Abstract
We report the first case of bacteremia by a novel Paenibacillus species, Paenibacillus pasadenensis, from a 55-year-old male patient with acute respiratory distress syndrome, following a microsurgical clipping procedure of a ruptured intracranial aneurysm. The bacterium was identified using 16S rRNA gene sequencing analysis, which was applied because current conventional methods employed in the clinical microbiology laboratory proved unsuccessful. Since this bacterium was first identified in 2006 and has never been reported elsewhere, we believe this report can provide practitioners with useful insight on the pathogenicity of this species.
Keywords: Paenibacillus pasadensis; Respiratory distress syndrome, Adult; RNA, Ribosomal; 16S
Introduction
The genus Paenibacillus was originally considered to be a part of the genus Bacillus but was later reclassified as a separate genus in 1993 [1]. These bacteria are recognized not only as pathogens capable of causing food poisoning and systemic infections, but also as a contaminant of blood cultures [2, 3, 4, 5, 6]. Paenibacillus pasadenensis is a spore-forming, Gram-positive, mesophilic, heterotrophic novel bacteria isolated from the Jet Propulsion Laboratory Spacecraft Assembly Facility (JPL-SAF) in 2006. Its pathogenicity has not hitherto been reported. Here, we report the first clinical isolation of P. pasadenensis in a 55-year-old male patient with acute respiratory distress syndrome (ARDS) following a microsurgical clipping procedure of a ruptured intracranial aneurysm.
Case Report
A 55-year-old male patient without a prior medical history was admitted to the emergency room of our university hospital for treatment of a severe headache and vomiting on May 12th, 2010. His vital signs included blood pressure of 180/100 mmHg, pulse rate of 88/min, respiratory rate of 24/min, and body temperature of 36.0℃. An initial head computed tomography (CT) scan revealed an acute extensive subarchnoid hemorrhage filling the basilar cisterns. Subsequent CT angiography showed an anterolaterally-directed ruptured aneurysm on the left mid-cranial artery bifurcation. As a result of these findings, microsurgical clipping was proposed. During the left pterional craniotomy and dural reflection, an intraoperative rupture was encountered and a rapid corticectomy with a retraction of the temporal lobe made the aneurysm clipping amenable.
Post-operatively, the patient was stuporous and responded only to basal stimuli. On post-operative day 2, a controlled mandatory ventilation mode mechanical ventilator was applied along with intravenous sedatives. The patient's neurologic status was stationary. Around post-operative day 5, the patient's body temporal temperature elevated to 38.1℃, and the arterial oxygen saturation levels dropped to 90%. Additional laboratory examinations revealed elevated C-reactive protein (27.0 mg/dL), leukocytosis (20,990/mm3) with a high neutrophil percentage (93%) and a left-shift. A chest CT discovered diffused bilateral lower lobe interstitial infiltrates with pleural effusion, consistent with a diagnosis of ARDS. Following this, the patient was placed on a regimen of IV teicoplanin (200 mg every 12 h), moxifloxacin (400 mg every 24 h) and meropenem (0.5 g every 12 h). On post-operative day 7, a culture of a sputum specimen was found to be positive for multi-drug-resistant Acinetobacter baumannii and methicillin-resistant Staphylococcus aureus, but they were not isolated later. Consequently, the administration of meropenem was changed to colistimethate sodium (160 mg every 12h). However, oxygenation deteriorated further (PaO2/FiO2 90-150 mmHg) and the patient became hemodynamically unstable despite the use of volume resuscitation and mechanical ventilation.
