Abstract
Rural Mexican immigrant women in the U.S. are infrequently screened and experience health disparities from cervical cancer. We explored cancer-related cultural beliefs in this population. We administered a cross-sectional survey to 39 Mexican immigrant women due for screening. We conducted univariate and bivariate analyses of participants’ characteristics, Pap test history, cancer-related knowledge and beliefs, and cultural consensus analysis about causes of cervical cancer and barriers to screening. For all the cultural consensus tasks, there was consensus (Eigenratios >3:1) among survey participants. Comparing the rankings of risk factor clusters, clusters related to sexual behaviors were ranked more severely than clusters related to genetic or other behavioral factors. There was agreement on ideas of cervical cancer causation and barriers to screening among these women. Hence, improved methods of disseminating important health information and greater access to care are needed, particularly in relationship to stigma about sex and birth control practices.
Keywords: Cervical cancer, Cancer screening, Cultural consensus, Immigrant, Hispanics/Latinos
Introduction
For the period 2006–2010 in the U.S., Hispanics/Latinas had uterine cervix incidence and mortality rates of 10.9 and 2.9 per 100,000 population, compared to rates for non-Hispanic whites of 7.2 and 2.1, respectively [1, 2]. Differences in incidence and mortality are related to lower rates of screening with the Pap test among U.S.-born Latinas and Latina immigrant populations compared to non-Latina whites. The U.S. Preventive Services Task Force (2012) guidelines recommend women between 21 and 30 years old receive a Pap test every 3 years; women between 30 and 65 years old receive a Pap test and HPV DNA test every 5 years or continue receiving a Pap test every 3 years [3]. Cervical cancer can be prevented by following these guidelines. Mexican and other foreign-born women have a 26 % higher rate of not being up-to-date with cervical cancer screening than U.S.-born women. Moreover, the rate of never being screened is 43 % greater for Latina immigrants than U.S.-born Latina women [4].
Disparities in cancer incidence, mortality and screening, coupled with additional health inequalities between urban and rural populations in the southeastern U.S., highlight the need to focus on cervical cancer prevention efforts among specific groups suffering cancer health disparities, among whom are Latina immigrants and farmworkers [5, 6]. Migrant and seasonal farmworker populations have greater exposure to environmental risk factors for cancer (e.g., pesticides), less access to health services, greater time constraints, and lower education than other Latino occupational groups in the U.S. [7, 8]. Access to cervical cancer screening and appropriate follow-up for Latina farmworkers is affected by multiple factors including language barriers, transportation challenges, fear of a potential positive diagnosis, perceived discrimination, and embarrassment around the test [9–14]. Cultural factors such as mistrust of healthcare providers that might contribute to adverse outcomes for this group are understudied and underestimated [15].
To gain a better understanding of cultural factors that might implicate screening practices among rural Mexican immigrant women, we examined knowledge and beliefs about causes of cervical cancer and perceived barriers to Pap test compliance in southeastern Georgia. The objective of the study was to explore cancer-related cultural beliefs of rural Mexican immigrants and to inform the development and testing of a lay health advisor efficacy trial to increase cervical cancer screening among rural Latina immigrant women.
Conceptual Framework
The cervical cancer prevention program, Salud es Vida (“Health is Life”), began as a participatory research project that trained lay health advisors, or promotoras, in rural, southeastern Georgia to conduct community-based health education in farmworker communities [16, 17]. Salud es Vida was designed using constructs from Social Cognitive Theory, especially self-efficacy and behavioral capability, and Popular Education approaches such as brainstorming [18, 19]. The program was developed and adapted from other lay health advisor training materials [20, 21]. Promotoras trained through the program expressed positive self-efficacy to receive a Pap test and to incentivize screening behavior among their fellow community members using peer influence [16]. The program is currently being tested for efficacy using an experimental design.
To explore cervical cancer beliefs among Latina immigrant women, we administered a survey to examine knowledge of cervical cancer etiology and barriers to health care. We used a mixture of survey questions and structured tasks to assess the extent of agreement among participants, or cultural consensus, in these domains. The structured task method allows for direct measurement of inter-participant agreement on the structure, organization, and content of a knowledge domain and the calculation of individual competence (cultural competence) and average level of competency for the group on the knowledge domain [22]. Cultural competence is an estimate of the degree to which an individual agrees with the group beliefs. Research conducted in southern California found that cultural beliefs about cervical cancer etiology had an effect on the decision to receive a Pap test, suggesting that beliefs—such as early initiation of sexual activity and sex during menstruation—are important predictors of actual behavior [23–25].
