Abstract
Background
Mentoring is increasingly recognized as a critical element in supporting successful careers in academic research in medicine and related disciplines, particularly for trainees and early career investigators from underrepresented backgrounds. Mentoring is often executed ad hoc; there are limited programs to train faculty to become more effective mentors, and the few that exist have a dearth of empirical support of their impact.
Methods
In 2013, we recruited 34 faculty from across the U.S. engaged in HIV-related clinical research to participate in a two-day Mentoring the Mentors workshop. The workshop included didactic and interactive content focused on a range of topics, such as mentor-mentee communication, leadership styles, emotional intelligence, understanding the impact of diversity (unconscious bias, microaggressions, discrimination, tokenism) for mentees, and specific tools and techniques for effective mentoring.
Results
Pre- and post-workshop online evaluations documented high rates of satisfaction with the program and statistically significant improvements in self-appraised mentoring skills (e.g. addressing diversity in mentoring, communication with mentees, aligning mentor-mentee expectations), as assessed via a validated mentoring competency tool.
Discussion
This is the first mentoring training program focused on enhancing mentors’ abilities to nurture investigators of diversity, filling an important gap, and evaluation results offer support for its effectiveness. Results suggest a need for refinement and expansion of the program and for more comprehensive, long-term evaluation of distal mentoring outcomes for those who participate in the program.
Keywords: Diversity, Mentoring Training, Underrepresented Minority Populations
Introduction
In times of economic instability and cuts to funding for health sciences and public health infrastructure, there is a pressing and substantial threat to the pipeline of new investigators seeking careers in scientific innovation and discovery. Decreasing availability of secure careers in academic research in light of constricted funding can serve as powerful deterrents to the next generation of investigators considering careers in academic medicine. These forces serve to deepen disparities in the numbers of scientists from underrepresented groups, such as racial and ethnic minorities and those from disadvantaged backgrounds seeking research careers (Ginther, Schaffer et al. 2011).
One critical tool to combat threats to scientific innovation and progress is effective mentoring and encouraging talent amongst early career investigators. Growing evidence documents the benefits of mentoring on productivity, job satisfaction, and quality of life (Eby, Allen et al. 2008, Stamm and Buddeberg-Fischer 2011). However, most experienced investigators who are positioned to provide mentoring have not participated in formal training in mentoring techniques. Rather, most academic faculty are expected to mentor without structure or training and often develop ad hoc methods and approaches that vary in consistency, intensity, and effectiveness (Straus, Johnson et al. 2013). With increased recognition of the importance of mentoring in academic research, some formal efforts are underway to develop and evaluate mentor training curricula with the goal of improving relevant outcomes among mentors and mentees, and to measure and monitor improvements in mentoring competence (Huskins, Silet et al. 2011, Fleming, House et al. 2013). The literature on mentoring offers some effective strategies and perspectives, including the importance of aligning mentor and mentee expectations and roles early in the mentoring relationship (Pfund, Maidl Pribbenow et al. 2006, Huskins, Silet et al. 2011, Pfund, House et al. 2013). However, there is paucity of empirical data on the relative efficacy of different mentor training methods and a gap in the literature on effective mentoring training programs for researchers mentoring investigators from underrepresented groups.
Through an National Institutes of Health (NIH)-funded grant awarded to the University of California, San Francisco (UCSF), a robust “Mentoring the Mentors” workshop focused on training mid-career and senior HIV investigators across the U.S. in tools and techniques specific to mentoring early stage investigators (ESIs) of diversity was developed and held in September 2012 at UCSF (Gandhi, Fernandez et al. 2014). A second workshop was conducted in October 2013, with each workshop drawing about 30 HIV faculty from approximately 15 institutions across the U.S. for intensive mentoring training. The first workshop yielded qualitative data showing improvement in mentoring capability, self-efficacy scores around mentoring and an improved understanding of the issues facing ESIs of diversity in academia (Gandhi, Fernandez et al. 2014). The curriculum included adapted elements of other mentor training programs (Johnson, Subak et al. 2010) and is situated within Social Cognitive Career Theory (SCCT) (Lent, Brown et al. 1994) an adaptation of Social Cognitive Theory (SCT) (Bandura 1986). SCCT applies the constructs of self-efficacy to professional choice-making, skill-development, and decision-making about career paths (short-term and long-term). In this approach, self-efficacy and outcome expectations interact to promote or deter activity, which can dictate level of academic productivity and success. We now report the results from the second training workshop for HIV researchers interested in mentoring ESIs of diversity, in which a validated measure of assessing mentoring competency (Fleming, House et al. 2013) was administered before and after the training.
