Abstract
Study Design
Controlled laboratory study
Objectives
To compare hip and knee kinematics and pain during a single limb squat between 3 movement conditions (‘usual’, ‘exaggerated’ dynamic knee valgus, ‘corrected’ dynamic knee valgus) in females with patellofemoral pain.
Background
Altered kinematics (increased hip adduction, hip medial rotation, knee abduction, and knee lateral rotation, collectively termed “dynamic knee valgus”) have been proposed to contribute to patellofemoral pain, however cross-sectional study designs prevent interpreting a causal link between kinematics and pain.
Methods
Twenty females with patellofemoral pain who demonstrated observable dynamic knee valgus performed single limb squats under ‘usual’, ‘exaggerated’, and ‘corrected’ movement conditions. Pain during each condition was assessed using a 0-100 mm visual analog scale. Hip and knee frontal and transverse plane angles at peak knee flexion and pain levels were compared using repeated measures, 1-way ANOVAs. Within condition associations between kinematic variables and pain were determined using Pearson correlation coefficients.
Results
In the ‘exaggerated’ compared to the ‘usual’ condition, increases were detected in hip medial rotation (mean +/-SD, 5.8±3.2°, P<.001), knee lateral rotation (5.5±4.9°, P<.001), and pain (8.5±10.8mm, P=.007). In the ‘corrected’ compared to the ‘usual’ condition, decreases were detected in hip adduction (3.5±3.7°, P=.001) and knee lateral rotation (1.6±2.8°, P=.06; however, average pain was not decreased (1.2±14.8mm, P=1.0). Pain was correlated with knee lateral rotation in the ‘usual’ (r=−0.47, P=.04) and ‘exaggerated’ (r=−0.49, P=.03) conditions. In the ‘corrected’ condition, pain was correlated with hip medial rotation (r=0.44, P=.05) and knee adduction (r=0.52, P=.02).
Conclusion
Avoiding dynamic knee valgus may be an important component of rehabilitation programs in females with patellofemoral pain, as this movement pattern is associated with increased pain.
Keywords: anterior knee pain, dynamic knee valgus, hip, knee, single-limb squat
INTRODUCTION
Altered movement patterns have been suggested as a contributing factor to a variety of musculoskeletal pain conditions including patellofemoral pain (PFP).15,36,38,46 A recently proposed theory34 linking lower limb movement patterns and PFP describes a collection of altered kinematics that includes increased femoral (hip) adduction and medial rotation, increased knee valgus (abduction), and increased lateral tibial (knee) rotation, collectively termed “dynamic knee valgus”. Because the patella is tethered between the femur and tibia, these altered hip and knee kinematics theoretically increase the quadriceps angle (Q-angle) and subsequent lateral forces on the patellofemoral joint, which lead to reduced patellofemoral joint contact area and increased patellofemoral joint stress.34
Evidence exists to support the relationship between femoral and tibial alignment and patellofemoral joint mechanics under static conditions. For example, increased knee abduction (via manipulating quadriceps attachments) has been linked to increased patellofemoral joint stress.20,35 Similarly, increased medial femoral rotation with respect to the tibia has been shown to be related to decreased patellofemoral contact area12,17,23,24,40 and increased patellofemoral joint stress.12,23,24
Despite the evidence linking static femoral and tibial alignment and patellofemoral mechanics, the link between dynamic knee valgus during movement and pain in people with PFP has not been clearly established. Several authors have reported altered kinematics such as increased hip adduction,32,39,47 increased hip medial rotation,32,42,50 increased knee abduction,39 and increased knee lateral rotation47 in females with PFP compared to pain-free subjects, however the cross-sectional nature of these studies prevents the interpretation of a causal link between kinematics and pain. Prospective studies have identified various biomechanical risk factors for PFP such as increased hip medial rotation,6 increased knee abduction moment,29 and increased knee abduction impulse,44 but no studies have directly manipulated kinematics during a functional task and measured the subjects’ subsequent pain response.
If dynamic knee valgus plays a role in the mechanism of PFP via altered hip and knee kinematics, then movement patterns that increase dynamic knee valgus on observation should increase measurable kinematic faults and those that decrease dynamic knee valgus on observation should decrease measurable kinematic faults. Furthermore, altered kinematics should be more readily detected in people who demonstrate observable dynamic knee valgus during a weight bearing task (ie, knee moves medially, inducing apparent valgus/abduction). With respect to pain, if symptoms are the result of cumulative microtrauma induced by repeated movements in a specific direction38 then increased dynamic knee valgus during a squatting movement should cause an increase in pain and decreased dynamic knee valgus should cause a decrease in pain.
We chose to test these hypotheses in a sample of females with PFP, who demonstrated observable dynamic knee valgus during a single limb squat task. The single limb squat is a pain-provoking activity for people with PFP; it imposes mechanical demands that could induce dynamic knee valgus (eg, small base of support that requires control of the lower extremity in the transverse and frontal planes), and it is commonly used in studies investigating lower extremity kinematics in people with PFP.25,41,47,48
The purpose of this study was to compare hip and knee kinematics and pain during a single limb squat between 3 movement conditions (usual, exaggerated dynamic knee valgus, corrected dynamic knee valgus). We hypothesized that, compared to the usual condition, hip adduction, hip medial rotation, knee abduction, and knee lateral rotation angles would be increased in the exaggerated condition and decreased in the corrected condition. In addition, pain was expected to increase in the exaggerated condition, decrease in the corrected condition, and positively correlate with hip adduction, hip medial rotation, knee abduction, and knee lateral rotation angles in all 3 conditions.
