Abstract
Background
International studies show that aggressive behavior against primary care physicians is not an uncommon occurrence. There has been no systematic study to date of the nature and frequency of such occurrences in Germany.
Methods
A four-page questionnaire was sent to a nationwide random sample of 1500 primary care physicians. It contained questions about the type, frequency, severity, and site of aggressive behavior against the physician.
Results
831 (59%) of 1408 correctly delivered questionnaires could be included in the analysis. 91% of the respondents (95% confidence interval [CI], 89%-93%) said they had been the object of aggressive behavior at some time in their career as a primary care physician, 73% (95% CI, 70%–76%) in the previous 12 months. Severe aggression or violence had been experienced by 23% (95% CI, 20%–25%) in their entire career and 11% (95% CI, 8%–13%) in the previous year. The vast majority of respondents said they felt safe in their offices. 66% of female and 34% of male respondents said they did not feel safe making house visits while on on-call duty.
Conclusion
The frequency and extent of aggression and violence against primary care physicians in Germany is comparable to those reported by international studies. Strategies for dealing with this problem should be developed. In particular, the issue of safety on emergency call needs to be addressed.
The subject of aggression and violence against doctors has thus far hardly been given any attention in medical education and continuing medical education in Germany. Individual authors assume that the prevalence of violent acts against doctors has increased over the past decades (1, 2), but systematic investigations into the problem are lacking.
A striking finding in international studies is the fact that aggressive behavior towards doctors is obviously a usual occurrence. Four Australian studies from 2003 to 2007, for example, showed that 68–73% of the participating primary care physicians had already gathered experiences with aggression directed at them during their careers (3– 6). In the 12 months preceding the surveys, incidence rates of aggression towards primary care physicians varied between 48% and 64% (3– 6). A study from Canada from 2010 concluded that 29% of all participating primary care physicians had been exposed to aggressive behavior in the month preceding the survey. Of these affected doctors, almost each one had experienced milder aggressive events, for example, verbal insults and verbal abuse. 26% had experienced moderate aggression—for example, damage to property (criminal damage)—and 8% had been victims of serious physical violence and sexual assaults (7).
In order to contribute to, and thereby improve, the available data on the problems of aggression and violence against primary care physicians in Germany, we conducted a national survey on the subject. Our objective was:
To gauge the general sense of personal safety in primary care physicians in the surgery, on house visits and visits to homes, and during on-call duties (practice based or house visits);
To determine the proportions of primary care physicians who in the course of their professional duties had ever experienced different aggressive behaviors in rooms within their practices, during visits to patients’ houses or care/nursing homes, and during on-call duties (in the practice and during home visits), and to determine the frequency of these events in the 12 months preceding the survey;
To document the most serious aggressive incident for each respective participant, including the circumstances leading to the assault, characteristics of the perpetrator, and the consequences of the assault.
Methods
Study design
The study was designed as a once-only postal questionnaire sent to a random sample of 1500 primary care physicians; the evaluation was anonymized. The study was approved by the ethics committee at Technische Universität München (TUM, Technical University Munich). The total study population consisted of all resident primary care physicians who were active in Germany in October 2013. The sample was drawn from a national database of addresses held by the company Adressendiscount (www.adressendiscount.de), which includes data from 132 000 physicians in private practice (according to data from the German Medical Association, this is equivalent to 90% of all doctors in Germany who provide treatment on an outpatient basis), of which 36 400 were primary care physicians. The addresses were selected by using the “Select cases—random sample” function in the software package SPSS. All selected physicians received a letter in October 2013 that contained information about the study, a questionnaire, and a stamped and addressed envelope. Reminders were sent at the beginning and the end of November 2013.
Questionnaire
The four-page questionnaire was developed after an inspection of the original questionnaires from several international sources (3– 9). A pilot version was tested qualitatively and quantitatively beforehand, in a continuing medical educational event for primary care physicians (n=30). Superfluous questions and the questionnaire’s quality and comprehensibility were discussed. On the basis of the evaluation of this test run, the final, four-page questionnaire was developed (eQuestionnaire). The questionnaire comprised six sections.
Section 1 included questions relating to the general feeling/perception of safety in the practice premises, during house and home visits, and during on-call work (practice based and during house/home visits).
-
Section 2 included questions relating to whether defined forms of aggression had been experienced in the practice premises at any point during their career as a primary care physician and in the preceding 12 months, and if so, how often. The individual forms of aggression are listed below; the predefined categorization as mild/slight, moderate, and serious/severe forms of aggression is given in square parentheses:
Verbal insult/abuse [mild/slight]
Threat/intimidation [moderate]
Mild physical violence (pushing, hassling, clinging) [moderate]
Pronounced physical violence (biting, hitting, kicking, suffocating/strangling) [serious/severe]
Threat using object or weapon [serious/severe]
Attack using object or weapon [serious/severe]
Sexual harassment (suggestive remarks and gestures; groping excluding breasts/genitals) [moderate]
Sexual abuse (groping of breasts and genitals; sexual coercion; rape) [serious/severe]
Criminal damage/theft [moderate].
Section 3 included the same questions as section 2, but relating to house/home visits and on-call duties.
Section 4 included questions relating to reputational damage, libel/slander, false statements on physician internet portals, and stalking.
In section 5, doctors were invited to provide further details about the incident that they themselves considered to be the most serious in their medical career. In addition to a free-text description of the incident, this section collected information on the perpetrator, the level of fear, location, timing, and consequences of the incident.
Section 6 included questions relating to the doctor’s person and practice.
Statistical evaluation
Previous experiences from a similarly conducted survey (10) prompted an expectation of a minimum return rate of 40% of the sample. The objective was the ability to estimate the prevalence of aggressive behavior directed at doctors with a 95% confidence interval of ± 4%. To this end, 600 evaluable responses were required for an assumed prevalence of 50% (calculated using EpiCalc 2000). In view of the expected response rate, we therefore wrote to 1500 doctors.
For the purposes of the descriptive evaluation, we calculated—depending on the type of data—means and standard deviations, medians, quartiles, minimum and maximum values or percentages and absolute frequencies, in total and separately for the sexes. 95% confidence intervals for frequencies for the most important prevalence estimates were produced by using the bootstrapping function in SPSS (1000 samples). Analyses for differences between female and male doctors were done according to the scale level by using Fisher’s exact test, the chi square test, the Mann-Whitney U test, or Student’s t test. Furthermore we calculated explorative logistic regression analyses (inclusion model) in order to study associations between:
Doctors’ characteristics (independent variables) and perceptions of safety (dependent variables)
Doctors’ characteristics and the experience of a serious incident (dependent) during the course of working as a primary care physician.