Methods
Study Design
We conducted a cross-sectional survey in Spanish with Latina immigrant women who had not received a Pap test in three or more years, had worked in agriculture, had no history of a hysterectomy, and were born in Mexico. Sample size determination for cultural consensus analysis follows the convention that given an average level of cultural competence (.5), a 95 % probability of answering questions correctly and a confidence level of .95, there should be a minimum of 17 participants [26]. We selected a purposive sample of 17–20 women aged 21–65 years living in the U.S. for 10 years or less and 17–20 women living in the U.S. for over 10 years to introduce variation in time living in the U.S. in the sample. To recruit women from a 3-county area with a total population of 64,000 (range of 4–13 % Hispanic population), 258 women were screened for eligibility, and 15 % were eligible [27]. The most common reason for not being eligible for the survey was having a Pap test within 3 years (85 % of all ineligibility reasons). Women who were up-to-date with their Pap tests because they had recent contact with the health care system due to birth control needs were ineligible for the study. Less common reasons for not being included in the study were country of origin other than Mexico, prior hysterectomy and lack of agricultural experience. Most women were recruited through major farm operations and a poultry processing plant. Survey participants received a $10 gift card.
Measures
The study was approved by the Georgia Southern University institutional review board. A trained female interviewer fluent in Spanish recruited the women and administered the paper and pencil survey face-to-face. Survey questions were adapted from a previous survey [28] with additional measures including the Acculturation Scale for Mexican–Americans (ASMA). The ASMA measures language acculturation using a 4-question instrument scored on a scale of 0 (low acculturation, Spanish language dominant) to 4 (high acculturation, English language dominant) [29]. Structured tasks included a 15-item note-card ranking and pile sort exercise on cervical cancer causes and a constrained 15-item pile sort of barriers to accessing health care. The interviewer performed a practice exercise using pictures of fruits to demonstrate the pile sort task. These items had been identified through freelisting tasks in previous studies with Latina immigrant women [23, 28]. For the pile sort exercises, we asked participants to sort items into four piles, as well as label each pile. Examples of causes included abortion, family history, and multiple sex partners. Examples of barriers included cost, not having access to transportation, and fear of the exam. We asked participants to agree or disagree with a list of 32 possible cervical cancer causes and seven attitudinal statements about cervical cancer.
Survey questions were pretested with five representative community members to ensure face validity, and several questions were modified to ensure comprehensibility. The survey took approximately 45 min to administer.
Statistical Methods
Descriptive and bivariate statistics of participants’ characteristics, cervical cancer screening history, knowledge, beliefs and perceptions about causes of cervical cancer and barriers to Pap test use were calculated using SPSS Statistics V. 21 (SPSS, Inc. Chicago, Illinois). UCINET 6.0 (Analytic Technologies, Lexington, Kentucky) was used to calculate cultural consensus for 32 agree/disagree questions about cervical cancer causes, seven agree/disagree questions about attitudes, and rank data for cervical cancer causes. Visual Anthropac (Analytic Technologies, Lexington, Kentucky) was used to analyze pile sort data on cervical cancer causes and barriers to health care. The results of the ranking and pile sort data were visualized using non-metric multidimensional scaling (MDS) and average linkage clustering set to five clusters. We used the rankings to further explore the dimensions underlying the pile sort MDS for the cervical cancer causes. Post-hoc analyses examined differences between pile sort categories (1–5) and the corresponding rankings using the ANOVA test, and of differences between the average ranks by groups using the LSD test [30].
Results
Description of Participants
The study sample comprised 39 women (20 women ≤10 years in the U.S. and 19 women >10 years in the U.S.) primarily from East and Central Mexico (Tamaulipas, Guanajuato, and Guerrero) (see Table 1). The average age for the entire sample was 40 years (±10.5) with an average of 8 years of education (±4.6). Thirty-three women (85 %) preferred speaking Spanish, whereas the others spoke both English and Spanish. The overall acculturation level, based on ASMA, was low on the 0–4 scale (.95), indicating participants were more comfortable conducting their daily lives in Spanish. Fifteen (39 %) women had visited a doctor in the last year; however, six (15 %) women reported that they used medical services in Mexico due to affordability. In addition, nine (23 %) women said that their last Pap test was in Mexico. Table 1 provides a summary of additional demographic indicators.
Table 1.
Demographic characteristics of survey participants by time in the U.S.