Methods
Participants
Faculty participants were recruited from Center for AIDS Research (CFAR) programs nationwide, from major HIV clinical trial networks, and using listservs geared towards HIV researchers. Recruitment efforts targeted mid-career and senior-level investigators with active mentoring responsibilities or interest in developing them.
Curriculum
The 2-day workshop at UCSF held October 7–8, 2013 focused on a series of topics designed to enhance mentoring techniques in general (definitions and formalization of mentoring, communication strategies, consistent use of individual development plans, setting goals and expectations for the mentor-mentee relationship, time-management for mentor and mentee, work-life balance, mentor and mentee evaluation tools, leadership styles etc.), as well as topics specifically related to diversity (unconscious bias, microaggressions, diversity supplements to NIH-sponsored grants and other minority-focused funding opportunities, resiliency, and self-awareness), via didactic presentations, break-out sessions, role-playing and small-group brainstorming sessions. The operationalization of diversity largely followed the guidance from the United States’ Institutes of Health (NIH), which provides categories of diversity based on whether a group is underrepresented in science across disciplines. This includes individuals from racial and ethnic groups that are not well represented in science, persons with disabilities, and those from disadvantaged backgrounds. We extended this definition to include diversity along other dimensions, including gender identity, sexual orientation, and religious or cultural views. Toward the end of the training curriculum, we implemented a Mentor Consultation Clinic, in which the participants broke into groups of 5–6 and provided input on one member’s current mentoring challenge. In this exercise, participants were instructed to apply the training content (e.g., active listening, awareness of bias) to a specific mentoring situation before offering advice and recommendations. More details on the workshop, including the agenda, are found at the following link: UCSF Mentoring the Mentors Workshop October 2013.
Evaluation
Participants completed online assessments prior to attending the training and again two weeks after the workshop. The baseline assessment included background and demographic questions and the validated Mentoring Competency Assessment tool (MCA)(Fleming, House et al. 2013). The MCA is a 26-item skills inventory that solicits self-appraisals of confidence in mentoring in six domains: maintaining effective communication (alpha = .62), aligning expectations (alpha = .76), assessing understanding (alpha = .72), addressing diversity (alpha = .65), fostering independence (alpha = .91), and promoting professional development (alpha = .80). The post-workshop assessment also asked participants to rank the importance of different components of the mentor training workshop, and solicited general, open-ended feedback on the program. Student t-tests compared means of attendees’ self-ratings of mentoring skills on all six domains of the MCA pre-and-post workshop. The p-values were not corrected for multiple outcomes for this exploratory analysis.
Results
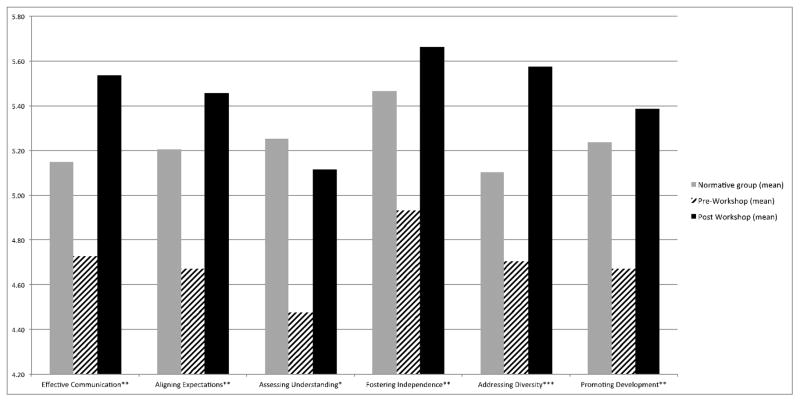
Recruitment efforts resulted in 34 individuals from 17 institutions attending the two-day workshop; distributions across gender, race/ethnicity, and academic discipline are presented in Table 1. We achieved a 100% evaluation completion rate for both the pre- and post-workshop survey with a US$5 gift card incentive. Numeric ratings of the workshop were favorable, with 71% rating the overall experience as excellent, 21% as very good, and 6% as good; 95% reported that they would be likely to recommend this program to colleagues. Based on post-workshop responses, Table 2 lists the workshop’s mentor-training topics in order of participant-reported importance, with communication strategies between mentor-mentee listed at the top and training on diversity listed as 5th in importance. Statistically-significant increases in the means of attendees’ self-ratings of mentoring skills after the workshop were demonstrated on all six domains of the MCA. Figure 1 demonstrates attendees’ pre-workshop means and post-workshop means for a variety of mentoring skills. As a reference, MCA scores from a normative group of senior mentors drawn from a national Clinical and Translational Science Award (CTSA) sample are shown (Fleming, House et al. 2013). Of note is that the normative scores for the CTSA sample are higher than our participants’ pre-workshop scores, which likely reflects that the CTSA control group had a greater number of senior faculty than our sample. However, our participants’ MCA scores in all domains, including “addressing diversity”, surpassed the CTSA group’s scores upon completion of our mentoring training workshop.