Lacking entries were not substituted (we report valid percentages). Significance tests and regression analyses (eSupplement and eTables 1– 7) were undertaken exclusively for the purposes of exploration. We did not adjust for multiple testing.
eTable 1. P values for individual doctors’ characteristics from the multivariate ordinal regression analyses of associations between doctors’ characteristics and their sense of safety in the five settings.
| Characteristic | Practice | House visit | Home visit | On-call practice | On-call house visit |
|---|---|---|---|---|---|
| Female sex yes/no | 0.002 | <0.001 | 0.03 | <0.001 | <0.001 |
| Serious aggression/ violence experienced yes/no | 0.008 | 0.001 | n. s. | <0.001 | 0.001 |
| Age > 55 years yes/no | n. s. | 0.001 | 0.03 | n. s. | 0.002 |
| Migration background yes/no | n. s. | n. s. | n. s. | 0.002 | n. s. |
| Singlehanded practice yes/no | 0.004 | n. s. | n. s. | n. s. | n. s. |
| City practice yes/no* | 0.004 | n. s. | n. s. | n. s. | 0.003 |
| Patient clientele financially weak yes/no | 0.04 | n. s. | n. s. | n. s. | n. s. |
*Coding for multivariable analysis in dummy variables big city yes/no and city yes/no (city without significant influence);
n. s. = non-significant
eTable 7. Multivariate logistic regression for association of doctors’ characteristics and report of at least one serious form of aggression (r² = 0.02).
| Characteristic | Prevalence | OR | OR (95% CI) | P value | OR | OR (95% CI) | P value |
|---|---|---|---|---|---|---|---|
| yes/no | univariate | multivariate | |||||
| Female sex yes/no | 23%/23% | 1.00 | (0.72–1.39) | 1.00 | 0.95 | (0.67–1.35) | 0.78 |
| Age > 55 years yes/no | 24%/20% | 1.13 | (0.95–1.34) | 0.16 | 0.86 | (0.61–1.21) | 0.38 |
| Migration background yes/no | 21%/23% | 0.90 | (0.42–1.91) | 0.85 | 0.93 | (0.43–2.02) | 0.86 |
| Singlehanded practice yes/no | 25%/20% | 1.32 | (0.95–1.84) | 0.10 | 1.30 | (0.92–1.83) | 0.14 |
| City practice yes/no* | 22%/23% | 0.96 | (0.65–1.41) | 0.85 | 0.93 | (0.60–1.43) | 0.73 |
| Patient clientele financially weak yes/no | 29%/20% | 1.62 | (1.10–2.37) | 0.02 | 1.62 | (1.01–2.51) | 0.02 |
*Coding for multivariable analysis in dummy variables big city yes/no and city yes/no (city without significant influence) [OR (95% CI) = 0.98 (0.67 to 1.45); p = 0.98]) OR. odds ratio; CI. confidence interval
Results
Response rate and participants’ characteristics
74 of 1500 sent letters were not delivered because they carried incorrect addresses. Furthermore, 14 doctors informed us that they had been wrongly contacted: 9 reported that they were not working as primary care physicians, and 5 were already retired. Four were deceased. Consequently, 1408 doctors had been contacted successfully. 835 study participants returned completed questionnaires. Since the protocol stipulated that a doctor’s sex was to be included in the analysis, four questionnaires were excluded from the evaluation as they did not contain this information. Our results are therefore based on data from 831 participants (59% of 1408).
40% of respondents were women and 60% men. Female doctors had been primary care physicians for a mean of 19 years, male doctors for 22 years. Female doctors worked slightly more often in large cities and conducted fewer house visits than their male colleagues (Table 1).
Table 1. Sociodemographic and practice characteristics (frequencies as percentages. means [standard deviations] or medians [1st/3rd quartile] where the distribution is notably skewed).
| Characteristic (No. of missing data) | Female doctors (n = 333) | Male doctors (n = 498) | Total (n = 831) | P value |
|---|---|---|---|---|
| Age in years (7) | 53 (8) | 56 (8) | 55 (8) | <0.001*1 |
| Migration background (4) | 7% | 4% | 5% | 0.18*2 |
| Worked as a general practitioner (years) (7) | 19 (9) | 22 (9) | 21 (9) | <0.001*1 |
Type of practice (6)
|
50% 48% 2% |
52% 48% 0% |
51% 48% 1% |
0.07*2 |
| No. of house visits/week (33) | 10 (8) | 16 (11) | 14 (10) | <0.001*1 |
| No. of on-call shifts/month (178) | 1 (1/2) | 1 (1/2) | 1 (1/2) | 0.91*3 |
| Location of practice (4) – City > 100000 population – City/town 10–100000 population – Town/village < 10000 population | 28% 36% 36% | 21% 36% 44% | 24% 36% 40% | 0.02*2 |
Patients’ financial profile (10)
|
9% 69% 2% |
9% 72% 19% |
9% 71% 21% |
0.62*2 |
*1= P value calculated from t-test;
*2= P value calculated from Fisher’s exact test (for dichotomous variables) or chi² test (for variables with three or more expressions);
*3= P value calculated from Mann-Whitney U test
Sense of safety
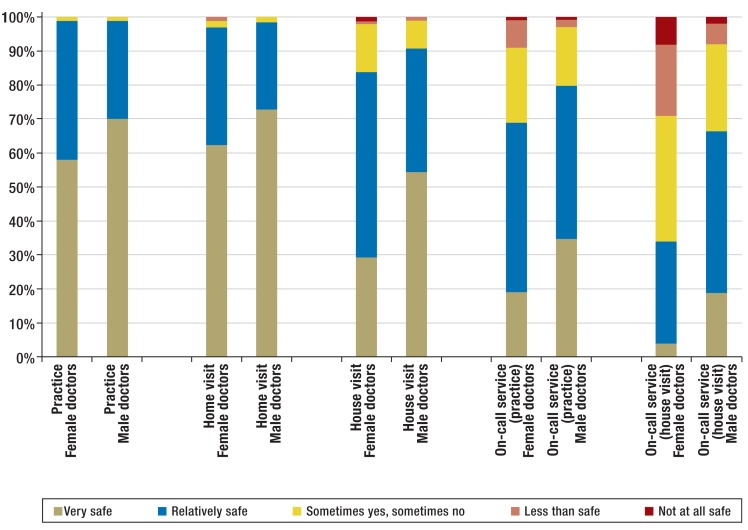
The majority of respondents felt safe or very safe in their own practices and during house visits (Figure). Fewer female doctors, however, felt very safe than male doctors (58% vs 70% in practices and 63% vs 73% during visits to homes). Regarding house visits or on-call service in surgeries, the proportion of participants who ticked “partly-partly,” “less likely to feel safe,” or “not at all safe” was larger: 16% of female doctors (house visit) and 31% (on-call duty in the surgery), and 9% and 20% of male doctors. Regarding the perception of safety during house visits when on call, the responses increased to 66% in women and 34% in men.
Figure.
General sense of safety in the practice, on home visits, on house visits, and during on-call service
All differences between female doctors and male doctors P<0.001 except for home visit (P=0.002, Mann-Whitney U test)
Number of doctors without a response (first digit, response “I don’t do this”; second digit, not available): practice 0+12, house visit 4+11, home visit 16+19, on-call service in the practice 144+28, on-call house visits 100+16
Personal experience of aggression
9% (95% CI 7% to 11%) of participants had never experienced aggressive behaviors during their career, and 27% (95% CI 24% to 40%) not during the preceding 12 months (Table 2). 91% (95% CI 89% to 93%) of participants reported that at some point during their career as a primary care physician they had been confronted with aggressive behavior in some form, and 73% (95% CI 70% to 76%) reported that this had been the case in the preceding 12 months. Mildly/slightly aggressive incidents had been experienced by 79% (95% CI 77% to 82%) of participants at some point and by 54% (95% CI 51% to 58%) in the preceding 12 months. More female doctors had been affected than male doctors (60% vs 51%, p=0.01). For moderate incidents, the proportions were 81% (ever experienced aggressive behavior, 95% CI 78% to 83%) and 58% (experienced aggressive behavior in the preceding 12 months, 95% CI 55% to 62%). For serious incidents, the proportions were 23% (ever, 95% CI 20% to 25%) and 11% (in preceding 12 months, 95% CI 8% to 13%; differences between the sexes did not reach significance).
