Abstract
Roughly one in three individuals is highly susceptible to motion sickness and yet the underlying causes of this condition are not well understood. Despite high heritability, no associated genetic factors have been discovered. Here, we conducted the first genome-wide association study on motion sickness in 80 494 individuals from the 23andMe database who were surveyed about car sickness. Thirty-five single-nucleotide polymorphisms (SNPs) were associated with motion sickness at a genome-wide-significant level (P < 5 × 10−8). Many of these SNPs are near genes involved in balance, and eye, ear and cranial development (e.g. PVRL3, TSHZ1, MUTED, HOXB3, HOXD3). Other SNPs may affect motion sickness through nearby genes with roles in the nervous system, glucose homeostasis or hypoxia. We show that several of these SNPs display sex-specific effects, with up to three times stronger effects in women. We searched for comorbid phenotypes with motion sickness, confirming associations with known comorbidities including migraines, postoperative nausea and vomiting (PONV), vertigo and morning sickness and observing new associations with altitude sickness and many gastrointestinal conditions. We also show that two of these related phenotypes (PONV and migraines) share underlying genetic factors with motion sickness. These results point to the importance of the nervous system in motion sickness and suggest a role for glucose levels in motion-induced nausea and vomiting, a finding that may provide insight into other nausea-related phenotypes like PONV. They also highlight personal characteristics (e.g. being a poor sleeper) that correlate with motion sickness, findings that could help identify risk factors or treatments.
Introduction
Motion sickness is provoked by exposure to a variety of motions (e.g. traveling in cars, boats or planes; amusement park rides; skiing; and riding on camels) (1). Simulators and virtual reality environments can also induce motion sickness (2). Symptoms of motion sickness include dizziness, nausea, vomiting, headache and pallor (3). Sweating, drowsiness, increased salivation, hyperventilation and emotional distress may also occur. Motion sickness is associated with other conditions including migraines, vertigo, postoperative nausea and vomiting (PONV) and chemotherapy-induced nausea and vomiting (CINV) (1,4).
Roughly one in three individuals is highly susceptible to motion sickness and the rest of the population may experience motion sickness under extreme conditions (5). The underlying etiology of motion sickness, however, is not well understood. One theory suggests that motion sickness results from contradictory information the brain receives during motion (1,5). The vestibular system of the inner ear, which senses motion and body position and influences balance, signals ‘moving’ to the brain, while the eye signals ‘stationary’ because the car or boat appears stationary relative to the viewer. The vestibular system is also thought to serve as a sensor of disequilibrium-causing neurotoxins (i.e. a toxin detector) and is believed to trigger the emetic response in order to rid the body of toxins. Thus, motion sickness may be an aberrant trigger of the emetic response. Evidence for the involvement of the vestibular system comes from the observation that individuals with complete loss of the vestibular apparatus, a component of the vestibular system, are immune to motion sickness (1).
A variety of factors influence risk for motion sickness. Women are more susceptible than men (6–9) and younger individuals are at increased risk (6,8). Ancestry may also play a role; there is some evidence that motion sickness occurs more frequently in individual with Asian ancestry compared with European ancestry (10,11). Some variables are situational and/or behavioral. For instance, one study showed that passengers without a view of the road ahead were about three times more likely to experience illness (8) and another report suggested that adopting a wider stance may reduce motion sickness (12). There is also evidence that diet and eating behavior influence risk (7).
Perhaps the most important and least understood variable is the underlying physiological susceptibility of the individual. In women, increased cortisol levels are predictive of motion sickness (13) and susceptibility to motion sickness changes as a function of the menstrual cycle, suggesting that levels of estrogen and other hormones might play a role (14). In both sexes, hyperglycemia is implicated in motion-induced nausea and vomiting (15). There is also some evidence that lower baseline levels of adrenocorticotropic hormone (16), also known as corticotropin, and low sympathetic nervous system activity (17) increases susceptibility. Finally, since antihistamines (e.g. Dramamine), anticholinergics (e.g. scopolamine) and sympathomimetics (e.g. d-amphetamine and ephedrine) are effective treatments, altered baseline activity of the receptors these drugs bind to might influence risk for motion sickness.
Although heritability estimates for motion sickness range from 57–70% (18), genome-wide association studies (GWAS) on this phenotype have not been reported. Here, we describe a large GWAS in which we find 35 regions significantly associated with motion sickness.
Results
Genome-wide association study of motion sickness
We performed a GWAS in 80 494 individuals from the customer base of 23andMe, Inc., a personal genetics company. Participants were of primarily European ancestry and were at most distantly related to each other (i.e. first cousins and closer were excluded). Motion sickness was assessed using online self-report. Participants responded to questions about their degree of car sickness on a scale of 0 (never motion sick), 1 (occasionally), 2 (sometimes) or 3 (frequently) as described in the Materials and Methods. Details about the cohort can be found in Table 1 and in the Materials and Methods. All analyses were controlled for age, sex and five principal components of genetic ancestry. Manhattan and quantile–quantile plots are provided in Figure 1 and Supplementary Material, Figure S1. The genomic control inflation factor was 1.156.
Table 1.
Cohort statistics for motion sickness GWAS
| Group | Total | Male | Female | ≤30 | 31–45 | 46–60 | ≥61 |
|---|---|---|---|---|---|---|---|
| Never | 40 042 | 25 137 | 14 905 | 5510 | 10 707 | 10 592 | 13 233 |
| Occasionally | 24 902 | 11 855 | 13 047 | 4597 | 8451 | 6459 | 5395 |
| Sometimes | 6723 | 3067 | 3656 | 1175 | 2015 | 1759 | 1774 |
| Frequently | 8827 | 3011 | 5816 | 1784 | 3173 | 2310 | 1560 |
| Total | 80 494 | 43 070 | 37 424 | 13 066 | 24 346 | 21 120 | 21 962 |
Degree of motion sickness stratified by sex and age. Females and younger people tend to be more motion sick.
Figure 1.
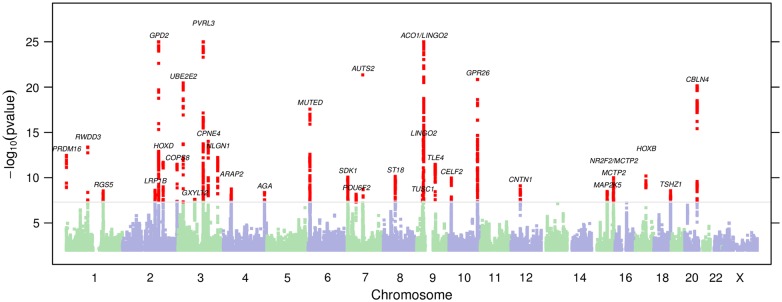
Manhattan plot. The 35 genome-wide-significant regions are listed with the proposed candidate gene; regions that are close together share a label.
