Abstract
A key objective of the 1993 National Institutes of Health (NIH) Revitalization Act was to ensure inclusion of minorities in clinical research. We conducted a literature search for the period from 1993 to 2013 to examine whether racial/ethnic minorities are adequately represented in published research studies of pulmonary diseases, particularly NIH-funded studies. We found a marked underrepresentation of minorities in published clinical research on pulmonary diseases. Over the last 20 years, inclusion of members of racial or ethnic minority groups was reported (in MeSH terms, journal titles, and MEDLINE fields) in less than 5% of all NIH-funded published studies of respiratory diseases. Although a secondary analysis revealed that a larger proportion of NIH-funded studies included any minorities, this proportional increment mostly resulted from studies including relatively small numbers of minorities (which precludes robust race- or ethnic-specific analyses). Underrepresentation or exclusion of minorities from NIH-funded studies is likely due to multiple reasons, including insufficient education and training on designing and implementing population-based studies of minorities, inadequate motivation or incentives to overcome challenges in the recruitment and retention of sufficient numbers of members of racial/ethnic minorities, underrepresentation of minorities among respiratory scientists in academic medical centers, and a dearth of successful partnerships between academic medical centers and underrepresented communities. This problem could be remedied by implementing short-, medium-, and long-term strategies, such as creating incentives to conduct minority research, ensuring fair review of grant applications focusing on minorities, developing the careers of minority scientists, and facilitating and valuing research on minorities by investigators of all backgrounds.
Keywords: ethnic minorities, National Institutes of Health, funding, health equality
At a Glance Commentary
Scientific Knowledge on the Subject
Racial and ethnic minority groups share a disproportionate burden from respiratory diseases. Biomedical and clinical research can have a major impact on the eradication of respiratory health disparities, provided that inclusion of racial and ethnic minorities is adequate.
What This Study Adds to the Field
Minorities are markedly underrepresented in published biomedical and clinical research on pulmonary diseases. Over the last 20 years, inclusion of members of racial or ethnic minority groups was reported (in MeSH terms, journal titles, and MEDLINE fields) in less than 5% of all National Institutes of Health–funded published studies of respiratory diseases.
In 1993, the U.S. Congress enacted the National Institutes of Health (NIH) Revitalization Act (Public Law 103-43), which was implemented in 1994. This legislative mandate had three key objectives: (1) include women and minorities as subjects in clinical research; (2) establish the Office of Research on Women’s Health; and (3) establish the Office of Research on Minority Health. Under this legislative mandate, the director of the NIH was asked to create guidelines to support outreach programs for the recruitment of women and minority subjects, to ensure inclusion of women and minorities as subjects in clinical research, and to evaluate the adequacy of such inclusion as part of peer review for grant applications.
In the 20 years since the enactment of the NIH Revitalization Act, there have been tremendous advances in the prevention and treatment of respiratory diseases. Such advances, coupled with sound educational and public health initiatives, have led to decreased use of tobacco products and markedly reduced morbidity and mortality from lung disorders, such as asthma, cystic fibrosis, chronic obstructive pulmonary disease (COPD), and lung cancer. Unfortunately, however, all racial or ethnic groups in the United States have not equally shared this substantial progress in respiratory health. In 2014, racial and ethnic minority groups continue to share a disproportionate burden from respiratory diseases (Table 1).
Table 1.
U.S. Racial and Ethnic Minority Groups Share a Disproportionate Burden of Respiratory Diseases
| Group | Condition | Disparity | Reference(s) |
|---|---|---|---|
| Puerto Ricans and African Americans | Asthma | Highest prevalence, morbidity, and mortality | 29 |
| African Americans | More likely to develop COPD at an early age | Increased susceptibility to the detrimental effects of cigarette smoking | 30 |
| Puerto Rican women | COPD | Second-highest age-adjusted mortality rate among all ethnic groups | 31 |
| Asian Americans and Pacific Islanders | Influenza and pneumonia | Sixth leading cause of death overall and fourth leading cause of death among those 65 years and older | 32 |
| African American men | Lung cancer | More prone to develop and die from lung cancer, and to present with nonlocalized disease | 33–35 |
| Hispanics and African Americans | Advanced lung cancer | More likely to have false hope about cure from chemotherapy than whites | 36 |
| African American adolescents | Obstructive sleep apnea | Disproportionately affected compared to other races/ethnicities | 37–39 |
| African Americans | Sarcoidosis and acute respiratory distress syndrome | Substantially increased risk of dying | 40 |
| Asian Americans, Native Hawaiians, and Pacific Islanders | Tuberculosis | Incidence rates are highest | 41 |
Definition of abbreviation: COPD = chronic obstructive pulmonary disease.