Table 2. Proportion in % of respondents (n = 831) who were at some point during their medical careers or during the preceding 12 months exposed to the listed forms of aggression at least once in the respective setting*.
| Form of aggression | Any setting | Practice | House visit | Home visit | On-call service | |
|---|---|---|---|---|---|---|
| Practice | House visit | |||||
| 0–26 | 4–10 | 20–23 | 30–32 | 95–100 | 70–77 | |
| Ever (95% CI)/ 12 months (95% CI) | Ever/ 12 months | Ever/ 12 months | Ever/ 12 months | Ever/ 12 months | Ever/ 12 months | |
| No aggression experienced | 9% (7–11%)/27% (24–40%) | 16%/38% | 67%/86% | 77%/91% | 70%/84% | 61%/81% |
| Verbal insult/abuse (l) | 79% (77–82%)/54% (51–58%) | 73%/48% | 29%/12% | 21%/6% | 26%/13% | 34%/17% |
| Threat/intimidation (m) | 38% (35–41%)/21% (18–24%) | 30%/17% | 10%/3% | 4%/2% | 9%/4% | 17%/7% |
| Slight physical violence (m) | 16% (13–18%)/7% (5–8%) | 9%/3% | 4%/1% | 4%/2% | 2%/< 1% | 7%/2% |
| Sexual harassment (m) − Female doctors − Male doctors |
17% (14–20%)/10% (8–12%) 28% (23–33%)/17% (13–21%) 10% (7–12%)/5% (3–7%) |
15%/9% 25%/15% 9%/5% |
4%/1% 6%/2% 2%/1% |
1%/1% 3%/2% −/− |
2%/1% 5%/2% 1%/< 1% |
2%/1% 4%/3% 1%/< 1% |
| Damage to property, theft (m) | 55% (51–58%)/35% (31–38%) | 54%/34% | 3%/1% | 1%/< 1% | 7%/4% | 3%/1% |
| Reputational damage, libel/slander on the internet | 48% (44–51%)/31% (27–34%) | |||||
| At least one form of moderate aggression | 81% (78–83%)/58% (55–62%) | 67%/44% | 13%/4% | 7%/4% | 15%/8% | 19%/8% |
| Pronounced physical aggression (s) | 8% (6–10%)/3% (2–4%) | 4%/2% | 2%/<1% | 3%/1% | 1%/− | 3%/1% |
| Threat with object or weapon (s) | 8% (6–10%)/3% (2–4%) | 4%/1% | 2%/<1% | <1%/- | 1%/<1% | 4%/1% |
| Attack with object or weapon (s) | 4% (3–5%)/1% (<1%-2%) | 2%/1% | 1%/<1% | 1%/<1% | 1%/<1% | 2%/1% |
| Sexual abuse (s) | 1% (<0.5– 2%)/<1% (0–1%) | 1%/<1% | <1%/<1% | <1%/<1% | −/− | −/− |
| Stalking (s) | 9% (7–10%)/5% (4–7%) | |||||
| At least one form of serious aggression | 23% (20–25%)/11% (9–13%) | 9%/3% | 4%/1% | 3%/1% | 2%/<1% | 6%/2% |
*Because of pronounced differences between the sexes for sexual harassment, female and male doctors are additionally listed separately. For “any setting“, 95% confidence intervals are shown additionally
Classification: l = light aggression; m = moderate aggression; s = serious aggression; <1% = at least 1 reported case. If proportion <0.5%; – = no case reported.
In absolute terms (without considering the amount of working time spent in the respective location), incidents of aggression are particularly common in doctors’ practices (85% ever and 63% in the preceding 12 months). They were notably less common during house visits (33% and 14%), during home visits (23% and 9%), during on-call work in practices (30% and 16%) or during house visits while on call (39% and 19%).
Verbal insults and abuse were by far the most often reported incidents (Table 2). 73% of participants reported having been subjected to verbal insults or abuse in their practices at some point during their careers, and 48% reported this for the preceding 12 months. Criminal damage or theft (54% and 34%) and reputational damage or libel/slander on the Internet (48% and 31%) were also mentioned often. Sexual harassment was committed particularly towards female doctors (25% and 15%).
Analysis of incidents experienced as the most serious
449 participants provided further details on the incident that they themselves had experienced as the most serious in their careers. 310 participants described events in a free text field in greater or lesser detail. 67 descriptions were of verbal insults, 54 of threats, 74 of physical violence or running rampage, 45 of violence with weapons or objects, and 70 of different other incidents. Example reports (case descriptions) are shown in the eBox.
eBox. Incident descriptions.
Verbal insults/abuse
“Verbal abuse because of allegedly incorrect treatment”
“Insulting comments when refused to prescribe a psychoactive drug to a patient with addiction disorder”
“Drug dependent patient calls me an arsehole because I won’t prescribe opiates.”
“Verbal abuse by several family members during emergency house visit in a socially problematic area.”
“Verbal abuse because of an allegedly unsatisfactory number of house visits.”
“Patient stands in my office, complains about having had to wait for far too long, then turns up the volume: accuses me of providing incorrect treatment. Verbally aggressive, approaches me, no physical contact!”
“When I refused to provide him with an unjustified sick note, the patient became annoyed, but restricted themselves to general verbal abuse, ’Can’t even rely on my own GP.’ And declared he would comment on me accordingly on the internet. Slammed the door on departing.”
Threats
“Noisy argument with threat of physical violence in a patient rampaging in their own home. Admitted to psychiatric hospital.”
“During an emergency house visit, the front door to the apartment was locked immediately once I’d entered. Because of the shabby apartment I felt a sense of threat. The patient refused to open the door and only did so after I had threatened to call the police several times.”
“Psychotic patient at risk of decompensating, motor restlessness, no distance, intimidating, threatening behavior.”
“Nocturnal visit on call. Patient under the influence of alcohol and aggressive after an argument with his wife. Threatens me with their large dog.”
“Underlying threat from a child’s father … if anything happens to the child…”
“Patient threatened me with their raised fist: he’d hit me in the face unless I immediately issue a prescription…”
“Verbal attack from a just arrived relative after the death of an 86 year old patient. High volume and insulting, threatened with investigating authorities.”
Physical violence/rampage
“House visit on call to patient under the influence of alcohol with massively aggressive behavior. Physical attack that necessitated police operation, and help from a neighbor who was present. The patient had thrown 2–3 large objects out of the window.”
“A patient got so agitated over the waiting times that he verbally abused me badly and stamped on my PC, which was placed on the floor, destroying it!”
“Physical attack with fist strokes directed at me as I was trying to protect the doctor’s assistant (words to the effect that: I responded with fisticuffs…).”
“Drunk patient rampages around the waiting room. The police is called out. Damage to car.”
“Patient with acute psychosis—danger to self and others, raging after attempted suicide—had to be fixated by police officers in order to enable administration of sedatives.”
“The patient started boxing and hitting me with substantial aggression. It was not his fault, however, as his Hb concentration was below 5 and his brain was not sufficiently supplied with oxygen.”
“Mentally disabled patient tries to throw a metal litter bin at me.”
Threats using weapons or objects
“Threatened with a gun in the consultation room.”
“Patient punched a hole in the counter using letter holder and threatened me.”
“Threatened with a kitchen knife while on call because the alcoholized man did not like his girlfriend’s medical treatment.”
“Threatened with a firearm during house visit. Police was present and attended.”
“During on-call house visit years ago, threatened by male patient (alcoholic) with a broken-off beer bottle and broom stick.”
“Emergency house visit night, to a drug dependent person on withdrawal who had an aggressive German shepherd dog. A knife was held to my throat in order to obtain a prescription. The dog was not locked away. Police refused help in an effort to admit patient to hospital!”
Other
“Drug dependent patient steals prescriptions, arrested in practice.”
“Four years ago the practice was broken into. The waiting room window was levered out and car keys placed at reception were stolen, as was the car that was parked on the car park in front of the practice (no one in the building, especially at night).”
