Abstract
Over the period 1990–2010, the increase in life expectancy for males in New York City was 6.0 years greater than for males in the United States. The female relative gain was 3.9 years. Male relative gains were larger because of extremely rapid reductions in mortality from HIV/AIDS and homicide, declines that reflect effective municipal policies and programs. Declines in drug- and alcohol-related deaths also played a significant role in New York City's advance, but every major cause of death contributed to its relative improvement. By 2010, New York City had a life expectancy that was 1.9 years greater than that of the US. This difference is attributable to the high representation of immigrants in New York's population. Immigrants to New York City, and to the United States, have life expectancies that are among the highest in the world. The fact that 38 percent of New York's population consists of immigrants, compared to only 14 percent in the United States, accounts for New York's exceptional standing in life expectancy in 2010. In fact, US-born New Yorkers have a life expectancy below that of the United States itself.
Rapid gains in life expectancy at birth in New York City (NYC) have been widely broadcast (New York City Department of Health and Mental Hygiene (NYC DHMH) 2011a; Alcorn 2012; Wang et al. 2013). They have been repeatedly cited in press conferences by Mayor Michael Bloomberg and in press releases from his office (e.g., City of New York Office of the Mayor 2011). There is no doubt that these gains are valid and not a product of poor measurement or random error.
The sources of major health accomplishments in such a sizable population deserve careful scrutiny, in part because some of the lessons may be exportable. With 8.3 million people in 2012, New York City is larger than most European countries, including Switzerland, Denmark, Finland, and Norway whose health circumstances are often favorably contrasted to those in the United States (Crimmins, Preston, and Cohen 2011; Woolf and Aron 2013).
In this article, we maintain a comparative perspective but direct attention to domestic rather than international differences. We compare levels and trends in life expectancy among residents of New York City to those in the United States as a whole between 1990 and 2010. The entire US, in effect, operates as a control group enabling us to identify factors that are relatively distinctive in New York City. We identify the causes of death and age/sex groups that are responsible for the rapid gains in life expectancy in New York City relative to the United States. Based on this analysis, we consider the contribution of socioeconomic advances, demographic change, behavioral factors, and health system performance to the rapid relative improvements and favorable current levels of life expectancy in New York City.
Data and Methods
Data on deaths are derived from vital statistics data files produced by the National Center for Health Statistics (NCHS) for years 1989–1990, 1999–2000, and 2008–2010. Data for 2008–10 were obtained under a data user agreement from the NCHS. These data contain information on detailed causes of death, age, sex, place of birth (distinguishing foreign birth and birth in US territories), and county of residence at the time of death.
To estimate death rates, we combined the deaths with the national and county-level mid-year population estimates prepared by the Census Bureau (National Cancer Institute 2013). Death rates by age, sex, and cause of death were produced for the United States and New York City for 1989–1990, 1999–2000, and 2009–2010.1 For simplicity, we refer to these years as 1990, 2000, and 2010, but readers should note that all analyses except those involving nativity are based on two-year averages centered on January 1 of the second of these years. For the calculation of life tables by nativity, we used 1990, 2000, and 2008–2010 data on deaths. Population estimates by nativity were obtained from the 5 percent samples of the 1990 and 2000 US Census of Population and the 2008–2010 American Community Survey using the Integrated Public Use Microdata Series (IPUMS-USA) (Ruggles et al. 2010). Those who were born in the 50 US states, District of Columbia, and the US territories were coded as native-born. Those who were born in foreign countries were coded as foreign-born. Deaths with unknown place of birth were allocated by age and sex based on the distribution of deaths with known place of birth.
We coded underlying causes of death into 16 mutually exclusive and exhaustive categories using the International Classification of Disease (ICD)-9 (1989–1990) and ICD-10 (1999–2000, 2008–2010) (see Appendix Table A.1 for details). We distinguished disease categories with epidemiologic significance, including HIV/AIDS, homicide, lung cancer, and cancers for which screening is common. In addition, we make reference to causes or a group of causes within the broader categories when these causes make up a substantial contribution within the broader category. In 2000 and 2010, we included an additional category, drug- and alcohol-related causes of death, based on a classification developed by the Centers for Disease Control and Prevention (CDC) (Miniño et al. 2011). The mapping of these specific causes to ICD-9 is problematic, and therefore we have limited the analyses of their contribution to the latter decade. Drug- and alcohol-related deaths draw from other categories used in this analysis and should not be treated additively with other causes.
We calculated age-, sex-, and cause-specific death rates for ages 0–1, 1–4, 5–9, and in subsequent five-year age groups up to age 100 with an open-ended age interval beginning at age 100.2 Using these rates, we estimated age-standardized death rates by sex and selected causes of death and for all causes combined for New York City and the United States for 1990, 2000, and 2010 using the total 2000 US population as the standard. The rates employed in this analysis are presented in Appendix Tables A.2a and A.2b. We produced period life tables by sex and nativity for New York City and the United States for each of the three time periods under study using standard life table procedures (Preston, Heuveline, and Guillot 2001). To estimate the contribution of the various causes of death to differences in life expectancy between New York City and the United States at each time period, we used the method developed by Arriaga (1984). The cause-specific contributions to the change in the difference in life expectancy between New York City and the United States over time can then be estimated as the difference between the cause-specific contributions to this difference at time 1 (e.g., 1990) and at time 2 (e.g., 2000).
Results
Over the entire 20-year period 1990–2010, females in New York City gained 6.25 years compared to only 2.39 years for females in the United States (Table 1). Males in New York City had an even larger gain of 10.49 years, compared to 4.49 years in the United States. For both sexes, life expectancy started below the national average in 1990, caught up to the national average in 2000, and exceeded it by 2010. While female gains in New York City were evenly spread across the two decades, male gains were substantially faster during the 1990s. In both decades for both sexes, the pace of improvement of life expectancy in New York City far surpassed the norm of 2.5 years per decade established over more than a century in developed countries (Oeppen and Vaupel 2002).
Table 1. Life expectancy at birth by sex, New York City and United States: 1990, 2000, and 2010.
| 1990 | 2000 | 2010 | Change 1990 to 2000 | Change 2000 to 2010 | Change 1990 to 2010 | |
|---|---|---|---|---|---|---|
|
|
||||||
| Males | ||||||
|
|
||||||
| New York | 67.54 | 74.30 | 78.03 | +6.76 | +3.73 | +10.49 |
| United States | 71.81 | 74.20 | 76.30 | +2.39 | +2.10 | +4.49 |
| NYC – US | -4.27 | +0.10 | +1.73 | +4.37 | +1.63 | +6.00 |
| Females | ||||||
|
|
||||||
| New York | 76.97 | 80.17 | 83.22 | +3.20 | +3.05 | +6.25 |
| United States | 78.77 | 79.55 | 81.16 | +0.78 | +1.61 | +2.39 |
| NYC – US | -1.80 | +0.62 | +2.06 | +2.42 | +1.44 | +3.86 |
SOURCE: Calculations by the authors, based on data pooled over two years: 1989–1990, 1999–2000, and 2009–2010.
For each of the three periods, Table 2 presents the difference in life expectancy at birth between NYC and the United States that is attributable to each of the 16 causes of death. These differences add up to the difference for all causes combined in each year. The table also shows the relative gain in life expectancy in NYC over the entire period that is attributable to each cause of death.
Table 2. A: Cause-specific contributions to differences in life expectancy between New York City and United States and to changes in these differences, males: 1990, 2000, and 2010 (in years).
| Cause of death | 1990a NYC – US |
2000a NYC – US |
2010a NYC – US |
Changeb 1990 to 2000 |
Changeb 2000 to 2010 |
Changeb 1990 to 2010 |
|---|---|---|---|---|---|---|
|
| ||||||
| Males | ||||||
|
|
||||||
| HIV/AIDS | −1.651 | −0.592 | −0.224 | 1.059 | 0.368 | 1.427 |
| Other infectious diseases | −0.332 | −0.039 | 0.048 | 0.293 | 0.087 | 0.380 |
| Lung cancer | 0.177 | 0.283 | 0.243 | 0.106 | −0.040 | 0.066 |
| Breast, colon, prostate, rectal, and anal cancer | −0.023 | −0.033 | −0.051 | −0.010 | −0.018 | −0.028 |
| All other cancers | −0.102 | 0.114 | 0.156 | 0.216 | 0.042 | 0.258 |
| Mental disorders | −0.125 | −0.033 | 0.110 | 0.092 | 0.143 | 0.235 |
| Nervous system and sense organ, incl. Alzheimer's | 0.052 | 0.200 | 0.294 | 0.148 | 0.094 | 0.242 |
| Circulatory diseases | −0.636 | −0.547 | −0.397 | 0.089 | 0.150 | 0.239 |
| Respiratory diseases | −0.165 | 0.246 | 0.226 | 0.411 | −0.020 | 0.391 |
| Diseases of the digestive system | −0.228 | 0.053 | 0.159 | 0.281 | 0.106 | 0.387 |
| Diseases of the genitourinary system | −0.112 | −0.003 | 0.125 | 0.109 | 0.128 | 0.237 |
| Perinatal conditions | −0.216 | −0.035 | 0.025 | 0.181 | 0.060 | 0.241 |
| Homicide | −0.855 | −0.166 | −0.066 | 0.689 | 0.100 | 0.789 |
| Other external causes | 0.481 | 0.621 | 0.862 | 0.140 | 0.241 | 0.381 |
| Symptoms, signs, and ill-defined conditions | −0.496 | −0.037 | 0.118 | 0.459 | 0.155 | 0.614 |
| All other causes | −0.039 | 0.073 | 0.101 | 0.112 | 0.028 | 0.140 |
| Life expectancy at birth | −4.269 | 0.105 | 1.728 | 4.374 | 1.623 | 5.997 |
| Drug- and alcohol-related causes | — | −0.229 | 0.107 | — | 0.336 | — |
| Non–drug- and alcohol-related causes | — | 0.334 | 1.621 | — | 1.287 | — |
|
| ||||||
| aNumbers may not add up because of rounding. Based on pooled data over two years 1989–1990, 1999–2000, and 2009–2010. | ||||||
| bPositive numbers indicate a decline in the cause-specific contribution and negative numbers indicate an increase in the cause-specific contribution to the difference in life expectancy between New York City and United States. | ||||||
| SOURCE: Calculations by the authors. | ||||||
| Table 2B: Cause-Specific Contributions To Differences In Life Expectancy Between New York City And United States And To Changes In These Differences, Females: 1990, 2000, And 2010 (In Years) | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Cause of death | 1990a NYC –US |
2000a NYC – US |
2010a NYC – US |
Changeb 1990 to 2000 |
Changeb 2000 to 2010 |
Changeb 1990 to 2010 |
|
| ||||||
| Females | ||||||
|
|
||||||
| HIV/AIDS | −0.455 | −0.318 | −0.130 | 0.137 | 0.188 | 0.325 |
| Other infectious diseases | −0.166 | 0.012 | 0.089 | 0.178 | 0.077 | 0.255 |
| Lung cancer | 0.117 | 0.193 | 0.232 | 0.076 | 0.039 | 0.115 |
| Breast, colon, prostate, rectal, and anal cancer | −0.083 | −0.046 | 0.003 | 0.037 | 0.049 | 0.086 |
| All other cancers | −0.066 | 0.032 | 0.082 | 0.098 | 0.050 | 0.148 |
| Mental disorders | 0.026 | 0.112 | 0.309 | 0.086 | 0.197 | 0.283 |
| Nervous system and sense organ, incl. Alzheimer's | 0.086 | 0.272 | 0.436 | 0.186 | 0.164 | 0.350 |
| Circulatory diseases | −0.822 | −0.487 | −0.385 | 0.335 | 0.102 | 0.437 |
| Respiratory diseases | −0.110 | 0.235 | 0.342 | 0.345 | 0.107 | 0.452 |
| Diseases of the digestive system | −0.009 | 0.131 | 0.184 | 0.140 | 0.053 | 0.193 |
| Diseases of the genitourinary system | −0.082 | 0.036 | 0.147 | 0.118 | 0.111 | 0.229 |
| Perinatal conditions | −0.200 | −0.046 | 0.002 | 0.154 | 0.048 | 0.202 |
| Homicide | −0.107 | −0.003 | 0.010 | 0.104 | 0.013 | 0.117 |
| Other external causes | 0.216 | 0.319 | 0.468 | 0.103 | 0.149 | 0.252 |
| Symptoms, signs, and ill-defined conditions | −0.186 | 0.046 | 0.134 | 0.232 | 0.088 | 0.320 |
| All other causes | 0.046 | 0.134 | 0.135 | 0.088 | 0.001 | 0.089 |
| Life expectancy at birth | −1.797 | 0.622 | 2.061 | 2.419 | 1.439 | 3.858 |
| Drug- and alcohol-related causes | — | −0.017 | 0.160 | — | 0.177 | — |
| Non–drug- and alcohol-related causes | — | 0.639 | 1.901 | — | 1.262 | — |
Numbers may not add up because of rounding. Based on pooled data over two years 1989–1990, 1999–2000, and 2009–2010.