Lead SNPs with P-values under 5 × 10−8 for motion sickness are shown in Table 2; 35 regions were significant (Supplementary Material, Fig. S2). The entire dataset is shown in Supplementary Material, Table S1. We created a genetic propensity score based on the number of risk alleles for the 35 index SNPs. Individuals in the top 5% of the distribution (allele dosage of 40.25 or more risk alleles) had an average motion-sickness score 0.546 units higher than those in the bottom 5% (28.37 or fewer risk alleles). The top 5% had 6.37 times increased odds of being ‘frequently’ motion sick as opposed to ‘never’ motion sick as compared with the bottom 5%. The variance in motion sickness explained by the propensity score (which may be inflated as it was assessed in the discovery population) was 0.029.
Table 2.
Genome-wide significant index SNPs
| SNP | Band | Position | Alleles | P-value | Effect | 95% CI | Frequency | Quality | Gene |
|---|---|---|---|---|---|---|---|---|---|
| rs66800491 | 3q13.13 | 109 634,127 | A/G | 4.2 × 10−44 | −0.078 | (−0.089, −0.067) | 0.683 | 0.982 | PVRL3 |
| rs56051278 | 2q24.1 | 157 381 754 | A/G | 1.5 × 10−29 | 0.066 | (0.055, 0.078) | 0.265 | 0.992 | GPD2 |
| rs10970305 | 9p21.1 | 31 372 583 | A/C | 1.0 × 10−27 | −0.057 | (−0.068, −0.047) | 0.505 | 0.956 | ACO1 |
| rs1195218 | 7q11.22 | 68 624 342 | A/G | 4.5 × 10−22 | 0.095 | (0.076, 0.114) | 0.916 | 1.000a | AUTS2 |
| rs705145 | 10q26.13 | 125 226 178 | A/C | 1.4 × 10−21 | −0.051 | (−0.062, −0.041) | 0.638 | 0.997 | GPR26 |
| rs11129078 | 3p24.3 | 22 592 321 | A/G | 3.4 × 10−21 | 0.057 | (0.045, 0.069) | 0.751 | 0.984 | UBE2E2 |
| rs6069325 | 20q13.2 | 54 139 486 | G/T | 7.2 × 10−21 | 0.069 | (0.054, 0.083) | 0.841 | 0.933 | CBLN4 |
| rs2153535 | 6p24.3 | 8 369 679 | C/G | 2.7 × 10−18 | 0.046 | (0.035, 0.056) | 0.480 | 0.969 | MUTED |
| rs2150864 | 9p21.1 | 29 363 265 | A/G | 6.3 × 10−15 | 0.042 | (0.032, 0.053) | 0.348 | 1.000 | LINGO2 |
| rs9834560 | 3q22.1 | 131 716 105 | A/C | 9.7 × 10−15 | −0.041 | (−0.051, −0.031) | 0.610 | 1.000 | CPNE4 |
| rs1858111 | 1p21.3 | 96 089 731 | A/G | 4.1 × 10−14 | −0.039 | (−0.050, −0.029) | 0.567 | 0.999 | RWDD3 |
| rs61759167 | 1p36.32 | 3 091 587 | C/T | 3.5 × 10−13 | 0.047 | (0.034, 0.059) | 0.231 | 0.918 | PRDM16 |
| rs11713169 | 3q26.31 | 173 384 589 | A/C | 5.9 × 10−13 | −0.052 | (−0.067, −0.038) | 0.160 | 0.918 | NLGN1 |
| rs2551802 | 2q31.1 | 177 022 158 | C/G | 2.0 × 10−12 | 0.040 | (0.029, 0.052) | 0.697 | 0.951 | HOXD |
| rs2318131 | 2q37.3 | 237 933 966 | A/C | 3.3 × 10−12 | 0.038 | (0.027, 0.049) | 0.343 | 0.999 | COPS8 |
| rs149951341 | 9q21.31 | 81 268 149 | A/C | 3.4 × 10−12 | −0.050 | (−0.064, −0.036) | 0.798 | 0.794 | TLE4 |
| rs9906289 | 17q21.32 | 46 644 677 | C/T | 6.4 × 10−11 | 0.083 | (0.058, 0.108) | 0.046 | 0.944 | HOXB |
| rs2360806 | 8q11.23 | 53 125 734 | A/C | 7.2 × 10−11 | 0.047 | (0.033, 0.061) | 0.162 | 0.958 | ST18 |
| rs4343996 | 7p22.2 | 3 362 642 | A/G | 8.7 × 10−11 | 0.034 | (0.023, 0.044) | 0.451 | 0.994 | SDK1 |
| rs7170668 | 15q26.2 | 96 014 143 | C/T | 1.0 × 10−10 | 0.035 | (0.024, 0.045) | 0.632 | 1.000 | NR2F2 |
| rs10752212 | 10p14 | 10 917 121 | A/G | 1.1 × 10−10 | 0.034 | (0.024, 0.044) | 0.532 | 0.974 | CELF2 |
| rs7957589 | 12q12 | 41 874 282 | A/T | 7.9 × 10−10 | −0.047 | (−0.061, −0.032) | 0.146 | 0.930 | CNTN1 |
| rs62018380 | 15q26.2 | 95 275 917 | A/C | 1.7 × 10−9 | 0.047 | (0.032, 0.062) | 0.869 | 0.960 | MCTP2 |
| rs6833641 | 4p15.1 | 35 563 786 | C/G | 1.8 × 10−9 | 0.046 | (0.031, 0.062) | 0.852 | 0.870 | ARAP2 |
| rs6946969 | 7q11.22 | 70 211 027 | A/G | 1.9 × 10−9 | 0.033 | (0.022, 0.043) | 0.658 | 0.996 | AUTS2 |
| rs17515225 | 2q22.1 | 141 545 755 | C/T | 2.5 × 10−9 | 0.032 | (0.021, 0.042) | 0.445 | 0.958 | LRP1B |
| rs10514168 | 18q22.3 | 73 098 949 | A/C | 2.7 × 10−9 | −0.047 | (−0.062, −0.031) | 0.854 | 0.861 | TSHZ1 |
| rs4076764 | 1q23.3 | 163 441 286 | C/T | 2.9 × 10−9 | 0.033 | (0.022, 0.044) | 0.649 | 0.933 | RGS5 |
| rs997295 | 15q23 | 68 016 343 | G/T | 3.3 × 10−9 | −0.033 | (−0.044, −0.022) | 0.588 | 0.994a | MAP2K5 |
| rs1378552 | 4q34.3 | 180 356 846 | C/T | 4.3 × 10−9 | −0.032 | (−0.043, −0.022) | 0.322 | 0.998 | AGA |
| rs60464047 | 7p14.1 | 39 418 538 | A/T | 6.7 × 10−9 | −0.043 | (−0.057, −0.028) | 0.850 | 0.956 | POU6F2 |
| rs34311235 | 2q22.2 | 142 767 433 | C/T | 7.9 × 10−9 | 0.032 | (0.021, 0.042) | 0.368 | 0.955 | LRP1B |
| rs1782032 | 9p21.2 | 25 804 285 | A/G | 9.0 × 10−9 | −0.031 | (−0.042, −0.020) | 0.544 | 0.920 | TUSC1 |
| rs1847202 | 3p13 | 72 934 371 | C/T | 2.5 × 10−8 | 0.031 | (0.020, 0.042) | 0.644 | 0.945 | GXYLT2 |
| rs34912216 | 7p22.2 | 4 118 377 | A/G | 2.7 × 10−8 | −0.035 | (−0.047, −0.023) | 0.727 | 0.849 | SDK1 |
Alleles are reported in alphabetical order with respect to the positive strand of build 37 of the human genome. The effect is the change per copy of the second allele on a four-point scale of increasing motion sickness. Frequency is the frequency of the alphabetically second allele in the cohort. Quality is imputation r2 for imputed SNPs, call rate for genotyped SNPs. Gene is a proposed candidate gene in the region.