“Female patient who had left the practice kept standing in front of the practice for days, trying to stop other patients from attending.”
“Verbal insults and lies on the internet (Jameda).”
“For several weeks, telephone terror during night and day (anonymous calls, especially at night)—stopped only with police involvement and an intercept device.”
“Patient with a history of alcohol dependency and medication abuse, who had avoided detoxification for years, has never followed medical advice, does not value other colleagues (’they are all a***holes’ suddenly accused me of acting medically incorrectly and takes me to court (was verbally aggressive, gesticulating).”
“Two practice break-ins committed by the same ’team.’ One of the female burglars had previously attended as a patient. Damages of around 800 Euros. Practice door jemmied open and 800 Euros stolen.”
“An immediate visit was requested because of a raised temperature and cough. I assessed the situation and scheduled the visit for after surgery hours (1.5 hours later). A female relative of the patient threatened me, followed my recommendation and called emergency services (112). Complaint made to the public prosecutor’s office for physical injury resulting from negligence, etc.”
“Attempted blackmail. Husband thought he had proof of my having a relationship with his (separated) wife (who lived elsewhere); threatened to pass the information to Bild newspaper, demanded DM 25 000.”
Serious incidents
“On call at night. House visit for complaint about upper abdominal pain, C2-related continuity delirium, attack with stabbing weapon, I fled through the window.”
“I worked in the drug substitution service for several years. A patient visited me at home on a Saturday morning (he reported to have missed a drug dispensing appointment) and demanded his drug ration, which I did not have available. He started rampaging, kicked against the door and broke a light in my front garden. We called the police. I (and my family) were really scared!”
“On-call shift, Sunday, 11.30. A masked individual rushes into reception pointing a knife and demands to be given the cash till. A colleague’s daughter (aged 13), who happened to be in the practice, was directly threatened. In spite of a large and immediate police operation (using a helicopter) the thief was not caught.”
“An elderly patient was not happy about the assessor’s statement (regarding care authorities and application for additional social services). Threatened with a stick in the practice. Threat of beating, later several demands (written) for damages. Later (because the assessor’s statement had been incorrect) written murder threats, later also against the solicitor I engaged to support me (…).”
“Locked into the apartment during a house visit by the patient’s wife and threatened with a gun by patient—he had already shot the window to pieces.”
“Called out by alcohol dependent patient and his friend during on-call shift, threatened with a knife, and greeted and bullied by three pit bull terriers on arrival at the apartment.”
“Psychiatric patient, hit out at me immediately on welcome greeting. My glasses flew away and I fell to the floor (had been hit on the temple); patient then tried to drag me up by my hair—only managed to flee once the patient was distracted; help found at nighttime only three houses further on; rescue services and police only intervened when the patient wanted to hit me again.”
“Murder threats on the telephone—several times, including to family members (husband, children), as I was held responsible for the wife’s death.”
“The patient requested diazepam. Knife attack, danger terminated only by police operation.”
From doctors’ perspectives’, 38% of the 449 incidents were regarded as slight/mild, 41% as moderate, 16% (73 incidents) as serious, and 4% (19 incidents) as very serious. In 13% the affected doctors were afraid and in 6%, very afraid (Table 3). 58% of incidents occurred in the surgeries/practices, 19% during house visits while on call, and 12% during normal house visits.
Table 3. Characteristic (level of fear, location and time) of the most serious incident by severity (frequencies reported as percentages).
| Characteristic (No. of missing data) | Slight(n = 171) | Moderate(n = 185) | Serious/very serious (n = 93) | Total(n = 449) |
|---|---|---|---|---|
| Level of fear during incident (6) | ||||
| −No fear | 34% | 11% | 9% | 19% |
| − Slightly worried | 44% | 23% | 5% | 27% |
| − Worried | 20% | 45% | 43% | 35% |
| − Afraid | 2% | 17% | 24% | 13% |
| − Very afraid | − | 4% | 19% | 6% |
| Where did the incident take place? (3) | ||||
| − In the practice | 64% | 58% | 47% | 58% |
| − During house visit | 7% | 12% | 22% | 12% |
| − During home visit | 5% | 1% | 1% | 2% |
| − In group practice | 7% | 3% | 5% | 5% |
| − During house visit while on call | 16% | 22% | 19% | 19% |
| − In private environment | 1% | 2% | 3% | 2% |
| − In practice and private environment | − | 1% | − | <1% |
| − Other | 2% | 2% | 2% | 2% |
| When did the incident take place? (6) | ||||
| − Normal working hours | 73% | 68% | 60% | 68% |
| − Weekend/Bank holiday | 11% | 10% | 11% | 11% |
| − At night | 15% | 19% | 21% | 18% |
| − Normal working hours and weekend | − | 1% | − | <1% |
| − Weekend and at night | 1% | 2% | 9% | 3% |
In four out of five incidents the perpetrators were male (Table 4). They hailed from diverse age groups. Alcohol, drugs, mental illness, or a combination of two or all three of these factors had a role in about half of these incidents (51%) and could not be excluded in another 15%. In 90 cases (20% of the total), the incident resulted in a report or complaint to the police, in 12 cases (3%), it triggered psychological damage, and in 2 cases (<1%) it led to physical injury. 81 affected doctors (18%) modified their behavior towards patients as a result of the incident.
Table 4. Characteristics of perpetrators in the most serious incident by severity (frequencies reported as percentages or means [standard deviations])*.
| Characteristic (No. of missing data) | Slight(n = 171) | Moderate(n = 185) | Serious/very serious (n = 93) | Total(n = 449) |
|---|---|---|---|---|
| Perpetrator: male sex(14) | 81% | 79% | 81% | 80% |
| Age of perpetrator in years (20) | 48 (16) | 44 (15) | 43 (14) | 45 (16) |
| Group of persons (19) | ||||
| − Patient | 76% | 69% | 75% | 73% |
| − Patient’s relative | 17% | 23% | 13% | 18% |
| − Patient and relative | 2% | 2% | 1% | 2% |
| − Other | 5% | 6% | 11% | 7% |
| Consciousness-altering factors in perpetrator (3) | ||||
| − None | 37% | 28% | 20% | 30% |
| − Alcohol | 12% | 17% | 13% | 14% |
| − Drugs | 7% | 6% | 4% | 6% |
| − Mental illness | 21% | 21% | 22% | 21% |
| − Alcohol and drugs | 2% | 3% | 4% | 3% |
| − Alcohol and mental illness | 4% | 2% | 8% | 4% |
| − Drugs and mental illness | 2% | 2% | 2% | 2% |
| − Alcohol, drugs, and mental illness | − | 2% | 3% | 1% |
| − Don’t know | 12% | 17% | 18% | 15% |
| − Other | 2% | 4% | 5% | 4% |
*Participants themselves chose the classification of severity.
Factors influencing the experience of violence and subjective sense of safety
The multivariate regression analyses (eSupplement and eTables 1– 7) found no association between doctors’ characteristics sex, age, migration background, or ty8pe and location of practice and the report of a serious incident of aggression. Only a financially weaker practice clientele was slightly associated with such experiences. A lowered sense of safety was, independently of individual work locations, clearly associated with the doctors’ characteristics female sex and the experience of a serious incident of aggression in the past. Older age and a city location had a significant association with three or two work settings respectively.
Discussion
Almost every doctor in the survey had experienced some kind of aggression at some point in their career. Slightly more than half of participating doctors had been exposed to slight or moderate aggression in the 12 months preceding the survey. More than one in 10 primary care physicians had been confronted with serious aggression or violence during this time period. Although the extent of safety within practice premises was generally perceived to be high, only one in three female doctors felt safe during house visits while on call.