Positive numbers indicate a decline in the cause-specific contribution and negative numbers indicate an increase in the cause-specific contribution to the difference in life expectancy between New York City and United States.
SOURCE: Calculations by the authors.
In 1990, NYC experienced excess mortality relative to the United States for most causes of death for both sexes. Important exceptions are lung cancer and “other external causes of death,” the major component of which is motor vehicle accidents. By 2010, NYC had lower mortality than the US in 12 out of 16 cause-of-death categories for males and 14 out of 16 for females. Mortality from HIV/AIDS remained higher in NYC than the national average, as did mortality from circulatory diseases. However, the latter result may reflect differences in diagnostic and coding practices rather than real differences. An experimental intervention in eight NYC hospitals with very high death rates from “heart disease” in 2009–11 revealed that heart disease had been overrecorded on death certificates by a factor of approximately two before the intervention (Al-Samarrrai et al. 2013). Many of the re-coded deaths were assigned to categories other than those included among circulatory diseases.
As shown in the last column of Table 2, death rates for each of the 16 causes of death declined faster in New York City than in the country as a whole over the past two decades.3 The two largest contributors to the relative increase in life expectancy in NYC over the entire period 1990 to 2010 both belonged to males. HIV/AIDS was responsible for 1.43 years of the 6.00 years of life expectancy that NYC males gained on US males, or 23.8 percent. Another 0.79 years or 13.2 percent was contributed by a rapid decline in homicide among NYC males. The large majority of gains in both cases occurred in the decade of the 1990s. HIV/AIDS and homicide made much smaller contributions to changes in the NYC–US difference in female life expectancy over this period, totaling 0.44 years or 11.5 percent. Thus, these two causes of death, which are considered in more detail below, are the main reason why males in NYC made faster strides than females. Without the contribution of HIV/AIDS and homicide, the NYC gains relative to the US would have been similar at 3.77 years for males and 3.41 years for females.
It is likely that HIV/AIDS made an even larger contribution to life expectancy gains in New York City than is indicated by this calculation. Deaths from this cause were likely to be seriously underestimated in New York City in 1989–1990. A 1988 report quotes city health officials as suggesting that at least half of HIV/AIDS deaths among drug abusers were missing from official reports (Fackelmann 1988). In a cohort study of intravenous drug users in NYC during 1982–86, more than 90 percent of deaths that should have been assigned to HIV/AIDS were not properly coded but rather assigned to such illnesses as tuberculosis, heart valve infection, or pneumonia (ibid.) A rapid rise in national deaths assigned to pneumonia during the 1980s has been attributed to the HIV/AIDS epidemic (McGinnis and Foege 1993).
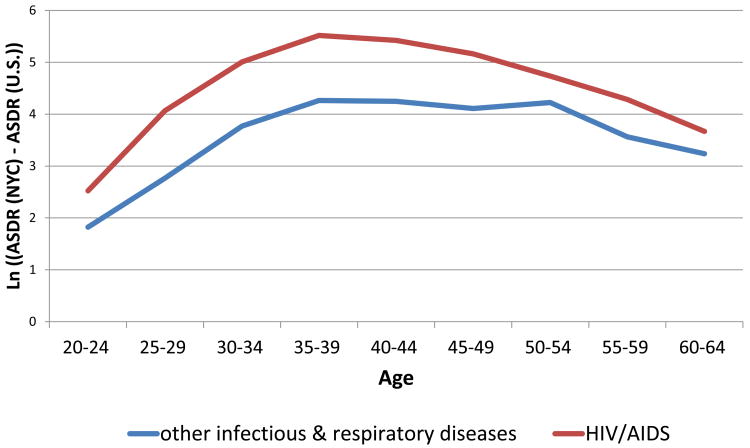
Figure 1 provides additional evidence that HIV/AIDS deaths were seriously underreported in NYC in 1990. It graphs, on a log scale, the difference in age-specific death rates per 100,000 from HIV/AIDS between NYC and the US for males in 1990 as a function of age. The difference mimics the unusual age pattern of mortality from this cause. The figure also presents the difference between NYC and US death rates from other infectious diseases and respiratory diseases combined. The typical age-pattern of mortality from these causes is U-shaped (Preston 1976), but in this case the pattern is an inverted U, similar in shape to the HIV/AIDS graph. The implication is that the HIV/AIDS epidemic has raised death rates from other infectious diseases, causing the full impact of HIV/AIDS itself to be understated when attention is confined to deaths in that category alone.
Figure 1. Differences in age specific death rates between New York City and the United States - HIV/AIDS and other infectious and respiratory diseases, Males 1990.
After the large declines in HIV/AIDS and homicide mortality during the 1990s, reductions from these causes were more modest during 2000–2010. Nevertheless, among males, HIV/AIDS remained the largest contributor to NYC's relative gains in life expectancy. The second and third largest contributors were “drug- and alcohol-related causes” and “other external causes,” among which motor vehicle accidents play the leading role. Among females, gains were widely distributed across causes of death. Two of the three leading contributors were the same as among men: HIV/AIDS and drug- and alcohol-related causes. The leading cause contributing to NYC's relative improvement during the 2000s among females was mental disorders, among which unspecified dementia is by far the leading component. It is not clear why NYC would have gained relative to the US in this category. Diagnostic and coding confusion with Alzheimer's disease may create spurious trends, but the category of “diseases of the nervous system and sense organs” was the fourth leading contributor to NYC's advance. Alzheimer's disease accounts for a slight majority of deaths in this category.
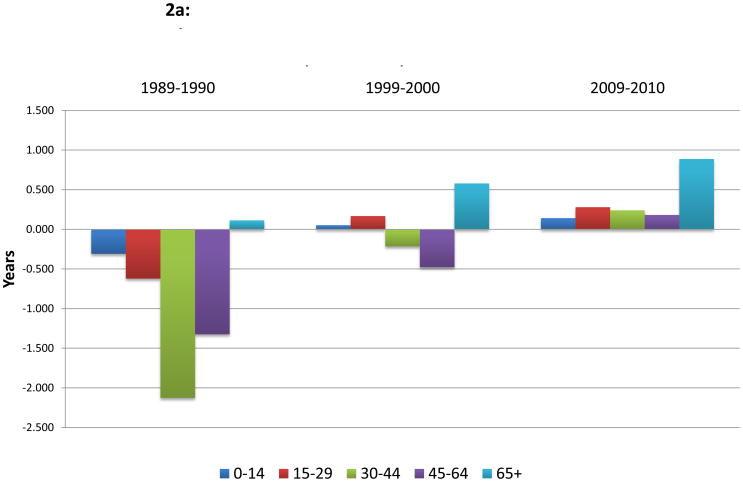
The pervasiveness of relative mortality improvements in NYC is also demonstrated by the age pattern of improvements. Figures 2a and 2b show the ages responsible for the difference in life expectancy at birth between NYC and the US in the three periods we consider. In 1990, ages 15–44 account for 64 percent of the male deficit in NYC (Figure 2a). This age pattern echoes the high death rates in NYC from HIV/AIDS and homicide and again suggests that the impact of HIV/AIDS may be underestimated by deaths in that category alone. The 2.75 “years lost” in this age interval in 1990 declined to 0.47 years by 2000, so that this age interval accounts for 62 percent of the gain in life expectancy for males during the 1990s. By 2010, all ages contribute to NYC's longevity advantage for males, with the largest contribution occurring at ages 65+.
