Abstract
There is growing recognition of the importance of knowledge translation activities in physical therapy to ensure that research findings are integrated into clinical practice, and increasing numbers of knowledge translation interventions are being conducted. Although various frameworks have been developed to guide and facilitate the process of translating knowledge into practice, these tools have been infrequently used in physical therapy knowledge translation studies to date. Knowledge translation in physical therapy implicates multiple stakeholders and environments and involves numerous steps. In light of this complexity, the use of explicit conceptual frameworks by clinicians and researchers conducting knowledge translation interventions is associated with a range of potential benefits. This perspective article argues that such frameworks are important resources to promote the uptake of new evidence in physical therapist practice settings. Four key benefits associated with the use of conceptual frameworks in designing and implementing knowledge translation interventions are identified, and limits related to their use are considered. A sample of 5 conceptual frameworks is evaluated, and how they address common barriers to knowledge translation in physical therapy is assessed. The goal of this analysis is to provide guidance to physical therapists seeking to identify a framework to support the design and implementation of a knowledge translation intervention. Finally, the use of a conceptual framework is illustrated through a case example. Increased use of conceptual frameworks can have a positive impact on the field of knowledge translation in physical therapy and support the development and implementation of robust and effective knowledge translation interventions that help span the research-practice gap.
Notwithstanding significant expansion of its evidence base, multiple studies have demonstrated that the physical therapy profession has often failed to implement evidence-based practice (EBP).1–3 Quality of care is diminished when patients do not receive services that are guided by the best available scientific evidence. In some instances, patients treated by physical therapists receive insufficient, ineffective, or potentially harmful treatment despite available scientific evidence that supports other clinical approaches.4 Knowledge translation (KT)5 interventions* have been proposed as a key means to promote the uptake of research evidence into clinical practice and thus contribute to improved care for patients treated by physical therapists.6,7 Despite this recognition of their importance, there remains debate and uncertainty regarding the best ways to design and implement KT interventions in health care, including physical therapy.8
Bridging the research-practice gap in physical therapy has proved difficult, in large part due to the complexity of designing and implementing successful KT interventions. An important challenge for KT in physical therapy relates to the different types of knowledge that need to be appraised and used to inform treatment decision making. The knowledge base that underlies physical therapist practice is multidimensional and requires physical therapists to master multiple types of knowledge if they are to provide optimal care for their patients.9,10 This knowledge goes beyond technical know-how, as human interactions and patient-clinician relationships are at the heart of the physical therapy profession. The manual, hands-on dimension of the profession is also a significant aspect of practice that influences treatment outcomes. Thus, the knowledge needed to guide physical therapist practice comprises multiple types of evidence drawn from different sources, including quantitative and qualitative research, as well as tacit and clinical knowledge.11 As a result, knowledge coming from higher-order sources of evidence such as meta-analysis and systematic reviews is often insufficient on its own to guide decision making related to best practices.12 Such knowledge has to be combined with clinical observations, patient and family preferences, and clinical judgment in order that well-informed clinical decisions can be enacted.13 Accounting for these diverse sources of knowledge is inherently challenging when implementing KT interventions.14
Gaps between actual practice by physical therapists and the best available research evidence exist in multiple areas. These gaps range from evaluation methods for the cervical spine,15 knowledge and use of low back pain clinical practice guidelines,3 and outcome measures in pediatric physical therapy.16 Those wanting to span the research-practice gap will need to ask the following question: How can we design and implement a high-quality KT intervention that will be more likely to shift clinical practice? Knowledge translation conceptual frameworks represent an important resource for those seeking to answer this question and may be especially valuable guides to the design of effective KT interventions for researchers and clinicians with less KT experience.17–19
In this article, we examine the potential contribution of KT conceptual frameworks to promote the uptake of new scientific evidence in physical therapist practice settings. We argue that, when selected and used appropriately, such frameworks are important resources for designers of KT interventions in physical therapy. We highlight 4 key benefits of using such frameworks, as well as reviewing some of the limits associated with their use. We then explore available KT frameworks in the rehabilitation and physical therapy fields and analyze a sample of 5 frameworks in order to provide guidance to physical therapy researchers and clinicians in the selection of a KT framework. Finally, we illustrate the use of a particular KT conceptual framework, the Ottawa Model of Research Use (OMRU), through a case example.
The Contributions of Conceptual Frameworks in Physical Therapy KT Interventions
Conceptual frameworks consist of a set of linked concepts and propositions that are designed to draw attention to what is important regarding a phenomenon of interest.5 Conceptual frameworks, therefore, can help organize thinking, observation, and interpretation related to a particular phenomenon and function as maps that enhance coherence of empirical inquiry.5,20 Kitson and colleagues defined a conceptual framework as “a set of variables and relationships that should be examined in order to understand a phenomenon.”21(p5) Thus, in the context of KT, a conceptual framework can be conceived of as an overarching representation of key elements to use and acknowledge in the process of designing and implementing a KT intervention, as well as the interrelationships among these elements.
Knowledge translation conceptual frameworks have been developed with the goal of helping to organize and understand the specific components, sequential stages, and contextual factors that need to be taken into account to facilitate successful implementation of a KT intervention and to achieve desired outcomes. The use of conceptual frameworks also can guide project planners in assessing specific barriers to KT interventions and developing strategies to decrease or eliminate these barriers. Similarly, they can support researchers and clinicians to identify specific facilitators and select strategies to enhance them. Highlighting these impacts, several authors have advanced the view that KT activities related to rehabilitation and disability would benefit from increased use of conceptual frameworks.7,22
Despite the development of many KT frameworks over the past 2 decades, their uptake across health care disciplines, including physical therapy, remains limited.8 To gauge the use of conceptual frameworks for KT interventions in physical therapy, we conducted a literature review in January 2014 using CINAHL, MEDLINE, and EMBASE databases and key words pertaining to KT and physical therapy. We identified 8 physical therapy KT studies16,23–29 that used an explicit conceptual framework. This observation is consistent with previous reviews that documented infrequent use of conceptual frameworks in KT implementation studies in physical therapy.30,31 Although infrequently used in KT interventions in physical therapy to date, conceptual frameworks provide multiple benefits for the design of KT interventions. Conceptual frameworks help to: (1) map KT interventions, (2) support evaluation and attention to sustainability, (3) establish common ground and enhance communication among stakeholders, and (4) encourage transparency and clarity about KT methods. These 4 benefits of conceptual frameworks are highlighted below.
