Abstract
Background
While electroconvulsive therapy (ECT) has been used for many years, there is insufficient research regarding the indications for continuation/maintenance (C/M)-ECT, its safety and efficacy, and the characteristics of patients with schizophrenia or schizoaffective disorder who receive multiple ECT sessions. The aims of this study were to characterize a series of patients who received 30 ECT sessions or more, to describe treatment regimens in actual practice, and to examine the results of C/M-ECT in terms of safety and efficacy, especially the effect on aggression and functioning.
Methods
We performed a retrospective chart review of 20 consecutive patients (mean age 64.6 years) with schizophrenia (n=16) or schizoaffective disorder (n=4) who received at least 30 ECT sessions at our ECT unit, and also interviewed the treating physician and filled out the Clinical Global Impression-Severity, Global Assessment of Functioning, and the Staff Observation Aggression Scale-Revised.
Results
Patients received a mean of 91.3 ECT sessions at a mean interval of 2.6 weeks. All had been hospitalized for most or all of the previous 3 years. There were no major adverse effects, and cognitive side effects were relatively minimal (cognitive deficit present for several hours after treatment). We found that ECT significantly reduced scores on the Staff Observation Aggression Scale-Revised subscales for verbal aggression and self-harm, and improved Global Assessment of Functioning scores. There were reductions in total aggression scores, subscale scores for harm to objects and to others, and Clinical Global Impression-Severity scores, these were not statistically significant.
Conclusion
C/M-ECT is safe and effective for chronically hospitalized patients. It improves general functioning and reduces verbal aggression and self-harm. More research using other aggression tools is needed to determine its effects and to reproduce our findings in prospective and controlled studies.
Keywords: electroconvulsive therapy, schizophrenia, maintenance, multiple sessions
Introduction
Electroconvulsive treatment (ECT) has been considered an acceptable practice in psychiatry for more than 75 years.1 After the introduction of effective psychotropic medications in the 1950s, there was a gradual decline in the use of ECT. However, over the years, there has been some disillusionment with regard to the limited success of pharmacological treatments in psychiatry. Even today, 30%–40% of patients who suffer from depression and 20%–40% of those with schizophrenia do not reach remission with pharmacological treatment.2,3 Accordingly, in the last 20 years, use of ECT has intensified in many parts of the world.4 ECT is considered acceptable today, especially in conditions of major depression, and its efficacy and safety are based on well established research.5,6 Although historically the first successful ECT treatments were used specifically for patients with schizophrenia, today they are less used and accepted in these patients, and this is despite the fact that the effectiveness of ECT in acute psychotic states (mainly catatonic conditions) is also well established.3,7
ECT proves beneficial not only for the affective condition of patients with schizophrenia, but also for positive symptoms8 and Brief Psychiatric Rating Scale indices of hostility, anxiety, and activation.9 Indeed, ECT has an effect of reducing agitation and aggression in general.10 However, within 6 months of achieving remission, over 50% of patients have a recurrence of symptoms on psychotropic medication alone.11 In view of the chronic characteristics of major mental illnesses, high recurrence rates, and high rates of resistance to drug therapy, some patients require multiple sessions of ECT. Besides using repetitive series of ECT for repeated acute states, there are clinicians who use ECT also when patients are clinically stable to prevent recurrences. These treatments include continuous (C)-ECT and maintenance (M)-ECT. C-ECT is provided immediately after achieving remission, with a gradual reduction of frequency and designed to reduce the possibility of rapid recurrence of symptoms. Evidence suggests that abrupt early cessation of ECT increases the chance of recurrence and that C-ECT reduces this risk.12 According to the American Psychiatric Association (APA), C-ECT is defined as a treatment lasting up to 6 months.13 M-ECT, however, has an unlimited duration and is intended to reduce the likelihood of new episodes (recurrences).14 In practice, the literature infrequently distinguishes between these two forms of ECT.15
Compared with the abundance of research on the effectiveness of ECT during the acute phase, there is limited research on C/M-ECT, and most of the existing research is anecdotal and methodologically problematic.15,16 Rabheru and Persad15 found that most existing information concerns C/M-ECT in the treatment of patients with affective disorders,15 and maintained that instead of the tendency to overuse C/M-ECT in patients with schizophrenia, that was prevalent in the distant past, today the trend is to underuse this effective method. However, these authors relied on individual case studies alone.15
As far back as 1943, the use of C/M-ECT was reported as a stabilizer for patients with schizophrenia who responded well to ECT in the acute phase.17 However, the quantity and quality of modern research on C/M-ECT with regard to patients with schizophrenia is low. In one study of 12 patients with resistant catatonic schizophrenia, 91% achieved remission following a series of ECT treatments, whereas 64% suffered a relapse within a year on medication alone.18 The recurrence of symptoms after an additional year of treatment, this time incorporating drug treatment and C-ECT (eleven ECT treatments in ascending intervals) for a duration of 24 weeks, was 57%, ie, a significantly lower rate than in the year they received medical treatment alone. Only one randomized controlled study has evaluated C-ECT (for up to 6 months) in patients with schizophrenia. In this important study, 45 patients were treated when they reached remission on ECT treatment and flupentixol for 6 months with flupentixol alone, C-ECT alone, or a combination of C-ECT and flupentixol. Recurrence rates were 93%, 93%, and 40%, respectively.19 Therefore, the combined treatment was considerably more effective than drug therapy or C-ECT administered separately. Hustig and Onilov found that some patients who were resistant to pharmacotherapy beforehand responded well after C-ECT,4 and assumed that ECT may have a rekindling effect on pharmacological treatment.
