Abstract
Introduction:
Burnout can create problems in every aspect of individual’s’ human life. It may have an adverse effect on interpersonal and family relations and can lead to a general negative attitude towards life.
Aim:
The purpose of this study is to investigate whether burnout is associated with the mental health status of health care providers.
Material and Methods:
The sample in this study consisted of 240 health care employees. The Greek version of Maslach’s Burnout Inventory (MBI) was used for measuring burnout levels and the Greek version of the Symptoms Rating Scale for Depression and Anxiety (SRSDA) questionnaire was used to evaluate health care providers’ mental health status. Descriptive statistics were initially generated for sample characteristics. Normality was checked by the Kolmogorov-Smirnov test and data was processed with parametric tests. General linear models with MBI dimensions as independent variables and SRSDA subscales as dependent variables were used to determine the relation between burnout and mental health status. Statistics were processed with SPSS v. 17.0 (SPSS, Chicago, IL, USA). Statistical significance was set at p=0.05.
Results:
The average age of the sample is 40.00±7.95 years. Regarding gender the percentage of men is 21.40% (N=49) and of women is 78.60% (N=180). Overall the professional burnout of health care workers is moderate. The mean score for emotional exhaustion is 26.41, for personal accomplishment 36.70 and for depersonalization 9.81. The mean for each subscale of SRSDA is 8.23±6.79 for Depression Beck-21, 3.96±4.26 for Depression Beck-13, 4.91±4.44 for Melancholia, 6.32±4.35 for Asthenia and 6.36±4.72 for Anxiety. The results of general linear models with the MBI dimensions as independent variables and the SRSDA subscales as dependent variables are shown that emotional exhaustion and personal accomplishment are statistically correlated with all subscales of SRSDA, while depersonalization is not correlated with any SRSDA subscale.
Conclusions:
Burnout appears to implicate mental health status of healthcare providers in work index. Emotional exhaustion is the burnout dimension that is correlated the most with employees’ mental health.
Keywords: Burnout, mental health status, health care workers, depression
1. INTRODUCTION
Burnout is defined as a syndrome, which is caused mainly by stress, especially among occupations with humanitarian and social contribution (1). The research about burnout is largely guided by the work of Maslach and Jackson who conceptualized burnout as a syndrome of three dimensions; the dimension of emotional exhaustion, the dimension of depersonalization and the dimension of personal achievement (1). In literature review, many studies that support the three-dimensional perception of burnout can be found (2-9).
About the measurement of burnout, there is a unanimity among most researchers in favor of MBI (10), although some researchers have attempted to use other measuring tools, either for comparison (11, 12) or because of their suitability for the research objective, the sample or the research content (13, 14).
Symptoms of burnout as already mentioned are the spiritual and emotional exhaustion, the depersonalization and the decreased sense of personal achievement. Moreover, distress symptoms such as fatigue, physical and mental, and feelings of depression, regarded as the most characteristic symptoms of burnout (15,16).
Researchers have demonstrated that the core of burnout is the reduction of energetic resources of the workers, and this is distinct in content of depression and anxiety (6, 17).
Depressive symptomatology is complex and includes the lack of pleasurable experiences, accompanied by feelings of anger, guilt, anxiety and symptoms of physical fatigue, data that do not distinguish the professional burnout (18).
The most recent phases of burnout may be accompanied by depressive symptomatology. Studies often reported high positive correlation between burnout and depression (19-21).
According to Brenninkmeyer et al, individuals with high levels of burnout compared with depressed people, are: (1) more alive in their behavior and seem to enjoy things and situations, although deprived of required energy, (2) rarely lose weight or rarely have thoughts of suicide, (3) have more realistic feelings of guilt when they feel them, (4) tend to perform, unlike depressed people, their indecision and inaction in their fatigue despite their illnesses, and (5) often have difficulties in sleeping, while depressed people tend to wake up too early (22).
Burnout can also create problems in every aspect of individual’s’ human life. It may have an adverse effect on interpersonal and family relations and can lead to a general negative attitude towards life. From this aspect, burnout is expected to have common features with depression (23, 24).