Mapping KT Interventions to Ensure That Essential KT Components Are Addressed
Conceptual frameworks cue KT designers to attend to a wide range of considerations that are critical for implementing a successful KT intervention. This is an important contribution, as it is not uncommon for KT interventions to target a single or only a few distinct individual barriers to the integration of evidence in clinical practice but to ignore other significant contextual features.32,33 Individual barriers include clinicians' receptivity or attitudes toward EBP,34 their ability to identify relevant scientific knowledge,35 and their capacity to integrate patient characteristics and preferences into the decision-making process.36 Individual factors, however, are not the only or even most important barriers to KT. Multiple contextual features function as key influencers for the translation of knowledge in health care and have to be considered when designing a KT intervention.37,38 For example, Rutten et al28 identified how external and environmental determinants, including governmental policies and organizational structures and cultures, were important factors to consider in their efforts to promote the uptake of low back pain clinical guidelines in physical therapist practice settings. Conceptual frameworks can help researchers identify and plan for the diverse features that need to be accounted for in planning a robust KT intervention.7,19,20
Supporting Efforts to Evaluate Impacts of the Intervention and to Promote Sustainability
The use of conceptual frameworks also can support efforts to evaluate the impacts of KT interventions. Given that KT conceptual frameworks typically include an evaluative aspect, those therapists using such frameworks will be cued to implement evaluation in their KT interventions. Many KT conceptual frameworks go further and incorporate indicators to guide and structure the evaluation process and help to appraise process and outcomes. Outcome evaluation might, for example, focus on changes of physical therapy clinician behaviors, departmental or organizational functioning, or patient health and well-being. In line with a focus on evaluating outcomes, many KT conceptual frameworks also identify the need to address the issue of sustainability of the KT intervention, beginning in the early planning phases of a project. Attention to sustainability and evaluation are considerations that can increase the probability of sustained impact.39,40 Users of KT frameworks will be primed to include these elements in their interventions.
Establishing Common Ground and Enhancing Communication Among Stakeholders
Knowledge translation interventions frequently involve multiple stakeholders, including researchers, clinicians, managers, and possibly patients. The potential diversity of stakeholders is illustrated by a KT study on fibromyalgia conducted by Brachaniec and colleagues41 that included representatives of patient groups and physical therapy clinicians and researchers. Stakeholders in KT interventions commonly have distinct backgrounds (disciplinary and professional). As a result, they may not always share a common set of understandings and expectations upon which to base the development of a KT intervention.42 Use of a KT framework might help address these differences of expectations and priorities by incorporating a structure and strategies to help identify and discuss the diverse perspectives of stakeholders. In this way, using a framework to plan a KT intervention might help to establish common ground among stakeholders involved in the intervention.
Because conceptual frameworks clearly outline core steps and concepts of a KT intervention, their use also may help enhance quality of communication among stakeholders by providing shared terminology and making project steps and their rationales clearer for all involved. Establishing shared language that enhances communication has been identified as an important predictor of successful KT implementation and sustainability.43 Increased communication also can contribute to a sense of shared “ownership” of the intervention. In turn, a greater sense of ownership will support an environment in which stakeholders feel welcome to offer suggestions for improvement, raise questions or concerns during the planning phase, and contribute to efforts to develop and sustain a shared action plan.7,14
Encouraging Transparency and Clarity About KT Methods
The use of conceptual frameworks also might contribute to transparency about the implementation process of KT interventions. Currently, many authors of physical therapy KT studies do not include a justification for their intervention design or their selection of specific KT strategies when they publish their results. Scott and colleagues44 reviewed 11 published physical therapy KT interventions studies and found that all were missing important methodological details concerning the KT intervention implemented. These authors also raised questions regarding an apparent over-reliance on educational strategies (ie, educational meetings, workshops, or brochures), without clear rationales offered for these approaches.44 Knowledge translation conceptual frameworks are not the only recourse for addressing these issues. They are, however, an important avenue to promote transparency and clarity about rationales and design decisions and to improve the quality of KT reports. This assertion is consistent with research by Moher et al,45 who demonstrated that the use of formal methodological guidelines increases the quality of reports of randomized controlled trials. Because frameworks function as scaffolding for KT interventions, they can assist manuscript reviewers and readers to understand the steps taken to select and implement particular KT strategies.46 Readers also will be better able to judge the applicability of these findings to their local setting.
We have sought to demonstrate the benefits of using KT conceptual frameworks and the roles they can play to increase the likelihood of implementing a successful KT intervention in physical therapy.
KT Conceptual Frameworks and Their Limits
Despite the benefits outlined above, it is important to acknowledge that conceptual frameworks are not guarantors of successful KT interventions. Several limitations are associated with the use of KT conceptual frameworks.20,47,48 We highlight here 2 primary limitations: (1) the lack of empirical evidence demonstrating the value of KT conceptual frameworks and (2) the risks associated with over-reliance on or misapplication of frameworks.