Table 1.
Participant characteristics (N=34)
| N (%) | ||
|---|---|---|
| Gender | Female | 24 (73%) |
| Male | 9 (27%) | |
| Race/Ethnicity | White | 26 (84%) |
| Black | 4 (13%) | |
| Hispanic | 2 (6%) | |
| Academic Discipline within HIV | Medicine | 12 (35%) |
| Social/Behavioral Science | 7 (21%) | |
| Public Health | 4 (12%) | |
| Nursing | 3 (9%) | |
| Epidemiology | 7 (21%) | |
| Basic science | 1 (3%) | |
| Academic Rank | Assistant Professor | 5 (15%) |
| Associate Professor | 14 (42%) | |
| Professor | 13 (39%) | |
| Any prior mentor training | Yes | 22 (65%) |
| Number of mentees as primary mentor | 0 | 2 (6%) |
| 1–2 | 15 (44%) | |
| 3–5 | 12 (35%) | |
| >5 | 5 (15%) | |
| Number of mentees as secondary mentor | 0 | 3 (9%) |
| 1–2 | 13 (38) | |
| 3–5 | 11 (32%) | |
| >5 | 7 (21%) | |
| Professional Activities (%) | Mean % (range) | |
| Research | 58 (10–90) | |
| Teaching | 12 (0–41) | |
| Clinical | 18 (0–52) | |
| Administration | 20 (2–90) | |
| Mentoring | 17 (5–40) |
Table 2.
Ranked importance of mentor training domains
| Importance* | Mentor Training Domain |
|---|---|
| 1 | Communication strategies with mentees |
| 2 | Leadership styles, self-awareness, and emotional intelligence |
| 3 | Specific tools and techniques for mentoring |
| 4 | Improving mentee productivity |
| 5 | Training on diversity and barriers faced by underrepresented groups |
| 6 | Time management techniques for both mentor and mentee |
| 7 | Funding mechanisms for mentoring |
| 8 | Mentoring literature |
| 9 | Life-work balance |
In increasing order of rated importance
Figure 1.
Pre and post workshop Mentor Competency Assessment scores
Notes: Difference between pre- and post-workshop means designated as follows: * = p <.05; ** = p < .01; *** = p< .001
Discussion
Shortly following attendance at our two-day mentor-training workshop for HIV researchers, participants gave favorable ratings of the experience and reported statistically significant increases in six domains of mentoring competency - including communication, aligning expectations, assessing understanding, addressing diversity, fostering independence, and promoting professional development - following the training. When ranking the training components of the program, strategies to improve communication and leadership skills were rated as most important by participants, followed by demonstration and explanation of specific tools and techniques for mentoring.
To our knowledge, this is the first mentor-training program for academic researchers focused on fostering ESIs of diversity, with specific training components on unconscious bias, microaggressions towards underrepresented groups, and communication strategies to address these barriers. This unique mentoring training program, for the first time, also demonstrated improvements on a validated and self-reported measure of assessing mentoring competency. Many academic institutions and funding agencies have prioritized increasing the diversity of their faculty, trainees, and staff. However, progress toward this goal has been slow, with historically low rates of representation amongst U.S.-based faculty of racial and ethnic minorities,(Koenig 2009) especially at higher levels of academic rank, and lower success rates in obtaining extramural grant funding among investigators from minority backgrounds (Ginther, Schaffer et al. 2011). Mentor training with a focus on issues of particular relevance to underrepresented groups may be a proactive and important approach to improve recruitment and retention of investigators from diverse backgrounds.
While the outcomes of this program evaluation are encouraging, we recognize the limits of the data. The participants were self-selected volunteers and thus may have been highly motivated to seek improvements in their mentoring techniques. Without a control condition of similar participants who did not attend the training, results should be considered in that context. Our sample also included a greater number of female than male participants (73% and 27% respectively), an imbalance that might limit generalizability. Further, it is not clear whether self-reported improvements in mentoring competency are associated with actual improvements in mentor effectiveness or more distal outcomes, such as parameters of mentee success. Our two-week follow-up timeframe was largely practical by design and thus does not provide insights into longer-term impacts of the program. We plan to develop future mentor training programs with formal evaluation monitoring that will include documentation of subsequent mentoring efforts, tracking of numbers and types of mentees, submission and outcomes of mentees’ funding submissions (e.g., intramural pilot awards, applying for and being awarded mentored career development awards (K series) and independent research grants (R series) from the NIH), mentee satisfaction and mentee publications. Likewise, outcome data documenting perceived effectiveness of the mentors from the perspective of those whom they mentor is necessary to more fully evaluate the effects of a comprehensive mentor-training program. The authors plan to apply for additional grants to design a robust longitudinal mentoring program for HIV researchers with prospective evaluation and monitoring of mentor and mentee outcomes to address this gap.