aGenotyped SNPs.
A few associated SNPs are in regions implicated in eye and ear development or balance. For example, our most significant association is with rs66800491 (P = 4.2 × 10−44), located roughly 1 Mb upstream of PVRL3, which encodes the cell adhesion protein Nectin-3. Loss of PVRL3 expression in both humans and mice results in ocular defects (19). The SNP rs10514168 (P = 2.7 × 10−9) is located downstream of TSHZ1, a gene involved in inner ear development in the mouse (20). Another association is with rs2153535 (P = 2.7 × 10−18), located upstream of MUTED, which is implicated in balance (21). Three additional associated SNPs are near genes with major roles in early development: rs2551802 (P = 2 × 10−12) between HOXD3 and HOXD4; rs9906289 (P = 6.4 × 10−11) in HOXB3; and rs149951341 (P = 3.4 × 10−12) near TLE4. The HOXD SNP is in linkage disequilibrium (LD) (r2 ≈ 0.9) with rs2072590, which is associated with ovarian cancer (22).
Several other associated SNPs are located near genes involved in neurological processes including synapse development and function: rs11713169 (P = 5.9 × 10−13) in NLGN1 encoding neuroligin; rs6069325 (P = 7.2 × 10−21) upstream of CBLN4 encoding a member of the cerebellin precursor protein family; rs62018380 (P = 1.7 × 10−9) downstream of MCTP2, a gene involved in intercellular signal transduction and synapse function; rs7957589 in PDZRN4 (P = 7.9 × 10−10) near CNTN1 (contactin 1), which plays a role in axon guidance during neural development (23); and two independent SNPs, rs4343996 and rs34912216 (P = 8.7 × 10−11 and 2.7 × 10−8, respectively) in SDK1 encoding sidekick-1, a cell adhesion molecule that localizes to synapses. The SNP rs2150864 (P = 6.3 × 10−15) is located ∼1.5 Mb upstream of LINGO2, a gene implicated in essential tremor (24). Additional associated SNPs in or near genes in neurological pathways include: rs9834560 (P = 9.7 × 10−15) in CPNE4 encoding copine-4, and two independent SNPS in or near AUTS2 (rs1195218 and rs6946969 (P = 4.5 × 10−22 and 1.9 × 10−9, respectively).
Other associated SNPs are in regions involved in glucose and insulin homeostasis. For example, the second most significant association we found is with rs56051278 (P = 1.5 × 10−29) in GPD2 that encodes glycerol-3-phosphate dehydrogenase 2, an enzyme implicated in glucose homeostasis. This SNP is in high LD (r2 ≈ 0.8) with rs2116665 (the non-synonymous substitution H264R in GPD2) that was previously associated with free fatty acid and glycerol levels (25). The SNP rs11129078 (P = 3.4 × 10−21) is located downstream of UBE2E2, which encodes a component of the ubiquitin–proteasome system. This system is implicated in the autophagy of pancreatic β-cells that produce insulin and plays important roles in insulin homeostasis (26). In addition, rs705145 (P = 1.4 × 10−21) is located just upstream of GPR26, encoding a G protein-coupled receptor. Mice with a deletion of the GPR26 gene develop hyperphagia and diet-induced obesity, which leads to metabolic complications linked to obesity including glucose intolerance, hyperinsulemia and dyslipidemia (27). The SNP rs4076764 (P = 2.9 × 10−9) is located upstream of RGS5, a regulator of G protein signaling. Loss of RGS5 in the mouse is also associated with hyperphagia (28). Finally, rs7170668 (P = 1 × 10−10) is located upstream of NR2F2 encoding COUP-TFII (chicken ovalbumin upstream promoter transcription factor II), a protein with roles in glucose homeostasis and energy metabolism (29). The remaining associated SNPs are in regions implicated in hypoxia (rs1858111 near RWDD3, P = 4.1 × 10−14); iron homeostasis (rs10970305 near ACO1, P = 1 × 10−27); brown adipose tissue (rs61759167 in PRDM16, P = 3.5 × 10−13); and other less characterized processes: rs2360806 (P = 7.2 × 10−11) in ST18, rs2318131 (P = 3.3 × 10−12) near COPS8, rs60464047 (P = 6.7 × 10−9) in POU6F2, rs10752212 (P = 1.1 × 10−10) near CELF2, rs6833641 (P = 1.8 × 10−9) near ARAP2, rs17515225 and rs34311235 (independently associated, P = 2.5 × 10−9 and 7.9 × 10−9, respectively) in LRP1B, rs1378552 (P = 4.3 × 10−9) in a gene desert on 4q34.3; and rs1782032 (P = 9 × 10−9) near TUSC1, and rs1847202 near SHQ1 and GXYLT2. Finally, rs997295 in MAP2K5 (P = 3.3 × 10−9) is in LD with rs2241423 (r2 ≈ 0.36), which is associated with body mass index (BMI) (30). Some of these SNPs are in or near genes (PRDM16, NRF2, MAP2K5, NLGN1, RGS5) that have also been implicated in the vascular system (31–38).