Difficulty in Demonstrating Benefits of Conceptual Frameworks in KT Intervention
Appropriately enough given KT's focus on evidence, concern has been voiced regarding the evidence base underlying the use of KT frameworks. It has been noted that there is limited evidence demonstrating that KT interventions designed using a conceptual framework—or a specific theory—are superior to those that are not.44 As the value of using a range of conceptual frameworks has yet to be confirmed empirically, some authors have suggested the use of an approach based on common sense.50 This recommendation was advanced for the use of psychological theories to underpin behavioral change studies. A similar argument could be made in regard to KT frameworks, as their evidence base also is limited.49 While acknowledging the lack of empirical evidence on this question, we believe that the arguments in favor of conceptual frameworks discussed above are sufficient to warrant that researchers strongly consider their use. Limited knowledge about the relative effectiveness of using or not using conceptual frameworks also may be the product of difficulty in comparing published studies due to limited methodological details available in most study reports.50 Further studies assessing the comparative effectiveness of KT studies using conceptual frameworks versus pragmatic approaches would help to address this question.30
Misapplication of Conceptual Frameworks
Like all tools, KT conceptual frameworks can be misapplied.31,51 Perhaps the most important limitation of conceptual frameworks is that users may use them in a simplistic or mechanistic fashion and thus fail to develop an effective KT intervention. Such frameworks should be understood as guides, not recipes. Researchers and clinicians who plan to implement a KT intervention will benefit from reading widely about KT, conferring about their study with colleagues and mentors experienced in KT, and even taking courses related to KT science. Developing a broader understanding of the field of KT thus can help guard against overreliance on or formulaic use of frameworks that would limit creativity and responsiveness on the part of KT implementers.19,52 In this sense, conceptual frameworks will be most effective when used in a careful and reflexive manner, including an acknowledgment of their intended purpose and inherent limitations.
Choosing a Conceptual Framework
Physical therapy clinicians and researchers who want to use a conceptual framework for their KT intervention have many options from which to choose. Wilson and colleagues53 identified more than 30 frameworks and theoretical models that can be used to guide a KT intervention in health care. To illustrate the diverse frameworks available for physical therapy clinicians and researchers, we selected examples of KT frameworks used across physical therapy, rehabilitation, and health care domains. Twenty-seven recent articles that use or describe the use of KT conceptual frameworks are presented in Table 1. As we did not aim at performing a systematic review of the literature, this table consists of a sample of pertinent frameworks that are currently in use by KT implementers in health care.
Table 1.
Examples of Conceptual Frameworks From Published Articlesa
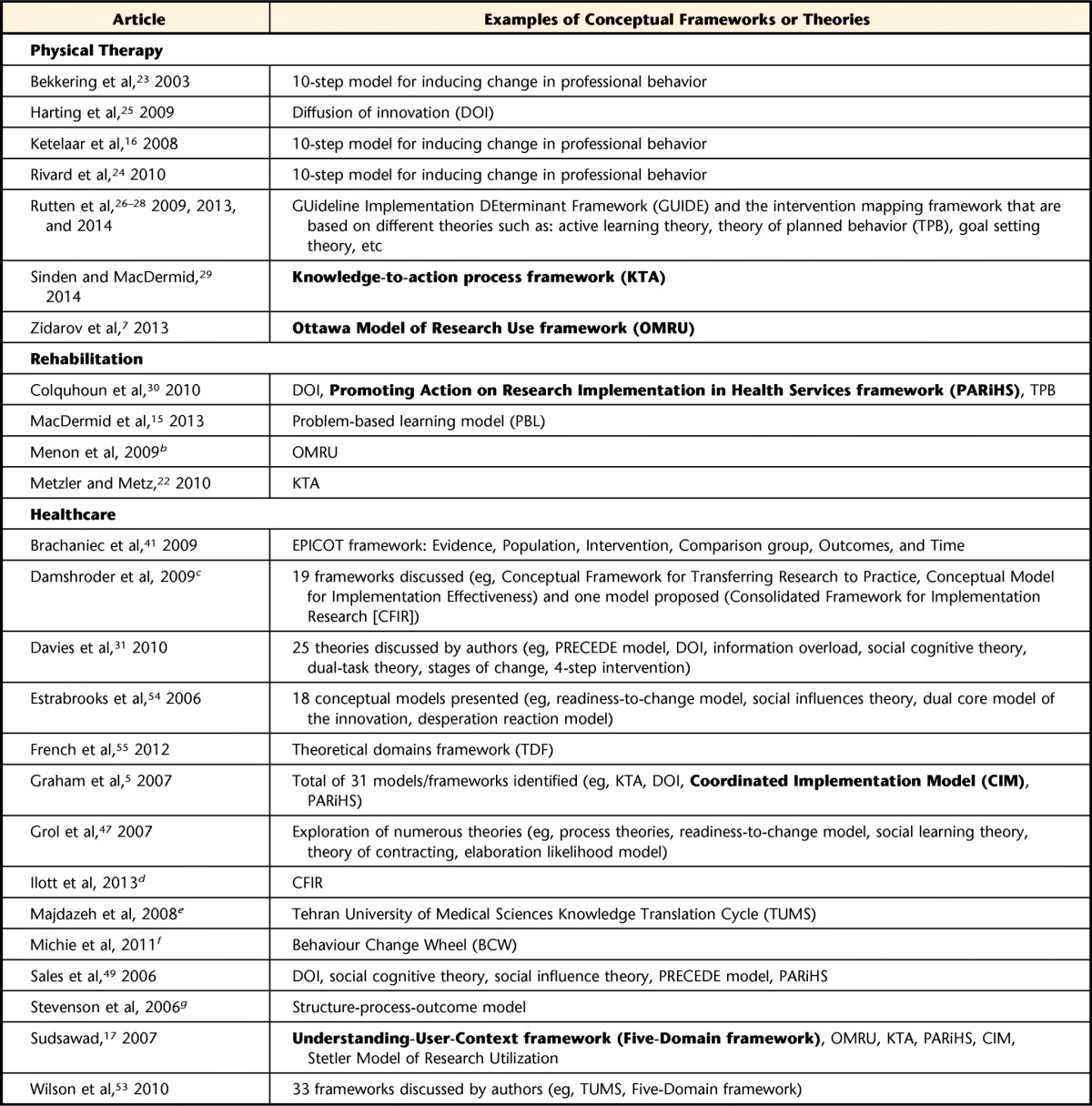
The 5 frameworks in bold type are analyzed in Table 2.
b Menon A, Korner-Bitensky N, Kastner M, et al. Strategies for rehabilitation professionals to move evidence-base knowledge into practice: a systematic review. J Rehabil Med. 2009;41:1024–1032.
c Damschroder LJ, Aron DC, Keith RE, et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation sciences. Implement Sci. 2009;40:50.
d Ilott I, Gerrish K, Booth A, Field B. Testing the consolidated framework for implementation research on health care innovations from South Yorkshire. J Eval Clin Pract. 2013;19:915–924.
e Majdzadeh R, Sadighi J, Nejat S, et al. Knowledge translation for research utilization: design of a knowledge translation model at Tehran University of Medical Sciences. J Contin Educ Health Prof. 2008;28:270–277.
f Michie S, van Stralen MM, West R, et al. The Behaviour Change Wheel: a new method for characterizing and designing behavior change interventions. Implement Sci. 2011;6:42.
g Stevenson KM, Dahl JL, Berry PH, et al. Institutionalizing effective pain management practices: practice change programs to improve the quality of pain management in small health care organizations. J Pain Symptom Manage. 2006;31:248–261.