METHODS
Subjects
Twenty females with chronic PFP, who were between 18 and 40 years of age, participated (mean +/− SD age: 22.4±4.3 years, height: 167.2±6.5 cm, body mass: 62.5±7.6 kg). Sample size was based on published data47 comparing kinematics in females with and without PFP. The number of subjects needed to achieve a power level of .80 with an alpha level of .05 ranged from 13 to 35 per group.10 Because this was a within-subjects design, sample size was estimated more liberally at 20 subjects per group.
Only females were studied due to the greater prevalence of PFP in females13,45 and documented sex differences in lower extremity kinematics.8,14,19 Chronic PFP was defined as pain located at the patellofemoral articulation (behind or around the patella) of at least 2 months duration.22 The average pain level during the previous week had to be at least 3 on an 11 point scale (0 represents no pain, 10 represents severe pain) and pain had to be elicited with at least 2 of the following provocation tests: resisted isometric quadriceps contraction performed at approximately 10° of knee flexion, squatting, prolonged sitting, and stair ascent or descent.28 An additional inclusion criterion was the presence of observable dynamic knee valgus (defined and described in the screening exam procedures) during a single limb squat test. Subjects were excluded if their body mass index was greater than 30 kg/m2. Additional exclusion criteria were: a history (or current report) of knee ligament, tendon, or cartilage injury, traumatic patellar dislocation, patellar instability, prior knee surgery, known pregnancy, neurological involvement that would influence coordination or balance during movement testing, and the absence of observable dynamic knee valgus. Subjective history, including verbal numeric pain rating, was obtained via telephone or in person prior to the clinical screening examination.
Procedures
This study was approved by the Institutional Review Board at Saint Louis University. Informed consent was obtained and the rights of the subjects were protected. To confirm that all inclusion and exclusion criteria were met, subjects underwent a clinical screening examination of the knee joint by the principal investigator (a physical therapist with 24 years of experience). Palpation was performed to rule out pain originating from the patellar tendon, quadriceps tendon, tibiofemoral joint, meniscii, or synovial plicae. Subjects completed a visual analog scale (VAS)7 to confirm the presence of pain in response to the 5 provocation tests. The VAS was a 100 mm line with a left anchor of “no pain” and a right anchor of “worst imaginable pain.” For the visual assessment of dynamic knee valgus, subjects performed a single limb squat on their involved (or most painful) limb. Subjects were instructed to keep the trunk upright and arms out to the side at 90° of shoulder abduction. After several practice trials, approximately 5 trials were observed to determine the presence or absence of dynamic knee valgus. If in the majority of trials, based in visual observation, the frontal plane knee angle (abduction) increased by 10° or more during the descent phase of the squat, the subject was classified as having “observable dynamic knee valgus”.
Intrarater and interrater reliability of observable dynamic knee valgus was determined in a separate study by analyzing videos of 30 people performing a single limb squat on 2 occasions. Participants were classified as “dynamic knee valgus” or “no dynamic knee valgus” according to the above criterion. Using the Kappa coefficient, intrarater reliability for the classification made by the principal investigator was .87, while interrater reliability (principal investigator and another rater) on the first testing occasion was .74. Validity of the observable dynamic knee valgus classification was determined by comparing the observed classification to a classification based on the 2-dimensional knee valgus angle (10° cut off) measured from the same videos. Percent agreement between the observed and quantified classifications was 90% with a Kappa value of .85.
If inclusion criteria were met, the subject returned on a different day to complete the testing procedures. Kinematic data were obtained using an 8-camera, 3-dimensional motion analysis system (Vicon, Oxford Metrics LTD. Oxford, England) sampling at 120 Hz. Subjects wore their own running shoes, and all subjects denied wearing orthotic inserts. Retro-reflective markers were placed on the skin of the lower limbs as previously described.18 Thermoplastic shells with 4 attached markers were placed on the lateral mid thighs and lateral mid shanks. Individual tracking markers were placed over the second sacral vertebra and bilaterally on the iliac crest, anterior superior iliac spine, calcaneus, lateral midfoot, and anterior midfoot. Calibration markers were placed bilaterally on the greater trochanter, medial and lateral femoral epicondyle, medial and lateral malleolus, and 1st and 5th metatarsal heads. Following marker placement, a static standing trial was collected during which subjects were instructed to stand facing straight ahead with feet hip-width apart. Calibration markers were removed after the static trial.
Subjects performed unilateral squats on their involved limb. Subjects were instructed to keep their trunk upright, keep their arms out to the side, and bend their knee to at least 60° (visually confirmed by investigator), however no instructions were given to keep the knee from extending forward beyond the toes. Subjects were instructed to complete each squat (from start of knee flexion back to full knee extension) in 4 seconds.47 Subjects were allowed several practice trials to become comfortable with the task. The squat was performed under 2 additional conditions, the order of which was counterbalanced: 1) exaggeration of dynamic knee valgus, and 2) avoidance (correction) of dynamic knee valgus. For the exaggerated condition, subjects were instructed to “let your knee fall in” (medially) during the descent phase of the squat. For the corrected condition, subjects were instructed to “keep your knee over the middle of your foot (don’t let your knee fall in)” during the descent phase of the squat. The exaggerated and corrected conditions were demonstrated first, and subjects were allowed several practice trials to get accustomed to the movement. The terms ‘exaggerated’ and ‘corrected’ were not verbalized to subjects to prevent bias in pain assessment. Three repetitions of each movement condition (usual, exaggerated, corrected) were recorded, and the speed of the squat cycle was calculated for each trial. A squat cycle was defined as the period between the start of knee flexion and the return to full knee extension. Subjects completed a VAS after each condition to rate their average pain during that particular condition.
