from low doses of intrathecal opioids that were balanced between their analgesic effects and their side effects. Both groups showed low percentages of PONV only 8% of each which still less than PONV after GA (19%) and these matched with previous studies.[8] It was acceptable because it was mild and not needed for treatment or hospital admission. The urine retention was noted in only 2/25 (8%) in Bupivacaine group that was mild and not requiring urinary catheter, and they were voided before discharging home. None of the patients in Lidocaine group showed urine retention. Both results were mismatched with Mulroy et al., who reported high incidence of retention (30%) post lidocaine spinal.[9] The incidences of Pruritus were 20% and 28% in both Bupivacaine and lidocaine respectively due to intrathecal fentanyl, but still mild and easily treated with diphenhydramine only. These results were matched with Yeh et al. who concluded that Pruritus was dose dependent,[10] and mismatched with Gürkan and Toker who reported that Pruritus was related to local anesthetic agent (Bupivacaine more than lidocaine).[11] None of the patients complained of PDPH before discharging home but during telephone interviews we reported 2 patients in Bupivacaine group and only one patient in lidocaine group where it was mild and only needed supportive treatment as hydration and bed rest for 24 h and did not need hospital admission. These results were accepted and can be reduced by replacing the Quincke needle to pencil-point needle as proved by Santanen et al.[12] Both groups did not show TNS that mismatched with Pollock, who reported 4% of TNS with lidocaine 20 mg.[13] The patients undergoing ambulatory anesthesia should be carefully selected and any extended stay up to 23 h or overnight should not be considered ambulatory surgery as proved by McGrath and Chung.[14] Recovery process can be divided into three phases; early, intermediate and late recovery. Early recovery last from discontinuation of anesthesia until patients recovered their protective reflexes and motor function. It takes place in fully equipped area and under supervision of highly trained nursing staff in PACU. Any technique of anesthesia made the early stage recovery so fast, that is, safe bypass PACU, it was considered as fast-tracking anesthesia. ASU or phase II is less expensive; less equipped and not need extensive monitoring. During ASU the patients were assessed to discharging home, and the total discharge time had been used as a measure of efficacy when comparing anesthetic agents or techniques. The late stage recovery when the patients fulfilled criteria of safe home discharging. The lack of identical fast-tracking and home-readiness criteria between studies makes the evaluation of the efficacy of different anesthetic agents and techniques difficult.[5] In the current study when comparing between two techniques of SSA as regards the recovery profiles we used the criteria to transfer to ASU when the patients were fully recovered from motor block and sensory block not above T12 and stable vital signs and when achieved at the end of surgery, the patients bypassed PACU. We used mentioned criteria plus the fast-tracking scoring system of White and Song that required a minimum score 12/14 with no zero scores was required.[15] We found that 9 patients (36%) in bupivacaine group transferred to PACU and stayed for 39.4 ± 3.05 min but none of patients in lidocaine group stayed in PACU and all patients bypassed it because the patients in bupivacaine group had longer time of motor block and sensory level was above T12 and it was the same reason of delaying of ambulation time which was 159.8 ± 14.3 versus 3.9 ± 0.3 min in lidocaine group. Patients in the lidocaine group showed minimal or no motor block and low-level sensory block below T12 so it was easy to be transferred directly to ASU and bypassed PACU. These results agreed with Pamela et al. when they found the ambulation time after SSA with lidocaine was 3.1 ± 0.9 min.