To date, there has been little analysis comparing the attributes of specific KT frameworks. There is continuing uncertainty about the relative strengths and limits of different KT frameworks, raising questions about which one would be the best to select for a given KT project.20,54 Each framework draws attention to different components of the KT process. As a result, particular frameworks likely have strengths and weaknesses and may be differently suited for application in particular contexts or to answer specific research questions.55
To address this uncertainty, we sought to evaluate a sample of currently available conceptual frameworks for their potential application for KT in the physical therapy field. To do so, we reviewed the more common barriers to EBP cited in current physical therapy literature. We then associated, for each of these barriers, attributes of KT conceptual frameworks aiming to address them. As more than 30 frameworks were identified through our literature search, we chose to analyze 5 KT conceptual frameworks from among those more commonly used in the context of rehabilitation and disability17: Understanding-User-Context framework (Five-Domain framework [5-DF]),56 OMRU,57,58 knowledge-to-action process framework (KTA),5,18 Promoting Action on Research Implementation in Health Services framework (PARiHS),59,60 and the Coordinated Implementation Model (CIM).61 The results of this exercise are presented in Table 2. Although only 5 example frameworks are presented here, the elements of the analysis presented in Table 2 could be used by researchers and clinicians to assess how other frameworks address barriers to EBP in physical therapy.
Table 2.
Analysis of 5 KT Conceptual Frameworksa
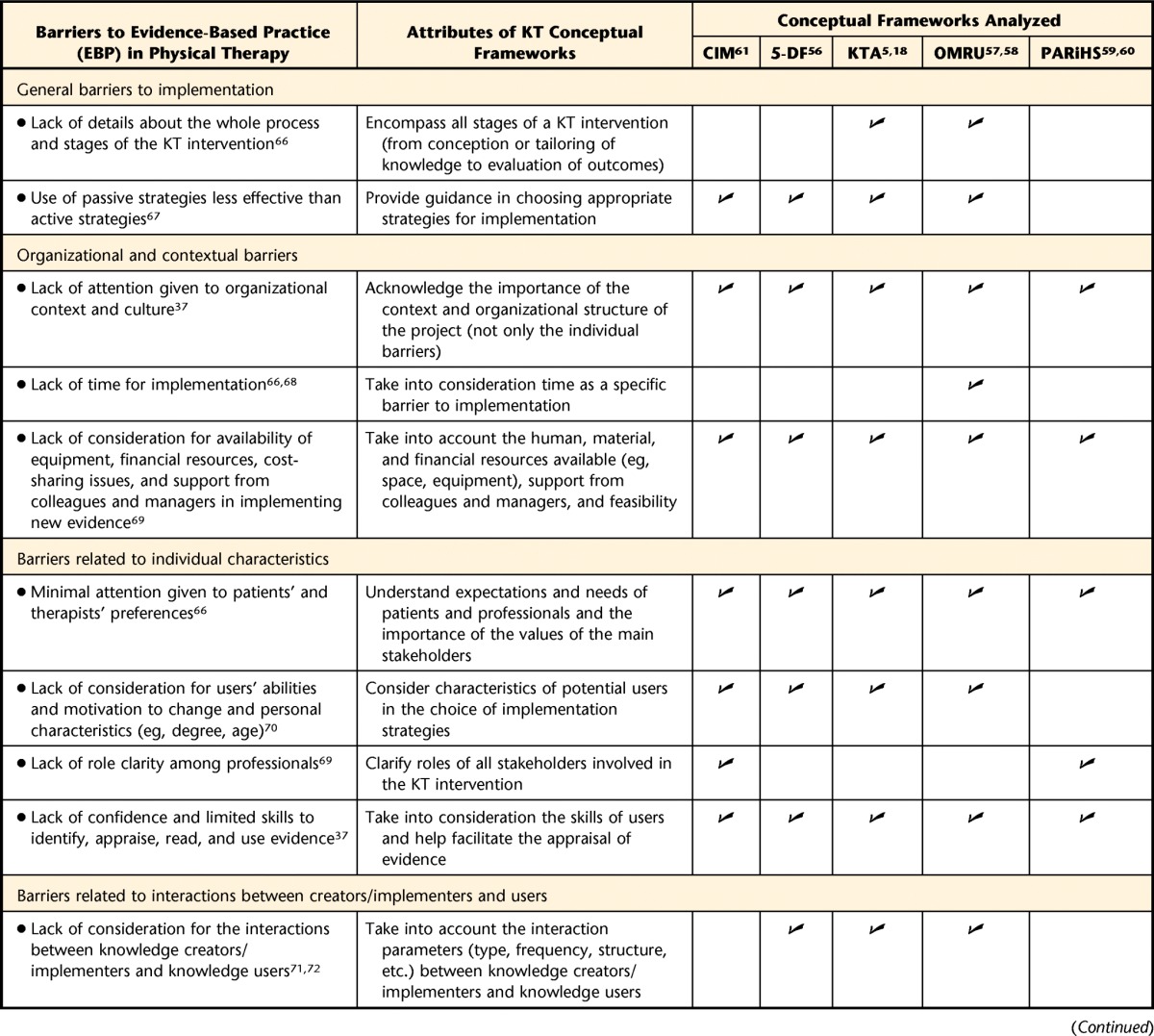
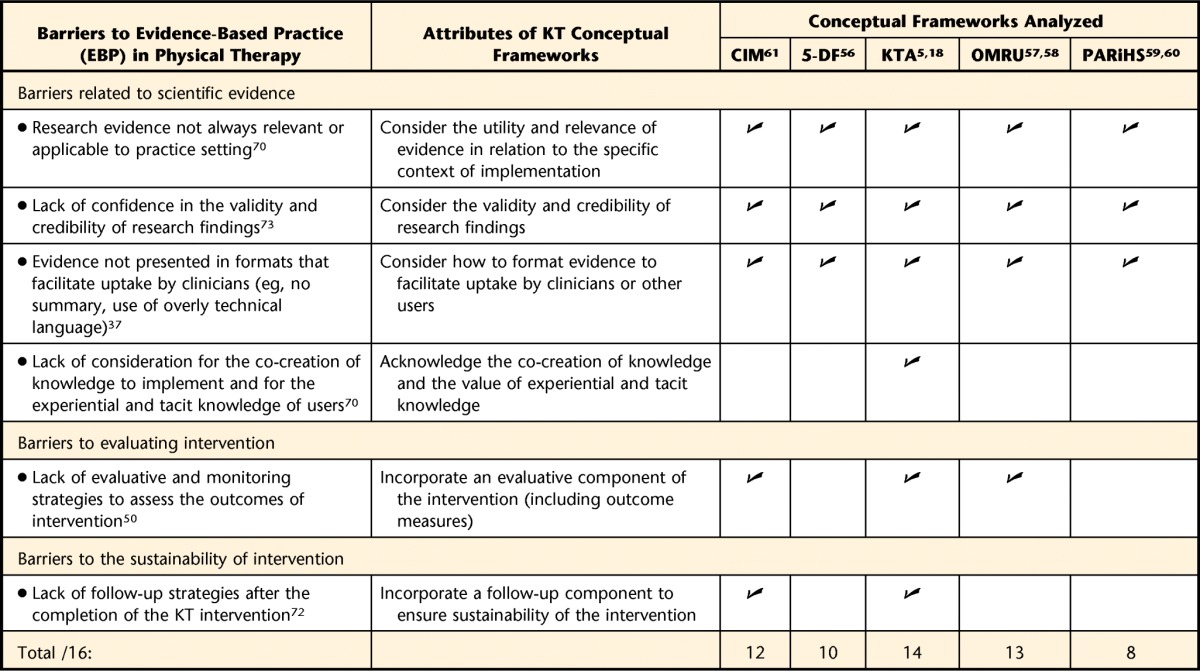
KT=knowledge translation, CIM=Coordinated Implementation Model,61 5-DF=Understanding-User-Context framework (Five-Domain framework),56 KTA=knowledge-to-action process framework,5,18 OMRU=Ottawa Model of Research Use,57,58 PARiHS=Promoting Action on Research Implementation in Health Services framework.59,60 A check mark was attributed to a framework when it addressed a specific barrier to EBP in physical therapy.
The first column of Table 2 presents specific barriers to EBP found in the physical therapy literature. The second column describes attributes or characteristics of KT conceptual frameworks addressing these barriers. The 5 columns on the right-hand side of the table present our analysis of the 5 selected frameworks. Two authors (A.H. and M-J.G.) independently reviewed the original texts presenting detailed features of each of the 5 frameworks. These evaluations were then compared, and a consensus was reached. A check mark was attributed to a framework when it presented the specific attribute listed in the second column of Table 2 (ie, when it addressed a specific barrier to EBP in physical therapy). Thus, check marks indicate when a framework fulfills the characteristics of the second column.
As illustrated in Table 2, none of the 5 selected conceptual frameworks account for all of the barriers to EBP implementation in physical therapy. In that they address the greatest number of barriers to EBP, the OMRU and the KTA frameworks appear to be promising frameworks for planning KT interventions in physical therapy. To illustrate how such conceptual frameworks can be used, a case example is presented below in which the OMRU framework is being applied in a KT intervention.