| Characteristic | Mexican women ≤10 years in U.S. (N = 20) | Mexican women > 10 years in U.S. (N = 19) | Mexican women total (N = 39) |
|---|---|---|---|
| Age, years | 36 (23–53) | 44 (24–56) | 40 (23–56) |
| Years of schooling | 9 (0–19) | 7 (1–19) | 8 (0–19) |
| Years in U.S. | 5 (.1–10) | 18 (11–35) | 12 (.1–35) |
| Median income category/week | $250–$500 | $250–$500 | $250–$500 |
| Score on ASMA acculturation scale (0 = low to 4 = high) | .75 (0–2) | 1.16 (0–2) | .95 (0–2) |
| Marital status | |||
| Married/living with a partner | 12 (60 %) | 17 (90 %) | 29 (74 %) |
| Single/other | 8 (40 %) | 3 (10 %) | 11 (28 %) |
| Currently employed | 18 (90 %) | 16 (84 %) | 34 (87 %) |
| Regular health care provider | 7 (35 %) | 8 (42 %) | 15 (38 %) |
| Women who have a chronic condition | 4 (20 %) | 5 (26 %) | 9 (23 %) |
| Health insurance | 0 (0 %) | 1 (5 %) | 1 (3 %) |
| Residence | |||
| Rent | 13 (65 %) | 7 (37 %) | 20 (51 %) |
| Own | 7 (35 %) | 12 (63 %) | 19 (49 %) |
Columns in mean values (ranges) for continuous variables and frequencies (percentages) for categorical variables. The Acculturation Scale for Mexican Americans (ASMA) was used to measure acculturation
Cervical Cancer Screening History and HPV Knowledge
Twenty-four women (62 %) reported having received gynecological services in the U.S. Seven (18 %) women reported they had never received a Pap test. Based on our inclusion criteria, the remaining women were not up-to-date (last Pap test >3 years) and were due for a Pap test. Regarding the change in time interval for receiving a regular Pap test from yearly to every 3 years, only four (10 %) women had heard of the change in guidelines. Fifteen (39 %) women reported that a provider had recommended receiving a Pap test. The health department was the most commonly reported facility for receiving a Pap test. Additional descriptive statistics on cervical cancer screening data are provided in Table 2.
Table 2.
Health history, cervical cancer screening history, and HPV knowledge among Mexican immigrant women
| Survey item | ≤10 years in U.S. (N = 20) (%) | > 10 years in U.S. (N = 19) (%) | Total (N = 39) (%) |
|---|---|---|---|
| Had gynecological services in the U.S. | 8 (40) | 16 (84) | 24 (62) |
| Had a provider who spoke Spanish | 6 (30) | 3 (16) | 9 (23) |
| Had never received a Pap test | 5 (25) | 2 (11) | 7 (18) |
| Pap test before the most recent Pap test was within the past 3 years | 6 (30) | 10 (53) | 16 (41) |
| Had heard of the change in Pap testing interval | 3 (15) | 1 (5) | 4 (10) |
| Had received a provider’s recommendation for a Pap test | 10 (50) | 5 (26) | 15 (39) |
| Had heard of HPV | 14 (70) | 8 (42) | 22 (56) |
| Thought HPV caused cervical cancer | 10 (50) | 8 (42) | 18 (46) |
| Thought HPV was sexually transmitted | 11 (55) | 9 (47) | 20 (51) |
| Thought HPV was common | 9 (45) | 10 (53) | 19 (49) |
| Thought HPV would go away on its own without treatment | 1 (5) | 2 (11) | 3 (8) |
| Thought HPV could cause abnormal Pap tests | 9 (45) | 10 (53) | 19 (49) |
| Had heard of the HPV vaccine | 8 (40) | 8 (42) | 16 (41) |
| Thought the HPV vaccine was an effective way to prevent HPV infection | 16 (80) | 18 (95) | 34 (87) |
| Had a history of a STD diagnosis | 0 (0) | 3 (16) | 3 (8) |
Columns in frequencies (percentages) of women who reported a characteristic
In response to an open-ended question about what they had heard about cervical cancer, many women knew that the cancer started in the genital area, and five (13 %) women mentioned the HPV vaccine or the Pap test as prevention methods. Twenty-seven (69 %) women said they did not know or knew very little about cervical cancer. Twenty-two (56 %) women had heard of HPV, and 18 (46 %) women believed HPV caused cervical cancer. Nearly half of study participants (49 %) agreed that HPV was very common and could cause abnormal Pap tests, but only 16 (41 %) women had heard of the HPV vaccine. Even though slightly over half of the women had heard of HPV, even more women [34 (87 %)] believed the vaccine would prevent HPV.
Cultural Consensus Analysis Findings
For all the cultural consensus tasks (see Table 3), there was consensus (Eigenratios >3:1) regardless of how long participants had lived in the U.S. There was consensus for the 39 agree/disagree questions on cervical cancer causes and agree/disagree statements on attitudes and beliefs (Eigenratio = 8.0) (see Table 4). Agree/disagree responses revealed a wide range (13–95 %) of endorsement of possible perceived causes (abortion, alcohol use, sex during one’s menstrual period, poor feminine hygiene, vaginal trauma, fate, and worry). Few endorsed the idea that psychosocial causes such as worry, stress, and fate were important causes. The only biomedical risk factor that was not highly endorsed was low income. There was consensus among the participants for the rank order of cervical cancer causes based on perceived severity (Eigenratio = 4.7). Out of the 15 possible causes of cervical cancer, the top five ranked causes were: (1) multiple sex partners; (2) HPV; (3) HIV; (4) lack of a regular Pap test; and (5) sexual relations before 16 years of age.
Table 3.