Information concerning use of M-ECT (over 6 months) in patients with schizophrenia is available. Most studies are retrospective reviews of medical files.11 Lévy-Rueff et al reviewed the clinical charts of a cohort of 19 patients with refractory and resistant schizophrenia or schizoaffective disorder who received on average 47 treatments of M-ECT at intervals of 1–8 weeks for a mean duration of 43 months, and showed a positive response to M-ECT with regard to mood symptoms, level of functioning, cooperation, and compliance with medication, along with a better ability of patients to take part in activities and to even return home or go back to work.20 The authors reported a decline in delusions and loss of appetite, suicidal ideation, and symptoms of anxiety. The cumulative duration of yearly hospitalizations was decreased by 80% and the mean duration of hospitalizations decreased by 40%. No improvement was observed for obsessive–compulsive symptoms, dissociation, or negative symptoms.20 In a prospective controlled study that included 21 patients with a diagnosis of major depression, bipolar disorder, or schizoaffective disorder, patients who agreed to M-ECT received an average of 19 treatments over a duration of 10 months, with a positive effect reflected by a longer time until rehospitalization, compared with patients who refused this treatment.21
An open study of 46 patients with schizophrenia found that combined treatment of medications and C/M-ECT after achieving remission was effective in safeguarding and improving symptoms, quality of life, and social functioning.22 There are no randomized controlled trials of M-ECT in patients with schizophrenia, and only one study available concerning patients with depression. Algorithms such as STABLE (for patients with depression receiving ECT) were not developed for the treatment of schizophrenia at all.22
According to the APA guidelines, patients who are suitable for C-ECT are those who have responded well to treatment with ECT previously, prefer C-ECT, are resistant to pharmacological therapy or have suffered drug side effects, and are able to give informed consent.14 As pointed out by Trevino et al this last requirement may be problematic due to the effect of the disorder on the patient’s ability to make informed decisions, and because of provisional cognitive impairment between one treatment of ECT and another.11 The APA prescribes specific guidelines relating to patients with schizophrenia, so C/M-ECT may be useful in combination with medication in patients who have responded well to ECT during the acute phase, if medication at the stable stage has not been effective, and in patients who cannot tolerate other treatments because of side effects or medical conditions.23 These guidelines stem in part from the fact that almost all studies of C/M-ECT have been done in patients who did not respond to pharmacological treatment or did not tolerate it.22 Based on the current medical literature, Zervas et al conclude that patients with schizophrenia who are particularly suitable for ECT are those with affective conditions or catatonia.3
Our study had the following objectives: to add to the existing knowledge about C/M-ECT by describing a series of patients with schizophrenia or schizoaffective disorder who received at least 30 ECT treatments; to examine the demographic characteristics, diagnoses, and main symptoms of patients who receive multiple ECT treatments; to describe the actual treatment regimen of patients who are exposed to multiple ECT treatments and how this is determined; to examine the results of treatment and especially the effect on dimensions of aggression and level of functioning; and to collect data on the complications and side effects of multiple ECT treatments.
Patients and methods
We performed a retrospective review of the medical records of 20 consecutive patients with schizophrenia or schizoaffective disorder who received 30 ECT treatments or more in the ECT unit at Be’er Ya’akov Mental Health Center. We collected data on the patients’ demographic characteristics, their hospitalization history, the legal status of their hospitalization, their psychiatric diagnoses and medical comorbidity, the reason for providing multiple ECT treatments, the treatment regimen, duration of ECT treatments, pharmacological treatment (prior, during, and after ECT) and the response to treatment, the response to ECT, and side effects (including cognitive impairment). These data were gathered from hospital and ECT unit files. Information was also gleaned from interviews with the treating doctors. Patients received a physical examination every 6 months, along with an electrocardiogram and a consultation with a specialist in internal medicine. In the year of the study (2013), we assessed each patient’s condition in a random month both before and after an ECT session.
