Abstract
Background
The aim of this study was to investigate the molecular epidemiological characteristics of metallo-β-lactamase (MBL)-producing Pseudomonas aeruginosa clinical isolates in Korea.
Materials and Methods
Three hundred and twenty nine P. aeruginosa clinical isolates were collected from 23 general hospitals in Korea from March to June 2014. Species were identified by matrix-assited laser desorption/ionization-time of flight and 16S rRNA sequencing. Antimicrobial susceptibility was determined by disk diffusion methods. Further, minimum inhibitory concentrations of carbapenems were determined by Etest. Polymerase chain reaction and sequencing were performed to identify genes encoding MBLs. Multi-locus sequence typing and pulsed-field gel electrophoresis were performed to determine epidemiological characteristics of MBL-producing P. aeruginosa isolates.
Results
Of the 329 isolates, 229 (69.6%) were susceptible to the carbapenems tested, including imipenem and meropenem; while 100 (30.4%) were non-susceptible to more than one of the carbapenems. Genes encoding imipenemase-6 (IMP-6) and Verona imipenemase-2 (VIM-2) MBLs were identified in 21 (6.4%) isolates (n = 17 and 4, respectively). All MBL-producing isolates showed multi-drug resistant phenotype, and a majority (n = 19) of the isolates were identified as sequence type 235 (ST235). The remaining isolates (n = 2) were identified as ST309 and ST463.
Conclusion
P. aeruginosa ST235 might play an important role in dissemination of MBL genes in Korea.
Keywords: Pseudomonas aeruginosa, metallo-β-lactamase, VIM-2 metallo-β-lactamase, International clone, Multi-locus sequence typing
Introduction
Carbapenems have widely been used as the mainstay for the treatment of severe infections caused by Pseudomonas aeruginosa. This is because they can easily permeate through the porins on the outer membrane of these microorganisms. Moreover, they have a high affinity for penicillin-binding proteins and a structure resistant to hydrolytic activities of most β-lactamases [1]. Unfortunately, a carbapenem-resistant P. aeruginosa (CRPA) has now emerged and is disseminating worldwide. According to a survey conducted in Korea in 2011, imipenem (a carbapenem) resistance rate of P. aeruginosa was 22% among 15,032 clinical isolates [2]. In fact, CRPA is considered a significant clinical threat because CRPA clinical isolates usually exhibit co-resistance to other classes of antimicrobial agents. Thus, there remain only a few alternatives for the treatment of systemic infections caused by carbapenem-resistant microorganisms [3].
Production of carbapenemase is the most important mechanism in P. aeruginosa for acquiring carbapenem resistance. Diverse kinds of carbapenemases have been identified in P. aeruginosa, including KPC and GES variants of class A; IMP-, VIM-, SPM-, and NDM-type metallo-β-lactamases (MBLs) of class B; OXA-40 and OXA-198 enzymes of class D [4, 5, 6, 7, 8, 9, 10, 11, 12]. MBL-producing P. aeruginosa (MPPA) has repeatedly been identified in Korea, since the first report for VIM-2 MPPA clinical isolates in 2002 [6]. A study in 2009 reported that IMP-6 was the dominant MBL (7.8%, 30/386) in P. aeruginosa clinical isolates collected in Korea followed by VIM-2 (0.3%, 1/386) [13].
multi-locus sequence typing (MLST) scheme for P. aeruginosa proposed by Curran et al. [14] has facilitated comparisons of epidemiological characteristics of strains from different hospitals or countries. Earlier studies reported that two international P. aeruginosa clonal complexes (CCs), CC111 and CC235, played a major role in dissemination of MBL genes worldwide [15, 16]. However, only a few studies have performed MLST experiments on MPPA in Asian countries. P. aeruginosa sequence type 235 (ST235) and ST357 producing IMP-1 MBL were identified in Japan [17]. P. aeruginosa ST235 producing IMP-6 or VIM-2 were also identified in Korea [13]. Furthermore, a recent study identified MPPA isolates of ST235 from Malaysia, Thailand, Sri Lanka, and Korea; ST773 from India, and ST298 from Taiwan [18].
The present study was conducted to investigate the molecular epidemiological characteristics of MPPA clinical isolates in Korea.
Materials and Methods
1. Bacterial strains and susceptibility testing
Non-duplicate P. aeruginosa clinical isolates (n = 329) were collected from 23 hospitals across 15 cities in Korea (Fig. 1) from March to June, 2014. The isolates were recovered from respiratory specimens (n = 120), urine (n = 96), pus (n = 78), blood (n = 24), and others (n = 11) (Table 1). Species identification was performed using the Bruker MALDI Biotyper (Bruker, Billerica, MA, USA) and 16S rRNA gene sequencing.