Applying the OMRU Framework to a KT Intervention Project
Our team is currently conducting a knowledge exchange project with ethics educators in physical therapy and occupational therapy programs across Canada. This project originated from an identified gap in the literature about what is actually taught and what should be taught in Canadian university ethics curricula (Laliberté et al, unpublished research).62 Originally, a straightforward KT strategy was chosen: a 1-day workshop bringing together all physical therapy and occupational therapy ethics educators in Canada. In the early phases of the project, however, our team identified the need to develop a more sophisticated KT approach and elected to adopt the OMRU framework to structure the intervention. The OMRU was chosen because it encompasses all stages of a KT intervention (from conception and tailoring of knowledge to evaluation of outcomes). Hence, this framework is particularly useful to develop a more rigorous KT design structure. It also helped the whole team (researchers, ethics educators, and program coordinators) understand and follow each step of the KT process. The framework provided useful guidance for selecting appropriate strategies for implementing our KT intervention. It also drew attention to how organizational and contextual barriers (eg, regulations and policies, remuneration systems, lack of time), as well as barriers related to individual characteristics (eg, awareness, attitudes, concerns, current practices) can influence the KT process. Finally, and unlike most other KT conceptual frameworks, the OMRU highlighted core elements of knowledge exchange that needed to be addressed in order to support an interactive process.63 As a result, many significant elements were changed or added to our original KT intervention planning. We highlight key changes below.
When looking at the “potential adopters” section of the framework, we realized that we lacked information about who was teaching ethics content in the different Canadian programs and under which conditions. We thus developed a survey to learn about ethics teachers and what they taught. With this survey, we learned that most educators did not have any postgraduate training in ethics (65%) and that most were not full-time university teachers (Laliberté et al, unpublished research). These findings changed the way we framed our 1-day workshop, putting more emphasis on practical and concrete day-to-day problems in ethics teaching. To learn about participants' expectations, we solicited input prior to the workshop and adjusted the planning in light of what we heard (including adding more time for open discussion and networking). The OMRU also guided our team toward integrating longer-lasting interventions to ensure sustainability. We thus developed a “wiki platform.” A “wiki” is a collaborative web-based tool that allows groups to jointly create and exchange knowledge on a given subject.64 The use of the wiki aims to promote continued engagement of participants after the workshop is completed and to create ongoing exchanges among participants.