[16] When the patients transferred to ASU, we assessed them with home-readiness criteria and we found that total discharge time or the time to home-readiness was 184.6 ± 14.2 min versus 153 ± 10.9 min in bupivacaine and lidocaine groups respectively. The main reason of delaying of total discharging time in the bupivacaine group was delaying in voiding (mild) retention of urine in two patients. These results matched with Ben-David et al. when they found a home–readiness time after knee arthroscopy done under SSA with low-dose lidocaine and fentanyl, or hyperbaric bupivacaine was 145 and 202 min respectively.[17] Larkin et al. suggested that patients of low risk (nonpelvic surgery or no history of urinary retention) did not need to void before being discharged home which was not used in our study to ensure safety of our patients.[18] Williams et al. suggested scoring system like White and song scoring system with adding shivering and orthrostasis when comparing general and neuraxial anesthesia.[19] In the current study the mean age in both groups was 40 years, average of age from 18 to 60 years and from ASA I and II. We excluded any patients with medical or cardiac diseases to ensure safety even SSA was safe in the current study as regards hemodynamic stability and safe home discharging and that was confirmed in the previous study which studied the effect of SSA on postoperative recovery and discharge criteria among geriatric patients over than 65 years.[20] in the current study we selected short procedures to be applicable with the concept of ambulatory surgery and we select type of patient as we excluded any cardiac or medical diseases patients, we select age of patients, and type of SSA to ensure rapid, safe, and efficient fast track anesthesia. In our study, we tried to ensure safety to our patients by; written instructions to the patients or their relatives upon home discharging to cover all delayed side effects of spinal as PDPH and TNS. We provided contact number, person and place to follow up our patients through regular interviews by telephone. We realized that if the study was carried out as blind approach, it would be better but because there were two different techniques, it was difficult. We used different volumes of local anesthetics to ensure the different baricity of the solutions (hypobaric versus hyperbaric). The estimation of the cost was not evaluated which considered as a weak point of the study.
CONCLUSION
Low dose lidocaine and fentanyl SSA as bilateral and hypobaric anesthesia and unilateral hyperbaric bupivacaine by small dose SSA were efficient clinically in ambulatory knee arthroscopy. Lidocaine SSA was more eligible for the concept of fast-tracking anesthesia. Both techniques were suitable for ambulatory anesthesia with acceptable postoperative side effects. Lidocaine SSA had shorter times of ambulation and home-readiness than bupivacaine SSA.
ACKNOWLEDGMENT
ALL members of Anesthesia Department in Prince Salman Military Hospital.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Millar J., II Fast-tracking in day surgery. Is your journey to the recovery room really necessary? Br J Anaesth. 2004;93:756–8. doi: 10.1093/bja/aeh277. [DOI] [PubMed] [Google Scholar]
- 2.Song D, Chung F. Fast-tracking in ambulatory anesthesia. Can J Anaesth. 2001;48:622–5. doi: 10.1007/BF03016193. [DOI] [PubMed] [Google Scholar]
- 3.Vaghadia H, Stewart AV, Collins L, Mitchell GW. Small dose selective spinal anesthesia for short duration outpatients’ gynecological laparoscopy: Recovery characteristics compared with propofol anesthesia. Br J Anaesth. 2001;86:570–2. doi: 10.1093/bja/86.4.570. [DOI] [PubMed] [Google Scholar]
- 4.Moemen ME. Selective spinal anesthesia. Eg J Anesth. 2003;19:99–106. [Google Scholar]
- 5.Korhonen AM. Discharge home in 3 h after selective spinal anaesthesia: Studies on the quality of anaesthesia with hyperbaric bupivacaine for ambulatory knee arthroscopy. Acta. Anaesthesiol Scand. 2006;50:627–703. [Google Scholar]