Figure 1. Map showing the locations of the participating hospitals in this study.
MBL, metallo-β-lactamase; IMP, imipenemase; VIM, Verona imipenemase.
Table 1. Antimicrobial susceptibilities of Pseudomonas aeruginosa clinical isolates by specimen.
| No. of isolates (%) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Respiratory (n = 120) | Blood (n = 24) | Urine (n = 96) | Pus (n = 78) | Other (n = 11) | Total (n = 329) | |||||||
| S | R | S | R | S | R | S | R | S | R | S | R | |
| AMC | 0 (0) | 120 (100) | 0 (0) | 24 (100) | 0 (0) | 96 (100) | 0 (0) | 78 (100) | 0 (0) | 11 (100) | 0 (0) | 329 (100) |
| TZP | 101 (84.2) | 19 (15.8) | 20 (83.3) | 4 (16.7) | 72 (75.0) | 22 (22.9) | 64 (82.1) | 14 (17.9) | 9 (81.8) | 2 (18.2) | 266 (80.9) | 61 (18.5) |
| TIM | 98 (81.7) | 22 (18.3) | 21 (87.5) | 3 (12.5) | 66 (68.7) | 30 (31.3) | 60 (76.9) | 18 (23.1) | 8 (72.7) | 3 (27.3) | 253 (76.9) | 76 (23.1) |
| ATM | 75 (62.5) | 29 (24.2) | 12 (50.0) | 8 (33.3) | 54 (56.2) | 26 (27.1) | 48 (61.5) | 19 (24.4) | 8 (72.7) | 3 (27.3) | 197 (59.9) | 85 (25.8) |
| CAZ | 87 (72.5) | 21 (17.5) | 18 (75.0) | 4 (16.7) | 62 (64.6) | 28 (29.2) | 56 (71.8) | 16 (20.5) | 7 (63.6) | 4 (36.4) | 230 (69.9) | 73 (22.2) |
| FEP | 87 (72.5) | 15 (12.5) | 16 (66.7) | 3 (12.5) | 56 (58.3) | 30 (31.3) | 60 (77.0) | 9 (11.5) | 7 (63.6) | 3 (27.3) | 226 (68.7) | 60 (18.2) |
| IPM | 81 (67.5) | 38 (31.7) | 18 (75.0) | 5 (20.8) | 63 (65.6) | 31 (32.3) | 62 (79.5) | 16 (20.5) | 6 (54.5) | 4 (36.4) | 230 (69.9) | 94 (28.6) |
| MEM | 84 (70.0) | 27 (22.5) | 20 (83.3) | 3 (12.5) | 64 (66.6) | 30 (31.3) | 62 (79.5) | 13 (16.7) | 6 (54.5) | 3 (27.3) | 236 (71.7) | 76 (23.1) |
| AMK | 111 (92.5) | 8 (6.7) | 23 (95.8) | 1 (4.2) | 69 (71.9) | 27 (28.1) | 72 (92.3) | 5 (6.4) | 10 (90.9) | 1 (9.1) | 285 (86.6) | 42 (12.8) |
| GEN | 103 (85.9) | 13 (10.8) | 21 (87.5) | 3 (12.5) | 65 (67.7) | 28 (29.2) | 67 (85.9) | 11 (14.1) | 10 (90.9) | 1 (9.1) | 266 (80.9) | 56 (17.0) |
| TOB | 104 (86.6) | 14 (11.7) | 20 (83.3) | 3 (12.5) | 68 (70.8) | 28 (29.2) | 65 (83.3) | 12 (15.4) | 9 (81.8) | 2 (18.2) | 266 (80.9) | 59 (17.9) |
| TMP/SMT | 0 (0) | 120 (100) | 0 (0) | 24 (100) | 0 (0) | 96 (100) | 0 (0) | 78 (100) | 0 (0) | 11 (100) | 0 (0) | 329 (100) |
| CIP | 78 (65.0) | 38 (31.7) | 15 (62.5) | 8 (33.3) | 53 (55.2) | 41 (42.7) | 51 (65.4) | 24 (30.8) | 9 (81.8) | 2 (18.2) | 206 (62.6) | 113 (34.3) |
| TET | 2 (1.7) | 116 (96.6) | 0 (0) | 24 (100) | 1 (1.0) | 95 (99.0) | 0 (0) | 78 (100) | 0 (0) | 11 (100) | 3 (0.9) | 324 (98.5) |
| CST | 120 (100) | 0 (0) | 24 (100) | 0 (0) | 96 (100) | 0 (0) | 78 (100) | 0 (0) | 11 (100) | 0 (0) | 329 (100) | 0 (0) |
S, susceptible; R, resistant; AMC, amoxicillin-clavulanic acid; TZP, piperacillin-tazobactam; TIM, ticarcillin-clavulanic acid; ATM, aztreonam; CAZ, ceftazidime; FEP, cefepime; IPM, imipenem; MEM, meropenem; AMK, amikacin; GEN, gentamicin; TOB, tobramycin; TMP/SMT, trimethoprim-sulfamethoxazole; CIP, ciprofloxacin; TET, tetracycline; CST, colistin.