The OMRU framework facilitated the identification of key steps for evaluation of the KT intervention, including use of the wiki and follow-up interviews with participants to explore whether they had changed their teaching as a result of the KT intervention. Overall, using the OMRU framework helped our team to select and tailor appropriate strategies to carry out our KT project. For each of the specific barriers identified, a strategy was chosen to address it. Evaluation methods also were integrated into the project design from an early stage of its development. This case example illustrates how the use of the OMRU helped our team navigate smoothly through the progression of a KT project.
Conclusion
In sum, KT conceptual frameworks have the potential to promote systematic and well-planned KT interventions in physical therapy. It has been argued that guidance is currently lacking “to help healthcare researchers, practitioners, or managers make decisions about what implementation strategies to use, in which contexts, and with what groups of stakeholders.”19(pS79) Indeed, planning how to integrate research into practice has been described as a “black box.”19 Conceptual frameworks for KT in physical therapy can help signpost the process of KT design and implementation, thus helping to plan, implement, and evaluate KT interventions.65
Conceptual frameworks, however, do not take away the need for thoughtful and creative planning and design of KT interventions. Those seeking to apply a conceptual framework will benefit from training in KT science and mentoring from experienced colleagues to help them optimize the KT process and avoid poor-quality interventions. They also will need to carefully examine available KT frameworks in order to select a robust framework that corresponds to the reality of their project and the implementation context. In order to support this selection process, we have analyzed a sample of 5 conceptual frameworks and considered whether they address key barriers to evidence uptake in physical therapy. Conceptual frameworks can help structure the design and implementation process in ways that promote successful KT interventions. Such frameworks are an important resource to advancing EBP in physical therapy and bridging the lingering research-practice gap.
Footnotes
Ms Hudon and Mr Gervais provided concept/idea/project design and data collection and analysis. Ms Hudon ensured project management. All authors provided writing and consultation (including review of manuscript before submission).
The authors thank the members of a journal club at McGill University for their valuable comments on a previous version of the manuscript. Ms Hudon is supported by a doctoral fellowship from the Fonds de Recherche du Québec en Santé (FRQ-S) and from the MENTOR program in collaboration with the Canadian Institutes of Health Research and the Quebec Research Rehabilitation Network (REPAR). Mr Gervais is supported by the CJM-IU-UQÀM Chair on Knowledge Translation in the Field of Child and Family Welfare and the KT Canada Student Fellowship and Training Program. Dr Hunt is supported by a Research Scholar Award from FRQ-S. This research was funded by Dominion of Canada General Insurance and administered by the Physiotherapy Foundation of Canada.
According to the Canadian Institutes of Health Research, KT can be defined as iterative processes that include synthesis, dissemination, and exchange between researchers and knowledge users in order to improve the usefulness of scientific knowledge and its application into clinical practices.
References
- 1. Schreiber J, Stern P. A review of the literature on evidence-based practice in physical therapy. Int J Allied Health Sci Pract. 2005;3:1–10. [Google Scholar]
- 2. Jette AM. The peril of inadequate evidence. Phys Ther. 2005;85:302–303. [PubMed] [Google Scholar]
- 3. Derghazarian T, Simmonds MJ. Management of low back pain by physical therapists in Quebec: how are we doing? Physiother Can. 2011;63:464–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McGlynn EA, Asch SM, Adams J, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348:2635–2645. [DOI] [PubMed] [Google Scholar]
- 5. Graham ID, Tetroe J; KT Theories Research Group. Some theoretical underpinnings of knowledge translation. Acad Emerg Med. 2007;14:936–941. [DOI] [PubMed] [Google Scholar]
- 6. Gross DP, Lowe A. Evaluation of a knowledge translation initiative for physical therapists treating patients with work disability. Disabil Rehabil. 2009;31:871–879. [DOI] [PubMed] [Google Scholar]
- 7. Zidarov D, Thomas A, Poissant L. Knowledge translation in physical therapy: from theory to practice. Disabil Rehabil. 2013;35:1571–1577. [DOI] [PubMed] [Google Scholar]
- 8. Grimshaw J, Thomas R, MacLennan G, et al. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess. 2004;8:iii–iv, 1–72. [DOI] [PubMed] [Google Scholar]
- 9. Jensen GM, Gwyer J, Shepard KF, Hack LM. Expert practice in physical therapy. Phys Ther. 2000;80:28–43. [PubMed] [Google Scholar]
- 10. Shepard KF, Hack LM, Gwyer J, Jensen GM. Describing expert practice in physical therapy. Qual Health Res. 1999;9:746–758. [DOI] [PubMed] [Google Scholar]
- 11. Dijkers MP, Murphy SL, Krellman J. Evidence-based practice for rehabilitation professionals: concepts and controversies. Arch Phys Med Rehabil. 2012;93:S164–S176. [DOI] [PubMed] [Google Scholar]
- 12. DiCenso A, Bayley L, Haynes RB. Accessing pre-appraised evidence: fine-tuning the 5S model into a 6S model. Evid Based Nurs. 2009;12:99–101. [DOI] [PubMed] [Google Scholar]
- 13. Bithell C. Evidence-based physiotherapy: some thoughts on “best evidence.” Physiotherapy. 2000;86:58–59. [Google Scholar]
- 14. Graham I, Logan J, Tetroe J. Models of implementation in nursing. In: Cullum N, Ciliska D, Haynes R, Marks S, eds. Evidence-Based Nursing. Oxford, United Kingdom: Blackwell Publishing Ltd; 2008:231–243. [Google Scholar]