Cervical cancer causes, attitudes, and beliefs of Mexican immigrant women by time in the U.S
| Variables | ≤10 years in U.S. (N = 20) (%) | > 10 years in U.S. (N = 19) (%) | Total (N = 39) (%) |
|---|---|---|---|
| Causes | |||
| Behaviors, experiences, and lifestyle choices | |||
| Sexual intercourse before age 16 yearsa | 17 (85) | 14 (74) | 31 (79) |
| Multiple sexual partnersa | 19 (95) | 18 (95) | 37 (95) |
| Spouse with multiple sexual partnersa | 18 (90) | 17 (90) | 35 (90) |
| Sex during menstrual period | 13 (65) | 14 (74) | 27 (69) |
| Smokinga | 12 (60) | 10 (53) | 22 (56) |
| Poor feminine hygiene | 19 (95) | 17 (90) | 36 (92) |
| Abortion | 16 (80) | 14 (74) | 30 (77) |
| Not getting a regular check-upa | 18 (90) | 17 (90) | 35 (90) |
| Dieta | 12 (60) | 7 (37) | 19 (49) |
| Many pregnancies | 15 (75) | 10 (53) | 25 (64) |
| Birth control pillsa | 16 (80) | 12 (63) | 28 (72) |
| Drink alcohol | 11 (95) | 9 (47) | 20 (51) |
| Vaginal trauma | 15 (75) | 14 (94) | 29 (74) |
| Genetic predisposition | |||
| Family history | 15 (75) | 11 (58) | 26 (67) |
| Other | |||
| Worry | 5 (25) | 6 (32) | 11 (28) |
| Chemicals in food | 9 (45) | 9 (47) | 18 (46) |
| Stress | 7 (35) | 4 (21) | 11 (28) |
| Fate | 5 (25) | 7 (37) | 12 (31) |
| Low incomea | 3 (15) | 2 (11) | 5 (13) |
| Symptoms and infections | |||
| Abnormal vaginal bleedinga | 16 (80) | 16 (84) | 32 (82) |
| Bloody stools | 10 (50) | 10 (53) | 20 (51) |
| Urinating frequently | 7 (35) | 8 (31) | 15 (38) |
| Pelvic rash | 13 (65) | 6 (32) | 19 (49) |
| Weight loss | 3 (15) | 6 (32) | 9 (23) |
| Human papilloma virus (HPV)a | 16 (80) | 17 (90) | 33 (85) |
| HIV infectiona | 17 (85) | 12 (63) | 29 (74) |
| Yeast infections | 17 (85) | 12 (63) | 29 (74) |
| High cholesterol | 5 (25) | 4 (21) | 9 (23) |
| High blood pressure | 4 (20) | 3 (16) | 7 (18) |
| Gonorrheaa | 19 (95) | 15 (79) | 34 (87) |
| Chlamydiaa | 15 (75) | 13 (68) | 28 (72) |
| Syphilisa | 19 (95) | 15 (79) | 34 (87) |
| Attitudes and beliefs | |||
| If cervical cancer is found early, it can be cured | 19 (95) | 18 (95) | 37 (95) |
| I would undergo cervical cancer treatment that is unpleasant or painful if it would increase my chances of living longer | 19 (95) | 19 (100) | 38 (97) |
| I would rather not know if I had cervical cancer | 3 (15) | 2 (11) | 5 (13) |
| I would be afraid to tell my husband or partner if I had cervical cancer | 4 (20) | 3 (16) | 7 (18) |
| I need a Pap smear only when I experience vaginal bleeding other than menstruation (or when I experience other symptoms) | 6 (30) | 5 (26) | 11 (28) |
| There is not much I can do to prevent cervical cancer | 3 (15) | 4 (21) | 7 (18) |
| I am very likely to get cervical cancer sometime in my lifetime | 10 (50) | 14 (74) | 24 (62) |
Columns represent numbers (percentages) agreed
Risk factors/symptoms generally accepted by medical profession
Table 4.
Cultural consensus analysis
| Measure | Ranking causes (N = 39) | Agree/disagree (N = 39) | Pile sort causes (N = 38) | Pile sort barriers (N = 38) |
|---|---|---|---|---|
| Eigenratioa | 4.7 | 8.0 | 7.4 | 14.2 |
| Average competence | .57 (±.32) | .53 (±.26) | .61 (±.10) | .57 (±.10) |
Eigenvalue ratios of 3.0 or greater and lack of negative competence scores indicate a good fit to the consensus model. A competence value of .50 indicates an average level of cultural competence
When participants completed the 15-item pile sort for cervical cancer causes, there was also consensus (Eigenratio = 7.4). Cluster analysis results suggested five clusters: (1) family history, destiny; (2) chemicals in the food, poor diet, smoking; (3) birth control pills, abortion, multiple pregnancies; (4) not using condoms, poor hygiene; and (5) multiple sex partners, sexual relations before age 16, HPV, HIV, not getting a regular Pap test (Fig. 1). The post hoc ANOVA test analyzing rankings for items in each group revealed that clusters 4 (not using condoms, poor hygiene) and 5 (multiple sex partners, sexual relations before age 16, HPV, HIV, not getting a regular Pap test), were the most severe (i.e., perceived as a major risk factor), and significantly more severe than causes in clusters 1 (family history, destiny) and 2 (chemicals in the food, poor diet, smoking) [F (4, 10) = 35.08, p < .001]. Causes in cluster 3 (birth control pills, abortion, multiple pregnancies) ranked in between the other clusters.