Antimicrobial susceptibilities were tested by disk diffusion method following the Clinical and Laboratory Standards Institute (CLSI) guidelines [19]. Antimicrobial agents tested were amoxicillin-clavulanate, piperacillin-tazobactam, ticarcillin-clavulanate, aztreonam, ceftazidime, cefepime, imipenem, meropenem, amikacin, gentamicin, tobramycin, trimethoprim-sulfamethoxazole, ciprofloxacin, tetracycline, and colistin. Minimum inhibitory concentrations (MICs) of imipenem and meropenem were determined by Etest on Mueller-Hinton agar (Becton, Dickinson and Company, Sparks, MD, USA) according to manufacturer's instruction.
2. Characterization of carbapenemase genes
Carbapenemase genes were detected by PCR using primers as previously described (for genes encoding KPC, VIM-2-, and OXA-48-type carbapenemases) [20, 21] and those designed in this study (for genes encoding GES-, IMP-1-, and NDM-type carbapenemases) (Table 2). Templates for PCR amplification from clinical isolates were whole cell lysates, and amplified products were subjected to direct sequencing. Both strands of the PCR product were sequenced twice with an automatic sequencer (model 3730xl; Applied Biosystems, Weiterstadt, Germany). Experimentally determined nucleotide sequences were compared to sequence databases using BLAST (http://blast.ncbi.nlm.nih.gov/).
Table 2. Nucleotide sequences of primers used in this study.
| Primer name | Target gene | Nucleotide sequence (5' to 3') | Product size (bp) | Reference |
|---|---|---|---|---|
| KPC-F | KPC-type | GTCACTGTATCGCCGTCTAGTTC | 909 | This study |
| KPC-R | TGGTGGGCCAATAGATGATT | |||
| GES-F | GES-type | CGCTTCATTCACGCACTATT | 855 | 20 |
| GES-R | GTCCGTGCTCAGGATGAGTT | |||
| IMP-1F | IMP-1-type | AAGGCGTTTATGTTCATACTTCG | 605 | This study |
| IMP-1R | TTTAACCGCCTGCTCTAATGTAA | |||
| VIM-2F | VIM-2-type | ATCATGGCTATTGCGAGTCC | 749 | 21 |
| VIM-2R | ACGACTGAGCGATTTGTGTG | |||
| NDM-F | NDM-type | GCCCAATATTATGCACCCGG | 738 | This study |
| NDM-R | CTCATCACGATCATGCTGGC | |||
| OXA-48F | OXA-48-type | GATTATCGGAATGCCTGCGG | 845 | 20 |
| OXA-48R | CTACAAGCGCATCGAGCATCA |
KPC, klebsiella pneumoniae carbapenemase; F, forward; R, reverse; GES, greece extended-spectrum β-lactamase; IMP, imipenemase; VIM, Verona imipenemase; NDM, New Delhi metallo-β-lactamase; OXA, oxacillinase.
3. Multi-locus sequence typing (MLST)
PCR and sequencing for 7 housekeeping genes (acsA, aroE, guaA, mutL, nuoD, ppsA, and trpE) were performed as described previously [14]. Experimentally determined nucleotide sequences of both strands were compared to pre-existing sequences in the MLST database to assign allelic numbers and STs (http://pubmlst.org/paeruginosa).