Despite the previous 10 days of regimented intravenous antibiotics and inotropics, the patient's condition worsened and progressed into severe sepsis. On May 27, lab results revealed a white blood cell count of 18,400/mm3, hemoglobin 8.8 g/dL, creatinine 2.8 mg/dL, blood urea nitrogen 111 mg/dL, alanine transaminase 116 IU/L, aspartate transaminase 88 IU/L, alkaline phosphatase 183 IU/L, sodium 155 mEq/L, potassium 4.7 mEq/L, and chloride 116 mEq/L. The erythrocyte sedimentation rate was 75 mm/hr and C-reactive protein was 23.5 mg/L. At this point, the patient's arterial oxygen saturation levels had dropped to 86%. In response, in addition to the existing assist-controlled mechanical ventilation, the patient was treated with 2 liters of IV normal saline, dopamine (3 µg/kg/min) and dobutamine (7 µg/kg/min). On post-operative day 17, gram-positive bacilli were detected in the patient's blood cultures. Blood was drawn from peripheral veins on both arms and feet, and six isolates could be obtained from six blood cultures. Of these, isolate 100604-2 was subjected to species identification, but it could not be identified using conventional methods in the clinical microbiology laboratory, including VITEK2 (bioMerieux, Hazelwood, MO, USA) and Microscan (Dade-Microscan, West Sacramento, CA, USA) analyses. On post-operative day 23, it was ascertained that there was little hope of recovery and his family requested the patient be transferred to a hospital located closer to their house. As a result the patient was discharged and transferred to the requested hospital. The patient died 3 days later.
The isolates including the isolate 100604-2 formed translucent, flat colonies of gram-positive bacilli, and showed no hemolysis on blood agar. To identify isolate 100604-2, 16S rRNA gene analysis was performed. A portion of the 16S rRNA gene was amplified and sequenced using the primer set fD1/rp2 [7]. Determined sequences (1,425 bp) were compared with the GenBank public database using the BLASTN program (http://blast.ncbi.nlm.nih.gov/Blast.cgi) and the EzTaxon public database (http://www.eztaxon.org/) [8]. Sequences showing high similarities were retrieved from the database and were aligned using the CLUSTALX program. A phylogenetic tree was also constructed by the neighbor-joining method and bootstrap values were evaluated from 1,000 replications.
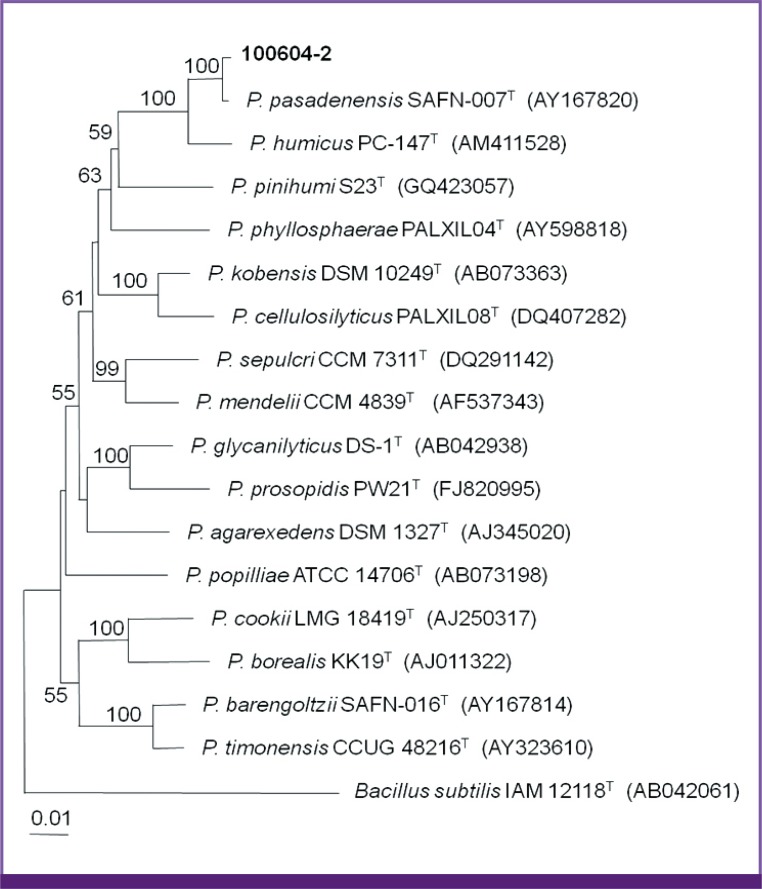
The 16S rRNA gene sequence (1,425 bp) of the isolate 100604-2 showed the highest similarity (99.6%) with a sequence of P. pasadenensis SAFN-007T (AY167820), followed by P. humicus PC-147T (AM411528) (98.0%), P. kobensis DSM 10249T (AB073363) (95.0%), and P. pinihumi S23T (GQ423057) (94.7%). Thus, the isolate 100604-2 was identified as P. pasadenensis. The constructed phylogenetic tree also indicated that isolate 100604-2 clustered with P. pasadenensis SAFN-007T (AY167820), which was supported strongly by bootstrap analysis (Fig. 1).