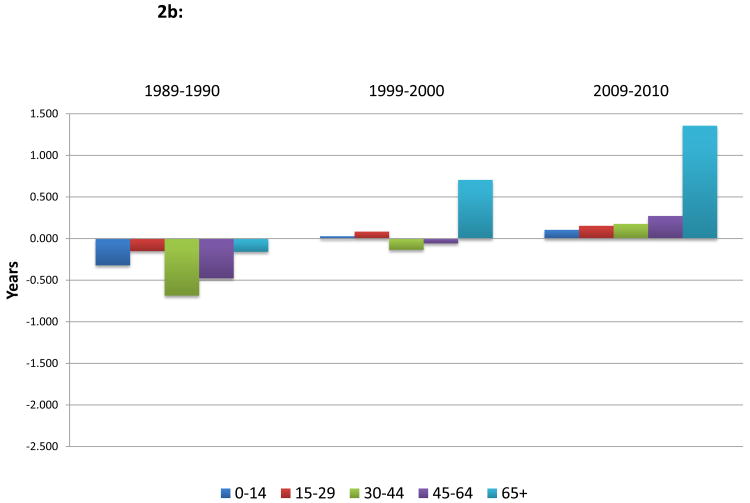
Figure 2.
a: Age group contributions to the difference in male life expectancy at birth in years, New York City - United States, 1989-90, 1999-2000, 2008-2010
b: Age group contributions to the difference in female life expectancy at birth in years, New York City - United States, 1989-90, 1999-2000, 2008-2010
Among females, Figure 2b shows that all age groups contributed to NYC's life expectancy disadvantage in 1990, and all ages contributed to its advantage by 2010. Once again, the basic story is the pervasiveness of improvements in NYC. Among females, the NYC advantage by 2010 is heavily concentrated at ages 65+. This age group contributes 66 percent of the female advantage in NYC at the end of the period.
The extensive scope of causes of death operating to create the NYC longevity advantage, and the broad range of ages involved, point to the possibility that broad systemic factors are at work. Before considering what they might be, we treat in more detail the two sources of exceptionally fast mortality declines among males in NYC: HIV/AIDS and homicide.
HIV/AIDS
New York City began the period with a much higher age-standardized death rate from HIV/AIDS than the US: 98.1 per 100,000 vs. 17.5 per 100,000 for males in 1990 and 17.7 vs. 2.0 for females (Appendix Tables A.2a and A.2b). Because NYC's baseline rate is so much higher, an equi-proportional decline in mortality in the US and NYC would be expected to have a bigger effect on life expectancy in NYC. However, NYC's success was not simply a matter of drawing equally from the improvements in prevention and treatment that became available during this period. For males, the HIV/AIDS death rate in NYC fell by 85 percent between 1990 and 2010, while falling by 77 percent in the US. For females, death rates fell by 73 percent in NYC but by only by 22 percent in the US.
The very large decline in HIV/AIDS mortality in NYC appears to be primarily attributable to aggressive identification of infected individuals and their treatment with antiretroviral therapy (ART), combined with an ambitious syringe exchange program aimed at injecting drug users (Chiasson et al. 1999; Marshall et al. 2012; Des Jarlais et al. 2005). Seventy-four percent of the relative decline in HIV/AIDS mortality for males occurred in the 1990s, during which ART was undoubtedly more consequential for mortality than needle exchanges, which initially affected only disease incidence. However, the annual number of syringes exchanged grew rapidly from 250,000 in 1991 to 3,000,000 in 2000. The incidence of HIV among injecting drug users declined precipitously during this period (Des Jarlais et al. 2005). Prevalence rose among those who acquired HIV through other routes, but mortality declined rapidly among both injecting drug users and others. The growth of programs providing opiate addicts with substitute drugs taken orally has played a complementary role (Cohen 2012). That disease identification is unusually effective in NYC is indicated by the below-average prevalence of undiagnosed HIV/AIDS (Trang et al. 2008).
Thus, the exceptionally large decline in HIV/AIDS mortality in NYC appears to result from aggressive and effective public health efforts to address a problem that was unusually severe in NYC.
Homicide
The age-standardized death rate from homicide for males declined by 77 percent in NYC between 1990 and 2010. Nearly all of this decline occurred during the 1990s. Meanwhile, the US male death rate from homicide declined by only 40 percent over the two decades. While NYC's male death rate from homicide was 3.2 times that of the US in the earlier period, it was only 1.2 times higher by the end of the period. Homicide death rates for women were 76 percent higher than US rates at the start of the period but were actually 15 percent lower by the end (Appendix Tables A.2a and A.2b).
The very large decline in homicide mortality in NYC was part of a comparable decline in many other crime rates during the period, including rape, assault, robbery, burglary, and auto theft. In a well-documented monograph, Zimring (2012) has considered the sources of the large reductions in crime rates. His conclusion is that changes in the size, organization, and tactics of the New York Police Department were principally responsible. Successful police tactics included suppressing public open-air drug markets, redeploying police to “hot spots” where crime frequency was greatest, and more aggressive searching and arresting, especially for minor offenses. His conclusion is based on detailed time-series analysis of programs and outcomes, comparisons with other cities, and process-of-elimination reasoning. As in the case of HIV/AIDS, municipal governance appears to have played the key role in the decline of homicide mortality.
We now consider other factors that may have contributed to the rapid improvement in New York City's longevity.
Economic and social factors
It is widely recognized that higher levels of education and income are associated with superior health and longevity (Smith 2007; Elo 2009). Such relations have also been observed within New York City (NYC DHMH 2010a). So a rapid upgrading of the social and economic circumstances of NYC's population relative to that of the US could potentially account for its rapid improvement in longevity.
Table 3 presents trends in two indicators of economic performance and two indicators of educational attainment. Over the 1990–2000 period, relative to the US New York City had rising poverty, declining household income, and less rapid upgrading of its educational distribution. Thus, it is unlikely that relative social and economic improvements in NYC were responsible for the rapid health improvements during this period. And this is the decade in which NYC's relative gains were by far the largest (Table 1).
Table 3. Indicators of economic and educational performance, New York City and United States: 1990 to 2010.
| 1990 | 2000 | 2008–2010 | |
|---|---|---|---|
|
|
|||
| Percent of population in poverty | |||
|
|
|||
| New York City | 19.3 | 21.2 | 19.4 |
| United States | 13.1 | 12.4 | 14.4 |
| Ratio, NYC/US | 1.47 | 1.71 | 1.34 |
| Median annual household income ($) | |||
|
|
|||
| New York City | 29,810 | 38, 394 | 50,044 |
| United States | 30,056 | 41,994 | 51,222 |
| Ratio, NYC/US | 0.99 | 0.91 | 0.98 |
| Percent aged 25+ who did not graduate from high school | |||
|
|
|||
| New York City | 31.7 | 27.7 | 21.0 |
| United States | 24.8 | 19.6 | 14.7 |
| Ratio, NYC/US | 1.27 | 1.41 | 1.43 |
| Percent aged 25+ who graduated from college | |||
|
|
|||
| New York City | 23.0 | 27.4 | 33.4 |
| United States | 20.3 | 24.4 | 28.0 |
| Ratio, NYC/US | 1.13 | 1.12 | 1.19 |
SOURCE: United States Census of Population 1990 and 2000, American Community Survey 2008–2010. Tabulations from Social Explorer, http://www.socialexplorer.com/ July 25, 2013.
These indicators improved faster in NYC than in the US during 2000 to 2008–10, so they may have contributed to NYC's relative advance during this period. On the other hand, NYC finished the two decades in much the same position it began. Median household income relative to the US changed by only 1 percent over the period; the relative proportion of high school dropouts increased in NYC, but so did the proportion of college graduates. Poverty levels increased modestly over the period in both NYC and the US, but the increase was somewhat greater in the US.
Averages can be misleading in such comparisons. Even with the same average level of income or educational attainment, greater disparities could produce worse aggregate outcomes because of non-linearities in the relation between causal factors and health outcomes (Preston 1980). But as Table 3 shows, disparities in educational outcomes actually grew over the period in NYC relative to the US; relative increases in proportions occurred at both ends of the educational distribution in NYC. As for income, Zimring (2012) found that per capita income grew sharply over the 1989–2007 period in Manhattan but fell in Bronx and Queens, suggesting an exacerbation rather than a reduction of spatial income inequalities in NYC. Income at the 20th percentile and 50th percentile in NYC grew by an identical factor over the same period (ibid.). Thus, there is no evidence that relative improvements in the level or distribution of either income or educational attainment in NYC are responsible for its rapid relative gains in life expectancy.
Were mortality trends during the period highly differentiated by economic status within NYC? The evidence is mixed but suggests that trends were relatively homogeneous. Over the period 1990–2010, and in both sub-decades, Manhattan had the fastest decline in the age-standardized death rate for both sexes (51 percent for males and 40 percent for females; Appendix Table A.3). The main reason was that it began the period with by far the highest death rate from HIV/AIDS (calculations not shown). The poorest borough, Bronx, had a mortality reduction that was very similar to that for the city as a whole (42 percent vs. 44 percent for males and 35 percent vs. 37 percent for females). Between 2001 and 2010, New Yorkers living in low-poverty neighborhoods gained 2.5 years of life expectancy while those in high-poverty areas gained 3.7 years. Non-Hispanic whites gained 2.2 years over this period while non-Hispanic blacks gained 3.8 years and Hispanics, 3.2 years (NYC DHMH 2013). The faster gains in life expectancy among non-Hispanic blacks and Hispanics may be related to the rapid growth in the foreign-born population among them. Foreign-born blacks have substantially lower mortality than US-born blacks (Singh and Siahpush 2002; Dupre, Gu, and Vaupel 2012). In 2010, 32.6 percent of blacks in NYC were foreign-born, up from 24.3 percent in 1990. The respective figures for the US were 8.3 percent and 4.6 percent (authors' calculations using IPUMS data described above).
Racial/ethnic/nativity composition
The demographic composition of NYC's population is unique within the United States. Only 26.0 percent of its population in 2008–10 consisted of native-born, non-Hispanic whites, compared to 62.2 percent of the US population as a whole. Most of the remaining groups—Hispanics, Asian and Pacific Islanders, as well as the foreign-born—have mortality levels below those of non-Hispanic whites (Anderson, Bulatao, and Cohen 2004). African Americans are the main exception to the pattern of lower mortality for minorities.