4. Pulse-field gel electrophoresis (PFGE)
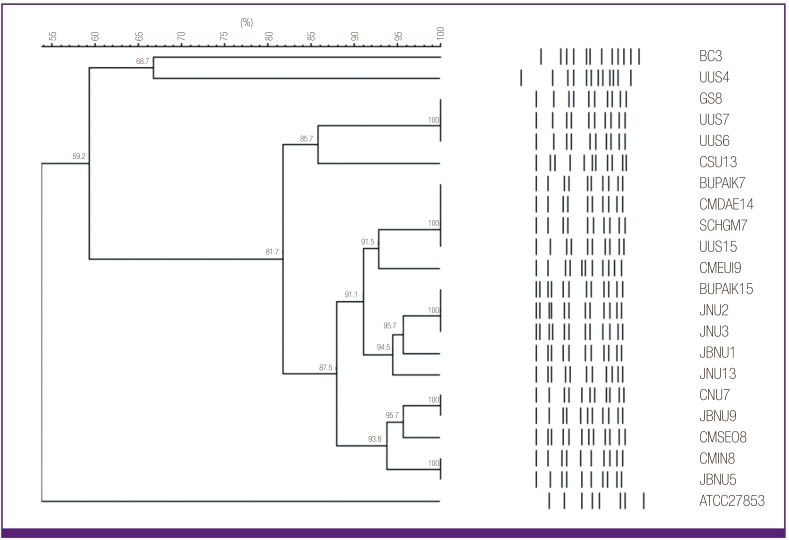
XbaI-digested genomic DNA was prepared and DNA fragments were separated for 20 h at 6 V/cm at 11℃ using the CHEF-DRII System (Bio-Rad, Hercules, CA, USA) with initial and final pulse times of 0.5 s and 30 s, respectively [13]. A lambda ladder (Bio-Rad) was used as DNA size marker. Band patterns were analyzed with UVIband/Map software (UVItech Ltd, Cambridge, UK) to generate a dendrogram based on the unweighted pair group method using arithmetic averages from the Dice coefficient.
Results
1. Antimicrobial susceptibilities of P. aeruginosa clinical isolates
Out of the 329 P. aeruginosa clinical isolates, 229 (69.6%) were found to be susceptible to the carbapenems tested, including imipenem and meropenem; while 100 (30.4%) were non-susceptible to more than one of the carbapenems (Table 3). Further, 92 of these 100 isolates exhibited non-susceptibility to both imipenem and meropenem. However, 7 imipenem-resistant isolates exhibited susceptibility to meropenem while only a single meropenem isolate was susceptible to imipenem. Compared with carbapenem-susceptible isolates, carbapenem-non-susceptible isolates exhibited higher resistance rates to ceftazidime (9.2% versus 52%), cefepime (3.9% versus 51%), amikacin (2.6% versus 36%), gentamicin (6.1% versus 42%), tobramycin (7% versus 43%), and ciprofloxacin (16.6% versus 75%). Additionally, the 329 isolates were susceptible to colistin. Antimicrobial susceptibility rates, by specimen, are described in Table 1.
Table 3. Antimicrobial susceptibilities of Pseudomonas aeruginosa clinical isolates.
| No. of isolates (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Carbapenem-susceptible (n = 229) | Carbapenem-non-susceptible (n = 100) | Total (n = 329) | |||||||
| Susceptible | Intermediate | Resistant | Susceptible | Intermediate | Resistant | Susceptible | Intermediate | Resistant | |
| Amoxicillin-clavulanate | 0 (0) | 0 (0) | 229 (100) | 0 (0) | 0 (0) | 100 (100) | 0 (0) | 0 (0) | 329 (100) |
| Piperacillin-tazobactam | 215 (93.9) | 0 (0) | 14 (6.1) | 51 (51) | 2 (2) | 47 (47) | 266 (80.9) | 2 (0.6) | 61 (18.5) |
| Ticarcillin-clavulanate | 208 (90.8) | 0 (0) | 21 (9.2) | 45 (45) | 0 (0) | 55 (55) | 253 (76.9) | 0 (0) | 76 (23.1) |
| Aztreonam | 174 (76.0) | 24 (10.5) | 31 (13.5) | 23 (23) | 23 (23) | 54 (54) | 197 (59.9) | 47 (14.3) | 85 (25.8) |
| Ceftazidime | 193 (84.3) | 15 (6.5) | 21 (9.2) | 37 (37) | 11 (11) | 52 (52) | 230 (69.9) | 26 (7.9) | 73 (22.2) |
| Cefepime | 194 (84.7) | 26 (11.4) | 9 (3.9) | 32 (32) | 17 (17) | 51 (51) | 226 (68.7) | 43 (13.1) | 60 (18.2) |
| Imipenem | 229 (100) | 0 (0) | 0 (0) | 1 (1) | 5 (5) | 94 (94) | 230 (69.9) | 5 (1.5) | 94 (28.6) |
| Meropenem | 229 (100) | 0 (0) | 0 (0) | 7 (7) | 17 (17) | 76 (76) | 236 (71.7) | 17 (5.2) | 76 (23.1) |
| Amikacin | 222 (97.0) | 1 (0.4) | 6 (2.6) | 63 (63) | 1 (1) | 36 (36) | 285 (86.6) | 2 (0.6) | 42 (12.8) |
| Gentamicin | 209 (91.2) | 6 (2.7) | 14 (6.1) | 57 (57) | 1 (1) | 42 (42) | 266 (80.9) | 7 (2.1) | 56 (17.0) |