Figure 1. Phylogenetic relationships of the isolate 100604-2 and its closely related Paenibacillus species based on partial 16S rRNA gene sequences. This tree was constructed by method of neighbor-joining, which was rooted by Bacillus subtilis IAM 12118T (AB042061). Numbers at branching nodes are percentages of 1,000 bootstrap replications. Only values >50% are shown.
In vitro antimicrobial susceptibility testing was performed by the broth microdilution method according to the guidelines of the Clinical and Laboratory Standards Institute (CLSI) [9]. Isolate 100604-2 showed a low minimum inhibitory concentration for several antimicrobial agents that included ceftazidime (1 mg/L), imipenem (≤0.06 mg/L), penicillin (≤0.06 mg/L), polymyxin B (1 mg/L), vancomycin (0.12 mg/L), and trimethoprim/sulfamethoxazole (0.06/1.18 mg/L).
Discussion
As of February 2014, the genus Paenibacillus is comprised of 148 species (http://www.bacterio.cict.fr/p/paenibacillus.html.). These facultative anaerobic, spore-forming, rod-shaped, and low G+C Gram-positive bacteria have been found in a variety of heterogeneous environments, such as soil, rhizosphere, insect larvae, and clinical samples [2, 4, 10, 11].
Recently, several Paenibacillus species have been reported to cause bacteremic infections in humans, making blood the most common source for isolation. Among these are P. thiaminolyticus, P. konsidensis, P. alve, P. polymyxa, P. larvae, and P. sputa [4, 6, 11, 12, 13]. Cerebrospinal fluid was the second common source for isolation [11]. Some species have been isolated from various sites including pleural fluid, urine, brain abscess after penetrating periorbital injury, wound infection, and endophthalmitis [5, 14, 15]. A case of P. macerans pseudobacteremia has been reported [2].
As Paenibacillus species are mainly environmental in origin and are not detectable on human skin, it is speculated that Paenibacillus contamination of microsurgical clipping devices can be the source of bacteremia, both in the present case and involving P. thiaminolyticus [11]. In addition, there were two cases of bacteremia from identified medical devices as the source (i.e., a hip prosthesis and a heart valve) [13, 16]. Because these bacteria were recovered from all blood cultures and the patient showed clinical and laboratory signs of severe sepsis, pseudobacteremia could be excluded.
In this study, we report the finding of P. pasadensis found in the blood of a patient with ARDS, following a microsurgical clipping procedure of ruptured intracranial aneurysm. Also, based on our current knowledge, this is the first identification of P. pasadensis in a human. This finding additionally indicates that P. pasadensis can be a causal agent of human disease. Misinterpretation and/or the underestimation of blood culture findings can prove to be fatal and/or can result in unnecessary consequences. Empirical antimicrobial therapy should be started as soon as possible after the notification of a positive blood culture, especially in high-risk patients.