- 15. MacDermid JC, Walton DM, Côté P, et al. Use of outcome measures in managing neck pain: an international multidisciplinary survey. Open Orthop J. 2013;7:506–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ketelaar M, Russell DJ, Gorter JW. The challenge of moving evidence-based measures into clinical practice: lessons in knowledge translation. Phys Occup Ther Pediatr. 2008;28:191–206. [DOI] [PubMed] [Google Scholar]
- 17. Sudsawad P. Knowledge Translation: Introduction to Models, Strategies, and Measures. Austin, TX: Southwest Educational Development Laboratory, National Center for the Dissemination of Disability Research; 2007. [Google Scholar]
- 18. Graham ID, Logan J, Harrison MB, et al. Lost in knowledge translation: time for a map? J Contin Educ Health Prof. 2006;26:13–24. [DOI] [PubMed] [Google Scholar]
- 19. Rycroft-Malone J. Theory and knowledge translation: setting some coordinates. Nurs Res. 2007;56(4 suppl):S78–S85. [DOI] [PubMed] [Google Scholar]
- 20. Francis J. Designing theoretically-informed implementation interventions. Implement Sci. 2006;1:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kitson AL, Rycroft-Malone J, Harvey G, et al. Evaluating the successful implementation of evidence into practice using the PARiHS framework: theoretical and practical challenges. Implement Sci. 2008;3:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Metzler MJ, Metz GA. Translating knowledge to practice: an occupational therapy perspective. Aust Occup Ther J. 2010;57:373–379. [DOI] [PubMed] [Google Scholar]
- 23. Bekkering GE, Engers AJ, Wensing M, et al. Development of an implementation strategy for physiotherapy guidelines on low back pain. Aust J Physiother. 2003;49:208–214. [DOI] [PubMed] [Google Scholar]
- 24. Rivard LM, Russell DJ, Roxborough L, et al. Promoting the use of measurement tools in practice: a mixed-methods study of the activities and experiences of physical therapist knowledge brokers. Phys Ther. 2010;90:1580–1590. [DOI] [PubMed] [Google Scholar]
- 25. Harting J, Rutten GM, Rutten ST, Kremers SP. A qualitative application of the diffusion of innovations theory to examine determinants of guideline adherence among physical therapists. Phys Ther. 2009;89:221–232. [DOI] [PubMed] [Google Scholar]
- 26. Rutten GM, Harting J, Bartholomew LK, et al. Evaluation of the theory-based Quality Improvement in Physical Therapy (QUIP) programme: a one-group, pre-test post-test pilot study. BMC Health Serv Res. 2013;13:194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rutten GM, Kremers SP, Rutten ST, Harting J. A theory-based cross-sectional survey demonstrated the important role of awareness in guideline implementation. J Clin Epidemiol. 2009;62:167–176. [DOI] [PubMed] [Google Scholar]
- 28. Rutten GM, Harting J, Bartholomew LK, et al. Development of a theory- and evidence-based intervention to enhance implementation of physical therapy guidelines for the management of low back pain. Arch Public Health. 2014;72:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Sinden K, MacDermid JC. Does the knowledge-to-action (KTA) framework facilitate physical demands analysis development for firefighter injury management and return-to-work planning? J Occup Rehabil. 2014;24:146–159. [DOI] [PubMed] [Google Scholar]
- 30. Colquhoun HL, Letts LJ, Law MC, et al. A scoping review of the use of theory in studies of knowledge translation. Can J Occup Ther. 2010;77:270–279. [DOI] [PubMed] [Google Scholar]
- 31. Davies P, Walker AE, Grimshaw JM. A systematic review of the use of theory in the design of guideline dissemination and implementation strategies and interpretation of the results of rigorous evaluations. Implement Sci. 2010;5:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Grimshaw JM, Eccles MP, Lavis JN, et al. Knowledge translation of research findings. Implement Sci. 2012;7:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rycroft-Malone J. Evidence-informed practice: from individual to context. J Nurs Manag. 2008;16:404–408. [DOI] [PubMed] [Google Scholar]
- 34. Shuval K, Berkovits E, Netzer D, et al. Evaluating the impact of an evidence-based medicine educational intervention on primary care doctors' attitudes, knowledge and clinical behaviour: a controlled trial and before and after study. J Eval Clin Pract. 2007;13:581–598. [DOI] [PubMed] [Google Scholar]
- 35. Boissel J-P, Amsallem E, Cucherat M, et al. Bridging the gap between therapeutic research results and physician prescribing decisions: knowledge transfer, a prerequisite to knowledge translation. Eur J Clin Pharmacol. 2004;60:609–616. [DOI] [PubMed] [Google Scholar]
- 36. Giguere A, Légaré F, Grad R, et al. Decision boxes for clinicians to support evidence-based practice and shared decision making: the user experience. Implement Sci. 2012;7:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Salbach NM, Jaglal SB, Korner-Bitensky N, et al. Practitioner and organizational barriers to evidence-based practice of physical therapists for people with stroke. Phys Ther. 2007;87:1284–1303. [DOI] [PubMed] [Google Scholar]
- 38. Marchionni C, Ritchie J. Organizational factors that support the implementation of a nursing Best Practice Guideline. J Nurs Manag. 2008;16:266–274. [DOI] [PubMed] [Google Scholar]
- 39. Stirman SW, Kimberly J, Cook N, et al. The sustainability of new programs and innovations: a review of the empirical literature and recommendations for future research. Implement Sci. 2012;7:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Tricco AC, Cogo E, Ashoor H, et al. Sustainability of knowledge translation interventions in healthcare decision-making: protocol for a scoping review. BMJ Open. 2013;3:pii: e002970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Brachaniec M, DePaul V, Elliott M, et al. Partnership in action: an innovative knowledge translation approach to improve outcomes for persons with fibromyalgia. Physiother Can. 2009;61:123–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Zwarenstein M, Reeves S. Knowledge translation and interprofessional collaboration: where the rubber of evidence-based care hits the road of teamwork. J Contin Educ Health Prof. 2006;26:46–54. [DOI] [PubMed] [Google Scholar]