| Tobramycin | 211 (92.1) | 2 (0.9) | 16 (7.0) | 55 (55) | 2 (2) | 43 (43) | 266 (80.9) | 4 (1.2) | 59 (17.9) |
| Trimethoprim-sulfamethoxazole | 0 (0) | 0 (0) | 229 (100) | 0 (0) | 0 (0) | 100 (100) | 0 (0) | 0 (0) | 329 (100) |
| Ciprofloxacin | 186 (81.2) | 5 (2.2) | 38 (16.6) | 20 (20) | 5 (5) | 75 (75) | 206 (62.6) | 10 (3.1) | 113 (34.3) |
| Tetracycline | 2 (0.9) | 0 (0) | 227 (99.1) | 1 (1) | 2 (2) | 97 (97) | 3 (0.9) | 2 (0.6) | 324 (98.5) |
| Colistin | 229 (100) | 0 (0) | 0 (0) | 100 (100) | 0 (0) | 0 (0) | 329 (100) | 0 (0) | 0 (0) |
2. Identification of MBL genes
PCR amplification and subsequent sequence analyses identified the blaIMP-6 and the blaVIM-2 in 5.2% (n = 17) and 1.2% (n = 4) carbapenem-non-susceptible isolates, respectively (Table 4). None of the isolates showed positive results when amplified for the detection of genes encoding KPC-, GES-, NDM, and OXA-48-type carbapenemases.
Table 4. Characteristics of Pseudomonas aeruginosa clinical isolates producing metallo-β-lactamase.
| Isolate | ST | MBL genotype | MIC (mg/L) | Co-resistant to: | |
|---|---|---|---|---|---|
| IPM | MEM | ||||
| GS8 | 235 | blaIMP-6 | >32 | >32 | AMK, AMC, ATM, FEP, CAZ, CIP, GEN, TET, TIM, TOB, TMP/SMT |
| CSU13 | 235 | blaIMP-6 | >32 | >32 | AMC, ATM, FEP, CAZ, CIP, TZP, TET, TIM, TMP/SMT |
| UUS6 | 235 | blaIMP-6 | >32 | >32 | AMK, AMC, ATM, FEP, CAZ, CIP, GEN, TZP, TET, TIM, TOB, TMP/SMT |
| UUS7 | 235 | blaIMP-6 | >32 | >32 | AMK, AMC, ATM, FEP, CAZ, CIP, GEN, TZP, TET, TIM, TOB, TMP/SMT |
| UUS15 | 235 | blaIMP-6 | >32 | >32 | AMK, AMC, ATM, FEP, CAZ, CIP, GEN, TZP, TET, TIM, TOB, TMP/SMT |
| CMSEO8 | 235 | blaIMP-6 | >32 | >32 | AMK, AMC, ATM, FEP, CAZ, CIP, GEN, TET, TIM, TOB, TMP/SMT |
| CNU7 | 235 | blaIMP-6 | >32 | >32 | AMK, AMC, ATM, FEP, CAZ, CIP, GEN, TET, TIM, TOB, TMP/SMT |
| SCHGM7 | 235 | blaIMP-6 | >32 | >32 | AMK, AMC, ATM, FEP, CAZ, CIP, GEN, TZP, TET, TIM, TOB, TMP/SMT |
| CMEUI9 | 235 | blaIMP-6 | >32 | >32 | AMC, ATM, FEP, CIP, TET, TMP/SMT |
| CMDAE14 | 235 | blaIMP-6 | >32 | >32 | AMK, AMC, ATM, FEP, CAZ, CIP, GEN, TZP, TET, TIM, TOB, TMP/SMT |
| BUPAIK7 | 235 | blaIMP-6 | >32 | >32 | AMK, AMC, ATM, FEP, CAZ, CIP, GEN, TZP, TET, TIM, TOB, TMP/SMT |
| BUPAIK15 | 235 | blaIMP-6 | >32 | >32 | AMK, AMC, ATM, FEP, CAZ, CIP, GEN, TET, TIM, TOB, TMP/SMT |
| JNU2 | 235 | blaIMP-6 | >32 | >32 | AMK, AMC, FEP, CAZ, CIP, GEN, TZP, TET, TIM, TOB, TMP/SMT |
| JNU3 | 235 | blaIMP-6 | >32 | >32 | AMK, AMC, FEP, CAZ, CIP, GEN, TZP, TET, TIM, TOB, TMP/SMT |
| JNU13 | 235 | blaIMP-6 | >32 | >32 | AMK, AMC, FEP, CAZ, CIP, GEN, TET, TIM, TOB, TMP/SMT |
| JBNU1 | 235 | blaIMP-6 | >32 | >32 | AMK, AMC, ATM, FEP, CAZ, CIP, GEN, TZP, TET, TIM, TOB, TMP/SMT |
| BC3 | 463 | blaIMP-6 | >32 | >32 | AMK, AMC, ATM, FEP, CAZ, CIP, GEN, TET, TIM, TOB, TMP/SMT |
| JBNU5 | 235 | blaVIM-2 | >32 | >32 | AMK, AMC, CAZ, CIP, GEN, TZP, TET, TIM, TOB, TMP/SMT |
| JBNU9 | 235 | blaVIM-2 | >32 | >32 | AMK, AMC, ATM, FEP, CAZ, CIP, GEN, TZP, TET, TIM, TOB, TMP/SMT |