Table 4 shows the racial/ethnic composition of NYC and of the US in the period under study. Throughout the period, NYC had a much higher proportion of Hispanics, Asian/Pacific Islanders, and immigrants, groups with superior longevity. As the largest “minority” group in NYC, immigrants warrant special attention. In Table 5, we present life expectancy estimates for foreign-born and native-born populations in both NYC and the US during the period under consideration.
Table 4. Racial/ethnic/nativity composition of the population and percent foreign-born, New York City and United States: 1990 to 2010 (percent).
| 1990 | 2000 | 2008–2010 | |
|---|---|---|---|
|
|
|||
| Race/ethnicitya | New York City | ||
| White | 43.5 | 36.3 | 34.1 |
| Black | 25.6 | 25.5 | 23.6 |
| Asian/Pacific Islander | 6.8 | 10.3 | 12.9 |
| Am. Indian/Alaskan Native/Other | 0.4 | 1.0 | 1.0 |
| Hispanic | 23.7 | 26.9 | 28.4 |
| Foreign-born | 29.3 | 36.6 | 37.8 |
| Race/ethnicitya | United States | ||
|
| |||
| White | 75.8 | 70.2 | 65.2 |
| Black | 11.8 | 12.5 | 12.9 |
| Asian/Pacific Islander | 2.8 | 3.9 | 5.0 |
| Am. Indian/Alaskan Native/Other | 0.9 | 1.0 | 0.9 |
| Hispanic | 8.8 | 12.5 | 16.1 |
| Foreign-born | 8.7 | 11.8 | 13.6 |
Mutually exclusive categories with all Hispanics included under Hispanic; other groups refer to non-Hispanic individuals using a “bridged” race variable, which assigns single race to multiple-race individuals in an attempt to provide consistent data series over time (https://usa.ipums.org/usa-action/variables/RACESING#description_section).
SOURCE: 1990 and 2000 Census of Population 5% Integrated Public Use Microdata Series (IPUMS), and 2008–2010 American Community Survey, downloaded from the Integrated Public Use Microdata Series (IPUMS-USA) (Ruggles et al. 2010).
Table 5. Life expectancy at birth, New York City and United States by sex and nativity: 1990, 2000, 2008–10.
| 1990 | 2000 | 2008– 2010 | Change 1990 to 2000 | Change 2000 to 2010 | Change 1990 to 2010 | |
|---|---|---|---|---|---|---|
|
|
||||||
| Males | ||||||
|
|
||||||
| New York | ||||||
| US-born | 64.97 | 71.92 | 75.28 | 6.95 | 3.36 | 10.31 |
| Foreign-born | 73.83 | 78.53 | 81.06 | 4.70 | 2.53 | 7.23 |
| United States | ||||||
| US-born | 71.33 | 73.71 | 75.38 | 2.38 | 1.67 | 4.05 |
| Foreign-born | 75.95 | 78.49 | 81.18 | 2.54 | 2.69 | 5.23 |
| Females | ||||||
|
|
||||||
| New York | ||||||
| US-born | 75.39 | 78.58 | 80.61 | 3.19 | 2.03 | 5.22 |
| Foreign-born | 81.03 | 83.59 | 85.72 | 2.57 | 2.13 | 4.70 |
| United States | ||||||
| US-born | 78.33 | 79.08 | 80.29 | 0.75 | 1.21 | 1.96 |
| Foreign-born | 81.85 | 82.88 | 85.07 | 1.04 | 2.19 | 3.23 |
SOURCE: Calculations by the authors.
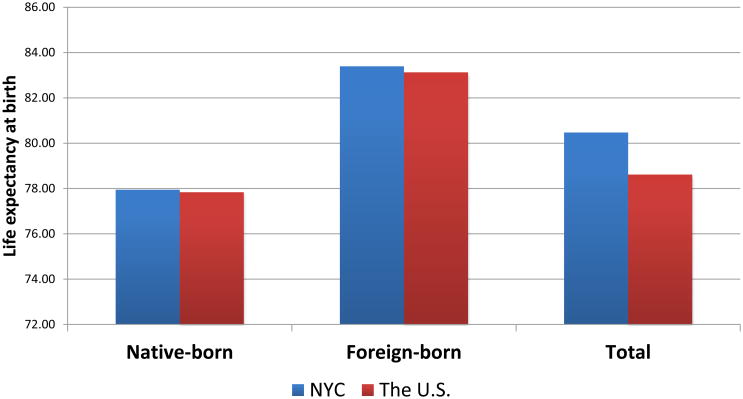
The results are remarkable. In 2008–10, US-born people in NYC and the US had virtually identical life expectancies: 75.3 vs. 75.4 years for males and 80.6 vs. 80.3 for females. Foreign-born persons in the two populations also had very similar life expectancies: 81.1 vs. 81.2 for males and 85.7 vs. 85.1 for females.4 In other words, virtually all of NYC's longevity advantage in the most recent period is a result of its very high proportion of immigrants. This conclusion is strikingly illustrated in Figure 3, which presents life expectancy (mean, males and females) by nativity for the US and the NYC population in 2008–2010.
Figure 3. Life expectancy at birth by nativity, New York City and the United States, 2008-2010.
Such a result is possible because the foreign-born proportions differ sharply between NYC (37.8 percent) and the US (13.6 percent) and because life expectancy differs dramatically between the foreign-born and the native-born in NYC (by 5.8 years for males and 5.1 years for females). The composition of the population becomes even more significant at ages 65+, where most of the recent (i.e., 2009–2010; see Figure 2) longevity advantage of NYC is concentrated. Forty-five percent of NYC's population at ages 65+ was foreign-born in 2008–10, compared to only 12.4 percent of the US population. These values have risen from 32.4 percent and 8.9 percent in 1990. Since 82 percent of newborn males and 90 percent of newborn females in 2010 survive to age 65 in the NYC life tables summarized in Table 1 (and 81 percent and 88 percent, respectively, in the US life tables), what happens at ages 65+ plays a central role in life expectancy outcomes.
Explanations of why the foreign-born in the United States have such low mortality have focused on migrant selectivity (“healthy migrant” effects) and better health habits (Jasso et al. 2004; Fenelon 2013). According to a comprehensive study of immigrant health in NYC (NYC DHMH 2006), the foreign-born in NYC have poorer health insurance coverage than the native-born, poorer access to Medicaid among those in poverty, and a lower frequency of cancer screening and of immunization. They are, however, less likely to smoke (13 percent prevalence vs. 23 percent), to be obese (16 percent vs. 21 percent), and to engage in binge drinking (12 percent vs. 16 percent). The incidence of HIV/AIDS is 61 percent lower than among US-born New Yorkers.
Table 6 shows that, in New York City during 2008–10, the foreign-born have lower age-adjusted death rates than the native-born for every cause of death that we are considering. This difference is maintained for each sex and for both sexes combined. The causes of death showing the greatest mortality advantage for the foreign-born are HIV/AIDS (83 percent reduction) and drug- and alcohol-related deaths (71 percent reduction). Homicide and lung cancer death rates are 47–48 percent lower among the foreign-born. Clearly, causes of death with a strong behavioral component play a major role in the low mortality of foreign-born New Yorkers.
Table 6. Age-standardized death rates by cause of death and nativity: New York City 2008–2010a.
| Cause of Death | Native-born | Foreign-born | Ratio Foreign-born to Native-born |
|---|---|---|---|
| HIV/AIDS | 19.56 | 3.40 | 0.174 |
| Drug- and alcohol-relatedb | 26.28 | 7.63 | 0.290 |
| Mental disorders | 16.30 | 8.52 | 0.523 |
| Homicide | 7.82 | 4.11 | 0.525 |
| Lung cancer | 46.02 | 24.21 | 0.526 |
| Other infectious diseases | 16.59 | 9.30 | 0.560 |
| Other external causes | 34.12 | 19.55 | 0.573 |
| Diseases of the digestive system | 22.10 | 13.09 | 0.592 |
| Respiratory diseases | 65.91 | 42.88 | 0.651 |
| All other causes | 40.39 | 26.88 | 0.666 |
| Diseases of the genitourinary system | 12.20 | 8.38 | 0.687 |
| Nervous system and sense organ, incl. Alzheimer | 14.99 | 10.34 | 0.690 |
| Circulatory diseases | 322.76 | 230.23 | 0.713 |
| Symptoms, signs, and ill-defined conditions | 5.42 | 4.01 | 0.739 |
| Breast, colon, prostate, rectal, and anal cancer | 45.22 | 34.11 | 0.754 |
| All other cancers | 94.87 | 73.17 | 0.771 |
| All causes | 768.33 | 512.62 | 0.667 |
Mean, male and female age-standardized death rate per 100,000.
Combination of causes appearing elsewhere in the table.
One potential contributor to a mortality advantage of the foreign-born may be return migration of individuals when they become sick, the so-called salmon bias. An investigation using longitudinal data from the Social Security Administration concluded that this factor is too weak to explain a significant part of the Hispanic mortality advantage in the US (Turra and Elo 2008). Even if it were a more important factor in NYC than in the country as a whole, the implication would still be that NYC's life expectancy was raised by the heavy representation of immigrants but that some portion of the increase would be spurious rather than real. In contrast, return migration of native-born New Yorkers who have moved to other parts of the US and who return to NYC when they become sick would have the opposite effect by reducing life expectancy in NYC among the native-born.
How much do changes in the nativity composition of NYC's population contribute to its relative improvement in longevity? To answer this question, we have held constant the nativity composition of the population in each age/sex category at its value in 1990. If the nativity composition of the population had not changed since 1990, NYC males and females would have had a life expectancy in 2010 that is 0.7 years lower than its actual life expectancy. The United States would have had a life expectancy that is 0.2 years lower than the actual. So changes in the nativity composition of the population contributed about 0.5 years to the faster gain in life expectancy in NYC. This factor represents 8 percent of the actual gain among males and 13 percent of the actual gain among females. The remainder of NYC gains over the two decades occurred primarily within the native-born category, where NYC males gained 6.3 years on US males and NYC females gained 3.3 years (Table 5). Life expectancy advances among the native-born were greater than among the foreign-born in NYC, whereas the opposite was true in the US as a whole. Nevertheless, among both native-born and foreign-born New Yorkers, the gains in life expectancy surpassed those of the US as a whole.
Although the contribution of changes in the nativity composition to the relative trends in life expectancy is modest, it is clear that the high proportion foreign-born is contributing the bulk of the current longevity advantage of NYC. In fact, the life expectancy of New Yorkers born in the United States is actually below that of the United States itself (compare Tables 1 and 5).