Biomedical and clinical research can have a major impact on the eradication of respiratory health disparities, provided that inclusion of racial and ethnic minorities is adequate. However, we hypothesized that racial and ethnic minorities continue to be markedly underrepresented in published research studies of pulmonary diseases in general, and NIH-funded studies in particular.
In this article, we examine the inclusion of minority populations in published studies on respiratory diseases from 1993 to 2013. Given that funding from the NIH is a hallmark of high-quality biomedical research, we also evaluate available data for inclusive research in NIH-funded studies published during the same time period. After finding a marked underrepresentation of minority populations in the past two decades of medical literature, we discuss potential causes and solutions to this problem.
Methods
We conducted two unique approaches to PubMed searches for data generation. The first type of search was limited to a defined list of 36 pulmonary diseases, which were used as search terms (see the online supplement). We thus conducted 37 disease-specific searches, one for each discrete disease search term plus a second term for “coal worker’s pneumoconiosis” (searched “coal worker pneumoconiosis”). We downloaded, compiled, and concatenated the list of the PubMed identification numbers (IDs) and year of publication generated from each search; we then removed duplicate publications.
In the second type of search, we queried PubMed using each pulmonary disease search term as described previously here, in conjunction with a minority search term based on U.S. Centers for Disease Control and Prevention classifications (1): “African American,” “Black,” “Latino,” “Hispanic,” “Asian,” “Asian American,” “Native American,” “American Indian,” “Alaska Native,” “Native Hawaiian,” “Pacific Islander,” and “minority.” This strategy yielded 444 searches. We repeated the process of downloading and compiling a list of the PubMed IDs and year of publication generated from each search, removing duplicate citations.
Both types of PubMed searches were restricted to studies conducted in human populations that were published between January 1, 1993 and December 31, 2013. We conducted the PubMed queries and downloads using the “RISmed” package developed for the R statistical programming language (2).
To determine which publications from our searches received NIH funding, we searched for “%NIH%” in the “Grant Number” field of the PubMed MEDLINE record. Resulting PubMed IDs for articles published between January 1, 1993 and December 31, 2013 were compared with PubMed IDs generated during our two types of PubMed searches to determine the proportion of NIH-funded pulmonary disease studies.
Because our PubMed searches would only capture inclusion of minorities for studies reporting such inclusion in MeSH terms, journal titles, and MEDLINE fields (which encompass the abstract, keywords, and other metadata) (3), we checked the full content of 100 randomly sampled articles in each category created using our PubMed searches.
Results
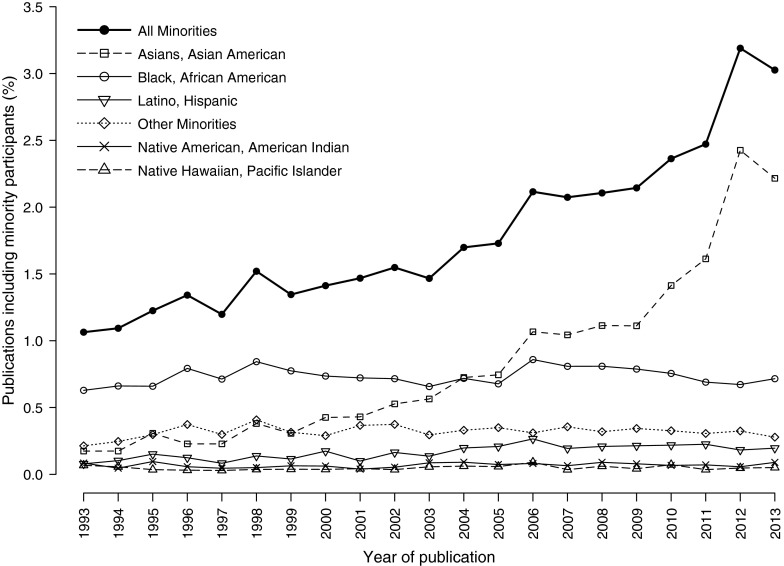
Our PubMed query yielded 737,690 unique pulmonary disease publications, of which 58,160 (7.9%) reported NIH funding. Inclusion of racial or ethnic minorities was reported in 13,117 (1.9%) of the 679,530 non–NIH-funded studies and in 2,534 (4.4%) of the 58,160 NIH-funded studies. Over the 20-year period, there was a modest increment in the proportion of non–NIH-funded publications that reported inclusion of racial or ethnic minorities, from 1.1% in 1993 to 3.0% in 2013 (Figure 1). In contrast, the percentage of the U.S. population that self-identified as nonwhite or as members of a racial or ethnic minority group increased by 46.8% from 1993 (26.5%) to 2013 (38.9%).
Figure 1.
Race-/ethnicity-specific proportions reported (in MeSH terms, journal titles, and MEDLINE fields) for non–National Institutes of Health–funded pulmonary publications in PubMed, 1993–2013. The percentage of publications involving minorities over time had a relatively flat trajectory for most racial/ethnic groups. Because a given publication may have included more than one minority group, the plot representing “All Minorities” will not necessarily sum to 100%.
