Abstract
Introduction:
Psoriasis is a chronic skin ailment which can be connected with an increased occurrence of other illnesses, including high blood pressure.
Examinees and methods:
A prospective study has been conducted which included 70 patients affected by psoriasis, both genders, older than 18 years. Average age being 47,14 (SD= ±15,41) years, from that there were 36 men or 51,43 and 34 women or 48,57%. Average duration of psoriasis was 15,52 (SD=±12,54) years.
Results:
Frequency of high blood pressure in those affected by psoriasis was 54,28%. Average age of the patients with psoriasis and high blood pressure was 53,79 year (SD=±14,15) and average duration of psoriasis was 17,19 years (SD=±13,51). Average values of PASI score were 16,65. Increase in values of PASI score and high blood pressure were statistically highly related (r=0,36, p=0,0001).
Conclusion:
Psoriasis was related to high blood pressure and there was a correlation between the severity of psoriasis and high blood pressure.
Keywords: psoriasis, high blood pressure
1. INTRODUCTION
Psoriasis is a chronic skin disease, which occurs in around 2-3% of population. Even in the past century, a relation between psoriasis and high blood pressure was spotted, so research which was conducted in Sweden and Germany on those affected by psoriasis showed an increased rate of high blood pressure (1, 2). By reviewing literature which enveloped 24 studies in which participated over 300.000 patients suffering from psoriasis, an increased frequency of high blood pressure was detected, and patients with severe psoriasis had higher odds for the appearance of high blood pressure compared to those with mild psoriasis (3). And despite increased occurrence in high blood pressure in those affected by psoriasis, a precise pathophysiological mechanism has not been determined, but it is considered that relation between psoriasis and increased blood pressure can be related with an increased level of angiotensin-converting enzyme, endothelin-1 (ET-1), and rennin in the patient with psoriasis (4, 5). One of the possibilities is that adipose tissue in those affected by psoriasis serves as a main source of angiotensinogen, which is later turned into angiotensin II, and that decrease in body weight leads to lower blood pressure (6). Angiotensin II besides retaining salt in kidneys also stimulates proliferation of T-cells (7). It is considered that endothelin-1 can play an important role in development of high blood pressure in those affected by psoriasis. Endothelin-1 is a protein which leads to constriction of blood vessels and increase in blood pressure, and it is produced by a couple of different kinds of cells, including keratinocytes, and the level of endothelin-1 is in correlation with severity of psoriasis (8). Medication for treating psoriasis can also affect the appearance of high blood pressure, so for example, Cyclosporine can lead to development of high blood pressure (9). We also can’t exclude the influence of stress and way of life on development of high blood pressure in those affected by psoriasis.
2. EXAMINEES AND METHODS
This prospective research was lead between November of 2011 and June of 2013. It enveloped 70 consecutively chosen patients, affected by psoriasis, both genders, over the age of 18. Average age being 47,14 (SD= ±15,41), from that there were 36 men, or 51,43 % and 34 women or 48,57%. Average duration of psoriasis was 15,52 (SD= ±12,54) years.
Research also included patients with documented cases of diagnosed psoriasis, ambulatory or hospital reports from dermatologist (dermatovenerologist), and pathophysiological report, of those who were treated at the clinic for skin diseases of University clinical center Tuzla. Research did not include patients which besides psoriasis suffered from some other skin disease, and those which suffered from psoriasis for less than a year. Research has been approved from the side of ethics committee of University clinical center Tuzla. Firstly, all examinees were explained the purpose of the research, asked for a written consent to participate in the research, taken history, got their skin and visible mucous membranes dermatologically tested and had their PASI score values determined, and they were checked for high blood pressure (based on the findings of internist).
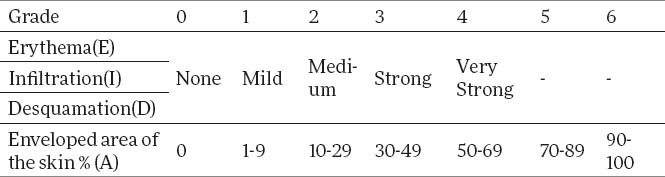
For determining the severity and outspread of psoriasis, Psoriasis Area and Severity Index (PASI) was used. In four regions body-head, torso, upper and lower extremities. In the four regions of the body-head, torso, upper and lower extremities evaluated the characteristics of the disease, severity of erythema, infiltration and desquamation with the score 1-4, and the affected area of skin psoriatic changes with the score 1-6 (Table 1). In assessing the severity of erythema scales may not be removed. Theoretically PASI can range from 0-72 (10).
Table 1.
Measurement of PASI
By this method we calculate :
Buttocks as a part of lower extremities, that is, region of the leg (l);
Armpits and shoulders as a part of upper extremities, that is, region of the arm (a);
The neck is calculated as a part of the head (h);
Torso (t).
