Abstract
A growing body of literature has identified size reductions of the corpus callosum (CC) in autism. However, to our knowledge, no published studies have reported on the growth of CC volumes in youth with autism. Volumes of the total CC and its sub-divisions were obtained from 23 male children with autism and 23 age-matched male controls at baseline and 2-year follow-up. Persistent reductions in total CC volume were observed in participants with autism relative to controls. Only the rostral body sub-division showed a normalization of size over time. Persistent reductions are consistent with the diagnostic stability and life-long impairment observed in many individuals with autism. Multimodal imaging studies are needed to identify specific fiber tracks contributing to CC reductions.
Keywords: magnetic resonance imaging, autism, corpus callosum, rostral body
Autism represents a set of etiologically heterogeneous neurodevelopmental disorders that share core deficits in social interaction, communication, and stereotyped or repetitive behaviors (American Psychiatric Association, 2000; Geschwind, 2007). Brain abnormalities in autism have been well documented in cross-sectional neuroimaging studies (Amaral, Schumann, & Nordahl, 2008; Brambilla et al., 2003; Pardo & Eberhart, 2007), including both structural and functional investigations. Findings from these studies have suggested that abnormal neural connectivity, involving short- and long-distance connections, may contribute to the development of autism symptoms (Courchesne & Pierce, 2005; Just, Cherkassky, Keller, Kana, & Minshew, 2007). However, a limited number of investigations have directly examined age-related brain changes in autism and their relationships to autism symptomatology. Identifying these changes and associations will be vital to understanding the developmental trajectory of neural connectivity in autism and its relation to diagnosis and symptom progression since the course might be more informative than the final outcome (Amaral, et al., 2008; Hardan, Libove, Keshavan, Melhem, & Minshew, 2009).
Recent studies, although limited in number, have examined the developmental course of the clinical features of autism over the life span. Clinical diagnoses tend to be quite stable through childhood, with one well-designed study showing that the vast majority of individuals receiving autism spectrum diagnoses at age 2 continue to meet diagnostic criteria at age 9 (Lord et al., 2008). In contrast, clinical accounts of the life course of individuals with autism describe considerable variations in symptom development. Some children lose skills over time, others seem to reach a plateau in adolescence, and others experience an improvement in some aspects of their deficits into adulthood (Billstedt, Gillberg, & Gillberg, 2005; Eaves & Ho, 2008; Howlin, Goode, Hutton, & Rutter, 2004; Kanner, 1971; Kobayashi, Murata, & Yoshinaga, 1992; Lotter, 1974; Rutter, 1967). In fact, studies have found improvements in social interaction, in the use of non-verbal behaviors, and in repetitive and stereotyped behaviors during late childhood and adolescence (Bolte, Dickhut, & Poustka, 1999; Charman et al., 2005; Esbensen, Seltzer, Lam, & Bodfish, 2009; Piven, Harper, Palmer, & Arndt, 1996; Seltzer et al., 2003). Some investigations have also reported improvements in verbal abilities throughout childhood (Charman, et al., 2005) and improved performance on first-order false belief and theory of mind tasks (Ozonoff & McEvoy, 1994; Ozonoff, Pennington, & Rogers, 1991; Ozonoff, Rogers, & Pennington, 1991). These observations of symptom and cognitive improvements are very encouraging and reflect ongoing maturation of the relevant neural circuitry; but the exact changes in the underlying neurobiology and neuroanatomy have yet to be investigated.
Over the last two decades, considerable evidence has emerged to support age-related changes in brain structures in autism. Neuropathologic investigations have reported an increase in brain size, with data indicating that this enlargement may be present in children but not adults. (Bailey et al., 1993; Bailey et al., 1998; Kemper & Bauman, 1998). Neuroimaging investigations of brain volume have also reported brain enlargement in autism (Bailey, et al., 1998; Courchesne, Carper, & Akshoomoff, 2003; Courchesne et al., 2001; Hardan, Minshew, Mallikarjuhn, & Keshavan, 2001; Lainhart, 2003; Piven et al., 1995; Redcay & Courchesne, 2005), with the largest increases being for grey matter (Amaral, et al., 2008; Courchesne, et al., 2001) and occurring early in childhood. These studies further suggest normalization occurring later in childhood and early adolescence and longitudinal investigations are underway to further specify the timing of these changes. Developmental changes have also been reported in surface parameters, with increased cortical thickness in young children that disappears in early adolescence (Hardan, Libove, et al., 2009). Similarly, increases in amygdala size have been described in young children with autism (Mosconi et al., 2009; Schumann, Barnes, Lord, & Courchesne, 2009), evolving into either size normalization or smaller amygdala in adolescence and adulthood (Nacewicz et al., 2006).
Cross-sectional and age-related corpus callosum (CC) structural abnormalities have been reported. Specifically, several investigations have reported reductions in corpus callosum (CC) mid-sagittal area (Boger-Megiddo et al., 2006; Egaas, Courchesne, & Saitoh, 1995; Just, et al., 2007; Manes et al., 1999; Piven, Bailey, Ranson, & Arndt, 1997; Vidal et al., 2006), volume (Hardan et al., 2009; Keary et al., 2009; Spencer et al., 2006; Waiter et al., 2005), density (Chung, Dalton, Alexander, & Davidson, 2004; Waiter, et al., 2005), and integrity (Alexander et al., 2007; Barnea-Goraly et al., 2004; Keller, Kana, & Just, 2007). A recent meta-analysis by our group confirmed total CC area reductions (Frazier & Hardan, 2009), including larger CC decreases in anterior regions, congruent with executive functioning and fine motor deficits in many individuals with autism (Hardan, Kilpatrick, Keshavan, & Minshew, 2003; Larson & Mostofsky, 2006). While substantial evidence has accrued regarding cross-sectional abnormalities, the developmental course of CC reductions is less clear. One study identified CC reductions very early in life (Boger-Megiddo, et al., 2006) and evidence from other studies, including the recently published meta-analysis, revealed a larger discrepancy with increasing age. However, the exact impact of age on CC development, and consequently on cognitive functions, will require longitudinal investigations and no such studies have been published thus far.
The primary aim of the present study was to examine changes in the CC in children and adolescents with autism and age- and gender-matched healthy controls scanned twice over a 2-year interval. Based upon existing cross-sectional neuroimaging findings, we anticipate that persistent reduction in CC size will be observed in children and adolescents with autism. A secondary aim was to assess the relationships between CC measurements and behavioral features as measured by the CBCL (CBCL; Achenbach, 1991) and the Sensory Profile Questionnaire (SPQ; Dunn, 1999). To our knowledge this is the first study to examine CC size in a longitudinal design.
Method
The methodology of this study is identical to the CC cross-sectional study previously published by our group and included the same children who participated in it (Hardan et al., 2009).