Using Visual3D™ software (C-Motion, Inc., Rockville, MD, USA) the marker trajectories were low-pass filtered using a fourth-order Butterworth filter with a 6 Hz cutoff frequency. A 6-degrees-of-freedom model incorporated the pelvis, thigh, shank and foot. For the pelvis the CODA model (Charnwood Dynamics Ldt., UK) was used. The frontal plane for the thigh was defined by the hip joint center2 and the 2 femoral epicondyle markers. The frontal plane for the shank was defined by the 2 femoral epicondyle markers and the midpoint of the malleoli markers. The frontal plane of the foot was defined by the 2 malleolus markers and the projection on the floor of the 2 malleolus markers. For each segment, the local coordinate system was located at the proximal endpoint. The frontal plane defined the orientation of the x axis (flexion-extension). The z axis (medial/lateral rotation) passed through each segment’s proximal and distal endpoints. The y-axis (abduction/adduction) was oriented orthogonal to both x and z axes.
Three dimensional hip and knee angles were calculated and expressed in the reference frame of the proximal segment, with positive values representing flexion, adduction, and medial rotation. For each trial, hip and knee angles at the time of peak knee flexion were obtained. The time of peak knee flexion was chosen based on pilot data which showed that the time of peak knee flexion was coincident (within 1-2 samples) with the time of peak knee extensor moment, a point of peak patellofemoral joint stress.1 Hip and knee angles were averaged over 3 trials for each movement condition.
Statistical Analysis
To estimate the within-session error of the kinematic variables, to be used as the threshold for evaluating the differences in kinematics across conditions, trial-to-trial variability of hip and knee frontal and transverse plane angles was determined by calculating the intraclass correlation coefficient (ICC(3,1)) and the standard error of measurement (SEM) across the 3 trials.
Differences in dependent measures across conditions were compared using repeated measures, 1-way ANOVAs. Post-hoc comparisons using a Bonferroni correction were made between the exaggerated and usual conditions, and between the corrected and usual conditions. Primary dependent measures included hip and knee frontal and transverse plane angles and pain (VAS scores). Because the amount of knee flexion and the speed of the squat were potential confounding variables, secondary dependent measures of peak knee flexion angle and squat cycle time also were compared between conditions. Pearson correlation coefficients were calculated to determine the relationships between pain and hip and knee angles in each of the 3 conditions. The alpha level was 0.05 (2-tailed) for all statistical tests.
RESULTS
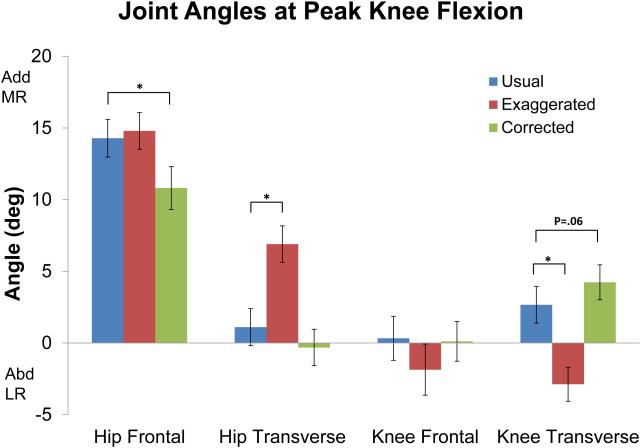
Trial-to-trial variability (ICC3,1 (SEM)) of the kinematic measures ranged from 0.81 (3.5°) to 0.98 (1.0°) (TABLE 1). In the exaggerated condition compared to the usual condition, subjects demonstrated increased hip medial rotation (P<.001) and increased knee lateral rotation (P<.001) at the time of peak knee flexion (TABLE 2, FIGURE). Pain also was increased in the exaggerated condition compared to the usual condition (P=.007). In the corrected condition compared to the usual condition, subjects demonstrated decreased hip adduction (P=.001) and decreased knee lateral rotation (P=.06) (TABLE 2, FIGURE). There was no difference in pain between the corrected and usual conditions. There were no differences in peak knee flexion angle or speed of squat cycle between any of the conditions (TABLE 2).
TABLE 1.
Trial-to-trial variability of hip and knee angles at peak knee flexion.
| ICC(3,1) | SEM(°) | ||
|---|---|---|---|
| Hip | Frontal | 0.89 | 2.0 |
| Transverse | 0.95 | 1.3 | |
| Knee | Sagittal | 0.81 | 3.5 |
| Frontal | 0.98 | 1.0 | |
| Transverse | 0.94 | 1.4 |
Abbreviations: ICC, intraclass correlation coefficient; SEM, standard error of measurement, SEM = where σ is the pooled standard deviation of the 3 trials.
TABLE 2.