The severity of each patient’s psychopathology before and after ECT was assessed using the Clinical Global Impression-Severity (CGI-S) questionnaire. Levels of aggression before and after treatment was measured using the Staff Observation Aggression Scale-Revised (SOAS-R)24 and level of functioning before and after treatment was evaluated using the Global Assessment of Functioning (GAF) questionnaire. These questionnaires were filled in by the treating doctors, who also reported the reasons for selection of multiple ECT treatments in these patients and their treatment regimen.
Approval for the collection and analysis of treatment data was received from the Helsinki Committee by our institutional review board. ECT itself was given as a standard treatment (with no institutional review board approval required). We deleted from the data any details that could personally identify the study patients. Differences in CGI-S, SOAS, and GAF scores were analyzed by repeated-measures t-test and variance was analyzed by the F-test.
Results
Sixteen patients with schizophrenia and four patients with schizoaffective disorder received bilateral C/M-ECT under general anesthesia between the years 2007 and 2013. The average age of the patients was 64.6±9.03 years. The average age at illness onset was 22.1±3.9 years. The mean number of diagnoses of physical disorders per patient was 2.25±1.48, while the most common diagnoses were hypertension (n=10), cataract (n=4), chronic obstructive pulmonary disease (n=3), and stroke (n=3). Patients received an average of 4.32±3.04 acute ECT treatments prior to C/M-ECT and between acute phase of the treatment and C/M-ECT. The mean number of treatments per patient was 91.3±56.32 (range 30–225).
The interval between treatments was flexible and was determined by the patient’s clinical condition, ranging from twice a week to once every 6 weeks (on average once every 2.6±1.47 weeks). Psychopharmacological treatment included various combinations of first-generation and second-generation antipsychotic drugs (including one patient who was treated with clozapine), anticholinergic drugs, benzodiazepines, antihistamines, and in one case carbamazepine. The most common symptoms were delusions (n=17), aggression (n=15), thought disturbances (n=14), and auditory hallucinations (n=12). Only five patients showed prominent affective symptoms (dysphoria or mood swings), and signs of catatonia were observed in one patient. Most of the patients had been hospitalized on and off consecutively for the previous 3 years. The clinical and demographic characteristics of the patients are shown in Table 1.
Table 1.
Clinical and demographic characteristics
| Age (onset) sex family status | ICD-10 diagnosis | Physical illnesses | Last hospital admission status | Series of acute ECT | Total number of treatments | Frequency (weeks) | Psychopharmacological treatment | Main symptoms | Duration hospitalization (in months) last 3 years | Duration hospitalization (in months) last year | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 73 | F20 | HTN | VH | 1 | 225 | 1 | SGA | AuH | 12 | 12 |
| (17) | Hernia | AC | AG | ||||||||
| Male | PD | ||||||||||
| Married | DTF | ||||||||||
| NS | |||||||||||
| 2 | 70 | F20 | Hepatitis B + C | CH | 3 | 66 | 1/2–1 | FGA | RPD | 12 | 12 |
| (21) | HTN | AC | SH | ||||||||
| Male | AG | ||||||||||
| Single | DTF | ||||||||||
| N | |||||||||||
| 3 | 75 | F25 | HTN | CH | 2 | 92 | 4–8 | SGA | DYS | 9 | 12 |
| (24) | Arrhythmia | FGA | Anx | ||||||||
| Female | Osteoporosis | AG | |||||||||
| Married | Cataract | RE | |||||||||
| Retinal degeneration | RPD | ||||||||||
| CD | |||||||||||
| 4 | 71 | F20 | HTN | CH | 10 | 107 | 3 | FGA | AG | 12 | 12 |
| (22) | AC | PSJ | |||||||||
| Female | DTF | ||||||||||
| Widow | RPD | ||||||||||
| N | |||||||||||
| 5 | 64 | F20 | Bronchiectasis | CH | 7 | 110 | 1–4 | FGA | LA | 12 | 12 |
| (19) | s/p ca of ovaries | BZD | Anx | ||||||||
| Female | AC | DTF | |||||||||
| Single | AuH | ||||||||||
| PD | |||||||||||
| AG | |||||||||||
| 6 | 64 | F20 | HTN | VH | 5 | 52 | 2 | SGA | AuH | 12 | 12 |
| (20) | LA | ||||||||||