- 6.Casati A, Fanelli G, Cappelleri G, Leoni A, Berti M, Aldegheri G, et al. Does speed of intrathecal injection affect the distribution of 0.5% hyperbaric bupivacaine? Br J Anaesth. 1998;81:355–7. doi: 10.1093/bja/81.3.355. [DOI] [PubMed] [Google Scholar]
- 7.Buckenmaier CC, 3rd, Nielsen KC, Pietrobon R, Klein SM, Martin AH, Greengrass RA, et al. Small-dose intrathecal lidocaine versus ropivacaine for anorectal surgery in an ambulatory setting. Anesth Analg. 2002;95:1253–7. doi: 10.1097/00000539-200211000-00028. [DOI] [PubMed] [Google Scholar]
- 8.Goel S, Bhardwaj N, Grover VK. Intrathecal fentanyl added to intrathecal bupivacaine for day case surgery: A randomized study. Eur J Anaesthesiol. 2003;20:294–7. doi: 10.1017/s0265021503000462. [DOI] [PubMed] [Google Scholar]
- 9.Mulroy MF, Salinas FV, Larkin KL, Polissar NL. Ambulatory surgery patients may be discharged before voiding after short-acting spinal and epidural anesthesia. Anesthesiology. 2002;97:315–9. doi: 10.1097/00000542-200208000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Yeh HM, Chen LK, Lin CJ, Chan WH, Chen YP, Lin CS, et al. Prophylactic intravenous ondansetron reduces the incidence of intrathecal morphine-induced pruritus in patients undergoing cesarean delivery. Anesth Analg. 2000;91:172–5. doi: 10.1097/00000539-200007000-00032. [DOI] [PubMed] [Google Scholar]
- 11.Gürkan Y, Toker K. Prophylactic ondansetron reduces the incidence of intrathecal fentanyl-induced pruritus. Anesth Analg. 2002;95:1763–6. doi: 10.1097/00000539-200212000-00054. [DOI] [PubMed] [Google Scholar]
- 12.Santanen U, Rautoma P, Luurila H, Erkola O, Pere P. Comparison of 27-gauge (0.41-mm) whitacre and quincke spinal needles with respect to post-dural puncture headache and non-dural puncture headache. Acta Anaesthesiol Scand. 2004;48:474–9. doi: 10.1111/j.0001-5172.2004.00345.x. [DOI] [PubMed] [Google Scholar]
- 13.Pollock JE. Neurotoxicity of intrathecal local anaesthetics and transient neurological symptoms. Best Pract Res Clin Anaesthesiol. 2003;17:471–84. doi: 10.1016/s1521-6896(02)00113-1. [DOI] [PubMed] [Google Scholar]
- 14.McGrath B, Chung F. Postoperative recovery and discharge. Anesthesiol Clin North America. 2003;21:367–86. doi: 10.1016/s0889-8537(02)00080-9. [DOI] [PubMed] [Google Scholar]
- 15.White PF, Song D. New criteria for fast-tracking after outpatient anesthesia: A comparison with the modified Aldrete's scoring system. Anesth Analg. 1999;88:1069–72. doi: 10.1097/00000539-199905000-00018. [DOI] [PubMed] [Google Scholar]
- 16.Pamela HL, Vaghadia H, Henderson C, Martin L, Michell GW. Small-dose selective spinal anesthesia for short duration outpatient laparoscopy: Recovery characteristics compared to desflurane anesthesia. Anesth Analg. 2002;48:474–9. doi: 10.1097/00000539-200202000-00021. [DOI] [PubMed] [Google Scholar]
- 17.Ben-David B, Maryanovsky M, Gurevitch A, Lucyk C, Solosko D, Frankel R, et al. A comparison of minidose lidocaine-fentanyl and conventional-dose lidocaine spinal anesthesia. Anesth Analg. 2000;91:865–70. doi: 10.1097/00000539-200010000-00018. [DOI] [PubMed] [Google Scholar]
- 18.Larkin KL, Salinas FV, Mulroy MF. Do ambulatory surgery patients need to void after a short acting spinal or epidural anesthetic? (abstract) Anesthesiology. 2000;93:A42. doi: 10.1097/00000542-200208000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Williams BA, Kentor ML, Vogt MT, Vogt WB, Coley KC, Williams JP, et al. Economics of nerve block pain management after anterior cruciate ligament reconstruction: Potential hospital cost sasvings via associated postanesthesia care unit bypass and same-day discharge. Anesthesiology. 2004;100:697–706. doi: 10.1097/00000542-200403000-00034. [DOI] [PubMed] [Google Scholar]
- 20.Ornek D, Metin S, Deren S, Un C, Metin M, Dikmen B, et al. The influence of various anesthesia techniques on postoperative recovery and discharge criteria among geriatric patients. Clinics (Sao Paulo) 2010;65:941–6. doi: 10.1590/S1807-59322010001000003. [DOI] [PMC free article] [PubMed] [Google Scholar]