Fig. 1.
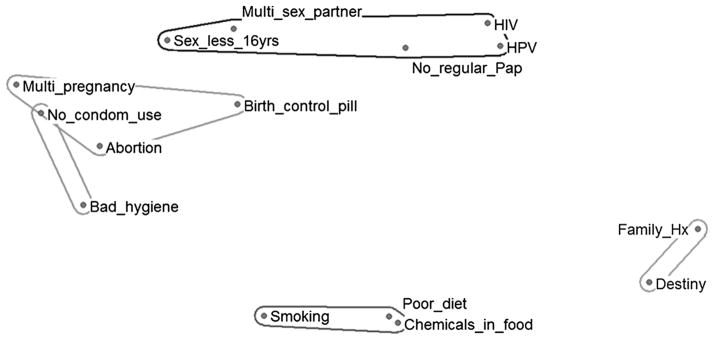
Perceptual map of pile sort of 15 cervical cancer causes. Notes Multi_sex partner = Having multiple sex partners; Sex_less_16 years = Sexual relations before 16 years of age; HPV = Infection with human papilloma virus—HPV; HIV = Having human immunodeficiency virus—HIV can lead to AIDS; No_regular Pap = Not getting regular pap tests; Multi_pregnancy = Many pregnancies; No_condom_use = Not using condoms; Birth_control_pill = Contraceptive pills (to not have babies); Bad_hygiene = Poor feminine hygiene; Smoking = Smoking; Poor_diet = Poor diet; Chemicals_in_food = Chemical products in food; Family_Hx = Family history; Destiny = Destiny or fate
When participants completed the 15-item pile sort for reasons not to get the Pap test or barriers to screening, there was consensus (Eigenratio = 14.2). The five clusters were (1) knowledge deficits (do not know the purpose, do not know the cost, do not know where to get it, lack of knowledge about the test); (2) fear (fear of positive results, fear of the exam, wait for symptoms to appear); (3) social and environmental constraints (no insurance, no transportation, do not speak or understand English, do not have a regular doctor in U.S.); (4) price and place barriers (not convenient, prefer to use services in Mexico, too expensive); and (5) my husband won’t give me permission (Fig. 2).
Fig. 2.
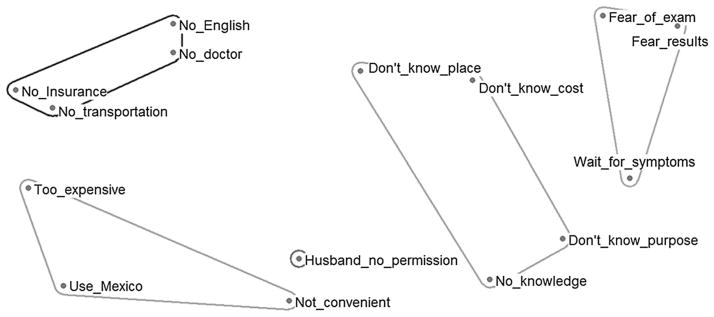
Perceptual map of pile sort of 15 barriers to cervical cancer screening. Notes No_English = Do not speak English; No_doctor = No regular doctor; No_insurance = Do not have health insurance; No_transportation = Do not have transportation; Too_expensive = Too expensive, costs a lot of money; Use_Mexico = Prefer to use medical services in Mexico; Not_convenient = Inconvenient, not worth it; Husband_no_permission = My husband will not allow me to go; No_knowledge = Do not know about cervical cancer; Do not_know_purpose = Do not know the purpose of the Pap test; Don’t_know_cost = Do not know the cost of the Pap Test; Don’t_know_place = Do not know where to go to get a Pap test; Wait_for_symptoms = Wait for symptoms before getting a Pap test; Fear_results = Fear of receiving negative results; Fear_of_exam = Embarrassment or fear of the exam
Discussion
These study findings provide insights into cultural beliefs and understandings of cervical cancer among an under screened Mexican immigrant farmworker population in the southeastern U.S. A sizable number of women were screened for inclusion in the study to identify a sample of under screened women with varying levels of time living in the U.S. In the course of recruiting participants, we informally learned that even among the recently screened, there was low knowledge of preventive measures (i.e., Pap tests and age-appropriate HPV vaccination) for cervical cancer prevention and control. Therefore, even though women receive Pap tests in the course of regular prenatal care, there may be little communication between the women and their provider regarding cervical cancer prevention.