| Female | CD | ||||||||||
| Married | PD | ||||||||||
| AG | |||||||||||
| S | |||||||||||
| 7 | 63 | F20 | COPD | VH | 2 | 31 | 2 | FGA | AuH | 12 | 12 |
| (25) | SLE | SGA | AG | ||||||||
| Female | Arrhythmia | DTF | |||||||||
| Divorced | CD | ||||||||||
| PD | |||||||||||
| 8 | 65 | F20 | Ischemic heart disease | VH | 2 | 30 | 2–3 | FGA | AuH | 9 | 12 |
| (23) | HTN | SGA | DTF | ||||||||
| Male | Cardiac insufficiency | RPD | |||||||||
| Single | CD | ||||||||||
| AG | |||||||||||
| 9 | 62 | F20 | s/p CVA | VH | 1 | 47 | 1–2 | CLZ | Anx | 12 | 12 |
| (34) | Diabetes | AH | CD | ||||||||
| Male | Cardiac insufficiency | DTF | |||||||||
| Divorced | Gastric-esophageal reflux | PD | |||||||||
| AuH | |||||||||||
| C | |||||||||||
| N | |||||||||||
| RE | |||||||||||
| DYS | |||||||||||
| 10 | 69 | F25 | HTN | VH | 9 | 203 | 1 | FGA | DTF | 12 | 12 |
| (17) | BZD | CD | |||||||||
| Female | AC | ||||||||||
| Single | |||||||||||
| 11 | 76 | F20 | Cataract | VH | 2 | 96 | 2 | FGA | N | 12 | 12 |
| (26) | COPD | SGA | RE | ||||||||
| Female | AG | ||||||||||
| Widow | |||||||||||
| 12 | 72 | F20 | Psoriasis | VH | 8 | 109 | 3–4 | SGA | AuH | 12 | 12 |
| (25) | Cataract | DTF | |||||||||
| Female | RPD | ||||||||||
| Married | CD | ||||||||||
| AG | |||||||||||
| 13 | 68 | F20 | Epilepsy | VH | 2 | 189 | 1 | FGA | DTF | 12 | 12 |
| (20) | Hypothyroidism | BZD | AuH | ||||||||
| Male | Anemia | AC | CD | ||||||||
| Single | s/p CVA SIADH | NS | |||||||||
| PD | |||||||||||
| AG | |||||||||||
| 14 | 79 | F25 | HTN | VH | 4 | 62 | 4 | SGA | DYS | 12 | 12 |
| 24 | Kidney failure s/p CVA | AH | NS | ||||||||
| Male | Parkinson | CD | |||||||||
| Married | S | ||||||||||
| 15 | 55 | F20 | Hepatitis C | VH | 4 | 35 | 1–4 | FGA | NS | 9 | 12 |
| (21) | PJ | ||||||||||
| Female | PD | ||||||||||
| Married | |||||||||||
| 16 | 43 | F20 | – | VH | 3 | 37 | 3–4 | FGA | AuH | 12 | 12 |
| (17) | SGA | AG | |||||||||
| Female | PD | ||||||||||
| Married | DTF | ||||||||||
| 17 | 49 | F25 | HTN | VH | 7 | 78 | 2 | FGA | DTF | 8 | 12 |
| (22) | Kidney failure | BZD | AuH | ||||||||
| Female | Hypothyroidism | AC | CD | ||||||||
| Married | PD | ||||||||||
| AG | |||||||||||
| 18 | 60 | F20 | HTN | CH | 9 | 90 | 2 | SGA | AuH | 12 | 12 |
| (21) | BZD | RPD | |||||||||
| Male | AG | ||||||||||
| Single | |||||||||||
| 19 | 63 | F20 | Cataract | VH | 2 | 66 | 4–8 | FGA | RPD | 12 | 12 |
| (23) | COPD | BZD | DTF | ||||||||
| Male | AG | ||||||||||
| Divorced | S | ||||||||||
| 20 | 58 | F20 | – | VH | 2 | 101 | 2–3 | SGA | Anx | 12 | 12 |
| (22) | CBZ | CD | |||||||||
| Female | DTF | ||||||||||
| Single | PD | ||||||||||
| AuH |
Abbreviations: ICD, International Classification of Diseases; ECT, electroconvulsive therapy; VH, voluntary hospitalization; CH, compulsory hospitalization; FGA, first-generation antipsychotic; SGA, second-generation antipsychotic; AC, anticholinergic; BZD, benzodiazepine; CLZ, clozapine; AH, antihistamine (promethazine); CBZ, carbamazepine; AuH, auditory hallucinations; AG, aggression; S, suicide; SH, self-harm; PD, paranoid delusions; RPD, reference and paranoid delusions; DTF, disturbance of thought form; NS, negative signs; N, negativism; DYS, dysphoria; RE, refusal to eat and drink; CD, concentration difficulty; PSJ, poor sexual judgment; PJ, poor judgment; LA, labile affect; C, catatonic; Anx, anxiety; HTN, hypertension; COPD, chronic obstructive pulmonary disease; SLE, systemic lupus erythematosus; RE, recurrent; s/p, state post; ca, cancer; CVA, cerebrovascular accident; SIADH, Syndrome of Inappropriate Antidiuretic Hormone Secretion.
The reasons for choosing C/M-ECT were lack of adequate response to medications, good response to ECT in the past, aggression, self-injury, refusal to eat and drink, physical problems limiting the ability to change the psychopharmacological regimen, and an attempt to prevent severe exacerbations that were evident from past history. The decision about the treatment regimen, ie, the interval between treatments, was determined for each individual case depending on the clinical condition of the patient, and not according to a uniform protocol.