Participants
Participants included 46 males (age range at baseline 7–13 years and follow-up 9–16 years), 23 with an autism spectrum disorder n=23 (autistic disorder n=19 and pervasive developmental disorder, not otherwise specified – PDD NOS n=4) and 23 healthy controls. Participants received initial and 2-year follow-up magnetic resonance imaging evaluations as part of a longitudinal study of structural brain changes in youth with autism. Only boys were included to limit structural variability associated with gender. Nine participants (5 autism, 4 controls) had either poor quality imaging data, could not tolerate imaging procedures, or were lost to follow-up. Thus, 37 participants (n=18 autism, n=19 controls) had complete imaging data at both time points. However, all primary analyses are based on the full sample (N=46), including individuals with missing observations, using statistical methods tolerant of missing time points.
Autism participants included children who met the following inclusion criteria: 1) diagnosis of autistic disorder or PDD NOS through expert clinical evaluation and two structured research diagnostic instruments including the Autism Diagnostic Interview-Revised (ADI-R) (Rutter, Le Couteur, & Lord, 2003) and the Autism Diagnostic Observation Schedule (ADOS) (Lord, Rutter, DiLavore, & Risi, 2002) and 2) absence of any neurological and genetic disorders. Those with autistic disorder met both ADI-R and ADOS criteria and those with PDD NOS met autism diagnosis on ADI-R and autism spectrum on ADOS. All subjects were medically healthy. Handedness was determined by a parent questionnaire and observation during neuropsychological testing. Socioeconomic status was assessed using the Hollingshead method (Hollingshead, 1975). Potential participants with autism were excluded if found to have evidence of an associated infectious, genetic, or metabolic disorder, such as Fragile X syndrome. Birth asphyxia, head injury, or seizure disorders were also exclusion criteria. Exclusions were based on neurologic history and examination, physical examination, and chromosomal analysis or metabolic testing, if indicated.
Typically developing control participants were recruited from surrounding communities through advertisements. Controls were recruited from areas that were socially and economically comparable to the communities from which participants with autism originated. In addition, controls were developmentally normal, free of neuropsychiatric disorders, had IQ scores ≥70, and negative family histories for neurological or psychiatric disorders. Potential control subjects were also screened to exclude those with family history of autism, developmental cognitive disorder, learning disability, affective disorder, anxiety disorder, schizophrenia, obsessive-compulsive disorder, or other neurologic or psychiatric disorders thought to have a genetic component. Additional exclusion criteria for both groups included primary sensory deficits (blindness, deafness) and paramagnetic metals in the body. After procedures were fully explained, parents of all participants or their legal guardians provided written informed consent. Verbal assent was obtained from all participants. The Institutional Review Board approved the study methodology, including MRI scanning.
Procedures
MRI scanning
MRI scans were acquired using a 1.5-T GE Signa MR Scanner (General Electric Medical Systems, Milwaukee, WI, USA) at both time points. For each subject, three different MR images were acquired and were used to generate the final segmented image: longitudinal relaxation time (T1-weighted), proton density (PD-weighted), and transverse relaxation time (T2-weighted) all acquired in the coronal plane. The T1-weighted spoiled GRASS (SPGR) sequence was acquired using the following parameters: slice thickness = 1.5 mm, slice number = 124, echo time (TE) = 5 ms, repetition time (TR) = 24 ms, flip angle = 40°, number of excitations (NEX) = 2, field of view (FOV) = 26 cm, matrix = 256×192. Both PD-weighted and T2-weighted images were obtained with the following parameters: slice thickness = 5 mm, TE = 96 ms for T2 and 36 ms for PD, TR = 3000 ms, NEX = 1, FOV = 26 cm, matrix = 256×192 with an echo train length = 8. MRI data were identified by scan number alone to retain blindness of raters and different scan numbers were used at follow-up. Image processing was performed on a SGI workstation (Silicon Graphics Inc., Mountain View, CA) using the Brain Research: Analysis of Images, Networks, and Systems 2 (BRAINS2, University of Iowa, Iowa City, IA, USA) software package (Magnotta et al., 2002). Six brain-limiting points (anterior, posterior, superior, inferior, left, and right) were then identified to normalize the image data to the standard Talairach stereotactic three-dimensional space (Talairach & Tournoux, 1988) in which the anterior-posterior commisure line specifies the x-axis, a vertical line rising from the x-axis through the interhemispheric fissure specifies the y-axis, and a transverse orthogonal line with respect to x and y coordinates specifies the z-axis. After fitting the image sequences to a standard three-dimensional space, the pixels representing grey matter, white matter, and cerebrospinal fluid were identified using a segmentation algorithm applied to the T1-weighted, T2-weighted, and PD-weighted image sequences as described elsewhere (Hardan, Libove, et al., 2009; White, Andreasen, Nopoulos, & Magnotta, 2003). Measurements were performed using the BRAINS2 masks as generated by a neural network and corrected by manual tracing (ICC >0.9). Total brain volume (TBV) was defined as the cerebrum, cerebellum, and brainstem while excluding cerebrospinal fluid. The same procedures were used for baseline (Time 1) and follow-up (Time 2) scans.
Corpus callosum measurements
Volume of the CC was generated by tracing the CC on the mid-sagittal slice and the 6 adjacent para-sagittal slices on each side, as obtained from the reformatted SPGR acquisition. The methodology of CC measurements has previously been published (Hardan, Pabalan, et al., 2009; Keary, et al., 2009). The number of parasagittal slices was determined by the ability to reliably determine the CC contours on each slice. Tracings of CC on all 13 slices were conducted by raters who were blind to diagnosis and identification data. Sub-divisions were measured based on the organization developed by Witelson and used in previous studies (Hardan, Minshew, & Keshavan, 2000). The boundaries of the different sub-divisions were determined on each slice (total 13) based on the Witelson method allowing the establishment of vertical lines dividing each slice into 7 different regions (Figure 1). The anterior and posterior commissure line was used to distinguish the rostrum from the rostal body. The regions below this line were included in the rostrum and the ones above it were considered as part of the rostral body. A computer script was developed to measure the volume of the total CC and the 7 sub-divisions on all slices. Reliability measurements of CC volumes assessed on 10 scans by 2 independent raters revealed adequate intra- and inter-rater reliability (ICCs>0.93). Baseline and follow-up measurements were completed in one batch at the end of the study.
Figure 1.
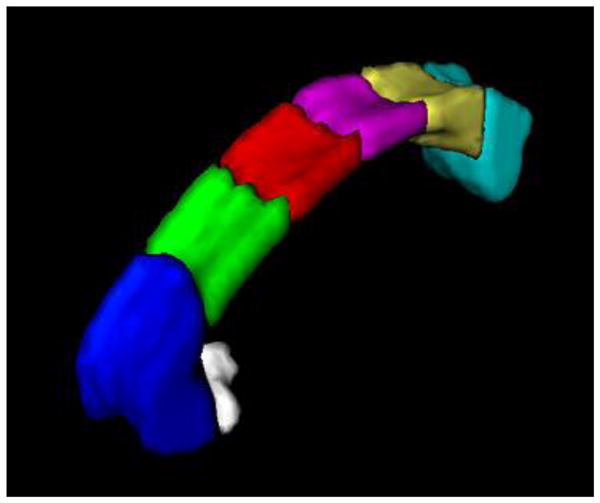
Witelson Sub-Divisions of the Corpus Callosum. Sub-division 1: rostrum in white; sub-division 2: genu in blue; sub-division 3: rostral body in green; sub-division 4: anterior-midbody in red; sub-division 5: posterior-midbody in purple; sub-division 6: isthmus in gold; sub-division 7: splenium in light blue.