Our findings on the beliefs around perceived causes of cervical cancer such as vaginal trauma, poor feminine hygiene, sex during menstruation, and abortion are similar to the findings of a study conducted among a diverse group of Latinas and non-Latina white women in central, urban Florida [28, 31]. In that study, Mexican women differed significantly from non-Latina white women in their beliefs that sex during a woman’s menstrual period, abortion, and vaginal trauma might cause cervical cancer. Although the women in our study endorsed the biomedical model of cervical cancer, similar to Latinas in urban Florida, they also endorsed cultural causes with moral implications, such as reproductive decisions (i.e., abortion, many pregnancies) [28]. These beliefs have been associated with religious notions of shame or guilt around sexual matters which might result in negative health consequences [32]. Moreover, several studies have found that the Pap test is embarrassing for Mexican women [20, 33, 34]. The causes related to sexual behaviors were ranked as more severe in the results, signifying that these behavioral risk factors are stigmatized in this population. In addition, the fear domain identified in the barriers pile sort points to potential lack of trust with health care providers. Without trust between the patient and the provider, it is less likely that fears or embarrassing feelings about a screening exam will be addressed [35].
Additional structural factors, such as access to health care, scheduling challenges, discrimination, and transportation issues need to be explored in future studies to understand their relationship to lower screening rates found among Mexican women [2]. The clusters for barriers identified in the pile sort exercise could be tested further as constructs in a “barriers to screening” scale instrument. In the perceptual map shown in Fig. 2, women differentiated knowledge, language, and financial barriers from structural barriers (e.g., transportation, access to health insurance). Beliefs surrounding cervical cancer may be similar among Mexican immigrant women in the urban and rural southeastern U.S. However, the perceived structural barriers to accessing health care are greater in rural areas.
For the ranking and agree/disagree questions, women exhibited an average level of competence for the domain, with some variability in competence levels. There remains possible confusion between HIV and HPV, since these items were sorted into the same piles and also ranked high for cervical cancer causes. Mexican women in the Florida study ranked HIV as the second most important cause based on severity and HPV fifth [28]. When combining the pile sort and rank data for causes in the Georgia sample, the categories related to sexual behaviors ranked significantly higher than other causes.
Based on our conversations with participants and observations in area health departments and community health centers, the Mexican immigrant women in the study area have not been receiving information that is relevant to them regarding cancer screening and appropriate follow-up. One study found that Spanish-language cervical cancer pamphlets were not aligned with the learning needs or health literacy levels of Mexican immigrant women [36]. For example, there was incomplete knowledge about the HPV vaccine, but higher endorsement of the belief that the vaccine would prevent HPV, possibly reflecting positive attitudes toward vaccines in general. Information gathered from our study has been incorporated into the Salud es Vida health education intervention toolkit, which is delivered by promotoras, to distinguish myths versus facts regarding cervical cancer risk factors and decrease stigma around sexual matters.
Conclusion
To our knowledge, this study was the first to examine cervical cancer knowledge and beliefs among this vulnerable immigrant population in southeastern Georgia. Mexican women who participated in this study were selected using purposive sampling. Whereas this type of nonprobability sampling limited our ability to generalize study findings, particularly to women who are less accessible and of other ethnic backgrounds, purposive sampling was necessitated by our inclusion criteria. Furthermore, although the cross-sectional study design precluded us from making causal inferences, it was appropriate given the objectives of our exploratory study to gain insights into cancer-related cultural beliefs of Mexican immigrant women due for screening and to collect data for refining data collection instruments for a promotora intervention study. The findings have informed the development of a culturally appropriate intervention to increase cervical cancer screening in this population.
Acknowledgments
This study was supported by the National Cancer Institute, Office of the Director, Grant Number R21 CA 163159. Content presented is solely the responsibility of the authors and does not necessarily represent the official views of National Cancer Institute. The authors wish to acknowledge the contributions of Ms. Andrea Hinojosa of Southeast Georgia Communities Project, the Vidalia onion farms, Claxton Poultry, and the promotoras for helping to facilitate contact with survey participants.
Contributor Information
John S. Luque, Email: jluque@georgiasouthern.edu, Jiann-Ping Hsu College of Public Health, Georgia Southern University, P.O. Box 8015, Hendricks Hall, Statesboro, GA 30460, USA
Yelena N. Tarasenko, Jiann-Ping Hsu College of Public Health, Georgia Southern University, P.O. Box 8015, Hendricks Hall, Statesboro, GA 30460, USA
Jonathan N. Maupin, School of Human Evolution and Social Change, Arizona State University, Tempe, AZ, USA
Moya L. Alfonso, Jiann-Ping Hsu College of Public Health, Georgia Southern University, P.O. Box 8015, Hendricks Hall, Statesboro, GA 30460, USA
Lisa C. Watson, Jiann-Ping Hsu College of Public Health, Georgia Southern University, P.O. Box 8015, Hendricks Hall, Statesboro, GA 30460, USA
Claudia Reyes-Garcia, Jiann-Ping Hsu College of Public Health, Georgia Southern University, P.O. Box 8015, Hendricks Hall, Statesboro, GA 30460, USA.