References
- 1.Ash C, Priest FG, Collins MD. Molecular identification of rRNA group 3 bacilli (Ash, Farrow, Wallbanks and Collins) using a PCR probe test. Proposal for the creation of a new genus Paenibacillus. Antonie Van Leeuwenhoek. 1993;64:253–260. doi: 10.1007/BF00873085. [DOI] [PubMed] [Google Scholar]
- 2.Noskin GA, Suriano T, Collins S, Sesler S, Peterson LR. Paenibacillus macerans pseudobacteremia resulting from contaminated blood culture bottles in a neonatal intensive care unit. Am J Infect Control. 2001;29:126–129. doi: 10.1067/mic.2001.111535. [DOI] [PubMed] [Google Scholar]
- 3.Teng JL, Woo PC, Leung KW, Lau SK, Wong MK, Yuen KY. Pseudobacteraemia in a patient with neutropenic fever caused by a novel paenibacillus species: Paenibacillus hongkongensis sp. nov. Mol Pathol. 2003;56:29–35. doi: 10.1136/mp.56.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ko KS, Kim YS, Lee MY, Shin SY, Jung DS, Peck KR, Song JH. Paenibacillus konsidensis sp. nov., isolated from a patient. Int J Syst Evol Microbiol. 2008;58:2164–2168. doi: 10.1099/ijs.0.65534-0. [DOI] [PubMed] [Google Scholar]
- 5.Roux V, Fenner L, Raoult D. Paenibacillus provencensis sp. nov., isolated from human cerebrospinal fluid, and Paenibacillus urinalis sp. nov., isolated from human urine. Int J Syst Evol Microbiol. 2008;58:682–687. doi: 10.1099/ijs.0.65228-0. [DOI] [PubMed] [Google Scholar]
- 6.Rieg S, Martin Bauer T, Peyerl-Hoffmann G, Held J, Ritter W, Wagner D, Kern WV, Serr A. Paenibacillus larvae Bacteremia in injection drug users. Emerg Infect Dis. 2010;16:487–489. doi: 10.3201/eid1603.091457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al Masalma M, Armougom F, Scheld WM, Dufour H, Roche PH, Drancourt M, Raoult D. The expansion of the microbiological spectrum of brain abscess with use of multiple 16S ribosomal DNA sequencing. Clin Infect Dis. 2009;48:1169–1178. doi: 10.1086/597578. [DOI] [PubMed] [Google Scholar]
- 8.Chun J, Lee JH, Jung Y, Kim M, Kim S, Kim BK, Lim YW. EzTaxon: a web-based tool for the identification of prokaryotes based on 16S ribosomal RNA gene sequences. Int J Syst Evol Microbiol. 2007;57:2259–2261. doi: 10.1099/ijs.0.64915-0. [DOI] [PubMed] [Google Scholar]
- 9.Clinical and Laboratory Standards Institute (CLSI) Performance standards for antimicrobial susceptibility testing; twenty-first informational supplement, M100-S21. Wayne, PA: CLSI; 2011. [Google Scholar]
- 10.McSpadden Gardener BB. Ecology of Bacillus and Paenibacillus spp. in Agricultural Systems. Phytopathology. 2004;94:1252–1258. doi: 10.1094/PHYTO.2004.94.11.1252. [DOI] [PubMed] [Google Scholar]
- 11.Ouyang J, Pei Z, Lutwick L, Dalal S, Yang L, Cassai N, Sandhu K, Hanna B, Wieczorek RL, Bluth M, Pincus MR. Case report: Paenibacillus thiaminolyticus: a new cause of human infection, inducing bacteremia in a patient on hemodialysis. Ann Clin Lab Sci. 2008;38:393–400. [PMC free article] [PubMed] [Google Scholar]
- 12.Kim KK, Lee KC, Yu H, Ryoo S, Park Y, Lee JS. Paenibacillus sputi sp. nov., isolated from the sputum of a patient with pulmonary disease. Int J Syst Evol Microbiol. 2010;60:2371–2376. doi: 10.1099/ijs.0.017137-0. [DOI] [PubMed] [Google Scholar]
- 13.Reboli AC, Bryan CS, Farrar WE. Bacteremia and infection of a hip prosthesis caused by Bacillus alvei. J Clin Microbiol. 1989;27:1395–1396. doi: 10.1128/jcm.27.6.1395-1396.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bosshard PP, Zbinden R, Altweqq M. Paenibacillus turicensis sp. nov., a novel bacterium harbouring heterogeneities between 16S rRNA genes. Int J Syst Evol Microbiol. 2002;52:2241–2249. doi: 10.1099/00207713-52-6-2241. [DOI] [PubMed] [Google Scholar]
- 15.Roux V, Raoult D. Paenibacillus massiliensis sp. nov., Paenibacillus sanguinis sp. nov. and Paenibacillus timonensis sp. nov., isolated from blood cultures. Int J Syst Evol Microbiol. 2004;54:1049–1054. doi: 10.1099/ijs.0.02954-0. [DOI] [PubMed] [Google Scholar]
- 16.Wu YJ, Hong TC, Hou CJ, Chou YS, Tsai CH, Yang DI. Bacillus popilliae endocarditis with prolonged complete heart block. Am J Med Sci. 1999;317:263–265. doi: 10.1097/00000441-199904000-00010. [DOI] [PubMed] [Google Scholar]