Behavioral Measurements
Child Behavior Checklist (CBCL; Achenbach, 1991). The CBCL was collected at baseline and follow-up to explore whether changes in behavior problems map onto changes in CC volumes in individuals with autism. The CBCL is a 113-item parent report instrument that evaluates numerous behavior problems in youth. Only the externalizing scale was examined in the present study. Preliminary analyses indicated that the externalizing problems scale decreased from baseline to follow-up in participants with autism. Furthermore, using only the externalizing scale minimizes Type 1 error inflation due to multiple comparisons.
The Sensory Profile Questionnaire (SPQ; Dunn, 1999). The SPQ was collected to explore whether baseline difficulties with sensory-motor function are related to CC volume changes over time. The SPQ is a 125-item parent-report measure that includes 13 sections evaluating sensory-motor difficulties and the influence of sensory-motor processing on coping and appropriate behavior.
Analytic Plan
Mixed effects regression models estimated group differences in CC growth. Separate models were computed for total CC volume and CC sub-divisions. Diagnostic Group (autism vs. healthy controls) was a fixed-effects factor; baseline Full Scale IQ and SES were time-invariant predictors; and Age was a time-varying covariate in each model. CC measurements at baseline and 2-year follow-up were included as repeated measures. A significant Age effect would specify CC growth with increasing age. A significant Diagnostic Group effect would indicate differences in CC volume between individuals with autism and healthy controls, irrespective of age. A significant two-way interaction between Age and Diagnostic Group would identify a unique pattern of CC growth in autism. This interaction is a longitudinal comparison where Age is a time-varying covariate (ie. each participant contributes two ages and two brain volumes to the analysis), equivalent to a time by diagnostic group interaction in a traditional repeated measures ANOVA model.
Mixed effects regression models are advantageous to repeated measures ANOVA in that they accommodate missing time points, explicitly evaluate the effects of age rather than the time of the measurement (baseline, follow-up), directly model the relationship between age and brain volumes, and utilize all available data. Model fit was considered by iteratively examining random effects and alternative covariance structures (Bryk & Raudenbush, 1992; Kreft, 1995; Peugh & Enders, 2005). Inclusion of random effects did not substantially enhance model fit. Final models presented are based on fixed effects and an autoregressive covariance structure appropriate for longitudinal data.
Results are presented with covariate adjustment (SES, Full Scale IQ, and total white matter) to more precisely estimate group differences in CC development. Analogous mixed effects regression models were used in a recent longitudinal study of the amygdala in autism (Mosconi, et al., 2009). Two additional models were computed with total brain volume and total white matter as dependent variables to assist in interpreting CC findings relative to global brain volumes.
For each mixed effects regression model, F-tests for the main and interaction terms were converted to Cohen’s d to examine the magnitude of these effects. Conventions for interpretation of Cohen’s d were small (d=.20), medium (d=.50), and large (d=.80) (Cohen, 1987). The effect size for Age gives the magnitude of growth in the CC regardless of diagnosis. The effect size for Diagnostic Group gives the magnitude of group differences in the CC regardless of age. The effect size for the interaction term of Age and Diagnostic Group gives the magnitude of group differences in the slope of CC growth (Rosenthal, 1991).
For any CC measurement showing a significant interaction, an exploratory regression was computed with changes in externalizing behavior on the CBCL predicting CC volume changes. Exploratory regressions were also computed with baseline ratings from the 13 sections of the SPQ and total ADI-R and ADOS scores predicting CC volume changes. A false discovery rate (multiple comparisons) correction was used to control experiment-wise Type 1 error rate (.05) for these 15 analyses. Analyses were computed only in autism participants.
Pearson correlations among volume changes in total white matter, total CC, and CC sub-divisions were computed to determine whether groups showed a different pattern of white matter development. Correlations were computed separately for autism and healthy control participants. Volume changes in these analyses were difference scores (Δ=2-Year Follow-Up – Baseline). All statistical analyses used α=.05 to determine statistical significance.
Results
Power
Power to detect group differences in the growth of the CC was conservatively estimated using a repeated measures ANOVA model where the interaction of Diagnostic Group (autism vs. controls) and Time (Baseline, 2-year follow-up) was the effect of interest. Using a total sample size of 46 (n=23 in both groups) and assuming a medium effect size (f=.25), power to detect a unique pattern of CC growth in autism was excellent (.91; α=.05, two-tailed). This approach is likely to lead to an underestimate in the actual power based on the fact that repeated measures ANOVA is likely less powerful than mixed effect regression modeling and the above power analysis does not take into account increases in the functional effect size as a result of a positive correlation between repeated measures. In the present data, the correlation between total CC at baseline and 2-year follow-up was .92. In this situation, an observed effect size of f=.25 yields a much larger functional effect size of f=.60. Thus, the present study was well powered to detect significant group differences in CC volumes.
Attrition and Baseline Comparisons
Individuals with incomplete imaging data across time points did not significantly differ from individuals with complete data in terms of age at baseline or follow-up, time between scans, baseline IQ measures, or autism symptom ratings on the ADI-R or ADOS. Individuals who completed both scans showed a trend toward lower SES than individuals with incomplete data (t(44)=1.89, p=.066). For this reason, and to be conservative, SES was included as a covariate in regression models. Nine of the children with autism were taking psychotropic medications and most of them were either taking a psychostimulant or a selective serotonin reuptake inhibitor, with only one subject receiving the atypical antipsychotic risperidone.
Controls were comparable to individuals with autism with regard to age at baseline and follow-up, time differences between first and second scans, socioeconomic status, total brain, total grey matter, and total white matter volumes (Table 1). The time between scans and the age of participants with autism at Time 2 were slightly larger (although non-significantly) relative to controls. This was likely due to the attempts to recruit participants with autism first, which led to a larger time interval between the two scans in this group compared to controls. Full-scale IQ was significantly higher in the control group (p<.001), but remained in the average range in individuals with autism. Individuals with autism were more likely to be left hand dominant (p=.040), but including handedness as a covariate in subsequent analyses did not alter the pattern of findings.
Table 1.
Baseline clinical characteristics of participants with autism and typically developing controls.
| Autism M (SD) |
Healthy Controls M (SD) |
t/χ2 (p) | |
|---|---|---|---|
| N | 23 | 23 | |
| Age at Time 1 (range) | 10.59 (8–12) | 10.55 (7–13) | 0.09 (.928) |
| Age at Time 2 (range) | 13.14 (9–15) | 12.45 (9–16) | 1.34 (.189) |
| Δ in age: (years) | 2.35 (0.73) | 1.91 (0.98) | −1.48 (.149) |
| SES | 4.52 (0.59) | 4.39 (0.58) | −0.75 (.456) |
| Handedness (% Right) | 73.91% | 95.65% | 4.21 (.040) |
| FSIQ | 94.61 (20.02) | 116.17 (13.20) | 4.31 (<.001) |
| VIQ | 93.52 (17.65) | 112.65 (14.70) | 4.00 (<.001) |
| PIQ | 96.48 (21.78) | 116.48 (12.99) | 3.78 (.001) |
| ADI-R Total | 51.35 (7.45) | ||
| ADOS Total | 15.52 (3.01) |
Note. SES=Socioeconomic status, FSIQ=full scale intelligence quotient, VIQ=Verbal intelligence quotient, PIQ=Performance intelligence quotient. DF=44, except Δ Time 2-Time 1 DF=35 and Age at Time 2 DF=38. Δ in age = Change in age between follow-up and baseline in years.