Daron G. Ferris, GRU Cancer Center, Georgia Regents University, Augusta, GA, USA
References
- 1.Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin. 2014;64(1):9–29. doi: 10.3322/caac.21208. [DOI] [PubMed] [Google Scholar]
- 2.American Cancer Society. Cancer facts and figures for Hispanics/ Latinos 2012–2014. Atlanta: American Cancer Society; 2012. [Accessed 2 Mar 2014]. http://www.cancer.org. [Google Scholar]
- 3.U.S. Preventive Services Task Force. [Accessed 2 Sept 2014];Screening for cervical cancer: clinical summary of US Preventive Services Task Force recommendation. 2012 Mar; AHRQ Publication No. 11-05156-EF-3. http://www.uspreventiveservicestaskforce.org/uspstf11/cervcancer/cervcancersum.htm.
- 4.Tsui J, Saraiya M, Thompson T, Dey A, Richardson L. Cervical cancer screening among foreign-born women by birthplace and duration in the United States. J Women Health. 2007;16(10):1447–57. doi: 10.1089/jwh.2006.0279. [DOI] [PubMed] [Google Scholar]
- 5.Yabroff KR, Lawrence WF, King JC, Mangan P, Washington KS, Yi B, Kerner JF, Mandelblatt JS. Geographic disparities in cervical cancer mortality: what are the roles of risk factor prevalence, screening, and use of recommended treatment? J Rural Health. 2005;21(2):149–57. doi: 10.1111/j.1748-0361.2005.tb00075.x. [DOI] [PubMed] [Google Scholar]
- 6.Scarinci IC, Garcia FA, Kobetz E, Partridge EE, Brandt HM, Bell MC, Dignan M, Ma GX, Daye JL, Castle PE. Cervical cancer prevention: new tools and old barriers. Cancer. 2010;116(11):2531–42. doi: 10.1002/cncr.25065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arcury TA, Quandt SA. Delivery of health services to migrant and seasonal farmworkers. Annu Rev Public Health. 2007;28:345–63. doi: 10.1146/annurev.publhealth.27.021405.102106. [DOI] [PubMed] [Google Scholar]
- 8.Alavanja MC, Hoppin JA, Kamel F. Health effects of chronic pesticide exposure: cancer and neurotoxicity. Annu Rev Public Health. 2004;25:155–97. doi: 10.1146/annurev.publhealth.25.101802.123020. [DOI] [PubMed] [Google Scholar]
- 9.Coronado GD, Thompson B, Koepsell TD, Schwartz SM, McLerran D. Use of Pap test among hispanics and non-hispanic whites in a rural setting. Prev Med. 2004;38(6):713–22. doi: 10.1016/j.ypmed.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 10.Scarinci IC, Bandura L, Hidalgo B, Cherrington A. Development of a theory-based (PEN-3 and health belief model), culturally relevant intervention on cervical cancer prevention among Latina immigrants using intervention mapping. Health Promot Pract. 2012;13(1):29–40. doi: 10.1177/1524839910366416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Han CS, Ferris DG, Waller J, Tharp P, Walter J, Allmond L. Comparison of knowledge and attitudes toward human papillomavirus, HPV vaccine, pap tests, and cervical cancer between US and Peruvian women. J Low Genit Tract Dis. 2012;16(2):121–6. doi: 10.1097/LGT.0b013e31823a05a3. [DOI] [PubMed] [Google Scholar]
- 12.Coughlin SS, Wilson KM. Breast and cervical cancer screening among migrant and seasonal farmworkers: a review. Cancer Detect Prev. 2002;26(3):203–9. doi: 10.1016/s0361-090x(02)00058-2. [DOI] [PubMed] [Google Scholar]
- 13.Fernandez ME, Diamond PM, Rakowski W, Gonzales A, Tortolero-Luna G, Williams J, Morales-Campos DY. Development and validation of a cervical cancer screening self-efficacy scale for low-income Mexican American women. Cancer Epidemiol Biomarkers Prev. 2009;18(3):866–75. doi: 10.1158/1055-9965.EPI-07-2950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee S, O’Neill AH, Ihara ES, Chae DH. Change in self-reported health status among immigrants in the United States: associations with measures of acculturation. PLoS One. 2013;8(10):e76494. doi: 10.1371/journal.pone.0076494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kagawa-Singer M, Dadia AV, Yu MC, Surbone A. Cancer, culture, and health disparities: time to chart a new course? CA Cancer J Clin. 2010;60(1):12–39. doi: 10.3322/caac.20051. [DOI] [PubMed] [Google Scholar]