| CMIN8 | 235 | blaVIM-2 | >32 | >32 | AMC, FEP, CAZ, TET, TIM, TMP/SMT |
| UUS4 | 309 | blaVIM-2 | >32 | 2 | AMK, AMC, ATM, FEP, CAZ, CIP, GEN, TET, TIM, TOB, TMP/SMT |
ST, sequence type; MBL, metallo-β-lactamase; MIC, minimum inhibitory concentration; IPM, imipenem; MEM, meropenem; AMK, amikacin; AMC, amoxicillin-clavulanic acid; ATM, aztreonam; FEP, cefepime; CAZ, ceftazidime; CIP, ciprofloxacin; GEN, gentamicin; TET, tetracycline; TIM, ticarcillin-clavulanic acid; TOB, tobramycin; TMP/SMT, trimethoprim-sulfamethoxazole; TZP, piperacillin-tazobactam.
3. Characteristics of MPPA clinical isolates
All MPPA clinical isolates were identified as ST235 (38-11-3-13-1-2-4), except one isolate (BC3) of ST463 (6-5-5-3-1-6-3) producing IMP-6 and another (UUS4) of ST309 (13-8-9-3-1-17-15) producing VIM-2 (Table 4). Moreover, all MPPA ST235 isolates exhibited similar (>80% similarity) XbaI-macrorestriction banding patterns by PFGE, while MPPA of ST463 and ST309 isolates displayed different (<70% similarity) patterns (Fig. 2). Further, all MPPA clinical isolates presented multidrug resistant phenotype in addition to high MIC values (>32 mg/L) for both imipenem and meropenem. UUS4 was the only exception that showed a low MIC value (2 mg/L) for meropenem (Table 4).
Figure 2. XbaI-macrorestriction patterns of metallo-β-lactamase-producing Pseudomonas aeruginosa clinical isolates.
Discussion
A molecular epidemiological study in 2008, based on a survey of 205 non-duplicated P. aeruginosa clinical isolates, collected from 18 university hospitals across 8 provinces of Korea, identified them as 62 different STs. Of these, 47.8% isolates (n = 98) were identified as CC235. These, in turn, comprised of ST235 (n = 96) and two single-locus ST235 variants- ST1015 (n = 1) and ST1162 (n = 1). The remaining isolates (n = 107) were identified as 59 different STs, including ST111, ST170, ST244, ST591, ST641, ST708, ST773, ST829, ST983, ST1015, ST1154, ST1162, and ST1166, sharing alleles with ST235 at less than 5 out of the 7 loci [22].
We previously reported (based on a survey in 2009) that clonal dissemination of MPPA ST235 is the principal cause for the diffusion of IMP-6 and VIM-2 MBL genes in Korea [13]. Despite a 5-year interval, our present study shows results similar to the previous survey. Compared with the earlier report, prevalence of MPPA is slightly lower in this study- from 8.0% (31/386) to 6.4% (21/329). This is due to lower prevalence of IMP-6- from 7.8% (30/386) to 5.2% (17/329). Although the prevalence of VIM-2 increased marginally from 0.3% (1/386) to 1.2% (4/329), IMP-6 was still the dominant MBL type in P. aeruginosa in Korea. The antimicrobial susceptibility rates of P. aeruginosa clinical isolates, recovered from blood specimens, for imipenem (18/24, 75.0%) and meropenem (20/24, 83.3%) were higher compared to those recovered from specimens other than blood, including respiratory, urinary, and wound specimens, (212/305, 69.5%; and 216/305, 70.8%, respectively) (Table 1).