Despite these limitations, we describe for the first time improvements in mentoring competency in six domains by faculty attending a robust mentoring training program, now in its second year, focused on nurturing ESIs of diversity. This innovative mentoring program fills an important gap in the HIV researcher community and should be adapted to other disciplines to hopefully help attract, engage, and retain investigators from underrepresented groups in academia. Further study of the long-term implications of mentoring training with longitudinal reinforcement and assessment of mentee outcomes is needed.
Acknowledgments
The authors wish to thank the investigators who participated in the workshop described in this paper and our colleagues who helped develop or facilitate the curriculum. This paper was supported by the following grants from the National Institutes of Health: R24MH094274 (Gandhi, P.I.), K24MH087220 (Johnson, P.I.), and K24DA037034 (Johnson, P.I.).
References
- Bandura A. Social foundations of thought and action: A social cognitive theory. Prentice-Hall, Inc; Englewood Cliffs, NJ, US: 1986. [Google Scholar]
- Eby LT, Allen TD, Evans SC, Ng T, Dubois D. Does Mentoring Matter? A Multidisciplinary Meta-Analysis Comparing Mentored and Non-Mentored Individuals. J Vocat Behav. 2008;72(2):254–267. doi: 10.1016/j.jvb.2007.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleming M, House S, Hanson VS, Yu L, Garbutt J, McGee R, Kroenke K, Abedin Z, Rubio DM. The Mentoring Competency Assessment: Validation of a New Instrument to Evaluate Skills of Research Mentors. Acad Med. 2013;88(7):1002–1008. doi: 10.1097/ACM.0b013e318295e298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gandhi M, Fernandez A, Stoff DM, Narahari S, Blank M, Fuchs J, Evans CH, Kahn JS, Johnson MO. Development and Implementation of a Workshop to Enhance the Effectiveness of Mentors Working with Diverse Mentees in HIV Research. AIDS Res Hum Retroviruses. 2014;30(8):730–737. doi: 10.1089/aid.2014.0018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginther DK, Schaffer WT, Schnell J, Masimore B, Liu F, Haak LL, Kington R. Race, ethnicity, and NIH research awards. Science. 2011;333(6045):1015–1019. doi: 10.1126/science.1196783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huskins WC, Silet K, Weber-Main AM, Begg MD, Fowler VG, Jr, Hamilton J, Fleming M. Identifying and aligning expectations in a mentoring relationship. Clin Transl Sci. 2011;4(6):439–447. doi: 10.1111/j.1752-8062.2011.00356.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MO, Subak L, Brown J, Lee K, Feldman M. An Innovative Program to Train Health Sciences Researchers to be Effective Clinical and Translational-Research Mentors. Academic Medicine. 2010;85(3):484–489. doi: 10.1097/ACM.0b013e3181cccd12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenig R. U.S. higher education. Minority retention rates in science are sore spot for most universities. Science. 2009;324(5933):1386–1387. doi: 10.1126/science.324_1386a. [DOI] [PubMed] [Google Scholar]
- Lent RW, Brown SD, Hackett G. Toward a unifying social cognitive Theory of career and academic interest, choice, and performance. Journal of Vocational Behavior. 1994;45:79–122. [Google Scholar]
- Pfund C, House S, Spencer K, Asquith P, Carney P, Masters KS, McGee R, Shanedling J, Vecchiarelli S, Fleming M. A research mentor training curriculum for clinical and translational researchers. Clin Transl Sci. 2013;6(1):26–33. doi: 10.1111/cts.12009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfund C, Maidl Pribbenow C, Branchaw J, Miller Lauffer S, Handelsman J. Professional skills. The merits of training mentors. Science. 2006;311(5760):473–474. doi: 10.1126/science.1123806. [DOI] [PubMed] [Google Scholar]
- Stamm M, Buddeberg-Fischer B. The impact of mentoring during postgraduate training on doctors’ career success. Med Educ. 2011;45(5):488–496. doi: 10.1111/j.1365-2923.2010.03857.x. [DOI] [PubMed] [Google Scholar]
- Straus SE, Johnson MO, Marquez C, Feldman MD. Characteristics of successful and failed mentoring relationships: a qualitative study across two academic health centers. Acad Med. 2013;88(1):82–89. doi: 10.1097/ACM.0b013e31827647a0. [DOI] [PMC free article] [PubMed] [Google Scholar]