Change Over Time
Global volumes
Table 2 presents total brain volume (TBV), total white matter (TWM), total CC, and CC sub-division volumes at baseline and follow-up. This table includes effect sizes (Cohen’s d) for the main effects of Age and Diagnostic Group and their interaction. TBV remained stable across age - increasing only very slightly when accounting for participant attrition - and there were no diagnostic group differences. TWM showed small increases with age and these changes were slightly larger in the autism group. However, the Age, Diagnosis, or Age by Diagnosis effects were not significant for either TBV or TWM (smallest p=.173).
Table 2.
Corpus callosum volumes (cm3) at baseline and 2-year follow-up.
| Time 1 | Time 2 |
Age Cohen’s d |
Dx. Cohen’s d |
Age X Dx. Cohen’s d |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Autism (N=22) | Controls (N=23) | Autism (N=19) | Controls (N=19) | ||||||||
| M | SD | M | SD | M | SD | M | SD | ||||
| TBV | 1349 | 119 | 1350 | 103 | 1347 | 126 | 1340 | 97 | .17 | .06 | .12 |
| TWM | 482 | 42 | 493 | 47 | 491 | 51 | 496 | 37 | .34 | .34 | .33 |
| Total CC | 5.83 | 1.04 | 6.63 | .88 | 6.24 | 1.05 | 6.82 | .94 | 1.82* | .49* | .30 |
| Rostrum | .06 | .06 | .08 | .05 | .09 | .05 | .08 | .05 | .40 | .11 | .04 |
| Genu | 1.62 | .36 | 1.75 | .27 | 1.71 | .35 | 1.83 | .33 | .87* | .03 | .09 |
| Rostral Body | .65 | .20 | .75 | .11 | .72 | .19 | .73 | .12 | .32 | .64* | .67* |
| Anterior Mid-Body | .59 | .17 | .68 | .11 | .67 | .16 | .71 | .12 | 1.40* | .31 | .05 |
| Posterior Mid-Body | .53 | .14 | .61 | .10 | .61 | .13 | .65 | .10 | 1.44* | .24 | .16 |
| Isthmus | .55 | .16 | .64 | .19 | .61 | .18 | .64 | .20 | .41 | .40 | .30 |
| Splenium | 1.77 | .38 | 2.07 | .47 | 1.89 | .37 | 2.14 | .45 | .94* | .22 | .07 |
Note.
p<.10,
p<.05.
TBV= Total Brain Volume, TWM= Total White Matter. Age = Age Main Effect, Dx. = Diagnosis Main Effect, Age X Dx. = Interaction of Age and Diagnosis; Main effects and interactions for CC volumes do not include TWM as a covariate; d= Cohen’s d. Positive effect sizes (d) indicate increasing volume with age (Age), lower volume in the autism group (Dx.), and larger increases in volume with age in the autism group relative to the controls (Age X Dx.). All volumes are in cm3.
CC volumes
Total CC volume increased substantially with age (B= 0.14, SE= .04, p= .002) in both participant groups (Figure 2, left panel). Irrespective of diagnosis, significant volume increases with age were observed for most sub-divisions (largest p=.025) including the genu (d=.87), anterior (d=1.40) and posterior mid-bodies (d=1.44), and the splenium (d=.94). The exceptions were the rostrum (d=.40, p= .110), rostral body (d=.32, p= .266), and isthmus (d=.41, p= .134) where volume tended to remain stable with age (not accounting for diagnostic group).
Figure 2.
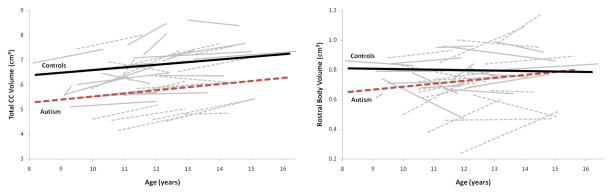
Total corpus callosum (CC; left panel) and rostral body sub-division (right panel) volumes across ages 8–16 years, separately for autism and control groups. Note: solid grey lines represent individual data from controls; dashed grey lines represent individual data from youth with autism.
Patients with autism had significantly lower total CC volumes across all ages (main effect B= −1.48, SE= .71, p= .041, d=.49) relative to healthy controls. This difference was reduced in magnitude slightly (d=.38) and no longer reached significance (p=.125) when TWM was included as a covariate. As can be seen in Figure 2 (left panel), changes with age in total CC volumes were similar across participant groups (3.1% and 1.5% increase per year in the autism and control groups respectively; p=.306).
Reductions in CC volumes for autism participants held for all the sub-divisions except the rostral body. Figure 2 (left panel) presents rostral body volumes across ages 8–16, separately for participant groups. Controls had only a slight non-significant decrease in rostral body volumes over time (1.4% decrease per year). In contrast, rostral body increased substantially in participants with autism (4.7% increase per year). At age 8, volumes were substantially lower in individuals with autism, but volumes normalized by age 14 (Age X Diagnosis interaction B= 0.03, SE= .01, p= .019; d=.67). This interaction effect remained significant (p= .008) and medium-to-large in magnitude (d= .72) when TWM was included as a covariate. There were no other significant interaction effects for other CC sub-divisions, with our without TWM as a covariate (smallest p= .122).
Correlates of CC Growth in Autism
Decreases in externalizing behavior were associated with increases in rostral body volumes in participants with autism (B=−.041, SE=.018, p=.046). Follow-up analyses indicated that this effect was primarily driven by decreases in aggression and oppositional behavior. Problems with modulating body position and movement (B=−.017, SE=.005, p=.002) and generating appropriate coping responses (B=−.004, SE=.001, p<.001) at baseline were significantly associated with rostral body increases over time. Both relationships survived false discovery correction. There was no significant relationship between baseline ADI-R (B=−.003, SE=.004, p=.448) and ADOS (B=−.006, SE=.010, p=.558) scores and changes in rostral body volumes in participants with autism.
CC Growth Patterns
To examine whether individuals with autism show a qualitatively distinct pattern of relationships in total white matter and CC growth, correlations between volume changes in TWM, total CC, and CC sub-divisions were computed separately in participants with autism and healthy controls. Correlations revealed a pattern of strong relationships in anterior and mid/body regions in healthy controls. In participants with autism, correlations were weaker and spread across anterior, mid/body, and posterior subdivisions (Table 3).
Table 3.