Pain and Kinematic Variables across Movement Conditions
| Condition | Comparison | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| Usual (n=20) |
Exaggerated (n=20) |
Corrected (n=20) |
Usual-Exaggerated | Usual-Corrected | ||||||
|
|
||||||||||
| Angle at Peak Knee Flexion |
Mean (SD) | Mean (SD) | Mean (SD) | Difference (SD) |
Confidence Interval*† |
P† | Difference (SD) |
Confidence Interval*† |
P† | |
| Hip Angle (°) | Frontal | 14.3 (5.9) | 14.8 (5.7) | 10.8 (6.7) | −0.5 (4.7) | −3.2, 2.2 | 1.0 | 3.5 (3.7) | 1.3-5.6 | .001 |
| Transverse | 1.1 (5.8) | 6.9 (5.7) | −0.3 (5.7) | −5.8 (3.2) | −7.7, -3.9 | <.001 | 1.4 (3.3) | −0.5, 3.4 | .21 | |
| Knee Angle (°) | Frontal | 0.3 (6.9) | −1.9 (8.0) | 0.1 (6.2) | 2.2 (4.2) | −0.2, 4.6 | .09 | 0.2 (1.9) | −0.9, 1.3 | 1.0 |
| Transverse | 2.7 (5.7) | −2.9 (5.3) | 4.2 (5.5) | 5.6 (4.9) | 2.7, 8.4 | <.001 | −1.5 (2.8) | −3.1, 0.05 | .06 | |
| Sagittal | 70.0 (7.5) | 70.3 (8.3) | 66.9 (8.5) | −0.3 (6.4) | −4.0, 3.4 | 1.0 | 3.1 (7.4) | −1.4, 7.4 | .26 | |
| Squat Cycle Time (sec) | 3.7 (0.9) | 3.7 (0.8) | 4.0 (0.9) | 0.005 (0.6) | −0.3, 0.3 | 1.0 | −0.3 (0.8) | −0.7, 0.2 | .56 | |
| Pain VAS (mm) | 28.3 (18.2) | 36.8 (19.5) | 27.1 (20.3) | −8.5 (10.8) | −14.8, −2.1 | .007 | 1.2 (14.8) | −7.5, 9.9 | 1.0 | |
Positive angle values are flexion, adduction, and medial rotation
95% confidence interval for the difference between conditions
Repeated measures, 1-way ANOVA, post-hoc pair-wise comparisons, 2 tailed, Bonferroni corrected (α=0.05)
Abbreviation: VAS, visual analog scale (0-100 mm)
FIGURE.
Hip and knee frontal and transverse plane angles at peak knee flexion. Abbreviations: Add, Adduction; MR, Medial Rotation; Abd, Abduction; LR, Lateral Rotation. Error bars represent 1 standard error. *indicates significant pair-wise comparisons using repeated measures, 1-way ANOVA, P<.05, Bonferroni corrected, 2-tailed.
In the usual and exaggerated conditions, increased pain was associated with increased knee lateral rotation (usual: r=−0.47, P=.04; exaggerated: r=−0.49, P=.03), while in the corrected condition, increased pain was associated with increased hip medial rotation (r=0.44, P=.05) and knee adduction (r=0.52, P=.02) (TABLE 3).
TABLE 3.
Association between Pain and Hip and Knee Angles at Peak Knee Flexion during a single leg squat*
| Condition |
|||
|---|---|---|---|
| Usual (n=20) | Exaggerated (n=20) | Corrected (n=20) | |
|
|
|||
|
|
|||
| Pain-Hip Frontal | .01 (.98) | −.25 (.28) | −.05 (.85) |
| Pain-Hip Transverse | .15 (.52) | .32 (.17) | .44 (.05)** |
| Pain-Knee Frontal | .20 (.39) | .16 (.50) | .52 (.02)*** |
| Pain-Knee Transverse | −.47 (.04)**** | −.49 (.03)**** | −.07 (.79) |
Abbreviation: VAS, visual analog scale
Data are Pearson correlation coefficients and related P-values
Increased pain associated with increased hip medial rotation
Increased pain associated with increased knee adduction
Increased pain associated with increased knee lateral rotation
DISCUSSION
We hypothesized that, compared to the usual condition, hip adduction, hip medial rotation, knee abduction, and knee lateral rotation angles would be increased in the exaggerated condition and decreased in the corrected condition. In addition, pain was expected to increase in the exaggerated condition, decrease in the corrected condition, and positively correlate with the amount of hip adduction, hip medial rotation, knee abduction, and knee lateral rotation angles in all 3 conditions.
As expected, hip medial rotation, knee lateral rotation, and pain were increased in the exaggerated condition. These findings support the proposed theory that transverse plane components of dynamic knee valgus may contribute to PFP.34 Cadaver studies have demonstrated that increased medial femoral rotation with respect to the tibia decreases contact area12,17,23,24,40 and increases stress12,23,24 at the patellofemoral joint, while in humans, knee lateral rotation during a valgus squat has been associated with lateral patellar translation in healthy subjects31 and reduced patellofemoral joint contact area in people with PFP.40 While the current study did not quantify patellofemoral alignment, contact area, or stress, it is the first study, to our knowledge, that directly tested the effect of increasing dynamic knee valgus on pain in people with PFP. Pain was correlated with knee lateral rotation in the usual and exaggerated conditions, suggesting that avoiding excessive knee lateral rotation during weight bearing tasks may be an important component of a rehabilitation program for this group of people with PFP.