Cognitive functions were not tested in a systematic way prior to or after treatment; however, confusion (n=3) and temporary memory problems (n=2) were documented in a minority of cases. These were obtained by subjective patient reporting and/or by staff observations. Other recorded side effects were rare, and included headaches (n=5), nausea (n=2), bradycardia (n=3), apnea (n=3), and a significant increase in blood pressure after treatment (n=4). No major complications were recorded.
Subscale scores for aggression towards objects and aggression towards others showed a significant reduction (52% and 59%, respectively, not statistically significant). Subscale scores for verbal aggression (shouting, cursing, threatening) and aggression towards self (eg, itching of the skin, self-hitting, hair pulling, head banging, dropping to the floor) decreased significantly (54% and 63%, respectively). The mean total Overt Aggression Scale (OAS) score fell by 55%, but this was not statistically significant. Mean CGI-S scores decreased following ECT treatment by 39% (not statistically significant). Level of functioning, as measured on the GAF scale, increased significantly by 17% (Table 2 and Figure 1).
Table 2.
CGI-S, OAS, and GAF scores before and after ECT
| Before ECT (mean ± SD) | After ECT (mean ± SD) | F | P-value | |
|---|---|---|---|---|
| Overall score OAS | 7.95±1.3 | 3.6±1.0 | 1.78 | NS |
| Verbal OAS | 2.6±1.1 | 1.4±0.8 | 1.73 | <0.001 |
| Objects OAS | 2.5±1.1 | 1.2±0.7 | 1.99 | NS |
| Self OAS | 1.2±1.0 | 0.45±0.6 | 2.47 | 0.005 |
| Others OAS | 1.7±0.7 | 0.7±0.7 | 1 | NS |
| CGI-S | 5.9±0.7 | 3.6±0.5 | 1.73 | NS |
| GAF | 23.0±4.9 | 26.9±6.9 | 5.73 | 0.032 |
Abbreviations: CGI-S, Clinical Global Impression-Severity; ECT, electroconvulsive therapy; GAF, Global Assessment of Functioning; NS, not statistically significant; SD, standard deviation; OAS, Over Aggression Scale.
Figure 1.
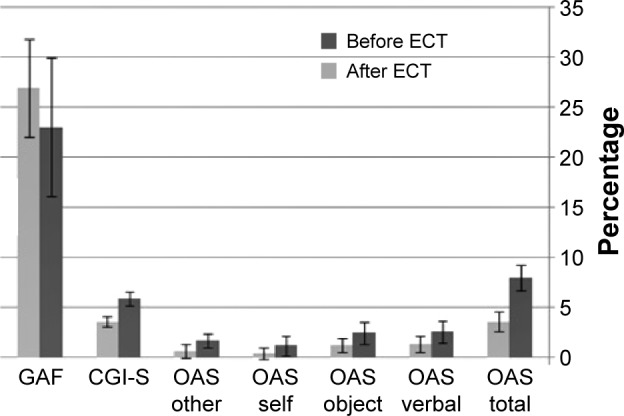
Changes in results in Global Assessment of Functioning, Clinical Global Impression-Severity, and OAS scores before and after ECT.
Note: Data are shown as the mean ± standard deviation.
Abbreviation: ECT, electroconvulsive therapy; OAS, Overt Aggression Scale; GAF, Global assessment of function; CGI-S, Clinical Global Impression-Severity.
All patients received treatment in the acute ward while on full hospitalization. They received between six and 12 treatments (first six treatments administered as twice week, and once a week or once every 10 days thereafter). All patients received at least 12 months of treatment with M-ECT. In Israel, due to rules and regulations, outpatient ECT procedure is performed like that: almost anyone comes from their houses so most of them are hospitalized in an acute ward in order to receive ECT treatment and after the ECT procedure discharged the next day. This is the reason why patients are evaluated in the acute ward when they are hospitalized for treatment. Moreover, from January 1, 2015 all patients can receive ECT without hospitalization due to reforms in the mental health field.
Discussion
While the use of ECT in the acute phase of major mental illnesses is well established and evidence-based, there is a lack of information on C/M-ECT. This retrospective study was designed to collect information on 20 patients with schizophrenia or schizoaffective disorder who received at least 30 ECT treatments at the Be’er Ya’akov Mental Health Center, in order to typify the patients who require prolonged ECT and to evaluate the results of these treatments, and especially their impact on the level of aggression and the level of functioning.
Our results demonstrate that all scale and subscale scores changed for the better (see Figure 1), although for some parameters, the sample did not have enough power to show statistical significance. This improvement was noted on a standard unchanged antipsychotic medication regimen (which was usually not effective), so we were able to neutralize the effect of ECT on our patients. Their general performance, as well as part of the results of the subscales for aggression (OAS) changed in a significant way. Our results are interesting in a further way, ie, while Zervas et al3 stated that schizophrenic patients who are particularly suitable for ECT are those with affective conditions or catatonia, in our study of C/M-ECT, only a quarter of the patients had schizoaffective disorder (n=4) or symptoms of catatonia (patient =1). Thus, if supported by additional research and studies in other countries, the indication for ECT in schizophrenia should perhaps be broadened.