For calculating the PASI, the summation of Erythemas, infiltrations and desquamations of single region is multiplied with the numerical value of the region of the body and with the percentage by which the lesions have spread at a single region. Results obtained for each single region are calculated in PASI.
Form for calculating PASI:
PASI=0,1×(Eh+Ih+Dh)×Ah+0,3×(Et+It+Dt)×At+0,2×(Ea+Ia+Da)×Aa+0,4×(El+Il+Dl)×Al
Legend: E- Erythema, I–Infiltration, D – Desqumation, A – Area, h–head, t–torso, a–arm, l–leg
Statistical analysis
For data processing and hypothesis testing was used statistical package Arcus Quickstat Biomedical Version 1.0. Statistical series are described measures of central tendency and variability measures. The relationship between variables was estimated correlation test. As the minimum value of the level of significance was taken as p <0.05.
3. RESULTS
Frequency of high blood pressure in those affected by psoriasis was 54,28%. Average age of patients with high blood pressure was 53,79 years (SD=±13,51).
Clinical characteristics of the affected were estimated based on the Psoriasis Area Severity Index – PASI. Average values of PASI score were 16,65.
Increase in values of PASI score and high blood pressure was statistically highly connected (Figure 1).
Figure 1.
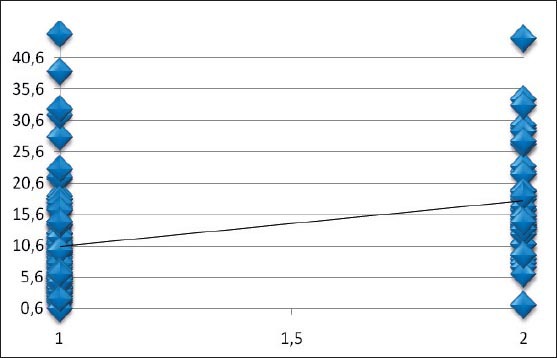
Relation between values of PASI score and high blood pressure (r=0,36; p=0,0001).
4. DISCUSSION
In this research, high blood pressure was recorded in 54,28 % of examinees. Results were similar to other studies which also showed an increased occurrence of high blood pressure, that is, highly increased risk of development of high blood pressure in those affected by psoriasis. Rosa et al. (11), found elevated blood pressure in 59,2% of patients with psoriasis. In research on patients affected by psoriasis which was lead in Germany, frequency of blood pressure was 39,1% (12). In research Sommer et al. (13), patients affected by psoriasis had 3 times higher frequency high blood pressure compared to the control group. In research Ghiasi et al. (14), it was shown that patients affected by psoriasis have 2,2 times higher risk for development of blood pressure compared to the control group.
Average age of the examinees affected by psoriasis with high blood pressure was 53,79 (SD=±14,15), they were somewhat older than average age of examinees, which was 47,14 years. (SD=±15,41). Altobelli et al. (15) found that those suffering from psoriasis had an increased risk for development of high blood pressure after 40 years, and that risk grew with age. Average duration of psoriasis in examinees suffering from psoriasis with increased blood pressure was 17,19 years (SD=±13,51) and it was somewhat longer than average duration of psoriasis on all examinees, which was 15,52 years (SD=±12,54). In research conducted in Malaysia which examined the frequency of comorbidity in those affected by psoriasis, frequency of high blood pressure in patients affected by psoriasis was 25,9% and more frequent if psoriasis lasted longer and developed later (16).
In this research, a link between severity of psoriasis and high blood pressure was found, there was a positive correlation between PASI and high blood pressure (r=0,36 p=0,0001). In research conducted in Middle East, severity of psoriasis had an effect on frequency of increased blood pressure, so frequency of blood pressure in mild and medium psoriasis (PASI<10) was 32% and in severe cases of psoriasis (PASI>10) it was 40,3%, and in control group it was 11,55% (17). In Great Britain, the frequency between high blood pressure and psoriasis was examined, and in severe forms of psoriasis it was 20%, in mild forms it was 14,7%, and control group’s scores ranged at 11,9% (18). Connection between psoriasis and high blood pressure and correlation between severity of psoriasis and high blood pressure was confirmed.