In the frontal plane, despite the appearance of excessive frontal plane movement of the femur and tibia (ie, on observation, knee appeared to move medially in the frontal plane), neither the hip adduction angle nor the knee abduction angle was increased in the exaggerated condition compared to the usual condition. This finding suggests that increased dynamic knee valgus noted on observation, may be primarily a consequence of the 2-dimensional nature of observational angles.48 It is also possible that in this population, hip adduction was already greater than normal in the usual condition, as has been reported in a study comparing individuals with PFP and control subjects,47 such that there was no more available motion in the frontal plane. Pain was not correlated with hip or knee frontal plane angles during the usual or exaggerated conditions (TABLE 3), suggesting that frontal plane variables make less of a contribution to pain than transverse plane variables.
In the corrected condition compared to the usual condition, hip adduction was decreased by 3.5 ± 3.7° (P=.001) and knee lateral rotation was decreased by 1.5 ± 2.8° (P=.06). These findings suggests that as a group, subjects altered somewhat different hip kinematic components in the exaggerated versus corrected conditions, even though the instructions for the corrected condition were basically a negation of those for the exaggerated condition (eg, “don’t let your knee fall in” versus “let your knee fall in”). It might be that, at the hip, correcting transverse plane motion is more difficult than correcting frontal plane motion. Previous authors have reported strength deficits in the hip lateral rotator muscles in females with PFP.4,9,21,37,43 As such, it is possible that hip lateral rotator weakness prevented a greater reduction in hip medial rotation in the corrected condition. Alternatively, it is possible that subjects were able to reduce medial rotation of the femur segment, but this was accompanied by forward rotation of the contralateral pelvis such that there was no net change in hip joint medial rotation. Analysis of segmental kinematics would be important to incorporate in future studies.
Contrary to our hypothesis, pain was not decreased in the corrected compared to the usual condition. One reason for this finding might be that the kinematics that were altered in the corrected condition were not related to pain. Indeed, at the hip, pain was only associated with greater hip medial rotation angles in the corrected condition. It is possible that if we had implemented a more in-depth training program consisting of multiple treatment sessions targeting movement pattern correction using different types of feedback (eg, visual via a mirror or computer screen, or tactile), greater improvements in hip transverse plane motion and pain would be achieved. Emerging evidence suggests that multimodal treatment programs incorporating instructions and practice of optimal movement patterns may improve pain and function,5,11,27,30 and in some cases, kinematics27,49 in people with PFP. Future studies should explore the isolated effects of movement pattern training on outcomes for multiple domains.
An alternative explanation for the lack of difference in pain between the usual and corrected conditions is that some subjects achieved a decrease in pain in the corrected condition, while others did not, eliminating an overall group effect. This possibility was explored, and indeed, in 9 subjects pain decreased by 5mm or more in the corrected condition, while in 11 subjects, pain stayed the same, increased, or decreased less than 5 mm. The 5 mm cutoff represents an average decrease of approximately 15% from the mean pain level under the usual condition, and has been used by previous investigators who compared within-session pain measurements.16 In the ‘decreased pain’ subgroup, pain was positively correlated with hip medial rotation (r=0.81, P=.005) in the corrected condition. In the ‘no decreased pain’ subgroup, pain was not correlated with any kinematic variable. This finding suggests that some females with PFP are able to achieve some pain reduction within a single session after simple instruction to correct a faulty movement pattern, and the reduction in pain is associated with a reduction in faulty hip transverse plane kinematics. It should be noted that, although reduced hip adduction was not, on average, associated with an immediate decrease in pain, it is possible that over time pain would diminish if a reduction in hip adduction were sustained.33 Identifying subgroups of individuals who are likely to respond to movement pattern training and identifying the components of dynamic knee valgus to target for sustained improvements in pain are important topics for future studies.
Interestingly, pain was associated with greater knee adduction angles in the corrected condition, which was contrary to our hypothesis. This finding is difficult to explain. It is possible that in the corrected condition, some subjects attempted to over-correct by forcing the knee into adduction, thereby increasing pain.
Although the findings of the current study generally support the relationship between pain and transverse plane angles of the hip and knee, the actual differences in hip and knee angles between the usual and corrected conditions was relatively small (hip = 1.4°, knee =1.5°). Even so, these differences are greater than their respective within-day SEM, and it is possible that subtle changes in transverse plane alignment are enough to offload painful areas of the patellofemoral joint.
Several limitations in the study must be acknowledged. First, skin markers were used to construct the lower extremity model. Such methods are subject to error from skin motion artifact,3,26 and hip and knee transverse plane angles are largely dependent on the orientation of the frontal plane of the thigh and shank. As such, inaccuracies in marker placement could introduce error in the transverse plane angle calculations. The strength of this study is its within-subject design and the fact that significant results were detected in the hypothesized direction. It is possible, however, that with improvements in the signal-to-noise ratio of transverse plane kinematic measurements, additional significant results would have been detected. Second, only 1 movement task was analyzed. The single limb squat was chosen because it is a pain-provoking activity for people with PFP that imposes mechanical demands which could induce dynamic knee valgus. Still, it is not known if similar findings would be detected in other weight bearing tasks, and as such, future studies should incorporate additional movement tasks. Third, subjects were instructed to keep their trunk upright during the squat, which could have altered their “usual’ pattern of performing the task, and thus could have influenced the load at the patellofemoral joint. While females have been shown to keep the trunk fairly upright during their usual performance of a single limb squat,18 and we did not notice excessive trunk movement in our subjects, future studies should investigate the contribution of the trunk to dynamic knee valgus. Lastly, the sample was relatively small and included only females who demonstrated observable dynamic knee valgus. Although this subgroup is important to study, as these subjects may be most likely to respond to movement pattern training, the results may not be generalizable to the entire population of people with PFP.