Enrichment
Analysis of all regions with P < 10−5 using GREAT (39) showed a significant enrichment in regions containing genes involved in fusion of atlas and occipital bones (FDR = 0.002) and abnormal arcus anterior morphology (FDR = 0.038) in mouse. The genes/gene families annotated with one or both of these processes were HOXB, HOXD, TSHZ1 and RARB regions (the SNP near RARB is rs2067120, P = 8.2 × 10−6).
Phenotypic study of motion sickness
We investigated comorbidities with motion sickness within the 23andMe database. Briefly, we looked at partial correlations between each of 695 different phenotypes and motion sickness, controlling for age, sex (where applicable) and five principal components. Table 3 shows selected large correlations exceeding the Bonferroni threshold of P < 6 × 10−5. The maximum P-value for correlations included in the table was 4 × 10−24. Some of the associated phenotypes are known symptoms of motion sickness (e.g. headache) or established comorbidities (migraines, vertigo, PONV and morning sickness). In addition to PONV, other gastrointestinal (GI) phenotypes were also associated with motion sickness [e.g. irritable bowel syndrome (IBS); acid reflux; stomach upset with antidepressants, codeine and non-steroidal anti-inflammatory drugs (NSAIDs); and indigestion with dairy products]. Other associations include poor sleep, poor circulation, altitude sickness, hay fever and neuroticism. Phenotypes associated with lower risk for motion sickness include a history of tobacco use, a good sense of direction, higher BMI and a better ability to handle stress.
Table 3.
Selected partial correlations with motion sickness
| Phenotype | ρ | N |
|---|---|---|
| Dizziness | 0.119 | 24 606 |
| PONV | 0.117 | 25 223 |
| Lightheaded during exercise | 0.114 | 23 434 |
| Vomiting from codeine | 0.114 | 12 176 |
| Altitude sickness | 0.111 | 41 661 |
| Morning sickness | 0.108 | 13 285 |
| Daytime sleepiness | 0.080 | 29 384 |
| Indigestion due to dairy products | 0.071 | 29 659 |
| Hay fever | 0.069 | 22 242 |
| Headache after red wine | 0.066 | 42 485 |
| Vertigo | 0.065 | 54 934 |
| Back pain frequency | 0.065 | 28 808 |
| Neuroticism | 0.063 | 38 711 |
| Rosacea | 0.063 | 24 635 |
| IBS | 0.062 | 34 348 |
| Mosquito bites itching more | 0.061 | 51 292 |
| Greater perceived stress | 0.060 | 32 486 |
| More colds last year | 0.060 | 34 759 |
| Drowsiness from Benadryl | 0.055 | 19 307 |
| Migraines | 0.055 | 72 901 |
| Seasonal affective disorder | 0.051 | 32 273 |
| GI pain from NSAIDs | 0.047 | 29 846 |
| More sleep needed | 0.046 | 39 115 |
| Nausea from antidepressants | 0.046 | 12 079 |
| Adventurous | −0.033 | 34 532 |
| BMI | −0.034 | 75 217 |
| Punctuality | −0.035 | 37 486 |
| Good sense of direction | −0.039 | 46 440 |
| Positive attitude towards self | −0.040 | 34 082 |
| Pack years (cigarettes) | −0.046 | 66 381 |
| Sound sleeper | −0.047 | 48 339 |
| Ability to handle stress | −0.072 | 30 965 |
Partial correlations (ρ) are controlled for age, sex and five principal components. N refers to the number of people with data for both motion sickness and the second trait. Traits are sorted by partial correlation (ρ).
Genetic correlations between motion sickness and related phenotypes
We determined if any of the 35 SNPs associated with motion sickness were also associated with six correlated and clinically important phenotypes (PONV, migraines, hay fever, altitude sickness, morning sickness and vertigo) (Supplementary Material, Table S2). Table 4 shows SNPs associated with these phenotypes with a (Bonferroni-corrected) P-value under 0.05/35 ≈ 0.0014 [under a more stringent threshold of 0.05/(35 × 6) ≈ 0.0002 only the first two are significant]. One motion sickness-associated SNP was significantly associated with migraines: rs61759167 in PRDM16 (P = 1.1 × 10−6). A previous study (40) reported an association between migraines and another SNP in PRDM16, rs2651899, which is in weak LD with rs61759167 (r2 ≈ 0.44). Three motion sickness-associated SNPs were also significantly associated with PONV: rs6833641 near ARAP2, rs1195218 near AUTS2 and rs6069325 near CBLN4. For all four examples, the higher risk allele for migraines or PONV is also the higher risk allele for motion sickness. We see an excess of associations with consistent direction of effect for PONV (27 consistent, P = 0.001) and vertigo (27 consistent, P = 0.001) and a similar trend for migraine (N = 23, P = 0.06). We did not detect individually significant associations between motion sickness-associated SNPs and altitude sickness, hay fever, morning sickness or vertigo. While these data suggest some shared etiology for motion sickness and PONV or migraines, it is difficult to assess whether or not this is due to shared causal SNPs.
Table 4.
Significant associations between motion sickness-associated SNPs and other phenotypes
| Phenotype | SNP | N | P-value | Effect | 95% CI |
|---|---|---|---|---|---|
| Migraine | rs61759167 | 72 901 | 1.1 × 10−6 | 0.08 | (0.051, 0.119) |
| PONV | rs1195218 | 25 223 | 0.00012 | −0.14 | (−0.213, −0.069) |
| PONV | rs6069325 | 25 223 | 0.00079 | 0.09 | (0.038, 0.143) |
| PONV | rs6833641 | 25 223 | 0.00101 | 0.09 | (0.037, 0.148) |
N is the number of people with data for motion sickness and migraines or PONV.
Sex-specific effects
Motion sickness is much more common in women than in men (Table 1) and several of our SNPs show much stronger effects in women than in men. The SNP rs66800491 has a 1.5× larger effect in women (−0.097 versus −0.062) and rs1847202 has a 3× larger effect in women (0.048 versus 0.016) (both SNPs P < 0.05 for interaction, corrected for 35 tests). Overall 26 of the 35 SNPs have estimated larger effects in women than men (binomial P < 0.003; Supplementary Material, Table S3).
Discussion
Here we report 35 novel genome-wide-significant associations for motion sickness (Table 2). Genes in regions associated with motion sickness appear to play roles in eye and ear development, balance and other neurological processes and glucose homeostasis. Two of the genome-wide-significant regions contain hypoxia-inducible genes. We also provide evidence that motion sickness is phenotypically associated with numerous conditions and traits (Table 3).