The response rate of 59% in the current study is high for a survey among doctors that did not offer any special incentives (7, 10– 15). The composition of participants seems largely representative in terms of the personal characteristics and the characteristics of practices of primary care physicians. Specialists in internal medicine working in general practice were not included, as the database we used did not differentiate between these and those working in hospitals for every federal state.
It seems entirely possible that doctors who had never encountered aggression and violence in the course of their work were less likely to participate in our survey, even though the process of filling in the questionnaire would have been much simpler for them. For this reason, the results presented here may somewhat overestimate the actual prevalence of aggression and violence. In milder forms of aggression, such as verbal insults, the subjective perception and memory has an important role, which can lead to overestimates but also underestimates of the actual prevalence. However, subjective perceptions are likely to have a much smaller role in the ultimately more relevant pronounced acts of aggression or for violence in the narrower sense.
To date in Germany in the preclinical setting, the only data on aggression and violence that have been available were those for rescue workers in North Rhine–Westphalia (8). In the 12 months preceding the survey, almost all participants in that study had experienced verbal aggression (98%), and more than half (59%) at least one violent assault. However, comparisons between the rescue services and primary care physicians would obviously make sense to a very limited degree only (perhaps in the setting of visits during on-call duties). Compared with other professional groups, the annual prevalence of non-physical and physical aggression against primary care physicians is lower than in police officers (80%/54%) (16) but much higher than in teachers (47%/2%) (17).
The data from the present survey are roughly consistent with the results from other, international, studies in terms of the experience of aggression (3– 7, 9, 18– 20) (eTable 8). However, because of the in some cases very different healthcare systems and primary care systems, as well as data collection methods, any comparisons should be treated with utmost caution.
eTable 8. Overview of aggression/violence against general practitioners in the international literature.
| First author (year) | Ness*1 (2000) | Miedema*2 (2010) | Forrest*3 (2011) | Joa*4 (2012) | Carmi-Iluz*5 (2005) | Authors’ own data |
|---|---|---|---|---|---|---|
| Country | UK | Canada | Australia | Norway | Israel | Germany |
| Study population | General Practitioners | General Practitioners | General Practitioners | Medical staff primary care center (nighttime service and on-call service) | Doctors medical center/primary care physicians/pediatricians | Primary care physicians |
| Participants/response rate | 380/91% | 774/20% | 804/26% | 190/N.A. | 177/89% | 831/59% |
| Prevalence | 12 months | Ever | 12 months | 12 months | 12 months | Ever/12 months |
| Types of aggression and violence | ||||||
| Any type of aggression | 98% | 91%/73% | ||||
| Mild aggression | 98% | 79%/54% | ||||
| Moderate aggression | 75% | 81%/58% | ||||
| Serious aggression | 39% | 23%/11% | ||||
| Non-physical | ||||||
| Verbal abuse | 54% | 92% | 58% | 64% | 56% | 79%/54% |
| Threats | 28% | 72% | 39% | 38%/21% | ||
| Stalking | 14% | 4% | 9%/5% | |||
| Physical | ||||||
| Criminal damage or theft | 36% | 18% | 55%/35% | |||
| Physical attack | 6% | 18% | 6% | 12% | 9% | 21%/10% |
| Injury | <1% | 5% | ||||
| Sexual | ||||||
| Sexual harassment | 48% | 6% | 9% | 17%/10% | ||
| Sexual abuse | 8% | 1% | 1%/<1% | |||
*1Ness GJ, House A, Ness AR: Aggression and violent behaviour in general practice: population based survey in the north of England. BMJ 2000; 320: 1447–8.
*2Miedema B, et al.: Prevalence of abusive encounters in the workplace of family physicians: a minor, major, or severe problem? Can Fam Physician 2010; 56: e101–8.
*3Forrest LE, et al:. A national survey of general practitioners’ experiences of patient-initiated aggression in Australia. Med J Aust 2011; 194: 605–8.
*4Joa TS, Morken T: Violence towards personnel in out-of-hours primary care: a cross-sectional study. Scand J Prim Health Care 2012; 30: 55–60.
*5Carmi-Iluz T, et al.: Verbal and physical violence towards hospital- and community-based physicians in the Negev: an observational study. BMC Health Services Research. 2005; 5: 54. N.A., not available
When interpreting the prevalence rates by work location, it needs to be borne in mind that doctors spend much more time in their practices than on house visits while on call. If we assume that survey participants spent one-tenth of their working time doing on-call shifts, aggressive incidents are relatively most common during those shifts.
When the result that serious forms of aggression are more common during on-call shifts/house visits is put together with the descriptions of a poor sense of safety (especially in participating female doctors), the conclusion has to be that this constitutes a problematic area of primary care physicians’ working activities.
Conclusions
Primary care physicians in Germany should prepare for the fact that they are highly likely in the course of their work to be confronted with forms of aggression. In Australia, a safety program for primary care physicians was introduced by the Royal Australian College of General Practitioners (RACGP) in 2009 (General Practice—a safe place) (21), in Germany the problem does not seem to have been perceived as such in the (specialist) public to date. On the basis of the data collected, however, it does seem advisable to introduce the subject matter into medical education and continuing medical education and to devise strategies for the professional handling of aggression.
In large parts of Germany it is common practice to send out doctors on call, alone and without any safety structure (for example, feedback/reporting systems after a completed visit, service telephones with an alarm function), to mostly unfamiliar patients. On the basis of our data, the conclusion is that this practice requires critical reflection. The use of medically trained drivers, who also accompany the visits, seems sensible from the perspective of safety, but often falls at the hurdle of financial affordability. Especially in view of the large proportion of female doctors entering primary care, solutions will have to be identified that guarantee better safety for doctors at work. Furthermore, additional scientific debate of the subject is desirable, in order to research, for example, triggers of aggression in the context of treatment provided by primary care physicians.
Supplementary Material
Florian Vorderwülbecke, Maximilian Feistle, Michael Mehring, Antonius Schneider, Klaus Linde
The results of the multivariate regression analyses of the associations between doctors’ characteristics and the sense of safety in the five settings are summarized in eTable 1, eTable 2 – 6 show the details of the individual analyses. We need to remember that doctors’ characteristics explain only a small part of the observed variance (Nagelkerke’s r² between 0.05 and 0.20)—that is, the sense of safety is influenced primarily by doctors’ characteristics or factors that were not captured in the survey. Despite this it is obvious that female sex and the experience of a serious incident of aggression in the past were associated with a notably reduced sense of safety in all settings. While age and sense of safety in the practice setting were not associated, older doctors felt significantly safer during house visits and home visits.
The association with a migration background reached significance only for the sense of safety within a group practice (<0.05). In this context it needs to be borne in mind that only 5% of doctors had a migration background; the statistical uncertainty relating to this characteristic is correspondingly high. In the univariate analyses, doctors with a migration background had a significantly reduced sense of safety in all settings. Once the influence of the other characteristics was considered in the multivariate analyses, the influence of the migration background lessened; in the practice and during house visits and home visits, the P values were, however, still between 0.06 and 0.08. Altogether, these results suggest that a migration background is associated with a reduced sense of safety.
Doctors working in singlehanded practices had a slightly reduced sense of safety compared those working in group practices or medical centers. A city location was associated with a reduced sense of safety within the practice as well as during house visits while on call. A patient clientele that was financially straitened tended to be associated with a reduced sense of safety in the univariate analyses, but the multivariate analyses found a significant association only for the practice setting.