In terms of the study population, there were some important sample characteristics. First, our sample included relatively elderly patients (mean age approximately 65 years). This is a typical finding, with most reports on C/M-ECT being in elderly patients.13,15,18 Although Lévy-Rueff et al20 reported on the use of M-ECT in patients with schizophrenia or schizo-affective disorder who had a mean age of 48±20 years, Suzuki et al18 reported on a series of patients with schizophrenia and a mean age of 61 years. Second, our sample included only patients with schizophrenia or schizoaffective disorder. With regards the last 20 patients who received multiple C/M-ECT in our institution, there were no patients with bipolar affective disorder. This is either because patients with affective disorder are not usually required to have numerous ECT treatments, because the doctors who treat them avoid giving multiple ECT treatments (bipolar affective disorder patients do not exhibit severe behavioral disorders that require “aggressive” treatment), or because of the technical and logistical complexity in providing multiple ECT treatments to outpatients who are not chronically hospitalized.
In this respect, the present study deals with a unique patient population, and there are few reports concerning such patients in the literature. Lévy-Rueff et al20 reported on a group of patients with schizophrenia or schizoaffective disorder who were hospitalized for on average 10 months during the year prior to M-ECT; however, after beginning treatment, they were hospitalized for an average of two months. Russell et al25 reported that their series of bipolar affective and schizoaffective patients were in the community for most of the year before starting C/M-ECT. Suzuki et al18 reported on C-ECT in patients with catatonic schizophrenia but did not provide data on hospitalization days at all. It seems that most of the reports regarding multiple ECT treatments available so far in the literature deal with affective patients with a disorder that is naturally less severe than in those discussed here or schizophrenia patients with a functional status and disease severity that enable them to live most of the time in the community.
The current study adds information regarding the benefit of C/M-ECT with regard to the most severe and chronic subgroup of adult patients with schizophrenia, who are hospitalized continuously for a long duration. Although the number of patients in our study is small and conclusions are hard to draw out of this sample, we found a benefit that has not previously been well documented in the literature. The study also adds necessary information on the impact of the ECT treatments not only on general clinical condition (as reflected by CGI-S scores), but also specifically on aggression and overall function. With regard to these three indices, the present study shows a clinically significant effect, even if for some of the variables the sample did not have sufficient statistical power. In terms of verbal aggression, self-injury, and overall level of functioning, the study showed significant benefits and statistical significance of C/M-ECT treatments for these patients. However, groups that used C/M-ECT in patients with schizophrenia and schizoaffective disorder did not specifically investigate aggression.3,18,20 Also, concerning general functioning on the GAF index, Suzuki et al18 did not find a statistically significant effect in patients with schizophrenia. Additionally, in contrast with the current study, Suzuki et al18 carried out their research using only seven patients.
As found in other studies,15,18,25 side effects and complications are not common, and minor if they do occur, even in elderly patients and in many cases patients who are physically ill. Minor side effects, such as headaches, nausea, and muscle pain, are no different from those reported following acute ECT treatments; they pass rapidly and are well tolerated. Major complications, including falls, prolonged apnea, cardiac dysrhythmias, and status epilepticus or delirium,10,11 are very rare. All the above require close monitoring by a skilled team during and after each ECT treatment.
The mortality rate with ECT nowadays is very low and estimated at 1:10,000.1 With regard to cognitive impairment, patients have reported that the most negative aspect of ECT is memory impairment.12 However, the available information indicates that, unlike acute ECT treatments, C/M-ECT does not cause objective cognitive impairment, probably because of the longer time interval between treatments. In fact, most studies that have examined ECT treatment indicators, such as the Mini-Mental State Examination, found a slight increase in cognitive function following long-term C/M-ECT.11,22,25
The present study shows that there is no single indication for C/M-ECT in our patients; however, C/M-ECT in this patient group is designed for treatment either at the start of a clinical exacerbation or to prevent a clinical exacerbation (psychotic symptoms or dangerous behaviors, such as aggression, suicide attempts, or refusal to eat and drink). Also, the treatment regimen is changeable and non-uniform, and is characterized by an individual approach, determined according to clinical judgment. Further studies will have to determine whether this approach is preferable to using algorithms such as STABLE. At present, this is also the most common approach11 and is the one recommended by the APA.14
Our study has several limitations. First, the sample size of the study was small. A second limitation is that this was a retrospective study, based on clinical impressions of the treating doctors who decided to administer ECT treatments to their patients. Therefore, their impression with regard to clinical improvement could be affected by their expectations of the impact of treatment, and thus could have biased their objectivity regarding evaluation. A third limitation is the lack of a control group, ie, a group of patients receiving placebo under general anesthesia, which is ethically problematic, or a group of patients with a similar clinical condition and who did not receive ECT. A fourth limitation is the lack of use of a standardized measure for examining cognitive impairment or improvement following treatment.