Since motion sickness is thought to stem from the brain receiving contradictory signals from the inner ear versus the eye (e.g. the inner ear signals ‘moving’ while the eye signals ‘stationary’), it is interesting that a region implicated in eye development (rs56100358 near PVRL3) is our most significant association. Chromosomal rearrangements that lead to loss of PVRL3 expression have been associated with ocular defects in humans and the PVRL3 knockout mouse exhibits lens and other vision problems (19). The associations with regions involved in the inner ear (rs12111385 near MUTED and rs1435985 near TSHZ1) are also interesting since disturbances in the vestibular system of the inner ear, which senses motion and body position and influences balance, are thought to play a central role in motion sickness. It has been suggested that the mouse homolog of MUTED controls the synthesis of otoliths of the vestibular labyrinth of the inner ear (21). Otoliths are sensitive to gravity and linear acceleration and play a role in balance. Mutations in TSHZ1 and deletions in the 18q22.3 region that includes TSHZ1 are associated with congenital aural atresia (41), a spectrum of ear deformities that involve malformation of the external auditory canal. More generally, our enrichment analysis suggests that genes involved in certain aspects of cranial developmental may play an important role in motion sickness. Associations with SNPs in or near genes involved in synapse formation and function (NLGN1, CBLN4, MCTP2, PDZRN4, CNTN1 and SDK1) and other neurological pathways (LINGO2, CPNE4, AUTS2) point to the importance of the brain in motion sickness.
Five associated SNPs are in or near genes implicated in glucose and insulin homeostasis or BMI. Although these SNPs are not in LD with SNPs reported in GWAS of type 2 diabetes (42–47), rs56051278 is in high LD (r2 ≈ 0.8) with rs2116665, a non-synonymous substitution (H264R) in the GPD2 gene. H264R has been associated with increased plasma glycerol and free fatty acid concentrations in a French Canadian population (25). Increased free fatty acid levels are indicative of glucose intolerance and hyperinsulinemia. Although it is unclear why genes involved in glucose and insulin regulation might also play a role in motion sickness, one study suggested that hyperglycemia may be related to the gastrointestinal symptoms of motion sickness (15). In this study, individuals who experienced motion-induced nausea and vomiting had lower levels of insulin than people who did not experience gastrointestinal symptoms. The study further suggested that stable glucose levels might help to relieve motion-induced gastrointestinal upset.
At least two of our associated SNPs are near hypoxia-inducible genes: RGS5 and RWDD3 (encoding the RSUME protein). RSUME promotes the activity of hypoxia-inducible factor 1 (HIF-1α), a master regulator of the hypoxic response (48); RGS5 is an apoptotic stimulator induced by hypoxia in endothelial cells (49). These data suggest a potential relationship between motion sickness and hypoxia. Motion sickness might lead to hypoxia or individuals predisposed to hypoxia might also be more susceptible to motion sickness. Both possibilities are intriguing since our phenotypic analysis suggested an association between motion sickness and altitude sickness, which occurs when individuals become hypoxic at higher altitudes (Table 3).
Among the regional association plots (Supplementary Material), one SNP in particular stands out: rs1195218 near AUTS2. This genotyped SNP has a P-value under 10−20 and no other SNPs in the region have P < 10−6. This lack of signal from LD is not terribly surprising, as none of the three proxy SNPs (r2 > 0.2) for this SNP in 1000 Genomes pass imputation quality control in our data. As the clusters for this SNP look excellent and the call rate is 99.98%, we believe this is a true signal.
Certain phenotypic associations are interesting given what is known about motion sickness. PONV is an established comorbidity of motion sickness (50) and is thought to stem from the anesthetics that are administered for surgery. It may not, therefore, be surprising that motion sickness was also associated with vomiting and/or nausea with use of codeine, antidepressants and NSAIDs. Additional gastrointestinal phenotypes (e.g. IBS, acid reflux and indigestion with dairy products) as well as other drug-related phenotypes like being drowsy when taking Benadryl and feeling jittery when taking Sudafed were also associated with motion sickness. Interestingly, our findings suggest shared genetic susceptibility for both motion sickness and PONV (Table 4).
Some phenotypic associations might provide clues about the etiology of motion sickness (e.g. poor circulation and becoming light headed with exercise) or they might suggest simple remedies for motion sickness such as improving sleep quality. A number of associated phenotypes were related to personality (e.g. neuroticism) or behavior (e.g. smoking). We note, however, that it is difficult to assess causality for these phenotype–phenotype associations. For example, does being a sound sleeper make one less susceptible to being motion sick, or vice versa, or are both related to a third condition? The validity of these novel phenotypic findings is bolstered by the fact that we also detected associations with known symptoms (dizziness and headache) and established comorbidities (PONV, migraines, vertigo and morning sickness) of motion sickness. In some cases we even identified shared genetic factors for motion sickness and related comorbidities (e.g. PONV and migraines). Some of the correlated phenotypes are not established comorbidities or symptoms of motion sickness, however, and do not have an obvious biological relationship to motion sickness.
Our web-based method of capturing phenotypic information allows us to build a very large cohort (e.g. 80 494 individuals in our study), but we may not have obtained a complete picture of an individual's susceptibility to motion sickness. For finding SNPs, the gain in power from having a large sample more than makes up for the reduction in power due to possible misclassification. An additional potential limitation is that we only surveyed individuals about car sickness; future studies should investigate these SNPs in populations phenotyped for other forms of motion sickness. An advantage of our web-based phenotypic collection method is that we can easily investigate whether seemingly related traits have shared underlying genetics. We identified four SNPs simultaneously associated with motion sickness plus PONV or migraines. These findings may provide clues into the etiology of all three conditions and may point to overlapping risk factors or treatments.
Materials and Methods
Human subjects
All participants were drawn from the customer base of 23andMe, Inc., a consumer genetics company. This cohort has been described in detail previously (51,52). Participants provided informed consent and participated in the research online, under a protocol approved by the external AAHRPP-accredited IRB, Ethical & Independent Review Services (E&I Review). Participant data are shared according to community standards that have been developed to protect against breaches of privacy. Currently, these standards allow for the sharing of summary statistics for at most 10 000 SNPs. Association data for a total of 8459 SNPs (P < 1 × 10−5) are shared in this publication (Table 2 and Supplementary Material, Table S1). Data for SNPs that did not reach this threshold are available upon request.