The logistic regression showed that the doctors’ characteristics collected in this study do not really provide any clues (pseudo Nagelkerke’s r² = 0.02) about which doctors were affected by a serious incident of aggression and which ones were not. A certain association was seen only for the characteristic of a financially straitened patient clientele.
eTable 2. Ordinal regression for factors influencing the sense of safety in the practice (Nagelkerke’s r² = 0.09).
| Characteristic | Mean (SD) | Mean (SD) | β; p univariate | β; p multivariate |
|---|---|---|---|---|
| yes | no | |||
| Female sex yes/no | 1.44 (0.54) | 1.31 (0.48) | 0.54; <0.001 | 0.48; 0.002 |
| Serious aggression/ violence experienced yes/no | 1.46 (0.55) | 1.33 (0.49) | 0.52; 0.002 | 0.47; 0.008 |
| Age > 55 years yes/no | 1.34 (0.49) | 1.38 (0.52) | 0.17; 0.26 | 0.26; 0.10 |
| Migration background yes/no | 1.56 (0.55) | 1.35 (0.51) | 0.52; 0.009 | 0.57; 0.08 |
| Singlehanded practice yes/no | 1.42 (0.54) | 1.30 (0.47) | 0.52; 0.001 | 0.45; 0.004 |
| City practice yes/no* | 1.45 (0.57) | 1.34 (0.49) | 0.52; 0.02 | 0.57; 0.004 |
| Patient clientele financially weak yes/no | 1.46 (0.55) | 1.34 (0.50) | 0.47; 0.007 | 0.38; 0.04 |
*Coding for multivariable analysis in dummy variables big city yes/no and city yes/no (city without significant influence); [β = 0.29; p = 0.05]);
Mean (SD) = mean value (standard deviation)
eTable 3. Ordinal regression for factors influencing the sense of safety during regular house visit (Nagelkerke’s r² = 0.10).
| Characteristic` | Mean (SD) | Mean (SD) | β; p univariate | β; p multivariate |
|---|---|---|---|---|
| yes | no | |||
| Female sex yes/no | 1.90 (0.75) | 1.57 (0.71) | 0.94; <0.001 | 0.80; <0.001 |
| Serious aggression/ violence experienced yes/no | 1.86 (0.77) | 1.66 (0.73) | 0.54; 0.001 | 0.57; 0.001 |
| Age > 55 years yes/no | 1.59 (0.71) | 1.79 (0.74) | 0.56; <0.001 | 0.48; 0.001 |
| Migration background yes/no | 2.02 (0.80) | 1.68 (0.74) | 0.86; 0.004 | 0.58; 0.06 |
| Singlehanded practice yes/no | 1.72 (0.75) | 1.69 (0.73) | 0.06; 0.66 | 0.05; 0.70 |
| City practice yes/no* | 1.80 (0.78) | 1.67 (0.73) | 0.32; 0.04 | 0.32; 0.07 |
| Patient clientele financially weak yes/no | 1.76 (0.72) | 1.69 (0.75) | 0.24; 0.15 | 0.15; 0.39 |
*Coding for multivariable analysis in dummy variables big city yes/no and city yes/no (city without significant influence); [β = 0.15; p = 0.28]);
Mean (SD) = mean value (standard deviation)
eTable 4. Ordinal regression for factors influencing the sense of safety during home visit (Nagelkerke’s r² = 0.05).
| Characteristic | Mean (SD) | Mean (SD) | β; p univariate | β; p multivariate |
|---|---|---|---|---|
| yes | no | |||
| Female sex yes/no | 1.41 (0.58) | 1.28 (0.48) | 0.48; 0.002 | 0.36; 0.03 |
| Serious aggression/ violence experienced yes/no | 1.39 (0.55) | 1.31 (0.51) | 0.30; 0.09 | 0.31; 0.09 |
| Age > 55 years yes/no | 1.29 (0.50) | 1.37 (0.54) | 0.33; 0.04 | 0.36; 0.03 |
| Migration background yes/no | 1.54 (0.60) | 1.32 (0.52) | 0.84; 0.01 | 0.61; 0.08 |
| Singlehanded practice yes/no | 1.35 (0.51) | 1.31 (0.51) | 0.19; 0.22 | 0.16; 0.38 |
| City practice yes/no* | 1.41 (0.57) | 1.30 (0.51) | 0.42; 0.02 | 0.38; 0.06 |
| Patient clientele financially weak yes/no | 1.42 (0.58) | 1.31 (0.51) | 0.44; 0.02 | 0.29; 0.13 |
*Coding for multivariable analysis in dummy variables big city yes/no and city yes/no (city without significant influence); [β = 0.13; p = 0.49]);
Mean (SD) = mean value (standard deviation)
eTable 5. Ordinal regression for factors influencing the sense of safety during on-call shifts in the practice (Nagelkerke’s r² = 0.10).
| Characteristic | Mean (SD) | Mean (SD) | β; p univariate | β; p multivariate |
|---|---|---|---|---|
| yes | no | |||
| Female sex yes/no | 2.22 (0.89) | 1.88 (0.80) | 0.73; <0.001 | 0.66; <0.001 |
| Serious aggression/ violence experienced yes/no | 2.24 (0.83) | 1.94 (0.85) | 0.69; <0.001 | 0.66; <0.001 |
| Age > 55 years yes/no | 1.99 (0.84) | 2.01 (0.84) | 0.04; 0.81 | 0.03; 0.15 |
| Migration background yes/no | 2.65 (0.92) | 1.98 (0.83) | 1.40; <0.001 | 1.07; 0.002 |
| Singlehanded practice yes/no | 2.09 (0.87) | 1.94 (0.82) | 0.34; 0.02 | 0.27; 0.08 |
| City practice yes/no* | 2.14 (0.88) | 1.98 (0.83) | 0.37; 0.05 | 0.33; 0.12 |
| Patient clientele financially weak yes/no | 2.17 (0.82) | 1.98 (0.85) | 0.47; 0.01 | 0.31; 0.11 |
*Coding for multivariable analysis in dummy variables big city yes/no and city yes/no (city without significant influence); [β = 0.15; p = 0.77]);
Mean (SD) = mean value (standard deviation)
eTable 6. Ordinal regression for factors influencing the sense of safety during house visits while on call (Nagelkerke’s r² = 0.20).
| Characteristic | Mean (SD) | Mean (SD) | β; p univariate | β; p multivariate |
|---|---|---|---|---|
| yes | no | |||
| Female sex yes/no | 2.98 (0.99) | 2.23 (0.88) | 1.49; <0.001 | 1.38; <0.001 |
| Serious aggression/ violence experienced yes/no | 2.74 (0.99) | 2.46 (0.99) | 0.59; <0.001 | 0.67; <0.001 |
| Age > 55 years yes/no | 2.35 (0.94) | 2.65 (1.00) | 0.62; <0.001 | 0.45; 0.002 |
| Migration background yes/no | 3.00 (0.99) | 2.50 (0.99) | -0.84; 0.01 | 0.39; 0.26 |
| Singlehanded practice yes/no | 2.54 (0.99) | 2.52 (0.99) | 0.03; 0.81 | 0.04; 0.76 |
| City practice yes/no* | 2.79 (1.01) | 2.45 (0.97) | 0.64; <0.001 | 0.58; 0.003 |
| Patient clientele financially weak yes/no | 2.66 (0.99) | 2.49 (0.99) | 0.33; 0.06 | 0.18; 0.31 |
*Coding for multivariable analysis in dummy variables big city yes/no and city yes/no (city without significant influence); [β = –0.08; p = 0.55]);
Mean (SD) = mean value (standard deviation)
Key Messages.
In the 12 months preceding the survey, more than half of participating doctors had been exposed to mild/slight or moderate aggression.