CONCLUSION
Compared to the usual condition, females with PFP had increased pain and increased hip medial rotation and knee lateral rotation in the exaggerated dynamic knee valgus condition. Increased pain was associated with increased knee lateral rotation in the usual and exaggerated conditions. In the corrected condition, hip adduction and knee lateral rotation decreased compared to the usual condition, and while the mean pain level was unchanged, increased pain was associated with increased hip medial rotation in the corrected condition. Avoiding or correcting dynamic knee valgus may be an important component of rehabilitation programs in females with PFP who demonstrate observable dynamic knee valgus.
KEY POINTS.
Findings
Exaggerating a faulty movement pattern (eg, increased hip medial rotation and knee lateral rotation) during performance of a single limb squat resulted in an immediate increase in pain, supporting a proposed mechanism for PFP. Correcting a movement fault within a single session led to improvements in some kinematics (hip adduction and knee lateral rotation), however pain, on average, was unchanged. Pain was primarily correlated with faulty hip and knee transverse plane kinematics.
Implication
Instructing patients to avoid dynamic knee valgus may be an important part of a rehabilitation program for females with PFP who demonstrate observable dynamic knee valgus.
Caution
From the within-session design, we cannot determine the long term effect of movement pattern modification on kinematics, pain, or other important outcomes. The sample was limited to females who demonstrated observable dynamic knee valgus, which limits the generalizability of the findings to the larger population of people with PFP.
ACKNOWLEDGEMENTS
The authors would like to thank Barbara Yemm, DPT, for her clinical insight and thoughtful input on the discussion section of this manuscript
The project described was supported by Award Number R15HD059080 from the Eunice Kennedy Shriver National Institute Of Child Health & Human Development. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute Of Child Health & Human Development or the National Institutes of Health.
This study was approved by the Institutional Review Board at Saint Louis University.
REFERENCES
- 1.Andriacchi TP, Andersson GB, Ortengren R, Mikosz RP. A study of factors influencing muscle activity about the knee joint. J Orthop Res. 1984;1:266–275. doi: 10.1002/jor.1100010306. [DOI] [PubMed] [Google Scholar]
- 2.Bell AL, Pedersen DR, Brand RA. A comparison of the accuracy of several hip center location prediction methods. J Biomech. 1990;23:617–621. doi: 10.1016/0021-9290(90)90054-7. [DOI] [PubMed] [Google Scholar]
- 3.Benoit DL, Ramsey DK, Lamontagne M, Xu L, Wretenberg P, Renstrom P. Effect of skin movement artifact on knee kinematics during gait and cutting motions measured in vivo. Gait Posture. 2006;24:152–164. doi: 10.1016/j.gaitpost.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 4.Bolgla LA, Malone TR, Umberger BR, Uhl TL. Hip strength and hip and knee kinematics during stair descent in females with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2008;38:12–18. doi: 10.2519/jospt.2008.2462. [DOI] [PubMed] [Google Scholar]
- 5.Boling MC, Bolgla LA, Mattacola CG, Uhl TL, Hosey RG. Outcomes of a weight-bearing rehabilitation program for patients diagnosed with patellofemoral pain syndrome. Arch Phys Med Rehabil. 2006;87:1428–1435. doi: 10.1016/j.apmr.2006.07.264. [DOI] [PubMed] [Google Scholar]
- 6.Boling MC, Padua DA, Marshall SW, Guskiewicz K, Pyne S, Beutler A. A prospective investigation of biomechanical risk factors for patellofemoral pain syndrome: the Joint Undertaking to Monitor and Prevent ACL Injury (JUMP-ACL) cohort. Am J Sports Med. 2009;37:2108–2116. doi: 10.1177/0363546509337934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carlsson AM. Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogue scale. Pain. 1983;16:87–101. doi: 10.1016/0304-3959(83)90088-X. [DOI] [PubMed] [Google Scholar]
- 8.Chumanov ES, Wall-Scheffler C, Heiderscheit BC. Gender differences in walking and running on level and inclined surfaces. Clin Biomech. 2008;23:1260–1268. doi: 10.1016/j.clinbiomech.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 9.Cichanowski HR, Schmitt JS, Johnson RJ, Niemuth PE. Hip strength in collegiate female athletes with patellofemoral pain. Med Sci Sports Exerc. 2007;39:1227–1232. doi: 10.1249/mss.0b013e3180601109. [DOI] [PubMed] [Google Scholar]
- 10.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd Lawrence Earlbaum Associates, Inc.; Hillsdale, NJ: 1988. [Google Scholar]