Phenotype collection
Participants were invited to fill out web-based questionnaires, which included four questions about motion sickness during road travel, whenever they logged into their 23andMe accounts. The responses to each question were translated into a motion sickness score of 0 (never), 1 (occasionally), 2 (sometimes) or 3 (frequently). Responses of ‘I am not sure’ or ‘Do not know’ were excluded from the analysis. The questions were prioritized (1–4) and a participant's final score was based on the question they answered that had the highest priority. The questions were:
‘How often do you experience motion sickness while in a car? (Never/Occasionally/Sometimes/Frequently/I am not sure)’
2. ‘Have you experienced motion sickness while riding in a car (car sickness)? (Yes, I do now frequently/Yes, I did frequently, but only as a child/Yes, occasionally/No/Do not know)’
‘As a child, how often did you experience motion sickness while in a car? (Never/Occasionally/Sometimes/Frequently/I am not sure)’
‘Can you read in a moving car without becoming nauseated? (Never/Sometimes/Always/I am not sure)’
Responses to the final question were scored as Never = 3, Sometimes = 1 and Always = 0. The four questions were developed over a period of several years, and customers could have encountered different questions depending on when and how they used the 23andMe product web site. The prioritization was not validated and was chosen to give preference to responses that were more general and current (i.e. giving lower priority to questions about childhood symptoms or the ability to read in a car).
Genotyping and imputation
Participants were genotyped and additional SNP genotypes were imputed against the August 2010 release of the 1000 Genomes data as described previously (53). Briefly, they were genotyped on at least one of three genotyping platforms, two based on the Illumina HumanHap550+ BeadChip, the third based on the Illumina Human OmniExpress+ BeadChip. The platforms included assays for 586 916, 584 942 and 1 008 948 SNPs, respectively. Genotypes for a total of 11 914 767 SNPs were imputed in batches of roughly 10 000 individuals, grouped by genotyping platform. Imputation was performed as given in ref. (53). Prior to the imputation we discarded genotyped SNPs that were not present in the imputation panel. For the GWAS, we added such SNPs back (if they passed quality control), for a total of 7 428 049 SNPs (7 378 897 imputed and 49 152 genotyped). To filter SNPs whose imputation results had changed over time, we performed an analysis of variance test for frequency differences across batches. The quality control criteria for imputed SNPs were a batch effect P-value of at least 10−50, average r2 across batches of at least 0.5, and minimum r2 across batches of at least 0.3. The batch effect filter eliminated SNPs for which the imputation batch explained >0.1% of variance in the imputed dosage. For genotyped SNPs, we required a MAF of at least 0.001, a Hardy–Weinberg P-value of at least 10−20, and a call rate at least 0.9.
Statistical analysis
In order to minimize population substructure while maximizing statistical power, the study was limited to individuals with European ancestry. Ancestry was inferred from the genome-wide genotype data and a principal component analysis that was performed as given in ref. (51,54). The cohort was filtered by relatedness to remove participants at a first cousin or closer relationship. More precisely, no two participants shared >700 cM of DNA identical by descent (IBD; approximately the lower end of sharing between a pair of first cousins). IBD was calculated using the methods described in ref. (55). All P-values were adjusted for genomic control.
The GWAS was performed using likelihood ratio tests for the linear regression
of car sickness on genotype, age, sex and five principal components of genetic ancestry. Genotypes were coded as a dosage from 0–2 (counting the estimated number of minor alleles present for imputed SNPs) or as a count 0, 1 or 2 (also number of minor alleles, for genotyped SNPs). Significant SNPs were grouped into regions with at least 500 Kb between pairs of significant SNPs; the SNP with the lowest P-value in each region was chosen to be the index SNP. As some of the regions were under 1 Mb apart, a joint regression with all index SNPs was run to make sure that they all represented independent signals. To further verify that none of the associations were substantially influenced by batch effects, we computed association tests including additional covariates representing genotyping date. Specifically, we divided participants into 20 equal sized groups based on when their genotype data was generated in order to capture information about genotyping platform as well as temporal variability in platform performance. For the SNPs in Table 2, none of the P-values changed by more than a factor of 10 and all of the associations remained genome-wide significant.
Partial correlation between car sickness C and a phenotype Y were computed by computing the correlation between the residuals produced by regressing both C and Y on age, sex and five principal components, using linear regression even if Y was a binary trait. We did not attempt to quantify the significance of these regressions nor any causality.
Tests of SNPs associated with motion sickness against other correlated traits were done using logistic or linear regressions as appropriate with the same covariates as in the GWAS (except for morning sickness, which dropped sex). The phenotypes studied (PONV, migraines, hay fever, altitude sickness, morning sickness and vertigo) were all case control except for morning sickness, which was scored on a five point scale: None; Mild (occasional bouts of queasiness or nausea, but did not require treatment); Moderate (nausea and some vomiting, but did not require treatment); Severe (severe nausea and vomiting that required treatment); Very severe (requiring hospitalization and intravenous fluid (IV) therapy).
Enrichment analysis using GREAT was conducted on all regions with an index SNP with P < 10−5, where regions were enforced to be 500 Kb apart. Windows of 500 Kb on either side of each index SNP were uploaded into GREAT using default settings.
Supplementary Material
Funding
This work was supported by the participants and by 23andMe. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript. Funding to pay the Open Access publication charges for this article was provided by 23andMe.
Supplementary Material
Acknowledgements
We thank the customers of 23andMe who answered surveys and participated in this research. We also thank all the employees of 23andMe, who together have made this research possible.
Conflict of Interest statement. The authors are or have been employed by 23andMe and own stock options in the company.