Correlations between volume changes in the total corpus callosum (CC) and other sub-divisions.
| ΔTotal CC | ||
|---|---|---|
| Controls | Autism | |
| ΔTotal White Matter | .32 | .02 |
| ΔW1: Rostrum | .52* | .36 |
| ΔW2: Genu | .74* | .79* |
| ΔW3: Rostral Body | .53* | .04 |
| ΔW4: Anterior Mid-Body | .82* | .60* |
| ΔW5: Posterior Mid-Body | .73* | .62* |
| ΔW6: Isthmus | .13 | .32 |
| ΔW7: Splenium | .36 | .49* |
Note. W1-7 = Witelson partitions 1–7.
p<.05. Test-retest correlations between baseline and 2-year follow-up volume measurements (not shown) were all significant (p<.001) and ranged .56–.92.
Discussion
The present study is the first to examine the developmental course of CC volume reductions in youth with autism. Results indicated that total CC volume reductions persist, but do not worsen, from childhood to adolescence. This longitudinal course contrasts with changes in cortical thickness from the same sample, where increased levels at baseline disappeared at follow-up in youths with autism compared to controls (Hardan et al., 2009). Results from the current investigation complement a large body of cross-sectional studies identifying CC reductions using samples ranging from toddlers age 3 (Boger-Megiddo, et al., 2006) to adults in their 40s (Egaas, et al., 1995; Just, et al., 2007; Keller, et al., 2007). However, a recent meta-analysis of these cross-sectional studies suggested worsening of CC reductions with age (Frazier & Hardan, 2009). It is likely that the present longitudinal results, because they directly evaluate development rather than making inferences from cross-sectional studies, more accurately estimate the trajectory of CC abnormalities in autism. Age-related meta-analytic findings may have been spurious due to sampling bias or other methodological differences across cross-sectional studies. For example, studies using older adolescents and adults tended to covary for total brain or intracranial volume when examining CC reductions (Just, et al., 2007; Piven, et al., 1997), increasing the magnitude of CC differences between participants with autism and healthy controls and potentially generating false positive findings (Tepest et al., 2010). These observations emphasize the importance of directly evaluating developmental changes using a longitudinal design, rather than using age-correlations within cross-sectional data and/or meta-analyses evaluating age effects (Amaral, et al., 2008; Giedd et al., 1999).
The present study also demonstrated that individuals with autism have a qualitatively distinct pattern of CC growth. Correlations among volume changes were weaker and spread across CC sub-divisions suggestive of a disturbed generalized axonal and/or myelination process in autism. In healthy controls, strong relationships were observed between rostral sub-divisions and total CC changes, but not with caudal subdivisions (isthmus and splenium). This pattern is consistent with ongoing frontal myelination and frontal lobe development in this age range (Giedd et al., 2009; Lenroot & Giedd, 2006). In autism, the pattern of correlations between volume changes in the total CC and sub-divisions was more distributed (genu, anterior and posterior mid-bodies, and splenium). The abnormal distribution of these relationships implies a more diffuse pattern of CC development in autism. Future longitudinal studies are needed to further specify the precise patterns of white matter development in autism and to determine whether neurobiologic abnormalities, as measured by different imaging methodologies, follow the same developmental trajectories.
The rostral body was the only CC sub-division which showed normalization by mid-adolescence. Normalization of this region appears independent of overall changes in deep white matter based on the low correlation between rostral body and total CC volume changes in individuals with autism (autism r=.04, healthy control r=.56). Interestingly, the rostral body was identified by our previous meta-analysis as showing the largest reductions of any CC sub-division (Frazier & Hardan, 2009). This region connects fiber tracks originating in pre-supplementary motor regions which support fine motor coordination, motor planning, and motor imitation; all of which are impaired in autism (Hardan, et al., 2003; Larson & Mostofsky, 2006). The rostral body has also been implicated in mirror neuron functions (Oberman & Ramachandran, 2007), facilitating attunement to others’ intentions and motivations (Gallese, 2006; Gallese, Eagle, & Migone, 2007). Normalization of the rostral body in adolescence parallels improvements in reciprocal social interaction (Piven, et al., 1996; Seltzer, et al., 2003) and repetitive behavior observed (Esbensen, et al., 2009) in sub-groups of individuals with autism (Charman, et al., 2005). In the present study, decreases in externalizing behavior were associated with rostral body volume increases. Additionally, greater problems with modulating body position and movement and generating appropriate coping responses at baseline were correlated with rostral body increases. These observations suggest that normalization of the rostral body parallels improvements in motor coordination and emotion regulation, possibly indicating an ongoing developmental or compensatory process. If replicated, these findings emphasize the role of longitudinal studies in identifying biologic correlates of phenotypic changes and prognostic factors in autism.
The primary limitations of the present study were a 1) modest sample size, 2) IQ differences between groups and medications status of children with autism, 3) participant attrition, 4) CC methodology and lack of its validation and 5) absence of more comprehensive behavioral characterization at baseline and at follow-up. Limitations in sample size, while common in labor and cost-intensive longitudinal imaging studies, reduce statistical power to detect small to medium effects. However, the fact that the present study could only detect larger effects is less problematic because smaller effects are less likely to replicate and may be less clinically interesting. This is because small effects indicate substantial overlap in structural imaging parameters between healthy and pathological groups (Giedd, et al., 2009). To address the sample size limitation, effect sizes were also presented and these can be aggregated with future longitudinal studies to increase the accuracy of estimates of developmental abnormalities in autism. The present study was also limited by IQ differences between healthy controls and participants with autism. Previous work has suggested a relationship between IQ and autism symptoms (Bennetto, Pennington, & Rogers, 1996; Spiker, Lotspeich, Dimiceli, Myers, & Risch, 2002), implying that removal of IQ through covariate adjustment may remove variance associated with the disorder (Levitt et al., 2003). In this present study, modeling IQ differences between groups did not alter the present pattern of findings, possibly because individuals with autism fell in the normal range of intellectual functioning. Participant attrition is a limitation of all longitudinal studies. Attrition in the present study was minimal given a 2-year follow-up window and slightly better than other longitudinal imaging studies examining younger participants with autism (Mosconi, et al., 2009). Statistical models that incorporate all available data were used to ensure that findings were not biased by dropout. Additionally, the measurement methodology of the CC has not been validated by postmortem studies and the lateral boundary was determined arbitrarily. Finally, without comprehensive phenotypic data at baseline and follow-up, the design prohibited correlations between changes in CC volumes and changes in symptoms.
In light of the above stated limitations, future longitudinal studies of the CC will benefit from including multiple waves of multi-modal neuroimaging as well as phenotypic data collection to maximize resolution of developmental trajectories and relationships between structural, functional, and phenotypic trends. These studies will benefit from larger sample sizes to resolve smaller effects and empirically search for subgroups of autism cases showing distinct trajectories. While larger sample sizes may require multi-site collaboration, these partnerships are desirable as they will ensure that identified sub-groups are more generalizable. Future work will also benefit from examination of sex effects and sampling a wide age range to provide a more complete developmental picture. A crucial next step will be linking developmental alterations in CC structure to developmental changes in local and distance neural connectivity, highlighting the importance of longitudinal designs in understanding the time course of brain abnormalities. Measurement of the CC will be an important component of these studies; being the largest inter-hemispheric fiber tract and connecting both homotopic and heterotopic cortical regions. As such, the CC is uniquely positioned as a structural index of developmental changes in long-distance connectivity. It is also a crucial spatial index of developmental changes in connectivity because of its topographical organization and continued maturation throughout childhood into young adulthood.