Among racial or ethnic minorities included in our PubMed search, the largest proportional increment was observed in Asians or Asian Americans (from 0.2% in 1993 to 1.9% in 2013), a finding largely explained by published studies from Thailand and East Asia (see Figure E1 in the online supplement). From 1993 to 2013, there was a modest gain in the representation of African Americans, with little to no change in the profound underrepresentation of Hispanics/Latinos, Native Americans, and Hawaiians/Pacific Islanders in the published literature on respiratory diseases (Figure 1).
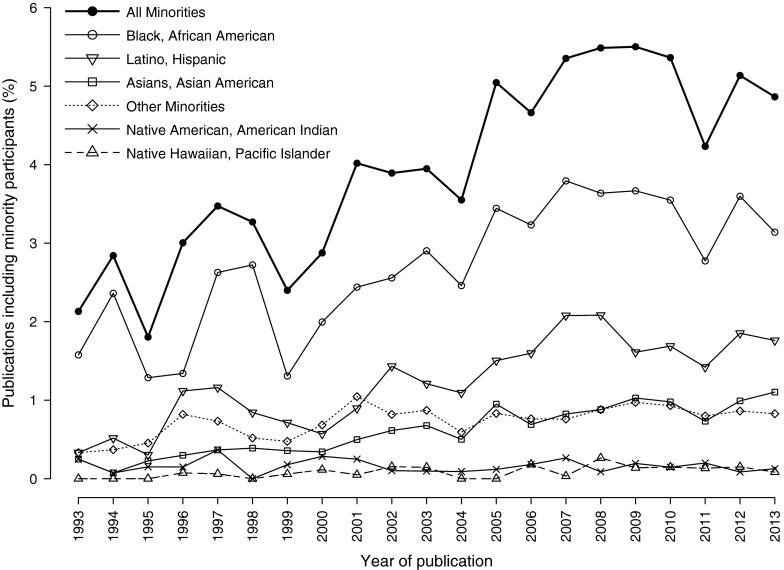
Among NIH-funded publications, there was a modest increment from 1993 to 2013 in the proportion of published studies reporting inclusion of African Americans, Hispanics/Latinos, Asian or Asian Americans, and others. On the other hand, there was little change in the very low proportion of published studies that reported inclusion of Native Americans or Hawaiians/Pacific Islanders (Figure 2).
Figure 2.
Race-/ethnicity-specific proportions reported (in MeSH terms, journal titles, and MEDLINE fields) for National Institutes of Health–funded pulmonary publications in PubMed, 1993–2013. The percentage of publications involving minorities showed a modest increase over time for some racial/ethnic groups. Because a given publication may have included more than one minority group, the plot representing “All Minorities” will not necessarily sum to 100%.
As a confirmatory analysis to assess the accuracy of our literature search for non–NIH-funded studies, we examined 100 randomly sampled minority-based search results, as well as 100 randomly sampled non–minority-based search results (i.e., sampled after excluding minority-related PMIDs). We found that 24 minority-based search results were inapplicable, as they were not pulmonary disease–related publications involving human subjects: 12 were opinion, editorial, or review articles; six were based on cell or animal models; three were not related to pulmonary disease (although they had pulmonary terms in the abstracts); one was pulmonary related, but inaccessible; and the remaining two were a meta-analysis and a methodological paper. Of the remaining 76 minority-based search results, inclusion of minorities was confirmed for 68 (89.5%) studies. Among the non–minority-based search results, 44 publications were excluded (3 were inaccessible, 21 did not involve human populations, and 20 did not use primary data [e.g., editorials, meta-analyses, and review articles]). Minorities were explicitly included in 28 of these 56 studies (50.0%). However, after excluding 23 studies that were conducted in countries considered source populations for U.S. minorities, the proportion of minorities in our non–minority-based sample dropped to 8.9%; the corresponding proportion for the minority-based search was 94.9%. Racial/ethnic characteristics could not be determined for 27 non–minority-based studies, potentially allowing for a greater proportion of minority representation among our non–minority-based sample. However, six of those studies were conducted in countries considered source populations for U.S. minorities, and another six were conducted in countries with predominantly white European populations (e.g., Norway, Sweden, Finland, and Denmark).
To assess the accuracy of our PubMed search for NIH-funded studies, we randomly sampled 100 non–minority-based search results citing NIH funding. We excluded 66 publications (1 was inaccessible, 6 were not pulmonary related, 36 did not involve human populations, and 23 did not use primary data). Of the remaining 34 studies, 11 (32.4%) explicitly included minorities, and were not conducted in countries considered source populations for U.S. minorities. Of interest, however, the average proportion of minorities (weighted by sample size) in these 11 non–minority-based NIH-funded studies was 12.3% (range = 3–34%). Moreover, only 3 of these 11 studies included a substantial proportion (≥25%) of minorities, although sample sizes tended to be relatively small (average = 161). Thus, only 3 (8.8%) of the 34 NIH-funded studies categorized as nonminority by our PubMed search included a substantial proportion of minorities.