- 11.Collins N, Crossley K, Beller E, Darnell R, McPoil T, Vicenzino B. Foot orthoses and physiotherapy in the treatment of patellofemoral pain syndrome: randomised clinical trial. Bmj. 2008;337:a1735. doi: 10.1136/bmj.a1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Csintalan RP, Schulz MM, Woo J, McMahon PJ, Lee TQ. Gender differences in patellofemoral joint biomechanics. Clin Orthop Relat Res. 2002:260–269. doi: 10.1097/00003086-200209000-00026. [DOI] [PubMed] [Google Scholar]
- 13.DeHaven KE, Lintner DM. Athletic injuries: comparison by age, sport, and gender. Am J Sports Med. 1986;14:218–224. doi: 10.1177/036354658601400307. [DOI] [PubMed] [Google Scholar]
- 14.Earl JE, Monteiro SK, Snyder KR. Differences in lower extremity kinematics between a bilateral drop-vertical jump and a single-leg step-down. J Orthop Sports Phys Ther. 2007;37:245–252. doi: 10.2519/jospt.2007.2202. [DOI] [PubMed] [Google Scholar]
- 15.Earl JE, Vetter CS. Patellofemoral pain. Phys Med Rehabil Clin N Am. 2007;18:439–458. doi: 10.1016/j.pmr.2007.05.004. viii. [DOI] [PubMed] [Google Scholar]
- 16.Enthoven P, Skargren E, Kjellman G, Oberg B. Course of back pain in primary care: a prospective study of physical measures. J Rehabil Med. 2003;35:168–173. doi: 10.1080/16501970306124. [DOI] [PubMed] [Google Scholar]
- 17.Fuchs S, Schutte G, Witte H. Effect of knee joint flexion and femur rotation on retropatellar contact of the human knee joint. Biomed Tech (Berl) 1999;44:334–338. [PubMed] [Google Scholar]
- 18.Graci V, Van Dillen LR, Salsich GB. Gender differences in trunk, pelvis and lower limb kinematics during a single leg squat. Gait Posture. 2012;36:461–466. doi: 10.1016/j.gaitpost.2012.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hewett TE, Ford KR, Myer GD, Wanstrath K, Scheper M. Gender differences in hip adduction motion and torque during a single-leg agility maneuver. J Orthop Res. 2006;24:416–421. doi: 10.1002/jor.20056. [DOI] [PubMed] [Google Scholar]
- 20.Huberti HH, Hayes WC. Patellofemoral contact pressures. The influence of q-angle and tendofemoral contact. J Bone Joint Surg Am. 1984;66:715–724. [PubMed] [Google Scholar]
- 21.Ireland ML, Willson JD, Ballantyne BT, Davis IM. Hip strength in females with and without patellofemoral pain. J Orthop Sports Phys Ther. 2003;33:671–676. doi: 10.2519/jospt.2003.33.11.671. [DOI] [PubMed] [Google Scholar]
- 22.Kannus P, Natri A, Paakkala T, Jarvinen M. An outcome study of chronic patellofemoral pain syndrome. Seven-year follow-up of patients in a randomized, controlled trial. J Bone Joint Surg Am. 1999;81:355–363. doi: 10.2106/00004623-199903000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Lee TQ, Anzel SH, Bennett KA, Pang D, Kim WC. The influence of fixed rotational deformities of the femur on the patellofemoral contact pressures in human cadaver knees. Clin Orthop Relat Res. 1994:69–74. [PubMed] [Google Scholar]
- 24.Lee TQ, Yang BY, Sandusky MD, McMahon PJ. The effects of tibial rotation on the patellofemoral joint: assessment of the changes in in situ strain in the peripatellar retinaculum and the patellofemoral contact pressures and areas. J Rehabil Res Dev. 2001;38:463–469. [PubMed] [Google Scholar]
- 25.Levinger P, Gilleard WL, Sprogis K. Frontal plane motion of the rearfoot during a one-leg squat in individuals with patellofemoral pain syndrome. J Am Podiatr Med Assoc. 2006;96:96–101. doi: 10.7547/0960096. [DOI] [PubMed] [Google Scholar]
- 26.Manal K, McClay I, Stanhope S, Richards J, Galinat B. Comparison of surface mounted markers and attachment methods in estimating tibial rotations during walking: an in vivo study. Gait Posture. 2000;11:38–45. doi: 10.1016/s0966-6362(99)00042-9. [DOI] [PubMed] [Google Scholar]
- 27.Mascal CL, Landel R, Powers C. Management of patellofemoral pain targeting hip, pelvis, and trunk muscle function: 2 case reports. J Orthop Sports Phys Ther. 2003;33:647–660. doi: 10.2519/jospt.2003.33.11.647. [DOI] [PubMed] [Google Scholar]
- 28.McConnell J. The management of chondromalacia patellae: A long term solution. Aust J Physiother. 1986;32:215–223. doi: 10.1016/S0004-9514(14)60654-1. [DOI] [PubMed] [Google Scholar]
- 29.Myer GD, Ford KR, Barber Foss KD, et al. The incidence and potential pathomechanics of patellofemoral pain in female athletes. Clin Biomech. 2010;25:700–707. doi: 10.1016/j.clinbiomech.2010.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nakagawa TH, Muniz TB, Baldon Rde M, Dias Maciel C, de Menezes Reiff RB, Serrao FV. The effect of additional strengthening of hip abductor and lateral rotator muscles in patellofemoral pain syndrome: a randomized controlled pilot study. Clin Rehabil. 2008;22:1051–1060. doi: 10.1177/0269215508095357. [DOI] [PubMed] [Google Scholar]