Acknowledgments
Dr. Frazier has received federal funding or research support from, acted as a consultant to, or received travel support from Shire Development, Inc., Bristol-Myers Squibb, National Institute of Health, and NARSAD. Dr. Hardan has received research grants from Bristol-Myers Squibb and Forest Pharmaceuticals. None of these directly relate to the present study. This work was directly supported by NIMH research grant MH64027 to Dr. Hardan. This publication was made possible by the Case Western Reserve University/Cleveland Clinic CTSA Grant Number UL1 RR024989 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health and NIH roadmap for Medical Research.
The authors wish to acknowledge the patients with autism, typically developing participants, and their families. Their effort and engagement was essential to the successful completion of this study.
Footnotes
Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH.
Contributor Information
Thomas W. Frazier, Cleveland Clinic
Matcheri S. Keshavan, Harvard Medical School
Nancy J. Minshew, University of Pittsburgh School of Medicine
Antonio Y. Hardan, Stanford University
References
- Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 profile. Burlington: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- Alexander AL, Lee JE, Lazar M, Boudos R, DuBray MB, Oakes TR. Diffusion tensor imaging of the corpus callosum in autism. Neuroimage. 2007;34:61–73. doi: 10.1016/j.neuroimage.2006.08.032. [DOI] [PubMed] [Google Scholar]
- Amaral DG, Schumann CM, Nordahl CW. Neuroanatomy of autism. Trends in Neurosciences. 2008;31(3):137–145. doi: 10.1016/j.tins.2007.12.005. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 2000. Text Revision. [Google Scholar]
- Bailey A, Luthert P, Bolton P, Le Couteur A, Rutter M, Harding B. Autism and megalencephaly. Lancet. 1993;341(8854):1225–1226. doi: 10.1016/0140-6736(93)91065-t. 0140-6736(93)91065-T [pii] [DOI] [PubMed] [Google Scholar]
- Bailey A, Luthert P, Dean A, Harding B, Janota I, Montgomery M. A clinicopathological study of autism. Brain. 1998;121(Pt 5):889–905. doi: 10.1093/brain/121.5.889. [DOI] [PubMed] [Google Scholar]
- Barnea-Goraly N, Kwon H, Menon V, Eliez S, Lotspeich L, Reiss AL. White matter structure in autism: preliminary evidence from diffusion tensor imaging. Biological Psychiatry. 2004;55(3):323–326. doi: 10.1016/j.biopsych.2003.10.022. S000632230301151X [pii] [DOI] [PubMed] [Google Scholar]
- Bennetto L, Pennington BF, Rogers SJ. Intact and impaired memory functions in autism. Child Development. 1996;67(4):1816–1835. [PubMed] [Google Scholar]
- Billstedt E, Gillberg IC, Gillberg C. Autism after adolescence: population-based 13- to 22-year follow-up study of 120 individuals with autism diagnosed in childhood. Journal of Autism and Developmental Disorders. 2005;35(3):351–360. doi: 10.1007/s10803-005-3302-5. [DOI] [PubMed] [Google Scholar]
- Boger-Megiddo I, Shaw DW, Friedman SD, Sparks BF, Artru AA, Giedd JN. Corpus callosum morphometrics in young children with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2006;36:733–739. doi: 10.1007/s10803-006-0121-2. [DOI] [PubMed] [Google Scholar]
- Bolte S, Dickhut H, Poustka F. Patterns of parent-reported problems indicative in autism. Psychopathology. 1999;32(2):93–97. doi: 10.1159/000029072. psp32093 [pii] [DOI] [PubMed] [Google Scholar]
- Brambilla P, Hardan A, di Nemi SU, Perez J, Soares JC, Barale F. Brain anatomy and development in autism: review of structural MRI studies. Brain Research Bulletin. 2003;61(6):557–569. doi: 10.1016/j.brainresbull.2003.06.001. S0361923003002235 [pii] [DOI] [PubMed] [Google Scholar]
- Bryk AS, Raudenbush SW. Hierarchical linear models: Applications and data analysis methods. Newbury Park, CA: Sage; 1992. [Google Scholar]
- Charman T, Taylor E, Drew A, Cockerill H, Brown JA, Baird G. Outcome at 7 years of children diagnosed with autism at age 2: predictive validity of assessments conducted at 2 and 3 years of age and pattern of symptom change over time. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2005;46(5):500–513. doi: 10.1111/j.1469-7610.2004.00377.x. JCPP377 [pii] [DOI] [PubMed] [Google Scholar]
- Chung MK, Dalton KM, Alexander AL, Davidson RJ. Less white matter concentration in autism: 2D voxel-based morphometry. Neuroimage. 2004;23:242–251. doi: 10.1016/j.neuroimage.2004.04.037. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Erlbaum; 1987. [Google Scholar]
- Courchesne E, Carper R, Akshoomoff N. Evidence of brain overgrowth in the first year of life in autism. Journal of the American Medical Association. 2003;290:337–344. doi: 10.1001/jama.290.3.337. [DOI] [PubMed] [Google Scholar]
- Courchesne E, Karns CM, Davis HR, Ziccardi R, Carper RA, Tigue ZD. Unusual brain growth patterns in early life in patients with autistic disorder: An MRI study. Neurology. 2001;57:245–254. doi: 10.1212/wnl.57.2.245. [DOI] [PubMed] [Google Scholar]
- Courchesne E, Pierce K. Why the frontal cortex in autism might be talking only to itself: local over-connectivity but long-distance disconnection. Current Opinion in Neurobiology. 2005;15(2):225–230. doi: 10.1016/j.conb.2005.03.001. S0959-4388(05)00033-4 [pii] [DOI] [PubMed] [Google Scholar]
- Dunn W. Sensory Profile. San Antonio, TX: Psychological Corporation; 1999. [Google Scholar]
- Eaves LC, Ho HH. Young adult outcome of autism spectrum disorders. Journal of Autism and Developmental Disorders. 2008;38(4):739–747. doi: 10.1007/s10803-007-0441-x. [DOI] [PubMed] [Google Scholar]
- Egaas B, Courchesne E, Saitoh O. Reduced size of corpus callosum in autism. Archives of Neurology. 1995;52:794–801. doi: 10.1001/archneur.1995.00540320070014. [DOI] [PubMed] [Google Scholar]
- Esbensen AJ, Seltzer MM, Lam KS, Bodfish JW. Age-related differences in restricted repetitive behaviors in autism spectrum disorders. Journal of Autism and Developmental Disorders. 2009;39(1):57–66. doi: 10.1007/s10803-008-0599-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frazier TW, Hardan AY. A meta-analysis of the corpus callosum in autism. Biological Psychiatry. 2009;66(10):935–941. doi: 10.1016/j.biopsych.2009.07.022. S0006-3223(09)00897-X [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallese V. Intentional attunement: a neurophysiological perspective on social cognition and its disruption in autism. Brain Research. 2006;1079(1):15–24. doi: 10.1016/j.brainres.2006.01.054. [DOI] [PubMed] [Google Scholar]