Discussion
In 2013, the U.S. Census estimated that over 123 million (∼39%) of the 316 million people living in the United States self-identified as members of a racial or ethnic minority group, as follows: Hispanics (17%); non-Hispanic blacks or African Americans (13.2%); Asians (5.3%); American Indians or Alaska Natives (1.2%); Native Hawaiians or Pacific Islanders (0.2%); and two or more races (2.4%) (4). We show a gross underrepresentation of minorities in published biomedical and clinical research on pulmonary diseases. Inclusion of members of racial or ethnic minority groups was reported in only 1.9% of all studies of respiratory disease, and in less than 5% of all NIH-funded studies of respiratory diseases published over the last 20 years.
Even though our secondary, in-depth analysis showed that a larger proportion of NIH-funded studies included any racial or ethnic minorities, this proportional increment largely resulted from detecting additional studies that included only a small proportion of racial or ethnic minorities (and thus did not report such inclusion in their MeSH terms, journal titles, or MEDLINE fields). In most cases, inclusion of a small number of members of minority groups in observational studies or clinical trials does not allow adequately powered analyses of racial- or ethnic-specific effects. For genetic studies, a common and unfortunate approach to solve this problem has been to entirely exclude minorities from analysis (5), rather than going beyond an early history of collecting data only in populations of European descent.
We may have missed studies that used terms like “Puerto Rican,” “Mexican,” or “Costa Rican,” as MEDLINE search fields do not appear to index Latinos by subgroups (i.e., these terms are not recognized as Latino or Hispanic). However, our secondary analysis and the findings of others (6–12) suggest that such underestimation is unlikely to explain our results, and corroborate our initial hypothesis that racial and ethnic minorities remain markedly underrepresented or entirely excluded from research studies. The reasons for this finding are variable, and may include insufficient education and training on the design and implementation of population-based studies of racial or ethnic minorities, inadequate motivation or incentives to overcome expected challenges in the recruitment and retention of sufficiently large numbers of members of racial and ethnic minorities, underrepresentation of racial and ethnic minorities among respiratory scientists (at the junior and senior faculty levels) in academic medical centers, and a dearth of successful partnerships between academic medical centers and members of underrepresented communities.
Genetic and environmental risk factors, as well as modifiers (e.g., healthcare access, response to and side effects from treatment) of respiratory diseases vary dramatically across racial and ethnic groups (13). Thus, underrepresentation of racial and ethnic minorities in research studies severely limits our ability to develop knowledge or awareness of racial- and ethnic-specific causes or modifiers of frequently encountered pulmonary diseases. Lack of new methods to prevent, diagnose, and treat respiratory diseases in ethnic minorities ultimately has profound financial costs. Ethnic disparities in health, for example, are estimated to have cost the United States over $1.2 trillion in medical costs between 2003 and 2006 (14). In spite of this financial incentive at a societal level and the 1993 NIH Revitalization Act, there has been a significant lack of progress in the inclusion of racial/ethnic minorities in biomedical research, and (not surprisingly) in elimination of health disparities. Over the past decade, health disparities have persisted (for 80%) or increased (for 13%) of the diseases or conditions targeted as part of the Healthy People 2010 objectives (15).
Given that the majority of respiratory diseases that disproportionately affect racial or ethnic minorities have no cure (e.g., sickle cell disease and asthma) or highly effective treatments (e.g., lung cancer), developing new means for prevention, screening, diagnosis, and management of these diseases through research studies would greatly help eliminate respiratory health disparities and thus achieve respiratory health equality. This approach should be viewed as an investment rather than an expense. In one study, the economic benefits of increased longevity attributable to biomedical research amounted to approximately $73 trillion dollars between 1970 and 1998 (16). Eliminating respiratory health disparities would almost certainly improve this return.
Credit should be given to the NIH for their funding efforts of lung disease in racial/ethnic minorities. For example, the NIH has recently funded several underrepresented minority–specific cohorts, such as the Genetics of Asthma in Latino Americans Study (17), the Jackson Heart Study (18), the Study of Latinos (19), the Strong Heart Study (20), the Consortium on Asthma Among African Ancestry Populations in the Americas (21), the Puerto Rico Genetics of Asthma and Lifestyle Study, and the Epigenetic Variation and Childhood Asthma in Puerto Ricans Study (22, 23). NIH’s funding for these cohorts is consistent with the spirit of the congressional mandate, but substantially more needs to be done by the NIH, the medical and scientific community, and the public as a whole to enact real change.