Behavioral factors
A. Smoking
In 2000, cigarette smoking was responsible for about 18 percent of deaths in the United States, making it the leading behavioral risk factor (Mokdad et al. 2004). Smoking is on the decline both nationally and in NYC, with a faster recent decline in the latter. In 2002, 22.3 percent of US adults were current smokers, compared to 21.5 percent of NYC residents. In 2010, the prevalence of smoking had declined to 19.3 percent in the US and to 14.0 percent in NYC (NYC DHMH 2011b). The NYC decline is rapid enough, and the consequences of smoking serious enough, to contribute substantially to a NYC longevity advantage. The question is how rapidly the reductions in smoking manifest themselves in life expectancy. Lags in the relation between smoking and mortality are relatively long. Furthermore, smoking histories (not simply current prevalence) have also been improving rapidly in the US (Preston and Wang 2006).
NYC's Department of Health and Mental Hygiene (2008, 2011a) has made annual estimates of the number of deaths attributable to smoking in NYC over this period. The age-adjusted rate of deaths attributable to smoking declined from 2.17 per thousand in 2002 to 1.63 per thousand in 2010, or by 24.7 percent. The method used in this calculation recognizes current smokers and former smokers, but not the duration of time since smoking ceased among ex-smokers. Because smoking declined so rapidly over the period, many ex-smokers in NYC would have been recent quitters and would have higher mortality than those who quit during earlier years (Jha et al. 2013). In one large study, those who had quit smoking in the previous five years had a 13 percent lower death rate than current smokers, whereas all former smokers as a group had a 50 percent lower death rate (Kenfield et al. 2008). Assigning to recent quitters the average relative risk for former smokers will overestimate the changes in smoking-attributable mortality during a period of unusually rapid smoking cessation.
Other population-level approaches to assessing deaths attributable to smoking use lung cancer as the basic indicator of the damage from smoking (Peto et al. 1992; Preston, Glei, and Wilmoth 2011). Lung cancer is the clearest marker of such damage because smoking is the overwhelming risk factor in death from lung cancer. Ninety percent of male and 84–85 percent of female lung cancer deaths in the US are attributable to smoking (Oza et al. 2011). Over the period 2000– 2010, the age-standardized death rate from lung cancer in NYC declined by 17.9 percent (Appendix Tables A.2a and A.2b). We believe that this is a better indication of the rate of decline in smoking-attributable mortality than that produced by the NYC Department of Health and Mental Hygiene. And it is similar to the decline in lung cancer mortality in the US over this decade, 15.6 percent.
It is possible that the impact of smoking reduction is registered more slowly for lung cancer mortality than for mortality from other causes. Oza et al. (2011) directly examined the time-patterns of relative mortality risks of smokers from various causes of death. Relative to the lag between smoking behavior and death for lung cancer, they found the lag structure to be longer for chronic obstructive pulmonary disease (COPD) and shorter for cardiovascular diseases. They estimated that the number of deaths attributable to smoking differed by only 1.7 percent when cause-specific lag structures were incorporated compared to when lung cancer was used as the only indicator. Thus, it appears that the pattern of lung cancer lags is sufficiently similar to that for the aggregate of other causes of death that serious distortions do not arise from assuming that they are the same.
Table 2 shows how much lung cancer mortality contributed to changes in the life expectancy gap between NYC and the US over the two decades under study. During the 2000 to 2010 decade, lung cancer mortality fell about as rapidly in the US as it did in NYC. Females in NYC gained a modest 0.04 years relative to the US while NYC males actually lost 0.04 years. These values would suggest that smoking differences played a negligible role in widening NYC's longevity advantage during the 2000s. This is despite the fact that in the 2000s, New York City and New York State took many initiatives to combat smoking: an increase in the city's cigarette tax from $0.08 to $1.50 per pack in 2002, which now combines with a state tax of $4.35/pack implemented in 2010 to give the highest tax in the country (www.tobaccofreekids.org); a Smoke-Free Air Act that prohibited smoking in virtually all indoor workplaces, including restaurants and bars; a mass media campaign emphasizing the health risks of smoking; expansion of smoking-cessation clinics in public hospitals; and widespread distribution of nicotine patches and gum to adult smokers (Frieden et al. 2008).
Relative improvements in lung cancer mortality were actually more favorable for NYC during the 1990s. Females in NYC gained 0.08 more years of life expectancy than females in the US, and NYC males gained 0.11 more years (Table 2). Because lung cancer deaths represent only about a quarter to a third of deaths attributable to smoking (Preston, Glei, and Wilmoth 2011), these changes suggest that relative improvements in smoking may account for 0.24 to 0.44 years of NYC's relative life expectancy gains during the 1990s. The relative growth of the foreign-born population during this period undoubtedly contributed to the improvement in smoking-related mortality since the prevalence of smoking among the foreign-born in NYC is only 57 percent of that of the native-born (NYC DHMH 2006).
B. Obesity and physical activity
Obesity accounts for approximately 15 percent of deaths in the US, second only to smoking among behavioral risk factors (Mokdad et al. 2005). Comparable self-reported data on height and weight are available from the Behavioral Risk Factor Surveillance System and its NYC counterpart, the Community Health Survey. Because the latter source does not begin until 2002, longer-term trends in obesity cannot be established in NYC.
Table 7 shows that New Yorkers had a lower prevalence of obesity than the US in both 2002 and 2008, with a similar gap of about 4–5 percentage points in the two years. The degree of excess mortality associated with obesity is a controversial subject (Flegal et al. 2013; Whitlock et al. 2009). Assuming a 40 percent excess risk of death among the obese, which is on the high side of current estimates, a 5 percent gap in obesity prevalence would account for about a 1.5 percent advantage in death rates for NYC. So this difference is responsible for little of NYC's superior longevity. Further evidence that obesity plays a negligible role in NYC's longevity advantage is that the 2007 prevalence of diabetes, one of the main health hazards associated with obesity, is higher in NYC than in the US (9.1 percent among adults vs. 7.5 percent) (NYC DHMH 2009a). The age-standardized death rate from diabetes in 2010 was 3 percent higher in NYC than in the US among females and 6 percent lower among males. Death rates from diabetes fell slightly faster in the US than in NYC between 2000 and 2010 (Appendix Tables A.2a and A.2b).
Table 7. Health behaviors, New York City and United States, 2002 and 2008a.
| 2002 | 2008 | |||
|---|---|---|---|---|
|
|
||||
| New York City % | United States median % | New York City % | United States median % | |
| Risk factor | ||||
| Current smoker | 21.8 | 23.2 | 16.0 | 18.4 |
| Obese (BMI ≥ 30) | 18.0 | 21.9 | 22.1 | 26.7 |
| Heavy drinker | 4.9 | 5.9 | 4.3 | 5.1 |
| Cancer screening | ||||
| Mammogram in the past 2 years, women 40+ | 77.4 | 76.1 | 77.3 | 76.0 |
| Pap smear in the past 3 years | 80.1 | 87.2 | 82.9 | 82.9 |
| Ever had sigmoidoscopy or colonoscopy, adults 50+ | 49.4 | 48.6 | 68.2 | 62.2 |
| Vaccinations | ||||
| Flu shot in the past year, adults 65+ | 63.0 | 68.6 | 56.6 | 71.1 |
| Ever had pneumonia vaccination, adults 65+ | 50.2 | 63.0 | 49.7 | 66.9 |
Data pertain to adults 18 years and over unless otherwise noted. Percentages are weighted.
SOURCE: New York City: Community Health Survey, Public Use Files, 2002 and 2008, excluding cases with missing information on age or variable of interest (http://www.nyc.gov/html/doh/html/data/survey.shtml). United States: States and District of Columbia, Centers for Disease Control and Prevention, Behavioral Risk Factor Surveillance System, http://apps.nccd.cdc.gov/brfss/. Accessed August 24, 2013.
High levels of physical activity among New Yorkers may contribute more to their longevity advantage. Mass transit use is much more frequent in NYC than elsewhere: a striking 38 percent of all transit trips nationally in 2000 were made in the greater New York City area (Taylor et al. 2008). According to a 2010 survey, New Yorkers who take public transportation for most of their commute get almost 30 minutes more daily physical activity (walking plus recreation) than those who use a car or taxi (NYC DHMH 2011c).
Unfortunately, translating a physical activity advantage into its implications for longevity is not feasible. The necessary large-scale randomized control trials have not been conducted, and observational data are fraught with reverse causal pathways because sick and disabled people are often unable to exercise (Steptoe and Wikman 2010). That physical activity levels may not be an important part of the NYC advantage is suggested by the fact that people aged 65+ in NYC are more likely to report no physical activity than their US counterparts (30 percent vs. 23 percent) (NYC DHMH 2010a). This age range is responsible for the bulk of NYC's longevity advantage in 2010.
C. Drug and alcohol abuse
Table 7 shows that New Yorkers are slightly less likely to be “heavy drinkers”5 than other Americans. This tendency is confirmed by the 2008 National Survey on Drug Use and Health, which shows NYC to have a lower prevalence of both heavy drinking and binge drinking at ages 12–20 and ages 21+ (NYC DHMH 2010b). However, differences are very small.
The same survey found that New Yorkers were slightly more likely than other Americans to have used illicit drugs or medications in a manner other than prescribed. Again, the differences were small: 16 percent reported use in the past year in NYC vs. 14 percent in the US. Marijuana was by far the most frequently reported substance. Heroin and cocaine use was more frequent in NYC, while abuse of pain relievers was more frequent in the US (NYC DHMH 2010c). On the other hand, a 2005 survey found that young people in NYC were less likely to have ever used marijuana, cocaine, inhalants, or methamphetamines than youth in the US (NYC DHMH 2007).
Identifying the contribution of drug and alcohol abuse to longevity differences is facilitated by a cause-of-death grouping instituted by the National Center for Health Statistics when it introduced the 10th revision of the International Statistical Classification of Diseases and Related Health Problems. The category of “drug- and alcohol-related deaths” consists primarily of causes related to mental disorders, poisoning, and liver diseases attributable to alcohol and drug use. Nationally, in 2000 about half of the causes in this category were related to alcohol use and the other half to drug use.