- Gallese V, Eagle MN, Migone P. Intentional attunement: mirror neurons and the neural underpinnings of interpersonal relations. Journal of the American Psychoanalytic Association. 2007;55(1):131–176. doi: 10.1177/00030651070550010601. [DOI] [PubMed] [Google Scholar]
- Geschwind D. Autism: Searching for coherence. Biological Psychiatry. 2007;62:949–950. doi: 10.1016/j.biopsych.2007.09.001. [DOI] [PubMed] [Google Scholar]
- Giedd JN, Blumenthal J, Jeffries NO, Rajapakse JC, Vaituzis AC, Liu H. Development of the human corpus callosum during childhood and adolescence: a longitudinal MRI study. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 1999;23(4):571–588. doi: 10.1016/s0278-5846(99)00017-2. S0278584699000172 [pii] [DOI] [PubMed] [Google Scholar]
- Giedd JN, Lalonde FM, Celano MJ, White SL, Wallace GL, Lee NR. Anatomical brain magnetic resonance imaging of typically developing children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48(5):465–470. doi: 10.1097/CHI.0b013e31819f2715. 00004583-200905000-00004 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardan AY, Kilpatrick M, Keshavan MS, Minshew NJ. Motor performance and anatomic magnetic resonance imaging (MRI) of the basal ganglia in autism. Journal of Child Neurology. 2003;18(5):317–324. doi: 10.1177/08830738030180050801. [DOI] [PubMed] [Google Scholar]
- Hardan AY, Libove RA, Keshavan MS, Melhem NM, Minshew NJ. A preliminary longitudinal magnetic resonance imaging study of brain volume and cortical thickness in autism. Biological Psychiatry. 2009;66(4):320–326. doi: 10.1016/j.biopsych.2009.04.024. S0006-3223(09)00508-3 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardan AY, Minshew NJ, Keshavan MS. Corpus callosum size in autism. Neurology. 2000;55(7):1033–1036. doi: 10.1212/wnl.55.7.1033. [DOI] [PubMed] [Google Scholar]
- Hardan AY, Minshew NJ, Mallikarjuhn M, Keshavan MS. Brain volume in autism. Journal of Child Neurology. 2001;16(6):421–424. doi: 10.1177/088307380101600607. [DOI] [PubMed] [Google Scholar]
- Hardan AY, Pabalan M, Gupta N, Bansal R, Melhem NM, Fedorov S. Corpus callosum volume in children with autism. Psychiatry Research. 2009;174(1):57–61. doi: 10.1016/j.pscychresns.2009.03.005. S0925-4927(09)00086-9 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingshead A. Four factor index of social status. Yale University Department of Sociology; New Haven, CT: 1975. [Google Scholar]
- Howlin P, Goode S, Hutton J, Rutter M. Adult outcome for children with autism. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2004;45(2):212–229. doi: 10.1111/j.1469-7610.2004.00215.x. [DOI] [PubMed] [Google Scholar]
- Just MA, Cherkassky VL, Keller TA, Kana RK, Minshew NJ. Functional and anatomical cortical underconnectivity in autism: evidence from an FMRI study of an executive function task and corpus callosum morphometry. Cerebral Cortex. 2007;17(4):951–961. doi: 10.1093/cercor/bhl006. bhl006 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanner L. Follow-up study of eleven autistic children originally reported in 1943. Journal of Autism and Childhood Schizophrenia. 1971;1(2):119–145. doi: 10.1007/BF01537953. [DOI] [PubMed] [Google Scholar]
- Keary CJ, Minshew NJ, Bansal R, Goradia D, Fedorov S, Keshavan MS. Corpus callosum volume and neurocognition in autism. Journal of Autism and Developmental Disorders. 2009;39(6):834–841. doi: 10.1007/s10803-009-0689-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller TA, Kana RK, Just MA. A developmental study of the structural integrity of white matter in autism. Neuroreport. 2007;18(1):23–27. doi: 10.1097/01.wnr.0000239965.21685.99. 00001756-200701080-00005 [pii] [DOI] [PubMed] [Google Scholar]
- Kemper TL, Bauman M. Neuropathology of infantile autism. Journal of Neuropathology and Experimental Neurology. 1998;57(7):645–652. doi: 10.1097/00005072-199807000-00001. [DOI] [PubMed] [Google Scholar]
- Kobayashi R, Murata T, Yoshinaga K. A follow-up study of 201 children with autism in Kyushu and Yamaguchi areas, Japan. Journal of Autism and Developmental Disorders. 1992;22(3):395–411. doi: 10.1007/BF01048242. [DOI] [PubMed] [Google Scholar]
- Kreft IGG. Hierarchical linear models: Problems and prospects. Journal of Educational and Behavioral Statistics. 1995;20(2):109–113. [Google Scholar]
- Lainhart JE. Increased rate of head growth during infancy in autism. Journal of the American Medical Association. 2003;290:393–394. doi: 10.1001/jama.290.3.393. [DOI] [PubMed] [Google Scholar]
- Larson JC, Mostofsky SH. Motor deficits in autism. In: Tuchman R, Rapin I, editors. Autism: A neurological disorder of early brain development. London: Mac Keith Press; 2006. [Google Scholar]
- Lenroot RK, Giedd JN. Brain development in children and adolescents: insights from anatomical magnetic resonance imaging. Neuroscience and Biobehavioral Reviews. 2006;30(6):718–729. doi: 10.1016/j.neubiorev.2006.06.001. S0149-7634(06)00045-5 [pii] [DOI] [PubMed] [Google Scholar]
- Levitt JG, O’Neill J, Blanton RE, Smalley S, Fadale D, McCracken JT. Proton magnetic resonance spectroscopic imaging of the brain in childhood autism. Biological Psychiatry. 2003;54(12):1355–1366. doi: 10.1016/s0006-3223(03)00688-7. S0006322303006887 [pii] [DOI] [PubMed] [Google Scholar]
- Lord C, Risi S, DiLavore PS, Shulman C, Thurm A, Pickles A. Autism from 2 to 9 years of age. Archives of General Psychiatry. 2008;63:694–701. doi: 10.1001/archpsyc.63.6.694. [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore PC, Risi S. Autism Diagnostic Observation Schedule: ADOS manual. Los Angeles, CA: Western Psychological Services; 2002. [Google Scholar]
- Lotter V. Social adjustment and placement of autistic children in Middlesex: a follow-up study. Journal of Autism and Childhood Schizophrenia. 1974;4(1):11–32. doi: 10.1007/BF02104997. [DOI] [PubMed] [Google Scholar]
- Magnotta VA, Harris G, Andreasen NC, O’Leary DS, Yuh WT, Heckel D. Structural MR image processing using the BRAINS2 toolbox. Computerized Medical Imaging and Graphics. 2002;26(4):251–264. doi: 10.1016/s0895-6111(02)00011-3. S0895611102000113 [pii] [DOI] [PubMed] [Google Scholar]