A recent retrospective study reviewed the records of 43 patients with schizophrenia who received and responded to an acute course of ECT.26 The relapse-free rate of all 43 patients at one year was 57.3%, and the median relapse-free period was 21.5 months. Multivariate analysis showed that the number of ECT sessions was associated with a significant increase in the risk of relapse. Patients who were treated with adjunctive mood stabilizers as maintenance pharmacotherapy after a response to the acute course of ECT were at a lower risk of relapse than those treated without mood stabilizers.26 Another therapeutic possibility, as supported by our results, could be administration of C/M-ECT in these patients.
Conclusion
The present study demonstrates the efficacy and safety of C/M-ECT in adult patients with chronic schizophrenia or schizoaffective disorder, with a significant positive effect seen for some indices of aggression and self-harm, as well as on the functioning of patients. Despite the limitations of the study, it is important research because information regarding C/M-ECT in patients with schizophrenia or schizoaffective disorder is limited, and information on the patient population similar to that examined in the present study, is limited. The present sample included many elderly patients, providing additional support for the efficacy and safety of C/M-ECT in elderly patients with schizophrenia.27 Larger studies are required to answer the questions that were beyond the scope of this study, ie, if a larger sample will show the effectiveness of C/M-ECT also on other subscales of aggression (aggression towards objects and toward others), and on CGI scores. Finally, if ethical considerations permit, it would be interesting to determine if these findings would also be seen in a controlled study. ECT, the most widely available non-pharmacological treatment for severe mental illness,27 still holds considerable promise for patients with schizophrenia.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Sadock BJ, Sadock VA, Ruiz P, editors. Kaplan & Sadock’s Comprehensive Textbook of Psychiatry. 9th ed. New York, NY, USA: Lippincott Williams & Wilkins; 2009. [Google Scholar]
- 2.Susan GK, Schneider RK. Clinical features of treatment-resistant depression. J Clin Psychiatry. 2001;62(Suppl 6):18–25. [PubMed] [Google Scholar]
- 3.Zervas IM, Theleritis C, Soldatos CR. Using ECT in schizophrenia: a review from a clinical perspective. World J Biol Psychiatry. 2012;13:96–105. doi: 10.3109/15622975.2011.564653. [DOI] [PubMed] [Google Scholar]
- 4.Hustig H, Onilov R. ECT rekindles pharmacological response in schizophrenia. Eur Psychiatry. 2009;24:521–525. doi: 10.1016/j.eurpsy.2009.04.005. [DOI] [PubMed] [Google Scholar]
- 5.Bailine S, Fink M, Knapp R, et al. Electroconvulsive therapy is equally effective in unipolar and bipolar depression. Acta Psychiatr Scand. 2010;121:431–436. doi: 10.1111/j.1600-0447.2009.01493.x. [DOI] [PubMed] [Google Scholar]
- 6.Kellner CH, Fink M, Knapp R, et al. Relief of expressed suicidal intent by ECT: a consortium for research in ECT study. Am J Psychiatry. 2005;162:977–982. doi: 10.1176/appi.ajp.162.5.977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tharyan P, Adams CE. Electroconvulsive therapy for schizophrenia. Cochrane Database Syst Rev. 2005;2:CD000076. doi: 10.1002/14651858.CD000076.pub2. [DOI] [PubMed] [Google Scholar]
- 8.Chanpattana W, Chakrabhand ML. Factors influencing treatment frequency of continuation ECT in schizophrenia. J ECT. 2001;17:190–194. doi: 10.1097/00124509-200109000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Chanpattana W, Chakrabhand ML. Combined ECT and neuroleptic therapy in treatment-refractory schizophrenia: prediction of outcome. Psychiatry Res. 2001;105:107–115. doi: 10.1016/s0165-1781(01)00321-3. [DOI] [PubMed] [Google Scholar]
- 10.Ujkaj M, Davidoff DA, Seiner SJ, Ellison JM, Harper DG, Forester BP. Safety and efficacy of electroconvulsive therapy for the treatment of agitation and aggression in patients with dementia. Am J Geriatr Psychiatry. 2012;20(1):61–72. doi: 10.1097/JGP.0b013e3182051bbc. [DOI] [PubMed] [Google Scholar]
- 11.Trevino K, McClintock SM, Husain MM. A review of continuation electroconvulsive therapy – application, safety, and efficacy. J ECT. 2010;26:186–195. doi: 10.1097/YCT.0b013e3181efa1b2. [DOI] [PubMed] [Google Scholar]