Table 2 shows that males in NYC lost 0.23 years of life expectancy relative to the US in 2000 from drug- and alcohol-related causes, but by 2010 the pattern had reversed: males in NYC lived 0.11 years longer than males in the US by virtue of their lower drug- and alcohol-related mortality. This turnaround of 0.34 years accounted for 21 percent of NYC's relative improvement of 1.62 years in life expectancy during this period. Male age-standardized death rates from these causes in NYC fell from 0.32/1000 to 0.25/1000 over the period, while US rates rose from 0.21/1000 to 0.27/1000 (Appendix Table A.2a). So the relative gains in NYC reflect both its own successes and US failures. A comparable turnaround among females accounted for 12 percent of NYC's relative gains in female life expectancy between 2000 and 2010. Thus, NYC's superior performance on drug- and alcohol-related deaths is responsible for a substantial fraction of relative gains in life expectancy over this period.
Trends in the number of deaths from “unintentional drug overdose” in NYC were flat during the 2000s until 2007, when they declined sharply and continued declining in 2008 (NYC DHMH 2010c). It is possible that this decline was associated with initiatives of the Department of Health and Mental Hygiene in 2007/08 to promote the use of buprenorphine and to accelerate the adoption of sterile syringes (NYC DHMH 2009b).
Quality and availability of medical services
As a center of medical training and research and an attractive residence for many professionals, New York City may provide more and better care to its residents than is typical in the United States. There are several useful quality indicators for recent years, but almost no data on trends. One trend indicator is the death rate from cancers for which screening is common and early detection can help prevent death. Death rates from breast, colon, anal, and prostate cancers declined sharply between 1990 and 2010 in both NYC and the US. The rates of decline were similar. Table 2 shows that, over the entire 1990–2010 period, females in NYC gained 0.09 years in longevity relative to the US from this source and males in NYC lost 0.03 years. Table 7 shows that the reported frequency of screening in 2002 and 2008 is slightly higher in NYC than in the US for breast cancer and colon cancer and lower for cervical cancer.
Table 7 presents data on vaccination against influenza and pneumonia. New York City residents aged 65+ were considerably less likely to receive either vaccination in 2002 and 2008. Data on Medicare recipients available from the Dartmouth Atlas Project indicate that Medicare Part B recipients aged 65–69 in NYC were significantly less likely to visit a primary care clinician than Part B recipients in the United States in 2010.6 Medicare patients with Part A and Part B coverage discharged from a hospital in NYC were more likely than US residents to be readmitted within 30 days after surgery or after diagnosis of pneumonia, acute myocardial infarction, or congestive heart failure. Diabetics aged 65–75 in NYC were more likely to receive an eye exam and a blood lipid test than diabetics in the United States, but differences are small.
These few comparisons do not suggest that health services in NYC are more successful at advancing residents' health than health services in the US, or that they have improved more rapidly. On the other hand, the comparisons do not take account of the high level of poverty in NYC (Table 3). In this regard, it is relevant that New York State in 2001 expanded Medicaid eligibility to childless adults with incomes up to 100 percent of the federal poverty level and to parents with incomes up to 150 percent of the federal poverty level. This expansion was associated with a statistically significant reduction in mortality among those aged 19–64 (Sommers, Baiker, and Epstein 2012). In New York, children under age one year and pregnant women are eligible for Medicaid with family incomes up to 200 percent of the federal poverty level, instead of the federal cutoff of 133 percent (Bihari 2013). To illustrate the reach of Medicaid in NYC, 59.2 percent of births in the city in 2009 were covered by Medicaid (NYC DHMH 2010d). While medical services do not appear to be superior in NYC, the fact that they are of roughly comparable quality (given the few data available on this matter) may point to a programmatic success.
Conclusion
NYC's effective campaign to combat the incidence of and mortality from HIV/AIDS made a large contribution to its exceptionally rapid gain in life expectancy. The contribution was especially large among males and in the decade of the 1990s. Over the entire period 1990–2010, reductions in mortality from HIV/AIDS were responsible for 24 percent of the faster longevity gains in NYC relative to the US among men and 8 percent among women. These contributions, estimated from vital statistics, are likely to be underestimated because deaths from HIV/AIDS were probably substantially underregistered during the baseline period of 1989–1990.
Other causes of death with clear-cut behavioral underpinnings also contributed to relative longevity gains in NYC. Reductions in homicide mortality contributed 13 percent of the 1990– 2010 gains among men and 3 percent among women. Drug- and alcohol-related causes contributed 26 percent of the male improvement between 2000 and 2010 and 14 percent of the female improvement. This relative improvement occurred because NYC had falling death rates from this set of causes while the US had rising rates. Deaths attributable to smoking fell faster in NYC than in the US, although the small difference suggests that smoking differences played a minor role in comparative mortality trends. “Other external causes of death” contributed some 6.5 percent of the decline relative to the US for both sexes.
Contrasting conditions in 1990 to those in 2010 puts our results in bold relief. In 1990, a slight majority (51 percent) of NYC's shortfall in life expectancy for both sexes combined was attributable to the combination of HIV/AIDS and homicide. As noted, that figure is probably an underestimate. Successful municipal campaigns to reduce the toll of these urban blights helped to produce a very different situation two decades later. By 2010, New York City had a sizable longevity advantage. That advantage is entirely attributable to the high proportion of immigrants in its population. In 2010, the foreign-born population in NYC and the US had nearly identical life expectancies. Likewise, the US-born population in NYC had nearly the same life expectancy as the US-born population in the US. The reason NYC had higher life expectancy for the population as a whole (by 1.7 years for males and 2.1 years for females) is simply that the foreign-born are a much higher fraction of NYC's population.
While many other pluses and minuses enter into the comparison, immigrants are playing the leading role in the longer lives of New Yorkers. Are they simply carrying with them the higher life expectancies that many other countries experience? The high concentration of immigrants in NYC from the high-mortality regions of Latin America, the Caribbean, Africa, and the Indian subcontinent should discourage such speculation. But perhaps the most telling datum is that immigrants to NYC in 2010 had as high a life expectancy as any country in the world in 2011 (compare Table 5 with World Health Organization 2013: Table 1). Immigrants to the US as a whole also enjoy this distinction. Immigrants are clearly being selected on traits associated with good health.
Thus, one of the most important features of NYC accounting for its superior longevity is its attractiveness to immigrants. While many of these features represent informal institutions and arrangements reflecting New York's long standing as a global gateway, others are direct products of governmental action. These include the Mayor's Office of Immigrant Affairs, which gives advice to undocumented immigrants about the city services they can receive, and the translation of important public documents into six languages to accommodate the one-half of New Yorkers who speak a language other than English at home (Waters and Kasinitz 2013; Foner 2007).
Policies regarding immigrants may seem an unlikely element in the set of public policies affecting life expectancy, but they clearly belong there because of the powerful longevity advantage of immigrants. New York City's exceptional longevity is a surprising and vivid illustration of the widespread impact of immigration on American life.
Acknowledgments
Principal support for this research was provided by a grant from the Robert Wood Johnson Foundation. Additional support was supplied by a grant from the National Institute on Aging, R01-AG040212. We are grateful to Ye Wang for research assistance and to Katherine Hempstead for helpful suggestions.
Appendix Table A.1. Coding of the causes of death by year of death according to International Cause of Death (ICD)-9 and ICD-10.
| Cause of death | ICD-9 for 1989, 1990 | ICD-10 for 1999, 2000, 2009, 2010 |
|---|---|---|
| HIV/AIDS | 042–044 | B20–B24 |
| Other infectious diseases | 001–139, 771.3 excluding 034.0, 135, 042–044 | A00–B99 excluding B20–B24 |
| Lung cancer | 162 | C33, C34 |
| Breast, colon, prostate, rectal, and anal cancer | 174, 175, 185, 153–154 | C50, C61, C18–C21 |
| All other cancers | 140–239 excluding 162, 174, 175, 185, 153–154 | C00–D48, excluding C33, C34, C50, C61, C18–C21 |
| Mental disorders | 290–319 | F01–F99 |
| Nervous system and sense organ, incl. Alzheimer's | 320–389 | G00–G98, H00–H57, H60–H93 |
| Circulatory diseases | 390–459 | I00–I99 |
| Respiratory diseases | 460–519, 034.0 | J00–J98 |
| Diseases of the digestive system | 520–579 | K00–K92 |
| Diseases of the genitourinary system | 580–629 | N00–N98 |
| Perinatal conditions | 760–779, excluding 771.3 | P00–P96 |
| Homicide | E960–E969 | X85–Y09, Y87.1 |
| Other external causes | E800–E999, excluding E960–E969 | V01–Y89, excluding X85–Y09, Y87.1 |
| Symptoms, signs, and ill-defined conditions | 780–799 | R00–R99 |
| All other causes | 135, 240–279, 280–289, 630–676, 680–709, 710–739, 740–759 | E00–E88, D50–D89, O00–O99, L00–L98, M00–M99, Q00–Q99, U00–U99 |
|
| ||
| Drug- and alcohol-related causesa ICD-10 for 1999, 2000, 2009, 2010 | D52.1, D59.0, D59.2, D61.1, D64.2, E06.4, E16.0, E23.1, E24.2, E24.4, E27.3, E66.1, F10, F11.0–F11.5, F11.7–F11.9, F12.0–F12.5, F12.7–F12.9, F13.0–F13.5, F13.7–F13.9, F14.0–F14.5, F14.7–F14.9, F15.0–F15.5, F15.7–F15.9, F16.0–F16.5, F16.7–F16.9, F17.0, F17.3–F17.5, F17.7–F17.9, F18.0–F18.5,F18.7–F18.9, F19.0–F19.5, F19.7–F19.9, G21.1, G24.0, G25.1, G25.4, G25.6, G31.2, G44.4, G62.0, G62.1, G72.0, G72.1, I42.6, I95.2, J70.2–J70.4, K29.2, K70, K85.2, K85.3, K86.0, L10.5, L27.0–L27.1, M10.2, M32.0, M80.4, M81.4, M83.5, M87.1, R50.2, R78.0, R78.1–R78.5, X40–X44, X45, X60–X64, X65, X85, Y10–Y14, Y15 | |
Coding of drug- and alcohol-related causes based on Miniño et al. (2011).