- Manes F, Piven J, Vrancic D, Nanclares V, Plebst C, Starkstein SE. An MRI study of the corpus callosum and cerebellum in mentally retarded autistic individuals. The Journal of Neuropsychiatry and Clinical Neurosciences. 1999;11:470–474. doi: 10.1176/jnp.11.4.470. [DOI] [PubMed] [Google Scholar]
- Mosconi MW, Cody-Hazlett H, Poe MD, Gerig G, Gimpel-Smith R, Piven J. Longitudinal study of amygdala volume and joint attention in 2- to 4-year-old children with autism. Archives of General Psychiatry. 2009;66(5):509–516. doi: 10.1001/archgenpsychiatry.2009.19. 66/5/509 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nacewicz BM, Dalton KM, Johnstone T, Long MT, McAuliff EM, Oakes TR. Amygdala volume and nonverbal social impairment in adolescent and adult males with autism. Archives of General Psychiatry. 2006;63(12):1417–1428. doi: 10.1001/archpsyc.63.12.1417. 63/12/1417 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oberman LM, Ramachandran VS. The simulating social mind: The role of the mirror neuron system and simulation in the social and communicative deficits of autism spectrum disorders. Psychological Bulletin. 2007;133(2):310–327. doi: 10.1037/0033-2909.133.2.310. [DOI] [PubMed] [Google Scholar]
- Ozonoff S, McEvoy R. A longitudinal study of executive function and theory of mind development in autism. Development and Psychopathology. 1994;6(3):415–431. [Google Scholar]
- Ozonoff S, Pennington BF, Rogers SJ. Executive function deficits in high-functioning autistic individuals: relationship to theory of mind. Journal of Child Psychology and Psychiatry and Allied Disciplines. 1991;32(7):1081–1105. doi: 10.1111/j.1469-7610.1991.tb00351.x. [DOI] [PubMed] [Google Scholar]
- Ozonoff S, Rogers SJ, Pennington BF. Asperger’s Syndrome: Evidence of an empirical distinction from high-functioning autism. Journal of Child Psychology and Psychiatry. 1991;32(7):1107–1122. doi: 10.1111/j.1469-7610.1991.tb00352.x. [DOI] [PubMed] [Google Scholar]
- Pardo CA, Eberhart CG. The neurobiology of autism. Brain Pathology. 2007;17(4):434–447. doi: 10.1111/j.1750-3639.2007.00102.x. BPA102 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peugh JL, Enders CK. Using the SPSS mixed procedure to fit cross-sectional and longitudinal multilevel models. Educational and Psychological Measurement. 2005;65(5):717–741. [Google Scholar]
- Piven J, Arndt S, Bailey J, Havercamp S, Andreasen NC, Palmer P. An MRI study of brain size in autism. The American Journal of Psychiatry. 1995;152(8):1145–1149. doi: 10.1176/ajp.152.8.1145. [DOI] [PubMed] [Google Scholar]
- Piven J, Bailey J, Ranson BJ, Arndt S. An MRI study of the corpus callosum in autism. American Journal of Psychiatry. 1997;154(8):1051–1056. doi: 10.1176/ajp.154.8.1051. [DOI] [PubMed] [Google Scholar]
- Piven J, Harper J, Palmer P, Arndt S. Course of behavioral change in autism: a retrospective study of high-IQ adolescents and adults. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35(4):523–529. doi: 10.1097/00004583-199604000-00019. [DOI] [PubMed] [Google Scholar]
- Redcay E, Courchesne E. When is the brain enlarged in autism? A meta-analysis of all brain size reports. Biological Psychiatry. 2005;58(1):1–9. doi: 10.1016/j.biopsych.2005.03.026. S0006-3223(05)00369-0 [pii] [DOI] [PubMed] [Google Scholar]
- Rosenthal R. Meta-analytic procedures for social research. Vol. 6. Newbury Park, CA: Sage Publications; 1991. [Google Scholar]
- Rutter M. The autistic child. Royal Institute of Public Health and Hygiene Journal. 1967;30(4):130–132. [PubMed] [Google Scholar]
- Rutter M, Le Couteur A, Lord C. Autism Diagnostic Interview-Revised Manual. Los Angeles: Western Psychological Services; 2003. [Google Scholar]
- Schumann CM, Barnes CC, Lord C, Courchesne E. Amygdala enlargement in toddlers with autism related to severity of social and communication impairments. Biological Psychiatry. 2009;66(10):942–949. doi: 10.1016/j.biopsych.2009.07.007. S0006-3223(09)00835-X [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seltzer MM, Krauss MW, Shattuck PT, Orsmond G, Swe A, Lord C. The symptoms of autism spectrum disorders in adolescence and adulthood. Journal of Autism and Developmental Disorders. 2003;33(6):565–581. doi: 10.1023/b:jadd.0000005995.02453.0b. [DOI] [PubMed] [Google Scholar]
- Spencer MD, Moorhead WJ, Lymer KS, Job DE, Muir WJ, Hoare P. Structural correlates of intellectual impairment and autistic features in adolescents. Neuroimage. 2006;33:1136–1144. doi: 10.1016/j.neuroimage.2006.08.011. [DOI] [PubMed] [Google Scholar]
- Spiker D, Lotspeich LJ, Dimiceli S, Myers RM, Risch N. Behavioral phenotypic variation in autism multiplex families: evidence for a continuous severity gradient. American Journal of Medical Genetics. 2002;114(2):129–136. doi: 10.1002/ajmg.10188. [pii] [DOI] [PubMed] [Google Scholar]
- Talairach J, Tournoux P. Co-planar Stereotaxic Atlas of the Human Brain: 3-Dimensional Proportional System - an Approach to Cerebral Imaging. New York: Thieme Medical Publishers; 1988. [Google Scholar]
- Tepest R, Jacobi E, Gawronski A, Krug B, Moller-Hartmann W, Lehnhardt FG. Corpus callosum size in adults with high-functioning autism and the relevance of gender. Psychiatry Research. 2010;183(1):38–43. doi: 10.1016/j.pscychresns.2010.04.007. S0925-4927(10)00120-4 [pii] [DOI] [PubMed] [Google Scholar]
- Vidal CN, Nicolson R, DeVito TJ, Hayashi KM, Geaga JA, Drost DJ. Mapping corpus callosum deficits in autism: An index of aberrant cortical connectivity. Biological Psychiatry. 2006;60:218–225. doi: 10.1016/j.biopsych.2005.11.011. [DOI] [PubMed] [Google Scholar]
- Waiter GD, Williams JH, Murray AD, Gilchrist A, Perrett DI, Whiten A. Structural white matter deficits in high-functioning individuals with autistic spectrum disorder: a voxel-based investigation. Neuroimage. 2005;24(2):455–461. doi: 10.1016/j.neuroimage.2004.08.049. S1053-8119(04)00512-9 [pii] [DOI] [PubMed] [Google Scholar]
- White T, Andreasen NC, Nopoulos P, Magnotta V. Gyrification abnormalities in childhood- and adolescent-onset schizophrenia. Biological Psychiatry. 2003;54(4):418–426. doi: 10.1016/s0006-3223(03)00065-9. S0006322303000659 [pii] [DOI] [PubMed] [Google Scholar]