Interestingly, new MPPA clones emerged in our current study. In the previous survey, all the MPPA clinical isolates (n = 31) were identified as ST235. Although ST235 continues to be the dominant strain among MPPA clinical isolates in this study, we identified two isolates as different STs- ST309 and ST463. MPPA ST235 has been identified in many Asian countries, including Japan, Malaysia, Thailand, Sri Lanka, and Korea [17, 18]. However, there are other MPPA strains that have also been identified in Asian countries: ST357 in Japan, ST773 in India, and ST298 in Taiwan. Recently, dissemination of IMP-6 MPPA ST244 in China was reported [23]. There is no evidence though, whether MPPA ST309 and ST463 entered Korea from foreign countries, or the strains acquired the MBL gene by horizontal transfer in this country itself. Nevertheless, what is alarming is that diversification of MPPA strains in Korea might be a signal for further dissemination of MPPA in the country.
In conclusion, our study underscores the findings that IMP-6 MPPA ST235 has disseminated in Korea, and that new MPPA strains, ST309 and ST463, have surfaced in the country. Given the impending hazards of these phenomena, it is crucial to monitor changes in MBL types and MPPA strains through periodic surveys for MPPA.
Acknowledgement
This study was supported by a grant (2013-E4405-01) by the Korean Center for Disease Control and Prevention, Republic of Korea.
References
- 1.Diene SM, Rolain JM. Carbapenemase genes and genetic platforms in Gram-negative bacilli: Enterobacteriaceae, Pseudomonas and Acinetobacter species. Clin Microbiol Infect. 2014;20:831–838. doi: 10.1111/1469-0691.12655. [DOI] [PubMed] [Google Scholar]
- 2.Yong D, Shin HB, Kim YK, Cho J, Lee WG, Ha GY, Choi TY, Jeong SH, Lee K, Chong Y KONSAR group. Increase in the prevalence of carbapenem-resistant Acinetobacter isolates and ampicillin-resistant non-typhoidal Salmonella species in Korea: a KONSAR study conducted in 2011. Infect Chemother. 2014;46:84–93. doi: 10.3947/ic.2014.46.2.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jeong SJ, Yoon SS, Bae IK, Jeong SH, Kim JM, Lee K. Risk factors for mortality in patients with bloodstream infections caused by cabapenem-resistant Pseudomonas aeruginosa: clinical impact of bacterial virulence and strain on outcome. Diagn Microbiol Infect Dis. 2014;80:130–135. doi: 10.1016/j.diagmicrobio.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 4.Poirel L, Nordmann P, Lagrutta E, Cleary T, Munoz-Price LS. Emergence of KPC-producing Psedomonas aeruginosa in the United States. Antimicrob Agents Chemother. 2010;54:3072. doi: 10.1128/AAC.00513-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang C, Cai P, Chang D, Mi Z. A Pseudomonas aeruginosa isolate producing the GES-5 extended-spectrum beta-lactamase. J Antimicrob Chemother. 2006;57:1261–1262. doi: 10.1093/jac/dkl116. [DOI] [PubMed] [Google Scholar]
- 6.Lee K, Lim JB, Yum JH, Yong D, Chong Y, Kim JM, Livermore DM. blaVIM-2 cassette-containing novel intergrons in metallo-β-lactamase-producing Pseudomonas aeruginosa and Pseudomonas putida isolates disseminated in a Korean hospital. Antimicrob Agents Chemother. 2002;46:1053–1058. doi: 10.1128/AAC.46.4.1053-1058.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jovcic B, Lepsanovic Z, Suljagic V, Rackov G, Begovic J, Topisirovic L, Kojic M. Emergence of NDM-1 metallo-β-lactamase in Pseudomonas aeruginosa clinical isolates from Serbia. Antimicrob Agents Chemother. 2011;55:3923–3931. doi: 10.1128/AAC.00226-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Potron A, Poirel L, Nordmann P. Plasmid-mediated transfer of the blaNDM-1 gene in Gram-negative rods. FEMS Microbiol Lett. 2011;324:111–116. doi: 10.1111/j.1574-6968.2011.02392.x. [DOI] [PubMed] [Google Scholar]
- 9.Yezil S, Shibl AM, Memish ZA. The molecular basis of β-lactamase production in Gram-negative bacteria from Saudi Arabia. J Med Microbiol. 2015;64:127–136. doi: 10.1099/jmm.0.077834-0. [DOI] [PubMed] [Google Scholar]