References
- 1.Covanis A. (2006) Panayiotopoulos syndrome: a benign childhood autonomic epilepsy frequently imitating encephalitis, syncope, migraine, sleep disorder, or gastroenteritis. Pediatrics, 118, e1237–e1243. [DOI] [PubMed] [Google Scholar]
- 2.Yang S., Schlieski T., Selmins B., Cooper S.C., Doherty R.A., Corriveau P.J., Sheedy J.E. (2012) Stereoscopic viewing and reported perceived immersion and symptoms. Optom. Vis. Sci., 89, 1068–1080. [DOI] [PubMed] [Google Scholar]
- 3.Murdin L., Golding J., Bronstein A. (2011) Managing motion sickness. BMJ, 343, d7430–d7430. [DOI] [PubMed] [Google Scholar]
- 4.Cuomo-Granston A., Drummond P.D. (2010) Migraine and motion sickness: what is the link? Prog. Neurobiol., 91, 300–312. [DOI] [PubMed] [Google Scholar]
- 5.Sherman C.R. (2002) Motion Sickness: review of causes and preventive strategies. J. Travel Med., 9, 251–256. [DOI] [PubMed] [Google Scholar]
- 6.Lawther A., Griffin M.j. (1988) A survey of the occurrence of motion sickness amongst passengers at sea. Aviat. Space Environ. Med., 59, 399–406. [PubMed] [Google Scholar]
- 7.Lindseth G., Lindseth P.d. (1995) The relationship of diet to airsickness. Aviat. Space Environ. Med., 66, 537–541. [PubMed] [Google Scholar]
- 8.Turner M. (1999) Motion sickness in public road transport: passenger behaviour and susceptibility. Ergonomics, 42, 444–461. [DOI] [PubMed] [Google Scholar]
- 9.Lentz J.M., Collins W.E. (1988) Motion sickness susceptibility and related behavioral characteristics in men and women. Aviat Space Env. Med, 59, 399–406. [PubMed] [Google Scholar]
- 10.Stern R.M., Hu S., Uijtdehaage S.H., Muth E.R., Xu L.H., Koch K.L. (1996) Asian hypersusceptibility to motion sickness. Hum. Hered., 46, 7–14. [DOI] [PubMed] [Google Scholar]
- 11.Klosterhalfen S., Kellermann S., Pan F., Stockhorst U., Hall G., Enck P. (2005) Effects of ethnicity and gender on motion sickness susceptibility. Aviat. Space Environ. Med., 76, 1051–1057. [PubMed] [Google Scholar]
- 12.Yu Y., Chung H.C., Hemingway L., Stoffregen T.A. (2013) Standing body sway in women with and without morning sickness in pregnancy. Gait Posture, 37, 103–107. [DOI] [PubMed] [Google Scholar]
- 13.Meissner K., Enck P., Muth E.R., Kellermann S., Klosterhalfen S. (2009) Cortisol levels predict motion sickness tolerance in women but not in men. Physiol. Behav., 97, 102–106. [DOI] [PubMed] [Google Scholar]
- 14.Matchock R.L., Levine M.E., Gianaros P.J., Stern R.M. (2008) Susceptibility to nausea and motion sickness as a function of the menstrual cycle. Womens Health Issues, 18, 328–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mo F.-F., Qin H.-H., Wang X.-L., Shen Z.-L., Xu Z., Wang K.-H., Cai Y.-L., Li M. (2012) Acute hyperglycemia is related to gastrointestinal symptoms in motion sickness: an experimental study. Physiol. Behav., 105, 394–401. [DOI] [PubMed] [Google Scholar]
- 16.Rl K. (1985) Endocrine correlates of susceptibility to motion sickness. Aviat. Space Environ. Med., 56, 1158–1165. [PubMed] [Google Scholar]
- 17.Muth E.R. (2006) Motion and space sickness: intestinal and autonomic correlates. Auton. Neurosci., 129, 58–66. [DOI] [PubMed] [Google Scholar]
- 18.Reavley C.M., Golding J.F., Cherkas L.F., Spector T.D., MacGregor A.J. (2006) Genetic influences on motion sickness susceptibility in adult women: a classical twin study. Aviat. Space Environ. Med., 77, 1148–1152. [PubMed] [Google Scholar]
- 19.Lachke S.A., Higgins A.W., Inagaki M., Saadi I., Xi Q., Long M., Quade B.J., Talkowski M.E., Gusella J.F., Fujimoto A., et al. (2012) The cell adhesion gene PVRL3 is associated with congenital ocular defects. Hum. Genet., 131, 235–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Coré N., Caubit X., Metchat A., Boned A., Djabali M., Fasano L. (2007) Tshz1 is required for axial skeleton, soft palate and middle ear development in mice. Dev. Biol., 308, 407–420. [DOI] [PubMed] [Google Scholar]
- 21.Zhang Q., Li W., Novak E.K., Karim A., Mishra V.S., Kingsmore S.F., Roe B.A., Suzuki T., Swank R.T. (2002) The gene for the muted (mu) mouse, a model for Hermansky–Pudlak syndrome, defines a novel protein which regulates vesicle trafficking. Hum. Mol. Genet., 11, 697–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goode E.L., Chenevix-Trench G., Song H., Ramus S.J., Notaridou M., Lawrenson K., Widschwendter M., Vierkant R.A., Larson M.C., Kjaer S.K., et al. (2010) A genome-wide association study identifies susceptibility loci for ovarian cancer at 2q31 and 8q24. Nat. Genet., 42, 874–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shimoda Y., Watanabe K. (2009) Contactins: emerging key roles in the development and function of the nervous system. Cell Adh Migr, 3, 64–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jasinska-Myga B., Wider C. (2012) Genetics of essential tremor. Parkinsonism Relat. Disord., 18(Supplement 1), S138–S139. [DOI] [PubMed] [Google Scholar]
- 25.St-Pierre J., Vohl M.-C., Brisson D., Perron P., Després J.-P., Hudson T.J., Gaudet D. (2001) A sequence variation in the mitochondrial glycerol-3-phosphate dehydrogenase gene is associated with increased plasma glycerol and free fatty acid concentrations among French Canadians. Mol. Genet. Metab., 72, 209–217. [DOI] [PubMed] [Google Scholar]
- 26.Hartley T., Brumell J., Volchuk A. (2009) Emerging roles for the ubiquitin–proteasome system and autophagy in pancreatic β-cells. Am. J. Physiol. Endocrinol. Metab., 296, E1–E10. [DOI] [PubMed] [Google Scholar]
- 27.Chen D., Liu X., Zhang W., Shi Y. (2012) Targeted Inactivation of GPR26 leads to hyperphagia and adiposity by activating AMPK in the hypothalamus. PLoS ONE, 7, e40764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Deng W., Wang X., Xiao J., Chen K., Zhou H., Shen D., Li H., Tang Q. (2012) Loss of regulator of G protein signaling 5 exacerbates obesity, hepatic steatosis, inflammation and insulin resistance. PLoS ONE, 7, e30256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li L., Xie X., Qin J., Jeha G.S., Saha P.K., Yan J., Haueter C.M., Chan L., Tsai S.Y., Tsai M.-J. (2009) The nuclear orphan receptor COUP-TFII plays an essential role in adipogenesis, glucose homeostasis, and energy metabolism. Cell Metab., 9, 77–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Speliotes E., Willer C. (2010) Association analyses of 249,796 individuals reveal 18 new loci associated with body mass index. Nat. Genet, 42, 937–948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Araujo J.A., Zhang M., Yin F. (2012) Heme oxygenase-1, oxidation, inflammation, and atherosclerosis. Front. Pharmacol., 3, 119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Arndt A.-K., Schafer S., Drenckhahn J.-D., Sabeh M.K., Plovie E.R., Caliebe A., Klopocki E., Musso G., Werdich A.A., Kalwa H., et al. (2013) Fine mapping of the 1p36 deletion syndrome identifies mutation of PRDM16 as a cause of cardiomyopathy. Am. J. Hum. Genet., 93, 67–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Arnold C., Feldner A., Pfisterer L., Hödebeck M., Troidl K., Genové G., Wieland T., Hecker M., Korff T. (2014) RGS5 promotes arterial growth during arteriogenesis. EMBO Mol. Med., 6, 1075–1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lisk C., McCord J., Bose S., Sullivan T., Loomis Z., Nozik-Grayck E., Schroeder T., Hamilton K., Irwin D.C. (2013) Nrf2 activation: a potential strategy for the prevention of acute mountain sickness. Free Radic. Biol. Med., 63, 264–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mizutani H., Okamoto R., Ito M. (2007) Big mitogen-activated protein kinase: a new player in vascular remodeling. Hypertens. Res., 30, 1015–1016. [DOI] [PubMed] [Google Scholar]