5. CONCLUSION
Psoriasis is related with high blood pressure, but further research is necessary in purpose of investigating mechanisms of connection between psoriasis and high blood pressure, in goals of prevention, screening and treatment of high blood pressure in those affected by psoriasis.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Lindegard B. Diseases associated with psoriasis in a general population of 159,200 middle-aged, urban, native Swedes. Dermatologica. 1986;172:298–304. doi: 10.1159/000249365. [DOI] [PubMed] [Google Scholar]
- 2.Henseler T, Christophers E. Disease concomitance in psoriasis. J Am Acad Dermatol. 1995;32(6):982–986. doi: 10.1016/0190-9622(95)91336-x. [DOI] [PubMed] [Google Scholar]
- 3.Armstrong AW, Harskamp CT, Armstrong EJ. The association between psoriasis and hypertension: a systematic review and meta-analysis of observational studies. J Hypertens. 2013;31(3):433–442. doi: 10.1097/HJH.0b013e32835bcce1. [DOI] [PubMed] [Google Scholar]
- 4.Ena P, Madeddu P, Glorioso N, Cerimele D, Rappelli A. High prevalence of cardiovascular diseases and enhanced activity of the renin-angiotensin system in psoriatic patients. Acta Cardiol. 1985;40(2):199–205. [PubMed] [Google Scholar]
- 5.Das UN. Is angiotensin-II an endogenous pro-inflammatory molecule? Med Sci Monit. 2005;11(5):RA155–162. [PubMed] [Google Scholar]
- 6.Engeli S, Böhnke J, Gorzelniak K, Janke J, Schling P, Bader M, et al. Weight loss and the renin-angiotensin-aldosterone system. Hypertension. 2005;45(3):356–362. doi: 10.1161/01.HYP.0000154361.47683.d3. [DOI] [PubMed] [Google Scholar]
- 7.Nataraj C, Oliverio MI, Mannon RB, Mannon PJ, Audoly LP, Amuchastegui CS, et al. Angiotensin II regulates cellular immune responses through a calcineurin-dependent pathway. J Clin Invest. 1999;104(12):1693–1701. doi: 10.1172/JCI7451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bonifati C, Mussi A, Carducci M, Pittarello A, D’Auria L, Venuti A, et al. Endothelin-1 levels are increased in sera and lesional skin extracts of psoriatic patients and correlate with disease severity. Acta Derm Venereol. 1998;78(1):22–26. doi: 10.1080/00015559850135779. [DOI] [PubMed] [Google Scholar]
- 9.Taler SJ, Textor SC, Canzanello VJ, Schwartz L. Cyclosporin-induced hypertension: incidence, pathogenesis and management. Drug Saf. 1999;20(5):437–449. doi: 10.2165/00002018-199920050-00004. [DOI] [PubMed] [Google Scholar]
- 10.Fredriksson T, Pettersson U. Severe psoriasis-oral therapy with new retinoid. Dermatologica. 1978;157:238–244. doi: 10.1159/000250839. [DOI] [PubMed] [Google Scholar]
- 11.Rosa DJ, Machado RF, Matias FA, Cedrim SD, Noronha FL, Gaburri D, et al. Influence of severity of the cutaneous manifestations and age on the prevalence of several cardiovascular risk factors in patients with psoriasis. Eur Acad Dermatol Venereol. 2012;26(3):348–353. doi: 10.1111/j.1468-3083.2011.04076.x. [DOI] [PubMed] [Google Scholar]
- 12.Jacobi A, Kupke C, Behzad M, Hertl M. Comorbidities, metabolic risk profile and health-related quality of life in German patients with plaque-type psoriasis: a cross-sectional prospective study. Int J Dermatol. 2013;52(9):1081–1087. doi: 10.1111/j.1365-4632.2012.05517.x. [DOI] [PubMed] [Google Scholar]
- 13.Sommer DM, Jenisch S, Suchan M, Christophers E, Weichenthal M. Increased prevalence of the metabolic syndrome in patients with moderate to severe psoriasis. Archives of Dermatological Research. 2006;298(7):321–328. doi: 10.1007/s00403-006-0703-z. [DOI] [PubMed] [Google Scholar]
- 14.Ghiasi M, Nouri M, Abbasi A, Hatami P, Abbasi MA, Nourijelyani K. Psoriasis and increased prevalence of hypertension and diabetes mellitus. Indian J Dermatol. 2011;56(5):533–536. doi: 10.4103/0019-5154.87149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Altobelli E, Petrocelli R, Maccarone M. Risk factors of hypertension, diabetes and obesity in Italian psoriasis patients: a survey on socio-demographic characteristics, smoking habits and alcohol consumption. Eur J Dermatol. 2009;19(3):252–256. doi: 10.1684/ejd.2009.0644. [DOI] [PubMed] [Google Scholar]
- 16.Mazlin MB, Chang CC, Baba R. Comorbidities associated with psoriasis–data from the malaysian psoriasis registry. Med J Malaysia. 2012;67(5):518–521. [PubMed] [Google Scholar]
- 17.Al-Mutairi N, Al-Farag S, Al-Mutairi A, Al-Shiltawy M. Comorbidities associated with psoriasis: an experience from the Middle East. J Dermatol. 2010;37(2):146–155. doi: 10.1111/j.1346-8138.2009.00777.x. [DOI] [PubMed] [Google Scholar]
- 18.Neimann AL, Shin DB, Wang X, Margolis DJ, Troxel AB, Gelfand JM. Prevalence of cardiovascular risk factors in patients with psoriasis. J Am Acad Dermatol. 2006;55(5):829–835. doi: 10.1016/j.jaad.2006.08.040. [DOI] [PubMed] [Google Scholar]