More than one in 10 primary care physicians had been confronted with serious aggression or violence in the past 12 months.
Although the general sense of safety within the practice setting was good, only one in three female doctors felt safe during on-call visits.
Concepts for dealing with aggressive behavior should be urgently developed.
A particular need for action exists for house visits while on call.
Acknowledgments
Translated from the original German by Birte Twisselmann, PhD.
The data collection was undertaken in the context of the MD project of Maximilian Feistle at the medical faculty at the Technische Universität München (TUM, Munich Technical University). The study was funded exclusively from financial resources of the Institute of General Practice, University Hospital Klinikum rechts der Isar, TUM.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
References
- 1.Mäulen B. Vorsicht Patient! Immer mehr schwere Gewaltdelikte gegen Ärzte. MMW Fortschr Med. 2013;155:14–20. doi: 10.1007/s15006-013-0266-9. [DOI] [PubMed] [Google Scholar]
- 2.Püschel K, Cordes O. Tödliche Bedrohung als Berufsrisiko. Dtsch Arztebl. 2001;98:A153–A157. [Google Scholar]
- 3.Tolhurst H, Baker L, Murray G, Bell P, Sutton A, Dean S. Rural general practitioner experience of work-related violence in Australia. Aust J Rural Health. 2003;11:231–236. [PubMed] [Google Scholar]
- 4.Alexander C, Fraser J. Occupational violence in an Australian healthcare setting: implications for managers. J Healthc Manag. 2004;49:377–390. [PubMed] [Google Scholar]
- 5.Magin PJ, Adams J, Sibbritt DW, Joy E, Ireland MC. Experiences of occupational violence in Australian urban general practice: a cross-sectional study of GPs. Med J Aust. 2005;183:352–356. doi: 10.5694/j.1326-5377.2005.tb07082.x. [DOI] [PubMed] [Google Scholar]
- 6.Koritsas S, Coles J, Boyle M, Stanley J. Prevalence and predictors of occupational violence and aggression towards GPs: a cross-sectional study. Br J Gen Pract. 2007;57:967–970. doi: 10.3399/096016407782604848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Miedema B, Hamilton R, Tatemichi SR, et al. Monthly incidence rates of abusive encounters for Canadian family physicians by patients and their families. Int J Family Med. 2010 doi: 10.1155/2010/387202. 387202 epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schmidt J, Feltes T. Gewalt gegen Rettungskräfte - Bestandsaufnahme zur Gewalt gegen Rettungskräfte in Nordrhein-Westfalen 2012. www.unfallkasse-nrw.de/fileadmin/server/download/PDF_2012/Gewalt_gegen_Rettungskraefte.pdf. (last accessed on 11 December 2014) [Google Scholar]
- 9.Forrest L, Parker R, Hegarty K, Tuschke H. Patient initiated aggression and violence in Australian general practice. Australian Family Physician. 2010;39:323–326. [PubMed] [Google Scholar]
- 10.Linde K, Friedrichs C, Alscher A, Wagenpfeil S, Meissner K, Schneider A. The use of placebo and non-specific therapies and their relation to basic professional attitudes and the use of complementary therapies among German physicians—a cross-sectional survey. PLoS One. 2014;9 doi: 10.1371/journal.pone.0092938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ziegler A, Hadlak A, Mehlbeer S, König IR. Comprehension of the description of side effects in drug information leaflets—a survey of doctors, pharmacists and lawyers. Dtsch Arztebl Int. 2013;110:669–673. doi: 10.3238/arztebl.2013.0669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Behmann M, Schmiemann G, Lingner H, Kühne F, Hummers-Pradier E, Schneider N. Job satisfaction among primary care physicians: results of a survey. Dtsch Arztebl Int. 2012;109:193–200. doi: 10.3238/arztebl.2012.0193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Unrath M, Zeeb H, Letzel S, Claus M, Pinzón LCE. The mental health of primary care physicians in Rhineland-Palatinate, Germany: the prevalence of problems and identification of possible risk factors. Dtsch Arztebl Int. 2012;109:201–207. doi: 10.3238/arztebl.2012.0201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wandrowski J, Schuster T, Strube W, Steger F. Medical ethical knowledge and moral attitudes among physicians in Bavaria. Dtsch Arztebl Int. 2012;109:141–147. doi: 10.3238/arztebl.2012.0141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koch K, Miksch A, Schürmann C, Joos S, Sawicki PT. The German Health Care System in international comparison: the primary care physicians’ perspective. Dtsch Arztebl Int. 2011;108:255–261. doi: 10.3238/arztebl.2011.0255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jager J, Klatt T, Bliesener T. NRW-Studie Gewalt gegen Polizeibeamtinnen und Polizeibeamte - Abschlussbericht 2013. www.polizei.nrw.de/media/Dokumente/131202_NRW_Studie_Gewalt_gegen_PVB_Abschlussbericht.pdf. (last accessed on 11. December 2014) [Google Scholar]
- 17.Bauer J, Unterbrink T, Hack A, et al. Working conditions, adverse events and mental health problems in a sample of 949 German teachers. Int Arch Occup Envirion Health. 2007;80:442–449. doi: 10.1007/s00420-007-0170-7. [DOI] [PubMed] [Google Scholar]
- 18.Carmi-Iluz T, Peleg R, Freud T, Shvartzman P. Verbal and physical violence towards hospital- and community-based physicians in the Negev: an observational study. BMC Health Services Research. 2005;5 doi: 10.1186/1472-6963-5-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ness GJ, House A, Ness AR. Aggression and violent behaviour in general practice: population based survey in the north of England. BMJ. 2000;320:1447–1448. doi: 10.1136/bmj.320.7247.1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Joa TS, Morken T. Violence towards personnel in out-of-hours primary care: a cross-sectional study. Scand J Prim Health Care. 2012;30:55–60. doi: 10.3109/02813432.2012.651570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Royal Australien College of General Practitioners (RACGP) General practice—a safe place: tips and tools. www.racgp.org.au/your-practice/business/tools/safetyprivacy/gpsafeplace. 2009. (last accessed on 11 December 2014)
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Florian Vorderwülbecke, Maximilian Feistle, Michael Mehring, Antonius Schneider, Klaus Linde
The results of the multivariate regression analyses of the associations between doctors’ characteristics and the sense of safety in the five settings are summarized in eTable 1, eTable 2 – 6 show the details of the individual analyses. We need to remember that doctors’ characteristics explain only a small part of the observed variance (Nagelkerke’s r² between 0.05 and 0.20)—that is, the sense of safety is influenced primarily by doctors’ characteristics or factors that were not captured in the survey. Despite this it is obvious that female sex and the experience of a serious incident of aggression in the past were associated with a notably reduced sense of safety in all settings. While age and sense of safety in the practice setting were not associated, older doctors felt significantly safer during house visits and home visits.
The association with a migration background reached significance only for the sense of safety within a group practice (<0.05). In this context it needs to be borne in mind that only 5% of doctors had a migration background; the statistical uncertainty relating to this characteristic is correspondingly high. In the univariate analyses, doctors with a migration background had a significantly reduced sense of safety in all settings. Once the influence of the other characteristics was considered in the multivariate analyses, the influence of the migration background lessened; in the practice and during house visits and home visits, the P values were, however, still between 0.06 and 0.08. Altogether, these results suggest that a migration background is associated with a reduced sense of safety.
Doctors working in singlehanded practices had a slightly reduced sense of safety compared those working in group practices or medical centers. A city location was associated with a reduced sense of safety within the practice as well as during house visits while on call. A patient clientele that was financially straitened tended to be associated with a reduced sense of safety in the univariate analyses, but the multivariate analyses found a significant association only for the practice setting.