- 31.Noehren B, Barrance PJ, Pohl MP, Davis IS. A comparison of tibiofemoral and patellofemoral alignment during a neutral and valgus single leg squat: An MRI study. Knee. 2012;19:380–386. doi: 10.1016/j.knee.2011.05.012. [DOI] [PubMed] [Google Scholar]
- 32.Noehren B, Pohl MB, Sanchez Z, Cunningham T, Lattermann C. Proximal and distal kinematics in female runners with patellofemoral pain. Clin Biomech. 2012;27:366–371. doi: 10.1016/j.clinbiomech.2011.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Noehren B, Scholz J, Davis I. The effect of real-time gait retraining on hip kinematics, pain and function in subjects with patellofemoral pain syndrome. Br J Sports Med. 2011;45:691–696. doi: 10.1136/bjsm.2009.069112. [DOI] [PubMed] [Google Scholar]
- 34.Powers CM. The influence of abnormal hip mechanics on knee injury: a biomechanical perspective. J Orthop Sports Phys Ther. 2010;40:42–51. doi: 10.2519/jospt.2010.3337. [DOI] [PubMed] [Google Scholar]
- 35.Ramappa AJ, Apreleva M, Harrold FR, Fitzgibbons PG, Wilson DR, Gill TJ. The effects of medialization and anteromedialization of the tibial tubercle on patellofemoral mechanics and kinematics. Am J Sports Med. 2006;34:749–756. doi: 10.1177/0363546505283460. [DOI] [PubMed] [Google Scholar]
- 36.Riegger-Krugh C, Keysor JJ. Skeletal malalignments of the lower quarter: correlated and compensatory motions and postures. J Orthop Sports Phys Ther. 1996;23:164–170. doi: 10.2519/jospt.1996.23.2.164. [DOI] [PubMed] [Google Scholar]
- 37.Robinson RL, Nee RJ. Analysis of hip strength in females seeking physical therapy treatment for unilateral patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2007;37:232–238. doi: 10.2519/jospt.2007.2439. [DOI] [PubMed] [Google Scholar]
- 38.Sahrmann SA. Movement system impairment syndromes of the extremities, cervical and thoracic spines. Elsevier/Mosby; St. Louis: 2011. [Google Scholar]
- 39.Salsich GB, Long-Rossi F. Do females with patellofemoral pain have abnormal hip and knee kinematics during gait? Physiother Theory Pract. 2010;26:150–159. doi: 10.3109/09593980903423111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Salsich GB, Perman WH. Patellofemoral joint contact area is influenced by tibiofemoral rotation alignment in individuals who have patellofemoral pain. J Orthop Sports Phys Ther. 2007;37:521–528. doi: 10.2519/jospt.2007.37.9.521. [DOI] [PubMed] [Google Scholar]
- 41.Souza RB, Draper CE, Fredericson M, Powers CM. Femur rotation and patellofemoral joint kinematics: a weight-bearing magnetic resonance imaging analysis. J Orthop Sports Phys Ther. 2010;40:277–285. doi: 10.2519/jospt.2010.3215. [DOI] [PubMed] [Google Scholar]
- 42.Souza RB, Powers CM. Differences in hip kinematics, muscle strength, and muscle activation between subjects with and without patellofemoral pain. J Orthop Sports Phys Ther. 2009;39:12–19. doi: 10.2519/jospt.2009.2885. [DOI] [PubMed] [Google Scholar]
- 43.Souza RB, Powers CM. Predictors of Hip Internal Rotation During Running: An Evaluation of Hip Strength and Femoral Structure in Women With and Without Patellofemoral Pain. Am J Sports Med. 2009;37:579–587. doi: 10.1177/0363546508326711. [DOI] [PubMed] [Google Scholar]
- 44.Stefanyshyn DJ, Stergiou P, Lun VM, Meeuwisse WH, Worobets JT. Knee angular impulse as a predictor of patellofemoral pain in runners. Am J Sports Med. 2006;34:1844–1851. doi: 10.1177/0363546506288753. [DOI] [PubMed] [Google Scholar]
- 45.Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR, Zumbo BD. A retrospective case-control analysis of 2002 running injuries. Br J Sports Med. 2002;36:95–101. doi: 10.1136/bjsm.36.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tiberio D. The effect of excessive subtalar joint pronation on patellofemoral mechanics: A theoretical model. J Orthop Sports Phys Ther. 1987;9:160–165. doi: 10.2519/jospt.1987.9.4.160. [DOI] [PubMed] [Google Scholar]
- 47.Willson JD, Davis IS. Lower extremity mechanics of females with and without patellofemoral pain across activities with progressively greater task demands. Clin Biomech. 2008;23:203–211. doi: 10.1016/j.clinbiomech.2007.08.025. [DOI] [PubMed] [Google Scholar]
- 48.Willson JD, Davis IS. Utility of the frontal plane projection angle in females with patellofemoral pain. J Orthop Sports Phys Ther. 2008;38:606–615. doi: 10.2519/jospt.2008.2706. [DOI] [PubMed] [Google Scholar]
- 49.Willy RW, Davis IS. The effect of a hip-strengthening program on mechanics during running and during a single-leg squat. J Orthop Sports Phys Ther. 2011;41:625–632. doi: 10.2519/jospt.2011.3470. [DOI] [PubMed] [Google Scholar]
- 50.Wirtz AD, Willson JD, Kernozek TW, Hong DA. Patellofemoral joint stress during running in females with and without patellofemoral pain. Knee. 2011 doi: 10.1016/j.knee.2011.09.006. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]