- 16.Luque JS, Mason M, Reyes-Garcia C, Hinojosa A, Meade CD. Salud es Vida: development of a cervical cancer education curriculum for promotora outreach with Latina farmworkers in rural Southern Georgia. Am J Public Health. 2011;101(12):2233–5. doi: 10.2105/AJPH.2011.300324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Watson-Johnson LC, Bhagatwala J, Reyes-Garcia C, Hinojosa A, Mason M, Meade CD, Luque JS. Refinement of an educational toolkit to promote cervical cancer screening among Hispanic immigrant women in rural southern Georgia. J Health Care Poor Underserved. 2012;23(4):1704–11. doi: 10.1353/hpu.2012.0150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–64. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 19.Wallerstein N, Bernstein E. Freire’s ideas adapted to health education. Health Educ Q. 1988;15:379–94. doi: 10.1177/109019818801500402. [DOI] [PubMed] [Google Scholar]
- 20.Fernandez ME, Gonzales A, Tortolero-Luna G, Williams J, Saavedra-Embesi M, Chan W, Vernon SW. Effectiveness of Cultivando la Salud: a breast and cervical cancer screening promotion program for low-income Hispanic women. Am J Public Health. 2009;99(5):936–43. doi: 10.2105/AJPH.2008.136713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Taylor VM, Coronado G, Acorda E, Teh C, Tu SP, Yasui Y, Bastani R, Hislop TG. Development of an ESL curriculum to educate Chinese immigrants about hepatitis B. J Commun Health. 2008;33(4):217–24. doi: 10.1007/s10900-008-9084-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Romney AK, Weller SC, Batchelder WH. Culture as consensus: a theory of culture and informant accuracy. Am Anthropol. 1986;88(2):313–38. [Google Scholar]
- 23.Chavez LR, Hubbell FA, McMullin JM, Martinez RG, Mishra SI. Structure and meaning in models of breast and cervical cancer risk factors: a comparison of perceptions among Latinas, Anglo women, and physicians. Med Anthropol Q. 1995;9(1):40–74. doi: 10.1525/maq.1995.9.1.02a00030. [DOI] [PubMed] [Google Scholar]
- 24.Hubbell FA, Chavez LR, Mishra SI, Valdez RB. Beliefs about sexual behavior and other predictors of Papanicolaou smear screening among Latinas and Anglo women. Arch Intern Med. 1996;156(20):2353–8. [PubMed] [Google Scholar]
- 25.McMullin JM, De Alba I, Chavez LR, Hubbell FA. Influence of beliefs about cervical cancer etiology on Pap smear use among Latina immigrants. Ethn Health. 2005;10(1):3–18. doi: 10.1080/1355785052000323001. [DOI] [PubMed] [Google Scholar]
- 26.Weller SC. Cultural consensus theory: applications and frequently asked questions. Field Methods. 2007;19:339–68. [Google Scholar]
- 27.U.S. Census Bureau. [Accessed 2 Mar 2014];United States Census. 2010 http://www.census.gov.
- 28.Luque JS, Castaneda H, Tyson DM, Vargas N, Proctor S, Meade CD. HPV awareness among Latina immigrants and Anglo American women in the Southern U.S.: cultural models of cervical cancer risk factors and beliefs. NAPA Bull. 2010;34(1):84–104. doi: 10.1111/j.1556-4797.2010.01053.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Deyo RA, Diehl AK, Hazuda H, Stern MP. A simple language-based acculturation scale for Mexican Americans: validation and application to health care research. Am J Public Health. 1985;75(1):51–5. doi: 10.2105/ajph.75.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ross N, Maupin J, Timura CA. Knowledge organization, categories, and ad hoc groups: folk medical models among Mexican migrants in Nashville. Ethos. 2011;39(2):165–88. [Google Scholar]
- 31.Luque JS, Castaneda H, Tyson DM, Vargas N, Meade CD. Formative research on HPV vaccine acceptability among Latina farmworkers. Health Promot Pract. 2012;13(5):617–25. doi: 10.1177/1524839911414413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guilfoyle S, Franco R, Gorin SS. Exploring older women’s approaches to cervical cancer screening. Health Care Women Int. 2007;28(10):930–50. doi: 10.1080/07399330701615358. [DOI] [PubMed] [Google Scholar]
- 33.Byrd TL, Chavez R, Wilson KM. Barriers and facilitators of cervical cancer screening among hispanic women. Ethn Dis. 2007;17(1):129–34. [PubMed] [Google Scholar]
- 34.Marvan ML, Ehrenzweig Y, Catillo-Lopez RL. Knowledge about cervical cancer prevention and psychosocial barriers to screening among Mexican women. J Psychosom Obstet Gynaecol. 2013;34(4):163–9. doi: 10.3109/0167482X.2013.846904. [DOI] [PubMed] [Google Scholar]
- 35.Sheppard VB, Wang J, Yi B, Harrison TM, Feng S, Huerta EE, Mandelblatt JS. Are health-care relationships important for mammography adherence in Latinas? J Gen Intern Med. 2008;23(12):2024–30. doi: 10.1007/s11606-008-0815-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hunter JL. Cervical cancer educational pamphlets: do they miss the mark for Mexican immigrant women’s needs? Cancer Control. 2005;12(Suppl 2):42–50. doi: 10.1177/1073274805012004S07. [DOI] [PubMed] [Google Scholar]