The logistic regression showed that the doctors’ characteristics collected in this study do not really provide any clues (pseudo Nagelkerke’s r² = 0.02) about which doctors were affected by a serious incident of aggression and which ones were not. A certain association was seen only for the characteristic of a financially straitened patient clientele.
eTable 2. Ordinal regression for factors influencing the sense of safety in the practice (Nagelkerke’s r² = 0.09).
| Characteristic | Mean (SD) | Mean (SD) | β; p univariate | β; p multivariate |
|---|---|---|---|---|
| yes | no | |||
| Female sex yes/no | 1.44 (0.54) | 1.31 (0.48) | 0.54; <0.001 | 0.48; 0.002 |
| Serious aggression/ violence experienced yes/no | 1.46 (0.55) | 1.33 (0.49) | 0.52; 0.002 | 0.47; 0.008 |
| Age > 55 years yes/no | 1.34 (0.49) | 1.38 (0.52) | 0.17; 0.26 | 0.26; 0.10 |
| Migration background yes/no | 1.56 (0.55) | 1.35 (0.51) | 0.52; 0.009 | 0.57; 0.08 |
| Singlehanded practice yes/no | 1.42 (0.54) | 1.30 (0.47) | 0.52; 0.001 | 0.45; 0.004 |
| City practice yes/no* | 1.45 (0.57) | 1.34 (0.49) | 0.52; 0.02 | 0.57; 0.004 |
| Patient clientele financially weak yes/no | 1.46 (0.55) | 1.34 (0.50) | 0.47; 0.007 | 0.38; 0.04 |
*Coding for multivariable analysis in dummy variables big city yes/no and city yes/no (city without significant influence); [β = 0.29; p = 0.05]);
Mean (SD) = mean value (standard deviation)
eTable 3. Ordinal regression for factors influencing the sense of safety during regular house visit (Nagelkerke’s r² = 0.10).
| Characteristic` | Mean (SD) | Mean (SD) | β; p univariate | β; p multivariate |
|---|---|---|---|---|
| yes | no | |||
| Female sex yes/no | 1.90 (0.75) | 1.57 (0.71) | 0.94; <0.001 | 0.80; <0.001 |
| Serious aggression/ violence experienced yes/no | 1.86 (0.77) | 1.66 (0.73) | 0.54; 0.001 | 0.57; 0.001 |
| Age > 55 years yes/no | 1.59 (0.71) | 1.79 (0.74) | 0.56; <0.001 | 0.48; 0.001 |
| Migration background yes/no | 2.02 (0.80) | 1.68 (0.74) | 0.86; 0.004 | 0.58; 0.06 |
| Singlehanded practice yes/no | 1.72 (0.75) | 1.69 (0.73) | 0.06; 0.66 | 0.05; 0.70 |
| City practice yes/no* | 1.80 (0.78) | 1.67 (0.73) | 0.32; 0.04 | 0.32; 0.07 |
| Patient clientele financially weak yes/no | 1.76 (0.72) | 1.69 (0.75) | 0.24; 0.15 | 0.15; 0.39 |
*Coding for multivariable analysis in dummy variables big city yes/no and city yes/no (city without significant influence); [β = 0.15; p = 0.28]);
Mean (SD) = mean value (standard deviation)
eTable 4. Ordinal regression for factors influencing the sense of safety during home visit (Nagelkerke’s r² = 0.05).
| Characteristic | Mean (SD) | Mean (SD) | β; p univariate | β; p multivariate |
|---|---|---|---|---|
| yes | no | |||
| Female sex yes/no | 1.41 (0.58) | 1.28 (0.48) | 0.48; 0.002 | 0.36; 0.03 |
| Serious aggression/ violence experienced yes/no | 1.39 (0.55) | 1.31 (0.51) | 0.30; 0.09 | 0.31; 0.09 |
| Age > 55 years yes/no | 1.29 (0.50) | 1.37 (0.54) | 0.33; 0.04 | 0.36; 0.03 |
| Migration background yes/no | 1.54 (0.60) | 1.32 (0.52) | 0.84; 0.01 | 0.61; 0.08 |
| Singlehanded practice yes/no | 1.35 (0.51) | 1.31 (0.51) | 0.19; 0.22 | 0.16; 0.38 |
| City practice yes/no* | 1.41 (0.57) | 1.30 (0.51) | 0.42; 0.02 | 0.38; 0.06 |
| Patient clientele financially weak yes/no | 1.42 (0.58) | 1.31 (0.51) | 0.44; 0.02 | 0.29; 0.13 |
*Coding for multivariable analysis in dummy variables big city yes/no and city yes/no (city without significant influence); [β = 0.13; p = 0.49]);
Mean (SD) = mean value (standard deviation)
eTable 5. Ordinal regression for factors influencing the sense of safety during on-call shifts in the practice (Nagelkerke’s r² = 0.10).
| Characteristic | Mean (SD) | Mean (SD) | β; p univariate | β; p multivariate |
|---|---|---|---|---|
| yes | no | |||
| Female sex yes/no | 2.22 (0.89) | 1.88 (0.80) | 0.73; <0.001 | 0.66; <0.001 |
| Serious aggression/ violence experienced yes/no | 2.24 (0.83) | 1.94 (0.85) | 0.69; <0.001 | 0.66; <0.001 |
| Age > 55 years yes/no | 1.99 (0.84) | 2.01 (0.84) | 0.04; 0.81 | 0.03; 0.15 |
| Migration background yes/no | 2.65 (0.92) | 1.98 (0.83) | 1.40; <0.001 | 1.07; 0.002 |
| Singlehanded practice yes/no | 2.09 (0.87) | 1.94 (0.82) | 0.34; 0.02 | 0.27; 0.08 |
| City practice yes/no* | 2.14 (0.88) | 1.98 (0.83) | 0.37; 0.05 | 0.33; 0.12 |
| Patient clientele financially weak yes/no | 2.17 (0.82) | 1.98 (0.85) | 0.47; 0.01 | 0.31; 0.11 |
*Coding for multivariable analysis in dummy variables big city yes/no and city yes/no (city without significant influence); [β = 0.15; p = 0.77]);
Mean (SD) = mean value (standard deviation)
eTable 6. Ordinal regression for factors influencing the sense of safety during house visits while on call (Nagelkerke’s r² = 0.20).
| Characteristic | Mean (SD) | Mean (SD) | β; p univariate | β; p multivariate |
|---|---|---|---|---|
| yes | no | |||
| Female sex yes/no | 2.98 (0.99) | 2.23 (0.88) | 1.49; <0.001 | 1.38; <0.001 |
| Serious aggression/ violence experienced yes/no | 2.74 (0.99) | 2.46 (0.99) | 0.59; <0.001 | 0.67; <0.001 |
| Age > 55 years yes/no | 2.35 (0.94) | 2.65 (1.00) | 0.62; <0.001 | 0.45; 0.002 |
| Migration background yes/no | 3.00 (0.99) | 2.50 (0.99) | -0.84; 0.01 | 0.39; 0.26 |
| Singlehanded practice yes/no | 2.54 (0.99) | 2.52 (0.99) | 0.03; 0.81 | 0.04; 0.76 |
| City practice yes/no* | 2.79 (1.01) | 2.45 (0.97) | 0.64; <0.001 | 0.58; 0.003 |
| Patient clientele financially weak yes/no | 2.66 (0.99) | 2.49 (0.99) | 0.33; 0.06 | 0.18; 0.31 |
*Coding for multivariable analysis in dummy variables big city yes/no and city yes/no (city without significant influence); [β = –0.08; p = 0.55]);
Mean (SD) = mean value (standard deviation)