- 10.Martins AF, Zavascki AP, Gaspareto PB, Barth AL. Dissemination of Pseudomonas aeruginosa producing SPM-1-like and IMP-1-like metallo-β-lactamases in hospitals from Southern Brazil. Infection. 2007;35:457–460. doi: 10.1007/s15010-007-6289-3. [DOI] [PubMed] [Google Scholar]
- 11.Sevillano E, Gallego L, García-Lobo JM. First detection of the OXA-40 carbapenemase in P. aeruginosa isolates, located on a plasmid also found in A. baumannii. Pathol Biol (Paris) 2009;57:493–495. doi: 10.1016/j.patbio.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 12.El Garch F, Bogaerts P, Bebrone C, Galleni M, Glupczynski Y. OXA-198, an acquired carbapenem-hydrolyzing class D β-lactamase from Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2011;55:4828–4833. doi: 10.1128/AAC.00522-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seok Y, Bae IK, Jeong SH, Kim SH, Lee H, Lee K. Dissemination of IMP-6 metallo-β-lactamses-producing Pseudomonas aeruginosa sequence type 235 in Korea. J Antimicrob Chemother. 2011;66:2791–2796. doi: 10.1093/jac/dkr381. [DOI] [PubMed] [Google Scholar]
- 14.Curran B, Jonas D, Grudmann H, Pitt T, Dowson CG. Development of a multilocus sequence typing scheme for the opportunistic pathogen Pseudomonas aeruginosa. J Clin Microbiol. 2004;42:5644–5649. doi: 10.1128/JCM.42.12.5644-5649.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Samuelsen O, Toleman MA, Sundsfjord A, Rydberg J, Leegaard TM, Walder M, Lia A, Ranheim TE, Rajendra Y, Hermansen NO, Walsh TR, Giske CG. Molecular epidemiology of metallo-β-lactamase-producing Pseuomonas aeruginosa isolates from Norway and Sweden shows import of international clones and local clonal expansion. Antimicrob Agents Chemother. 2010;54:346–352. doi: 10.1128/AAC.00824-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Castanheira M, Deshpande LM, Costello A, Davies TA, Jones RN. Epidemiology and carbapenem resistance mechanisms of carbapenem-non-susceptible Pseuomonas aeruginosa collected during 2009-11 in 14 European and Mediterranean countries. J Antimicrob Chemother. 2014;69:1804–1814. doi: 10.1093/jac/dku048. [DOI] [PubMed] [Google Scholar]
- 17.Kitao T, Tada T, Tanaka M, Narahara K, Shimojima M, Shimada K, Miyoshi-Akiyama T, Kirikae T. Emergence of a novel multidrug-resistant Pseudomonas aeruginosa strain producing IMP-type metallo-β-lactamases and AAA(6')-lae in Japan. Int J Antimicrob Agents. 2012;39:518–521. doi: 10.1016/j.ijantimicag.2012.01.020. [DOI] [PubMed] [Google Scholar]
- 18.Kim MJ, Bae IK, Jeong SH, Kim SH, Song JH, Choi JY, Yoon SS, Thamlikitkul V, Hsueh PR, Yasin RM, Lalitha MK, Lee K. Dissemination of metallo-β-lactamse-producing Pseudomonas aeruginosa of sequence type 235 in Asian countries. J Antimicrob Chemother. 2013;68:2820–2824. doi: 10.1093/jac/dkt269. [DOI] [PubMed] [Google Scholar]
- 19.Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing: twenty- fourth informational supplement (M100-S24) Wayne, PA, USA: CLSI; 2014. [Google Scholar]
- 20.Bae IK, Jang SJ, Kim J, Jeong SH, Cho B, Lee K. Interspecies dissemination of the bla gene encoding PER-1 extended-spectrum β-lactamase. Antimicrob Agents Chemother. 2011;55:1305–1307. doi: 10.1128/AAC.00994-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tam VH, Chang KT, Abdelraouf K, Brioso CG, Ameka M, McCaskey LA, Weston JS, Caeiro JP, Garey KW. Prevalence, resistance mechanisms, and susceptibility of multidrug-resistant bloodstream isolates of Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2010;54:1160–1164. doi: 10.1128/AAC.01446-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bae IK, Suh B, Jeong SH, Wang KK, Kim YR, Yong D, Lee K. Molecular epidemiology of Pseudomonas aeruginosa clinical isolates from Korea producing β-lactamases with extended-spectrum activity. Diagn Microbiol Infect Dis. 2014;79:373–377. doi: 10.1016/j.diagmicrobio.2014.03.007. [DOI] [PubMed] [Google Scholar]
- 23.Chen Y, Sun M, Wang M, Lu Y, Yan Z. Dissemination of IMP-6 producing Pseudomonas aeruginosa ST244 in multiple cities in China. Eur J Clin Microbiol Infect Dis. 2014;33:1181–1187. doi: 10.1007/s10096-014-2063-5. [DOI] [PubMed] [Google Scholar]