- 12.Odeberg H, Rodriguez-Silva B, Salander P, Mårtensson B. Individualized continuation electroconvulsive therapy and medication as a bridge to relapse prevention after an index course of electroconvulsive therapy in severe mood disorders: a naturalistic 3-year cohort study. J ECT. 2008;24:183–190. doi: 10.1097/YCT.0b013e318177275d. [DOI] [PubMed] [Google Scholar]
- 13.O’Connor DW, Gardner B, Presnell I, Singh D, Tsanglis M, White E. The effectiveness of continuation-maintenance ECT in reducing depressed older patients’ hospital re-admissions. J Affect Disord. 2010;120:62–66. doi: 10.1016/j.jad.2009.04.005. [DOI] [PubMed] [Google Scholar]
- 14.American Psychiatric Association . The Practice of Electroconvulsive Therapy: Recommendations for Treatment, Training, and Privileging: A Task Force Report of the American Psychiatric Association. Washington, DC, USA: American Psychiatric Association; 2001. [Google Scholar]
- 15.Rabheru K, Persad E. A review of continuation and maintenance electroconvulsive therapy. Can J Psychiatry. 1997;42:476–484. doi: 10.1177/070674379704200503. [DOI] [PubMed] [Google Scholar]
- 16.Petrides G, Tobias KG, Kellner CH, Rudorfer MV. Continuation and maintenance electroconvulsive therapy for mood disorders: review of the literature. Neuropsychobiology. 2011;64:129–140. doi: 10.1159/000328943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kellner CH, Knapp RG, Petrides G, et al. Continuation electroconvulsive therapy vs pharmacotherapy for relapse prevention in major depression – a multisite study from the consortium for research in electroconvulsive therapy (CORE) Arch Gen Psychiatry. 2006;63:1337–1344. doi: 10.1001/archpsyc.63.12.1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Suzuki K, Takano T, Ebina Y, Takamatsu K, Awata S, Matsuoka H. Continuation electroconvulsive therapy to prevent relapse of schizophrenia in relapse-prone patients. J ECT. 2007;23:204–205. doi: 10.1097/YCT.0b013e3180544972. [DOI] [PubMed] [Google Scholar]
- 19.Chanpattana W, Chakrabhand ML, Sackeim HA, et al. Continuation ECT in treatment-resistant schizophrenia: a controlled study. J ECT. 1999;15:178–192. [PubMed] [Google Scholar]
- 20.Lévy-Rueff M, Gourevitch R, Loo H, Olié JP, Amado I. Maintenance electroconvulsive therapy: an alternative treatment for refractory schizophrenia and schizoaffective disorders. Psychiatry Res. 2010;175:280–283. doi: 10.1016/j.psychres.2008.10.012. [DOI] [PubMed] [Google Scholar]
- 21.Swoboda E, Conca A, Konig P, Waanders R, Hansen M. Maintenance electroconvulsive therapy in affective and schizoaffective disorder. Neuropsychobiology. 2001;43:23–28. doi: 10.1159/000054861. [DOI] [PubMed] [Google Scholar]
- 22.Rabheru K. Maintenance electroconvulsive therapy (M-ECT) after acute response – examining the evidence for who, what, when, and how? J ECT. 2012;28:39–47. doi: 10.1097/YCT.0b013e3182455758. [DOI] [PubMed] [Google Scholar]
- 23.Lehman AF, Lieberman JA, Dixon LB, et al. American Psychiatric Association; Steering Committee on Practice Guidelines. Practice guideline for the treatment of patients with schizophrenia, second edition. Am J Psychiatry. 2004;161(2 Suppl):1–56. [PubMed] [Google Scholar]
- 24.Nijman H, Palmstierna T. Measuring aggression with the Staff Observation Aggression Scale-Revised. Acta Psychiatr Scand Suppl. 2002;412:101–102. doi: 10.1034/j.1600-0447.106.s412.21.x. [DOI] [PubMed] [Google Scholar]
- 25.Russell JC, Rasmussen KG, O’Connor M, Copeman CA, Ryan DA, Rummans TA. Long-term maintenance ECT: a retrospective review of efficacy and cognitive outcome. J ECT. 2003;19:4–9. doi: 10.1097/00124509-200303000-00002. [DOI] [PubMed] [Google Scholar]
- 26.Shibasaki C, Takebayashi M, Fujita Y, Yamakawi S. Factors associated with the risk of relapse in schizophrenic patients after a response to electroconvulsive therapy: a retrospective study. Neuropsychiatr Dis Treat. 2015;11:67–73. doi: 10.2147/NDT.S74303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kerner N, Prudic J. Current electroconvulsive therapy practice and research in the geriatric population. Neuropsychiatry. 2014;4:33–54. doi: 10.2217/npy.14.3. [DOI] [PMC free article] [PubMed] [Google Scholar]