Future Directions
Short-term approaches
In recognition of the major negative impact of a reduction in the number of physician-scientists in the United States, the NIH instituted a system by which “new investigators” (those submitting a first R01 grant) can be funded if their score is within 10 percentile points of the fundable range for established investigators. We believe that the dearth of research studies in racial or ethnic minorities fully justifies a similar approach. In particular, the fundable range for studies focused exclusively on well characterized cohorts of racial or ethnic minorities should be more generous than for studies not fulfilling this requirement. We believe that this would strongly motivate researchers of all racial, ethnic, and cultural backgrounds to conduct research studies of pulmonary diseases in minorities. A complementary approach is to increase the number of requests for applications for research studies to be conducted exclusively or predominantly in racial or ethnic minority groups.
Funding agencies could also do more to collect evidence on adequate inclusion of minorities, determine what research is needed to reduce health disparities, promote research training on disparities, and provide venues for discussion of disparities in biomedical research. Moving forward, we suggest that inclusion of racial or ethnic minorities be reported in the abstract of NIH-funded studies. At a minimum, NIH-funded studies should include a substantial proportion of members of racial/ethnic groups that are most heavily affected by the diseases being investigated, so that valid conclusions can be drawn about these groups. Such efforts would not only benefit individuals affected with pulmonary diseases, but also those affected with diseases such as cancer: at present, less than 2% of clinical trials sponsored by the National Cancer Institute are focused on racial or ethnic minorities (6).
Medium-term approaches
For physicians and Ph.D. scientists, conducting patient-centered studies requires formal education and training in the general principles of clinical research, including statistics and epidemiology. This requires coursework, usually leading to a master’s degree, as well as training in all aspects of clinical research under adequate supervision and mentorship. The NIH has placed much effort on mentorship and development of minority researchers, including minority research fellowship programs, minority international research training grants, minority biomedical research support programs, initiatives for minority student development, a minority-based community oncology program, and minority high school student research programs. However, a recent study found that senior faculty at academic medical centers are less likely to be engaged or to mentor junior faculty in research studies involving minorities, a situation that clearly must be corrected (24). In the context of investigating health disparities, additional areas of study should include best practices for partnering with minority communities and community organizations, proper assessment of race/ethnicity and socioeconomic status (25), cultural sensitivity and training, building and promoting multicultural, diverse research teams, and ethical conduct of research in vulnerable populations.
Funding and career development programs for early-stage and midcareer investigators devoted to research on respiratory health in minorities must be available. Given the roadblocks encountered by all respiratory scientists, and the additional obstacles faced by researchers pursuing a career related to health disparities, early-stage investigators (who may themselves come from disadvantaged backgrounds) are more likely to abandon research in favor of more secure or lucrative teaching or clinical positions, and thus need to be provided with appropriate guidance and support. However, coursework, training, and mentoring will not have a major impact unless minority research is acknowledged as justifiable and valued by leaders at both the NIH and academic medical centers. Their commitment and response may be gauged in part by the appropriate mobilization of resources.
Long-term approaches
Addressing shortages
As discussed previously here, the entire research community should be encouraged to pursue minority research. However, physicians and scientists who belong to minority groups are more likely to provide healthcare to and conduct research in underserved populations by virtue of their upbringing and cultural background (26). Representation of minorities in healthcare professions has not kept pace with the changing demographics of the general U.S. population, thereby potentially creating even greater disparities in research and healthcare delivery and outcomes.
A study found that minority physicians and scientists (other than Asians) are markedly underrepresented in the medical community, particularly among faculty in U.S. medical schools (∼8% compared with ∼34% in the general population) (27). Similarly, minorities are underrepresented among respiratory scientists with doctoral degrees other than an M.D. Both a membership survey of the American Thoracic Society (ATS) and a survey of training directors in 1999–2000 found remarkable underrepresentation of minority physicians among ATS members or trainees in pediatric and adult fellowships in pulmonary and critical care medicine. For example, only 5.6% of ATS members self-identified as underrepresented minorities at that time. In contrast, black and Hispanic fellows represented about 13% of internal medicine residents and 10% of cardiology fellows, respectively, in 2006–2007. Thus, a more concerted and coordinated effort by medical schools, academic medical centers, and governmental agencies, such as the NIH, is needed to foster the development of minority physicians and scientists in respiratory medicine.
Reducing barriers for career advancement
Disparities are self-perpetuating. Minority scientists are often best placed to gain community “buy in” and trust in minority populations, but these scientists are at a disadvantage in other ways. For example, minority scientists often have difficulty obtaining funding. According to one analysis, black and Asian scientists in the United States are 13 and 4% less likely, respectively, to get funded than white scientists (28). Such inequalities further challenge investigators desiring to focus on minorities.