- 36.Samarelli A.V., Riccitelli E., Bizzozero L., Silveira T.N., Seano G., Pergolizzi M., Vitagliano G., Cascone I., Carpentier G., Bottos A., et al. (2014) Neuroligin 1 induces blood vessels maturation by cooperating with the α6 integrin. J. Biol. Chem. 10.1074/jbc.M113.530972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Silini A., Ghilardi C., Figini S., Sangalli F., Fruscio R., Dahse R., Pedley R.B., Giavazzi R., Bani M. (2012) Regulator of G-protein signaling 5 (RGS5) protein: a novel marker of cancer vasculature elicited and sustained by the tumor's proangiogenic microenvironment. Cell. Mol. Life Sci., 69, 1167–1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Spiering D., Schmolke M., Ohnesorge N., Schmidt M., Goebeler M., Wegener J., Wixler V., Ludwig S. (2009) MEK5/ERK5 signaling modulates endothelial cell migration and focal contact turnover. J. Biol. Chem., 284, 24972–24980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McLean C.Y., Bristor D., Hiller M., Clarke S.L., Schaar B.T., Lowe C.B., Wenger A.M., Bejerano G. (2010) GREAT improves functional interpretation of cis-regulatory regions. Nat. Biotechnol., 28, 495–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chasman D.I., Schürks M., Anttila V., de Vries B., Schminke U., Launer L.J., Terwindt G.M., van den Maagdenberg A.M.J.M., Fendrich K., Völzke H., et al. (2011) Genome-wide association study reveals three susceptibility loci for common migraine in the general population. Nat. Genet., 43, 695–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ales Dostal J.N. (2006) Identification of 2.3Mb gene locus for congenital aural atresia in 18q22.3 deletion: a case report analyzed by comparative genomic hybridization. Otol. Amp Neurotol. Otol Neurotol, 27, 427–432. [DOI] [PubMed] [Google Scholar]
- 42.Sladek R., Rocheleau G., Rung J., Dina C., Shen L., Serre D., Boutin P., Vincent D., Belisle A., Hadjadj S., et al. (2007) A genome-wide association study identifies novel risk loci for type 2 diabetes. Nature, 445, 881–885. [DOI] [PubMed] [Google Scholar]
- 43.Steinthorsdottir V., Thorleifsson G., Reynisdottir I., Benediktsson R., Jonsdottir T., Walters G.B., Styrkarsdottir U., Gretarsdottir S., Emilsson V., Ghosh S., et al. (2007) A variant in CDKAL1 influences insulin response and risk of type 2 diabetes. Nat. Genet., 39, 770–775. [DOI] [PubMed] [Google Scholar]
- 44.Saxena R., Voight B.F., Lyssenko V., Burtt N.P., de Bakker P.I.W., Chen H., Roix J.J., Kathiresan S., Hirschhorn J.N., Daly M.J., et al. (2007) Genome-wide association analysis identifies loci for type 2 diabetes and triglyceride levels. Science, 316, 1331–1336. [DOI] [PubMed] [Google Scholar]
- 45.Zeggini E., Weedon M.N., Lindgren C.M., Frayling T.M., Elliott K.S., Lango H., Timpson N.J., Perry J.R.B., Rayner N.W., Freathy R.M., et al. (2007) Replication of genome-wide association signals in UK samples reveals risk loci for type 2 diabetes. Science, 316, 1336–1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Scott L.J., Mohlke K.L., Bonnycastle L.L., Willer C.J., Li Y., Duren W.L., Erdos M.R., Stringham H.M., Chines P.S., Jackson A.U., et al. (2007) A genome-wide association study of type 2 diabetes in Finns detects multiple susceptibility variants. Science, 316, 1341–1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Burton P.R., Clayton D.G., Cardon L.R., Craddock N., Deloukas P., Duncanson A., Kwiatkowski D.P., McCarthy M.I., Ouwehand W.H., Samani N.J., et al. (2007) Genome-wide association study of 14,000 cases of seven common diseases and 3,000 shared controls. Nature, 447, 661–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Carbia-Nagashima A., Gerez J., Perez-Castro C., Paez-Pereda M., Silberstein S., Stalla G.K., Holsboer F., Arzt E. (2007) RSUME, a small RWD-containing protein, enhances SUMO conjugation and stabilizes HIF-1α during hypoxia. Cell, 131, 309–323. [DOI] [PubMed] [Google Scholar]
- 49.Jin Y., An X., Ye Z., Cully B., Wu J., Li J. (2009) RGS5, a hypoxia-inducible apoptotic stimulator in endothelial cells. J. Biol. Chem., 284, 23436–23443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Apfel C.C., Heidrich F.M., Jukar-Rao S., Jalota L., Hornuss C., Whelan R.P., Zhang K., Cakmakkaya O.S. (2012) Evidence-based analysis of risk factors for postoperative nausea and vomiting. Br. J. Anaesth., 109, 742–753. [DOI] [PubMed] [Google Scholar]
- 51.Eriksson N., Macpherson J.M., Tung J.Y., Hon L.S., Naughton B., Saxonov S., Avey L., Wojcicki A., Pe'er I., Mountain J. (2010) Web-based, participant-driven studies yield novel genetic associations for common traits. PLoS Genet, 6, e1000993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tung J.Y., Do C.B., Hinds D.A., Kiefer A.K., Macpherson J.M., Chowdry A.B., Francke U., Naughton B.T., Mountain J.L., Wojcicki A., et al. (2011) Efficient replication of over 180 genetic associations with self-reported medical data. PLoS ONE, 6, e23473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Eriksson N., Benton G.M., Do C.B., Kiefer A.K., Mountain J.L., Hinds D.A., Francke U., Tung J.Y. (2012) Genetic variants associated with breast size also influence breast cancer risk. BMC Med. Genet., 13, 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Eriksson N., Tung J.Y., Kiefer A.K., Hinds D.A., Francke U., Mountain J.L., Do C.B. (2012) Novel Associations for hypothyroidism include known autoimmune risk loci. PLoS ONE, 7, e34442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Henn B.M., Hon L., Macpherson J.M., Eriksson N., Saxonov S., Pe'er I., Mountain J.L. (2012) Cryptic distant relatives are common in both isolated and cosmopolitan genetic samples. PLoS ONE, 7, e34267. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