Appendix Table A.2a. Age-standardized crude death rates (ASCDR) by selected cause of death, New York City and the United States: Males 1990, 2000, and 2010 (rates per 100,000 population).
| Cause of death | 1990 | 2000 | 2010 | Change 1990 to 2000 |
Change 2000 to 2010 |
Change 1990 to 2010 |
|---|---|---|---|---|---|---|
|
| ||||||
| New York City | ||||||
|
|
||||||
| HIV/AIDS | 98.08 | 35.54 | 14.44 | −62.54 | −21.10 | −83.64 |
| Lung cancer | 73.14 | 55.75 | 43.70 | −17.39 | −12.05 | −29.44 |
| Homicide | 44.88 | 14.35 | 10.33 | −30.53 | −4.02 | −34.55 |
| Diabetes | 18.43 | 25.89 | 23.25 | 7.46 | −2.64 | 4.82 |
| All causes | 1386.15 | 1005.47 | 773.54 | −380.68 | −231.93 | −612.61 |
| Drug- and alcohol-related causes | — | 31.84 | 24.77 | — | -7.07 | — |
| United States | ||||||
|
|
||||||
| HIV/AIDS | 17.49 | 8.00 | 4.11 | −9.49 | −3.89 | −13.38 |
| Lung cancer | 88.96 | 75.57 | 59.85 | −13.39 | −15.72 | −29.11 |
| Homicide | 14.20 | 9.12 | 8.54 | −5.08 | −0.58 | −5.66 |
| Diabetes | 21.28 | 27.45 | 24.62 | 6.17 | −2.83 | 3.34 |
| All causes | 1206.12 | 1056.69 | 885.78 | −149.43 | −170.91 | −320.34 |
| Drug- and alcohol-relatedcauses | — | 20.71 | 27.19 | NA | 6.48 | NA |
SOURCE: Calculations by the authors.
Appendix Table A.2b. Age-standardized crude death rates (ASCDR) by selected cause of death, New York City and the United States: Females 1990, 2000, and 2010 (rates per 100,000 population).
| Cause of death | 1990 | 2000 | 2010 | Change 1990 to 2000 |
Change 2000 to 2010 |
Change 1990 to 2010 |
|---|---|---|---|---|---|---|
|
| ||||||
| New York City | ||||||
|
|
||||||
| HIV/AIDS | 17.72 | 14.91 | 6.51 | −2.81 | −8.40 | −11.21 |
| Lung cancer | 30.00 | 30.02 | 26.73 | 0.02 | −3.29 | −3.27 |
| Homicide | 7.04 | 2.92 | 1.97 | −4.12 | −0.95 | −5.07 |
| Diabetes | 15.42 | 20.56 | 17.78 | 5.14 | −2.78 | 2.36 |
| All causes | 807.06 | 660.77 | 510.95 | −146.29 | −149.82 | −296.11 |
| Drug- and alcohol-related causes | — | 8.40 | 8.22 | — | −0.18 | — |
| United States | ||||||
|
|
||||||
| HIV/AIDS | 1.97 | 2.53 | 1.54 | 0.56 | −0.99 | −0.43 |
| Lung cancer | 35.92 | 40.14 | 37.78 | 4.22 | −2.36 | 1.86 |
| Homicide | 3.99 | 2.83 | 2.32 | −1.16 | −0.51 | −1.67 |
| Diabetes | 19.43 | 22.49 | 17.31 | 3.06 | −5.18 | −2.12 |
| All causes | 739.28 | 712.28 | 616.24 | −27.00 | −96.04 | −123.04 |
| Drug- and alcohol-related causes | — | 7.62 | 13.59 | NA | 5.97 | NA |
SOURCE: Calculations by the authors.
Appendix Table A.3. Age-standardized crude death rates (ASCDR) in New York City by borough, 1990–2010 (rates per 100,000 population).
| Borough | 1990 | 2000 | 2010 | Percent decline 1990–2010 |
||
|---|---|---|---|---|---|---|
|
| ||||||
| Males | ||||||
|
|
||||||
| Bronx | 1610 | 1164 | 940 | 42 | ||
| Brooklyn | 1414 | 1039 | 792 | 44 | ||
| Manhattan | 1449 | 987 | 703 | 51 | ||
| Queens | 1201 | 902 | 712 | 41 | ||
| Staten Island | 1314 | 1046 | 842 | 36 | ||
| New York City | 1386 | 1005 | 774 | 44 | ||
| Females | ||||||
|
|
||||||
| Bronx | 893 | 756 | 580 | 35 | ||
| Brooklyn | 843 | 679 | 528 | 37 | ||
| Manhattan | 771 | 627 | 466 | 40 | ||
| Queens | 738 | 607 | 471 | 36 | ||
| Island | 876 | 707 | 592 | 32 | ||
| New York City | 807 | 661 | 511 | 37 | ||
SOURCE: Calculations by the authors.
Footnotes
People at ages 85+ were allocated into five-year age groups based on intercensal estimates of the resident population by sex and age prepared by the Census Bureau. http://www.census.gov/popest/data/intercensal/national/files/US-EST90INT-07-1990.csv; http://www.census.gov/popest/data/intercensal/national/nat2010.html. Both were downloaded in February 2013.
In calculating age-specific death rates, we have not adjusted for population undercount in the national or the NYC data. It is estimated that the undercount in NYC was 3.34 percent in 1990, 0.45 percent in 2000, and 0.83 percent in 2010 (Communication with Department of City Planning, New York City, November 2013). The respective estimates for the US made by the Census Bureau are 1.65 percent, 0.12 percent, and 0 percent (Robinson 2001; US Census Bureau 2013). Age-specific undercount estimates for NYC have not been made. Adjustment for the somewhat higher population undercount in NYC than in the US would have the largest impact on our estimates for males in 1990, for whom undercount estimates are the most pronounced. It would reduce NYC–US differences in age-specific death rates and thus the NYC–US difference in life expectancy at birth. Such adjustment, however, would not be large enough to alter our main conclusions.
Male death rates for cancers (breast, colon, and prostate) for which screening is common rose slightly in NYC relative to the US, but the decline in mortality from these cancers among females was larger than the male increase.
The life expectancy differences between NYC and the US are identical when comparing life expectancies at age one, which are not affected by the fact that almost no foreign-born babies are present in the United States during the risky perinatal period. However, the discrepancy in life expectancies between native-born and foreign-born in 2008-10 is smaller at age one than at zero by 0.36-0.50 years in the four comparisons by sex and residence shown in Table 5.
Adult men drinking more than 2 drinks per day and adult women more than 1 drink per day.
All information on the use of services by Medicare recipients was obtained from the Dartmouth Atlas Project and downloaded from http://www.dartmouthatlas.org/tools/downloads.aspx/. County-level data were aggregated to obtain estimates for NYC as a whole. For further detail, see also Goodman et al. (2010, 2011).
Publisher's Disclaimer: This is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication. PDR is providing this early version of the manuscript as a service to our readers. The manuscript will undergo copyediting, typesetting, and a proof review before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers apply.
Contributor Information
Samuel H. Preston, Population Studies Center, University of Pennsylvania.
Irma T. Elo, Population Studies Center, University of Pennsylvania.
References
- Alcorn Ted. Redefining public health in New York City. Lancet. 2012;379:2037–2038. doi: 10.1016/s0140-6736(12)60879-4. [DOI] [PubMed] [Google Scholar]
- Al-Samarrai T, et al. Impact of a hospital-level intervention to reduce heart disease overreporting on leading causes of death. Preventing Chronic Disease. 2013;10(4):1–10. doi: 10.5888/pcd10.120210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson Norman B, Bulatao Rodolfo A, Cohen Barney. Critical Perspectives on Racial and Ethnic Differences in Health in Late Life. Washington, DC: National Academies Press (US); 2004. [PubMed] [Google Scholar]
- Arriaga Eduardo. Measuring and explaining the change in life expectancies. Demography. 1984;21(1):83–96. [PubMed] [Google Scholar]
- Bihari Michael. Medicaid eligibility—An overview of Medicaid eligibility and benefits. understanding your state's Medicaid Program. 2013 http://healthinsurance.about.com/od/medicaid/a/medicaid_overview.htm.
- Chiasson M, et al. Declining HIV/AIDS mortality in New York City. Journal of Acquired Immune Deficiency Syndromes. 1999;21(1):59–64. doi: 10.1097/00126334-199905010-00008. [DOI] [PubMed] [Google Scholar]
- City of New York, Office of the Mayor. Mayor Bloomberg, Deputy Mayor Gibbs, Health Commissioner Farley announce New Yorkers living longer than ever, outpacing national trend. 2011 Press Release No. 453, 27 December. [Google Scholar]
- Cohen Jon. Miracle on 34th Street: Success with Injectors. Science. 2012;337:178–180. doi: 10.1126/science.337.6091.178. [DOI] [PubMed] [Google Scholar]
- Crimmins Eileen, Preston Samuel, Cohen Barney. Explaining Divergent Levels of Longevity in High Income Countries. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- Des Jarlais DC, et al. HIV incidence among injection drug users in New York City, 1990 to 2002: Use of serologic test algorithm to assess expansion of HIV prevention services. American Journal of Public Health. 2005;95(8):1439–1444. doi: 10.2105/AJPH.2003.036517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupre Matthew E, Gu Danan, Vaupel James W. Survival differences among native-born and foreign-born older adults in the United States. PLOS One. 2012;7(5):e37177. doi: 10.1371/journal.pone.0037177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elo Irma T. Social class differentials in health and mortality: Patterns and explanations in comparative perspective. Annual Review of Sociology. 2009;35:553–572. [Google Scholar]
- Fackelmann Kathy. AIDS toll underestimated in IV drug users. Science News. 1988 Nov 12; www.thefreelibrary.com.