Grant applications for studies where the principle investigator is a minority often focus on health disparities, and thus should be reviewed by study sections composed of researchers who are familiar with and value minority research. Grant applications should be regarded more—and not less—favorably for studying minority populations. To increase the representation of minorities in publications, we strongly favor the inclusion of qualified physicians and scientists who belong to minority groups or who predominantly conduct research on minorities in the respiratory field journals’ editorial boards.
Once minority physicians and scientists enter an academic career in respiratory medicine, development and support of adequate skills obtained by adequate education and training is essential (see previous discussion). Lack of publication in high-impact journals may discourage future research in the field and investigators from exploring the field. Similarly, many academic institutions promote based on the impact of an investigator’s research. As a result, even promotion and tenure can be affected. The current dearth of minority respiratory researchers in decision-making bodies, including promotion committees, NIH study sections, and honorary societies, must be remedied to enhance advocacy for minority scientists and minority research.
Finally, investigators must reach out to healthcare providers and residents within diverse underrepresented communities and invite them to form active partnerships that improve health and reduce disparities, so that members of the healthcare and general communities have a vested interest in studies relevant to racial/ethnic minorities.
Conclusions
Our data demonstrate that inclusion of racial and ethnic minority groups—who, collectively, are expected to outnumber non-Hispanic whites by 2043—was reported in only 4.4% of NIH-funded publications on pulmonary diseases from 1993 to 2013. Although nearly one-third of the NIH-funded studies categorized by our PubMed search as nonminority were found to include some minorities, only a few of these studies (3 of 34 [8.8%]) included a substantial proportion of minorities (≥25%). In spite of tangible efforts by the NIH, racial and ethnic minorities continue to be markedly underrepresented in biomedical research of pulmonary diseases.
We believe that this problem can be remedied by implementing vigorous short-, medium-, and long-term strategies. Such approaches include creating incentives to conduct minority research, ensuring fair review of grant applications focusing on minorities, developing and fostering the careers of minority scientists and physician-scientists, and facilitating and valuing research on minorities by investigators of all backgrounds.
The NIH, the medical and scientific communities (including organizations, such as the ATS), the general public, and policy makers need to work together to rectify the unjust exclusion of racial or ethnic minorities from respiratory research. Acting as one, we must guarantee that all Americans are equal beneficiaries of federally funded programs.
Acknowledgments
Acknowledgment
The authors thank Danielle de Bruin, Jonathan Witonsky, Chris Gunter, Maria Pino Yanes, Joshua Galanter, and Pedro Avila for their helpful comments, analysis, and editing of the manuscript.
Footnotes
Supported by National Institutes of Health grants R01-ES015794, R01-HL088133, R01-HL078885, R25-CA113710, T32-GM007546, R01-HL004464, R01-HL104608, HL117004, and P60MD006902 (E.G.B.), HL04370, HL079966, HL117191, and HL073373 (J.C.C.), and K01HL092601 (M.G.F.), the Flight Attendant Medical Research Institute, RWJF Amos Medical Faculty Development Award, the Sandler Foundation, the American Asthma Foundation (E.G.B.), and by an endowment from the Heinz Foundation (J.C.C.).
Author Contributions: Conception and design—E.G.B. and J.C.C.; analysis and interpretation—E.G.B., S.S.O., and J.C.C.; drafting the manuscript for important intellectual content—E.G.B., S.S.O., M.G.F., and J.C.C.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org
Originally Published in Press as DOI: 10.1164/rccm.201410-1944PP on January 13, 2015
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.U.S. Centers for Disease Control and PreventionCDC–populations–definitions–racial–ethnic–minorities–minority health–definitions [accessed 2014 Oct 29]. Available from: http://www.cdc.gov/minorityhealth/populations/REMP/definitions.html
- 2.Kovalchik S.RISmed: download content from NCBI databases. R package version 2.1.2. CRANR-projectorg, 2nd ed. [accessed 2014 Aug 7]. Available from: http://CRAN.R-project.org/package=RISmed
- 3.U.S. National Library of MedicinePubMed BASICS [accessed 2014 Aug 11]. Available from: http://nnlm.gov/training/resources/pmtri.pdf