- 43. Palinkas LA, Aarons GA, Chorpita BF, et al. Cultural Exchange and the implementation of evidence-based practices: two case studies. Res Soc Work Pract. 2009;19:602–612. [Google Scholar]
- 44. Scott SD, Albrecht L, O'Leary K, et al. Systematic review of knowledge translation strategies in the allied health professions. Implement Sci. 2012;7:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Moher D, Jones A, Lepage L; CONSORT Group (Consolidated Standards for Reporting of Trials). Use of the CONSORT statement and quality of reports of randomized trials: a comparative before-and-after evaluation. JAMA. 2001;285:1992–1995. [DOI] [PubMed] [Google Scholar]
- 46. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357. [DOI] [PubMed] [Google Scholar]
- 47. Grol RP, Bosch MC, Hulscher ME, et al. Planning and studying improvement in patient care: the use of theoretical perspectives. Milbank Q. 2007;85:93–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Sales A, Smith J, Curran G, Kochevar L. Models, strategies, and tools: theory in implementing evidence-based findings into health care practice. J Gen Intern Med. 2006;21(suppl 2):S43–S49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Bhattacharyya O, Reeves S, Garfinkel S, Zwarenstein M. Designing theoretically-informed implementation interventions: fine in theory, but evidence of effectiveness in practice is needed. Implement Sci. 2006;1:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. LaRocca R, Yost J, Dobbins M, et al. The effectiveness of knowledge translation strategies used in public health: a systematic review. BMC Public Health. 2012;12:751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Mendel P, Meredith LS, Schoenbaum M, et al. Interventions in organizational and community context: a framework for building evidence on dissemination and implementation in health services research. Admin Policy Mental Health. 2008;35:21–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Oxman AD, Fretheim A, Flottorp S. The OFF theory of research utilization. J Clin Epidemiol. 2005;58:113–116. [DOI] [PubMed] [Google Scholar]
- 53. Wilson PM, Petticrew M, Calnan MW, Nazareth I. Disseminating research findings: what should researchers do? A systematic scoping review of conceptual frameworks. Implement Sci. 2010;5:91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Estabrooks CA, Thompson DS, Lovely JJ, Hofmeyer A. A guide to knowledge translation theory. J Contin Educ Health Prof. 2006;26:25–36. [DOI] [PubMed] [Google Scholar]
- 55. French SD, Green SE, O'Connor DA, et al. Developing theory-informed behaviour change interventions to implement evidence into practice: a systematic approach using the Theoretical Domains Framework. Implement Sci. 2012;7:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Jacobson N, Butterill D, Goering P. Development of a framework for knowledge translation: understanding user context. J Health Serv Res Policy. 2003;8:94–99. [DOI] [PubMed] [Google Scholar]
- 57. Hogan DL, Logan J. The Ottawa model of research use: a guide to clinical innovation in the NICU. Clin Nurse Spec. 2004;18:255–261. [DOI] [PubMed] [Google Scholar]
- 58. Logan J, Graham ID. Toward a comprehensive interdisciplinary model of health care research use. Sci Commun. 1998;20:227–246. [Google Scholar]
- 59. Kitson A, Harvey G, McCormack B. Enabling the implementation of evidence-based practice: a conceptual framework. Qual Health Care. 1998;7:149–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Rycroft-Malone J, Kitson A, Harvey G, et al. Ingredients for change: revisiting a conceptual framework. Qual Safety Health Care. 2002;11:174–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Lomas J. Retailing research: increasing the role of evidence in clinical services for childbirth. Milbank Q. 1992;71:439–475. [PubMed] [Google Scholar]
- 62. Hudon A, Laliberté M, Hunt M, et al. What place for ethics? An overview of ethics teaching in occupational therapy and physiotherapy programs in Canada. Disabil Rehabil. 2014;36:775–780. [DOI] [PubMed] [Google Scholar]
- 63. Graham ID, Logan J. Innovations in knowledge transfer and continuity of care. Can J Nurs Res. 2004;36:89. [PubMed] [Google Scholar]
- 64. Wagner C. Wiki: A technology for conversational knowledge management and group collaboration. Communications of the Association for Information Systems. 2004;13:265–289. [Google Scholar]
- 65. Oborn E. Facilitating implementation of the translational research pipeline in neurological rehabilitation. Curr Opin Neurol. 2012;25:676–681. [DOI] [PubMed] [Google Scholar]
- 66. Jette DU, Bacon K, Batty C, et al. Evidence-based practice: beliefs, attitudes, knowledge, and behaviors of physical therapists. Phys Ther. 2003;83:786–805. [PubMed] [Google Scholar]
- 67. Jones ML, Cifu DX, Backus D, Sisto SA. Instilling a research culture in an applied clinical setting. Arch Phys Med Rehabil. 2013;94(1 suppl):S49–S54. [DOI] [PubMed] [Google Scholar]
- 68. Grimmer-Somers K, Lekkas P, Nyland L, et al. Perspectives on research evidence and clinical practice: a survey of Australian physiotherapists. Physiother Res Int. 2007;12:147–161. [DOI] [PubMed] [Google Scholar]
- 69. Bayley MT, Hurdowar A, Richards CL, et al. Barriers to implementation of stroke rehabilitation evidence: findings from a multi-site pilot project. Disabil Rehabil. 2012;34:1633–1638. [DOI] [PubMed] [Google Scholar]
- 70. Bridges PH, Bierema LL, Valentine T. The propensity to adopt evidence-based practice among physical therapists. BMC Health Serv Res. 2007;7:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Corcoran M. Dissemination or knowledge translation? Am J Occup Ther. 2006;60:487–488. [Google Scholar]
- 72. Lloyd C, King R, Bassett H. Occupational therapy and clinical research in mental health rehabilitation. Br J Occup Ther. 2005;68:172–176. [Google Scholar]
- 73. Pollock AS, Legg L, Langhorne P, Sellars C. Barriers to achieving evidence-based stroke rehabilitation. Clin Rehabil. 2000;14:611–617. [DOI] [PubMed] [Google Scholar]