- Fenelon Andrew. Revisiting the Hispanic mortality advantage in the United States: The role of smoking. Social Science and Medicine. 2013;82:1–9. doi: 10.1016/j.socscimed.2012.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foner Nancy. How exceptional is New York? Migration and multiculturalism in the empire city. Ethnic and Racial Studies. 2007;30(6):999–1023. [Google Scholar]
- Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: A systematic review and meta-analysis. Journal of the American Medical Association. 2013;309(1):71–82. doi: 10.1001/jama.2012.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frieden Thomas R, Bassett Mary T, Thorpe Lorna E, Farley Thomas A. Public health in New York City, 2002–2007: Confronting epidemics of the modern era. International Journal of Epidemiology. 2008;37:966–977. doi: 10.1093/ije/dyn108. [DOI] [PubMed] [Google Scholar]
- Goodman David C, Brownlee Shannon, Chang Chiang-Hua, Fisher Elliott S. Regional and racial variation in primary care and the quality of care among Medicare beneficiaries. The Dartmouth Institute for Health Policy and Clinical Practice; 2010. http://www.dartmouthatlas.org/tools/downloads.aspx. [PubMed] [Google Scholar]
- Goodman David C, Fisher Elliott S, Chang Chiang-Hua. After hospitalization: A Dartmouth Atlas Report on Post-Acute Care for Medicare Beneficiaries. The Dartmouth Institute for Health Policy and Clinical Practice; 2011. http://www.dartmouthatlas.org/tools/downloads.aspx. [PubMed] [Google Scholar]
- Jasso Guillermina, Massey Douglas S, Rosenzweig Mark R, Smith James P. Immigrant health: Selectivity and acculturation. In: Anderson Norman B, Bulatao Rodolfo A, Cohen Barney., editors. Critical Perspectives on Racial and Ethnic Differences in Health in Late Life. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- Jha P, et al. 21st-Century hazards of smoking and benefits of cessation in the United States. New England Journal of Medicine. 2013;368:341–350. doi: 10.1056/NEJMsa1211128. [DOI] [PubMed] [Google Scholar]
- Kenfield Stacey, Stampfer Meir J, Rosner Bernard A, Colditz Graham A. Smoking and smoking cessation in relation to mortality in women. Journal of the American Medical Association. 2008;299(17):2037–2047. doi: 10.1001/jama.299.17.2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall Brandon, et al. Complex systems approach to evaluate HIV prevention in metropolitan areas: Preliminary implications for combination intervention strategies. PLOS One. 2012;7(9):e44833 1–16. doi: 10.1371/journal.pone.0044833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinnis JM, Foege WH. Actual causes of death in the United States. Journal of the American Medical Association. 1993;270(18):2207–2212. [PubMed] [Google Scholar]
- Miniño AM, Murphy SL, Xu JQ, Kochanek KD. National Vital Statistics Reports. 10. Vol. 50. Hyattsville, MD: National Center for Health Statistics; 2011. Deaths: Final data for 2008. [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. Journal of the American Medical Association. 2004;291(10):1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Correction: Actual causes of death in the United States, 2000. Journal of the American Medical Association. 2005;293(3):293–294. doi: 10.1001/jama.293.3.293. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute. U.S. Population data 1969–2011. [Accessed February 2013];2013 http://seer.cancer.gov/popdata/download.html.
- New York City Department of Health and Mental Hygiene (NYC DHMH) The Health of Immigrants in New York City. New York: 2006. [Google Scholar]
- New York City Department of Health and Mental Hygiene (NYC DHMH) Substance use among New York City youth. NYC Vital Signs. 2007;6(1) [Google Scholar]
- New York City Department of Health and Mental Hygiene (NYC DHMH) Annual Summary of Vital Statistics 2007. New York: 2008. [Google Scholar]
- New York City Department of Health and Mental Hygiene (NYC DHMH) Diabetes among New York City adults. NYC Vital Signs. 2009a;8(5) [Google Scholar]
- New York City Department of Health and Mental Hygiene (NYC DHMH) Agency Biennial Report: 2007–2008. New York: 2009b. [Google Scholar]
- New York City Department of Health and Mental Hygiene (NYC DHMH) Health Disparities in Life Expectancy and Death. New York: 2010a. [Google Scholar]
- New York City Department of Health and Mental Hygiene (NYC DHMH) Health of older New Yorkers. NYC Vital Signs. 2010a;8(4) [Google Scholar]
- New York City Department of Health and Mental Hygiene (NYC DHMH) Health consequences of alcohol use in New York City. NYC Vital Signs. 2010b;9(5) [Google Scholar]
- New York City Department of Health and Mental Hygiene (NYC DHMH) Illicit drug use in New York City. NYC Vital Signs. 2010c;9(1) [Google Scholar]
- New York City Department of Health and Mental Hygiene (NYC DHMH) Summary of Vital Statistics 2009: The City of New York. New York: 2010d. [Google Scholar]
- New York City Department of Health and Mental Hygiene (NYC DHMH) Summary of Vital Statistics 2010: The City of New York. New York: 2011a. [Google Scholar]
- New York City Department of Health and Mental Hygiene (NYC DHMH) Trends in cigarette use among adults in New York City, 2002–10. Epi Data Brief. 2011b;12 [Google Scholar]
- New York City Department of Health and Mental Hygiene (NYC DHMH) Health benefits of active transportation in New York City. NYC Vital Signs. 2011c;10(3) [Google Scholar]
- New York City Department of Health and Mental Hygiene (NYC DHMH) Increased life expectancy in New York City: What accounts for the gains? Epi Research Report 2013 [Google Scholar]
- Oeppen Jim, Vaupel James. Broken limits to life expectancy. Science. 2002;296(5570):1029–1031. doi: 10.1126/science.1069675. [DOI] [PubMed] [Google Scholar]
- Oza Shefali, Thun Michael J, Henley S Jane, Lopez Alan D, Majid Ezzati. How many deaths are attributable to smoking in the United States? Comparison of methods for estimating smoking-attributable mortality when smoking prevalence changes. Preventive Medicine. 2011;52:428–433. doi: 10.1016/j.ypmed.2011.04.007. [DOI] [PubMed] [Google Scholar]
- Peto R, Lopez A, Boreham J, Thun M, Heath C. Mortality from tobacco in developed countries: Indirect estimation from national vital statistics. Lancet. 1992;339(8804):1268–1278. doi: 10.1016/0140-6736(92)91600-d. [DOI] [PubMed] [Google Scholar]
- Preston Samuel H. Mortality Patterns in National Populations. New York: Academic Press; 1976. [Google Scholar]
- Preston Samuel H. Causes and consequences of mortality change in less developed countries in the twentieth century. In: Easterlin R, editor. Population and Economic Change in Developing Countries. University of Chicago Press; 1980. pp. 289–360. [Google Scholar]
- Preston SH, Glei Dana, Wilmoth John. Contribution of smoking to international differences in life expectancy. In: Crimmins Eileen, Preston Samuel, Cohen Barney., editors. International Differences in Mortality at Older Ages: Dimensions and Sources. Washington, DC: National Academies Press; 2011. pp. 105–131. [PubMed] [Google Scholar]
- Preston Samuel H, Heuveline Patrick, Guillot Michel. Demography: Measuring and Modeling Population Processes. Oxford: Blackwell; 2001. [Google Scholar]
- Preston SH, Wang Haidong. Changing sex differentials in mortality in the United States: The role of cohort smoking patterns. Demography. 2006;43(4):413–434. doi: 10.1353/dem.2006.0037. [DOI] [PubMed] [Google Scholar]
- Robinson J Gregor. Report No 1 prepared for the Executive Steering Committee for ACE Policy II. Washington, DC: US Census Bureau; 2001. ESCAP II: Demographic Analysis Results. http://www.census.gov/dmd/www/pdf/Report1.PDF. [Google Scholar]
- Ruggles Steven, et al. Integrated Public Use Microdata Series: Version 5.0 [Machine-readable database] Minneapolis: University of Minnesota; 2010. [Google Scholar]
- Singh Gopal K, Siahpush Mohammad. Ethnic-immigrant differentials in health behaviors, morbidity, and cause-specific mortality in the United States: An analysis of two national data bases. Human Biology. 2002;74(1):83–109. doi: 10.1353/hub.2002.0011. [DOI] [PubMed] [Google Scholar]
- Smith James. The impact of socioeconomic status on health over the life-course. Journal of Human Resources. 2007;42(4):739–764. [Google Scholar]
- Sommers Benjamin D, Baicker Katherine, Epstein Arnold M. Mortality and access to care among adults after state Medicaid expansions. New England Journal of Medicine. 2012;367:1025–1034. doi: 10.1056/NEJMsa1202099. [DOI] [PubMed] [Google Scholar]
- Steptoe Andrew, Wikman Anna. The contribution of physical activity to divergent trends in longevity. In: Crimmins Eileen, Preston Samuel, Cohen Barney., editors. International Differences in Mortality at Older Ages: Dimensions and Sources. Washington, DC: National Academies Press; 2010. pp. 193–217. [PubMed] [Google Scholar]
- Taylor Brian, Miller Douglas, Iseki Hiroyuki, Fink Camille. Nature and/or nurture? Analyzing the determinants of transit ridership across US urbanized areas. Transportation Research, Part A: Policy and Practice. 2008;43(1):60–77. doi: 10.1016/j.tra.2008.06.007. [DOI] [Google Scholar]
- Trang QN, et al. Population prevalence of reported and unreported HIV and related behaviors among the household adult population in New York City, 2004. AIDS. 2008;22(2):281–287. doi: 10.1097/QAD.0b013e3282f2ef58. [DOI] [PubMed] [Google Scholar]
- Turra Cassio, Elo Irma. The impact of salmon bias on the Hispanic mortality advantage: New evidence from Social Security data. Population Research and Policy Review. 2008;27:515–530. doi: 10.1007/s11113-008-9087-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Census Bureau. Revised 2010 demographic analysis estimates. [Accessed 25 November 2013]; http://www.census.gov/popest/research/demo-analysis.html.
- Wang Haidong, Schumacher Austin E, Levitz Carly E, Mokdad Ali H, Murray Christopher JL. Left behind: Widening disparities for males and females in US county life expectancy, 1985–2010. Population Health Metrics. 2013;11(8):1–15. doi: 10.1186/1478-7954-11-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters Mary C, Kasinitz Philip. Immigrants in New York City: Reaping the benefits of continuous immigration. Daedalus. 2013;142(3):92–106. [Google Scholar]
- Whitlock G, Lewington S, Sherliker P. Prospective studies collaboration—Body-mass index and cause-specific mortality in 900 000 adults: Collaborative analyses of 57 prospective studies. Lancet. 2009;37:1083–1096. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf Steve, Aron Laudan. National Research Council and Institute of Medicine. US Health in International Perspective: Shorter Lives, Poorer Health. Washington, D.C.: National Academies Press; 2013. [PubMed] [Google Scholar]
- World Health Organization. World Health Statistics 2013. Geneva: 2012. [Google Scholar]
- Zimring Franklin E. The City that Became Safe: New York's Lessons for Urban Crime and Its Control. New York: Oxford University Press; 2012. [Google Scholar]