- 4.U.S. Department of Commerce/U.S. Census BureauState & County QuickFacts [accessed 2014 Aug 20]. Available from: http://quickfacts.census.gov/qfd/states/00000.html
- 5.Shriner D, Adeyemo A, Ramos E, Chen G, Rotimi CN. Mapping of disease-associated variants in admixed populations. Genome Biol. 2011;12:223. doi: 10.1186/gb-2011-12-5-223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen MS, Jr, Lara PN, Dang JHT, Paterniti DA, Kelly K. Twenty years post-NIH Revitalization Act: Enhancing Minority Participation in Clinical Trials (EMPaCT): laying the groundwork for improving minority clinical trial accrual: renewing the case for enhancing minority participation in cancer clinical trials. Cancer. 2014;120:1091–1096. doi: 10.1002/cncr.28575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sullivan PS, McNaghten AD, Begley E, Hutchinson A, Cargill VA. Enrollment of racial/ethnic minorities and women with HIV in clinical research studies of HIV medicines. J Natl Med Assoc. 2007;99:242–250. [PMC free article] [PubMed] [Google Scholar]
- 8.Murthy VH, Krumholz HM, Gross CP. Participation in cancer clinical trials: race-, sex-, and age-based disparities. JAMA. 2004;291:2720–2726. doi: 10.1001/jama.291.22.2720. [DOI] [PubMed] [Google Scholar]
- 9.Braunstein JB, Sherber NS, Schulman SP, Ding EL, Powe NR. Race, medical researcher distrust, perceived harm, and willingness to participate in cardiovascular prevention trials. Medicine (Baltimore) 2008;87:1–9. doi: 10.1097/MD.0b013e3181625d78. [DOI] [PubMed] [Google Scholar]
- 10.Wissing MD, Kluetz PG, Ning Y-M, Bull J, Merenda C, Murgo AJ, Pazdur R. Under-representation of racial minorities in prostate cancer studies submitted to the US Food and Drug Administration to support potential marketing approval, 1993–2013. Cancer. 2014;120:3025–3032. doi: 10.1002/cncr.28809. [DOI] [PubMed] [Google Scholar]
- 11.Mak WWS, Law RW, Alvidrez J, Pérez-Stable EJ. Gender and ethnic diversity in NIMH-funded clinical trials: review of a decade of published research. Adm Policy Ment Health. 2007;34:497–503. doi: 10.1007/s10488-007-0133-z. [DOI] [PubMed] [Google Scholar]
- 12.Thomson GE, Mitchell F, Williams MB Institute of Medicine (US) Committee on the Review and Assessment of the NIH’s Strategic Research Plan and Budget to Reduce and Ultimately Eliminate Health Disparities. Washington, DC: National Academies Press; 2006. Examining the Health Disparities Research Plan of the National Institutes of Health: unfinished business. [PubMed] [Google Scholar]
- 13.Celedón JC, Roman J, Schraufnagel DE, Thomas A, Samet J. Respiratory health equality in the United States: the American Thoracic Society perspective. Ann Am Thorac Soc. 2014;11:473–479. doi: 10.1513/AnnalsATS.201402-059PS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The economic burden of health inequalities in the United States. Washington, DC: Joint Center for Political and Economic Studies. 2009[accessed 2014 Sept 3]. Available from: http://jointcenter.org/research/fact-sheet-economic-burden-health-inequalities-united-states
- 15.National Center for Health StatisticsHealthy People 2010: final review. Washington, DC: U.S. Government Printing Office; 2012 [Google Scholar]
- 16.Murphy K, Topel R. Diminishing returns? The costs and benefits of improving health. Perspect Biol Med. 2003;46(3 suppl):S108–S128. [PubMed] [Google Scholar]
- 17.Burchard EG, Avila PC, Nazario S, Casal J, Torres A, Rodriguez-Santana JR, Toscano M, Sylvia JS, Alioto M, Salazar M, et al. Genetics of Asthma in Latino Americans (GALA) Study. Lower bronchodilator responsiveness in Puerto Rican than in Mexican subjects with asthma. Am J Respir Crit Care Med. 2004;169:386–392. doi: 10.1164/rccm.200309-1293OC. [DOI] [PubMed] [Google Scholar]
- 18.Sempos CT, Bild DE, Manolio TA. Overview of the Jackson Heart Study: a study of cardiovascular diseases in African American men and women. Am J Med Sci. 1999;317:142–146. doi: 10.1097/00000441-199903000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Daviglus ML, Pirzada A, Talavera GA. Cardiovascular disease risk factors in the Hispanic/Latino population: lessons from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL) Prog Cardiovasc Dis. 2014;57:230–236. doi: 10.1016/j.pcad.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 20.Dixon AE, Yeh F, Welty TK, Rhoades ER, Lee ET, Howard BV, Enright PL. Asthma in American Indian adults: the Strong Heart Study. Chest. 2007;131:1323–1330. doi: 10.1378/chest.06-1968. [DOI] [PubMed] [Google Scholar]
- 21.Consortium on Asthma among African-Ancestry Populations in the Americas (CAAPA) [accessed 2014 Sept 24]. Available from: http://www.caapaproject.net
- 22.Brehm JM, Acosta-Pérez E, Klei L, Roeder K, Barmada MM, Boutaoui N, Forno E, Cloutier MM, Datta S, Kelly R, et al. African ancestry and lung function in Puerto Rican children. J Allergy Clin Immunol. 2012;129:1484–1490.e6. doi: 10.1016/j.jaci.2012.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rosas-Salazar C, Ramratnam SK, Brehm JM, Han Y-Y, Boutaoui N, Forno E, Acosta-Pérez E, Alvarez M, Colón-Semidey A, Canino G, et al. Prematurity, atopy, and childhood asthma in Puerto Ricans. J Allergy Clin Immunol. 2014;133:357–362. doi: 10.1016/j.jaci.2013.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Beech BM, Calles-Escandon J, Hairston KG, Langdon SE, Latham-Sadler BA, Bell RA. Mentoring programs for underrepresented minority faculty in academic medical centers: a systematic review of the literature. Acad Med. 2013;88:541–549. doi: 10.1097/ACM.0b013e31828589e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Isaacs SL, Schroeder SA. Class—the ignored determinant of the nation’s health. N Engl J Med. 2004;351:1137–1142. doi: 10.1056/NEJMsb040329. [DOI] [PubMed] [Google Scholar]
- 26.Marrast LM, Zallman L, Woolhandler S, Bor DH, McCormick D. Minority physicians’ role in the care of underserved patients: diversifying the physician workforce may be key in addressing health disparities. JAMA Intern Med. 2014;174:289–291. doi: 10.1001/jamainternmed.2013.12756. [DOI] [PubMed] [Google Scholar]
- 27.Guevara JP, Adanga E, Avakame E, Carthon MB. Minority faculty development programs and underrepresented minority faculty representation at US medical schools. JAMA. 2013;310:2297–2304. doi: 10.1001/jama.2013.282116. [DOI] [PubMed] [Google Scholar]
- 28.Ginther DK, Schaffer WT, Schnell J, Masimore B, Liu F, Haak LL, Kington R. Race, ethnicity, and NIH research awards. Science. 2011;333:1015–1019. doi: 10.1126/science.1196783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rosser FJ, Forno E, Cooper PJ, Celedón JC. Asthma in Hispanics: an 8-year update. Am J Respir Crit Care Med. 2014;189:1316–1327. doi: 10.1164/rccm.201401-0186PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Foreman MG, Zhang L, Murphy J, Hansel NN, Make B, Hokanson JE, Washko G, Regan EA, Crapo JD, Silverman EK, et al. COPDGene Investigators. Early-onset chronic obstructive pulmonary disease is associated with female sex, maternal factors, and African American race in the COPDGene Study. Am J Respir Crit Care Med. 2011;184:414–420. doi: 10.1164/rccm.201011-1928OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brehm JM, Celedón JC. Chronic obstructive pulmonary disease in Hispanics. Am J Respir Crit Care Med. 2008;177:473–478. doi: 10.1164/rccm.200708-1274PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.American Lung AssociationState of lung disease in diverse communities 2010[accessed 2014 Oct 8]. Available from: http://www.lung.org/assets/documents/publications/lung-disease-data/solddc_2010.pdf
- 33.Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z, et al. editors. SEER cancer statistics review, 1975–2011 [based on November 2013 SEER data submission]. Bethesda, MD: National Cancer Institute. 2014. Apr [accessed 2014 Oct 8]. Available from: http://seer.cancer.gov/csr/1975_2011/
- 34.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63:11–30. doi: 10.3322/caac.21166. [DOI] [PubMed] [Google Scholar]
- 35.Alberg AJ, Nonemaker J. Who is at high risk for lung cancer? Population-level and individual-level perspectives. Semin Respir Crit Care Med. 2008;29:223–232. doi: 10.1055/s-2008-1076742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Weeks JC, Catalano PJ, Cronin A, Finkelman MD, Mack JW, Keating NL, Schrag D. Patients’ expectations about effects of chemotherapy for advanced cancer. N Engl J Med. 2012;367:1616–1625. doi: 10.1056/NEJMoa1204410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Spilsbury JC, Storfer-Isser A, Kirchner HL, Nelson L, Rosen CL, Drotar D, Redline S. Neighborhood disadvantage as a risk factor for pediatric obstructive sleep apnea. J Pediatr. 2006;149:342–347. doi: 10.1016/j.jpeds.2006.04.061. [DOI] [PubMed] [Google Scholar]
- 38.Johnson EO, Roth T. An epidemiologic study of sleep-disordered breathing symptoms among adolescents. Sleep. 2006;29:1135–1142. doi: 10.1093/sleep/29.9.1135. [DOI] [PubMed] [Google Scholar]
- 39.Rudnick EF, Walsh JS, Hampton MC, Mitchell RB. Prevalence and ethnicity of sleep-disordered breathing and obesity in children. Otolaryngol Head Neck Surg. 2007;137:878–882. doi: 10.1016/j.otohns.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 40.Mirsaeidi M, Machado RF, Schraufnagel D, Sweiss NJ, Baughman RP. Racial difference in sarcoidosis mortality in the United States. Chest. 2015;147:438–449. doi: 10.1378/chest.14-1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.U.S. Centers for Disease Control and PreventionReported tuberculosis in the United States, 2013. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; October 2014