Various studies are focused on assessing the direction of the relation between depression and burnout. The question is whether depression can be considered as a result of burnout or the opposite. In a study, conducted by Glass et al, in nurses was found that under certain conditions burnout can develop into depression (25). However, Glass and McKnight found that burnout and depression associated bidirectional, i.e. that depression can cause burnout and vice versa (17). Burnout can be seen as an issue related to the work environment, while depression is more comprehensive as a concept and does not have specific connectivity with the working environment (26). But, Iacovides et al, found that nurses who suffer from burnout syndrome did not exhibit depressive symptoms (27).
Within this context of reasoning that trying to distinguish depression from burnout, raises the question for how depression and burnout can be identified in a mental model. Trying to find a clinical concept in a meaningful social-psychological framework seems to be quite difficult. Furthermore, the nature of the relation between burnout and depression is not yet clarified theoretically. Some questions such as whether burnout leads to depression or vice versa, or if both have some common and some unique causes, have been the focus of several studies.
2. AIM
The purpose of this study is to investigate whether burnout is associated with the mental health status of health care providers. The research questions were:
What is the level of burnout among health care providers?
What is the mental health status among health care providers?
Is there a correlation between burnout and mental health status? Which dimension of burnout is correlated the most with mental health status?
3. MATERIAL AND METHODS
Sample and Sampling
The sample in this study consisted of 240 health care employees who were randomly selected from health care units of all over Greece. Local ethical committees approved the study protocol. Doctors, nurses and other healthcare workers (midwives, social workers) participated in the study. The response rate was 80.00% (240 out of 300 questionnaires), with 76.33% of the questionnaires (229 out of 300) completed without any missing data in the psychometric section and thus suitable for final evaluation.
Demographic Data
For measuring the demographic data of the sample questions about gender, age, marital status, number of children, higher degree, profession, years in profession and years in department were used.
Burnout Measuring
The Greek version of Maslach’s Burnout Inventory (MBI) was used for measuring burnout levels [28]. MBI is a seven point Likert scale of 22 items (0: never happens to me, 6: it happens to me every day). The 22 questions are consisted in three dimensions of burnout; emotional exhaustion, personal accomplishment and depersonalization. Questions 5, 10, 11, 15, 22 refer to depersonalization, 4, 7 9, 12, 17, 18, 19, 21 refer to personal accomplishment and the rest refer to depersonalization. To discriminate between the levels of each dimension of burnout, scores that provided by the Greek version of MBI were used, referring to burnout dimensions in health care professionals in Greece, classifying burnout in low, moderate and high category (28).
Mental Health Status Measuring
The Greek version of the Symptoms Rating Scale for Depression and Anxiety (SRSDA) questionnaire was used to evaluate health care providers’ mental health status [29]. SRSDA includes 42 items and contains six subscales; the 21-item Beck Depression Subscale, the 13-item Beck Depression Subscale, the Melancholia Subscale, the Asthenia Subscale, the Anxiety Subscale and the Mania Subscale.
The composition of the SRSDA subscales is as follows:
The 21- item Beck Depression Subscale (BDI-21) includes items 1, 8, 11, 13, 14, 17, 18, 19, 20, 21, 22, 23, 25, 26, 27, 28, 29, 31, 32, 34 and 41. These are scored as: a=0, b=1, c=2, d=3.
The 13- item Beck Depression Subscale (BDI-13) includes items 1, 8, 11, 13, 14, 19, 20, 22, 28, 29, 32, 34 and 41. These are scored as: a=0, b=1, c=2, d=3.
The 12-item Melancholia Subscale includes items 8, 11, 13, 17, 19, 20, 21, 22, 26, 29, 32, and 34. These are scored as: a=0, b=1, c=2, d=3.
The 12-item Asthenia Subscale includes items 2, 5, 9, 17, 21, 24, 25, 27, 28, 29, 32 and 38. These are scored as: a=0, b=1, c=2, d=3.
The 14-item Anxiety Subscale includes items 3, 4, 5, 12, 15, 17, 21, 24, 25, 27, 33, 39, 40 and 42. These are scored as: a=0, b=1, c=2, d=3.
The 5-item Mania Subscale includes items 6, 10, 16, 30, 37. These are scored as: a= -1, b=0, c=0, d= +1.
The optimal cut-off points established for the Greek population in each subscale are as follows: BDI-21:14/15, BDI-13:7/8, Melancholia:8/9, Asthenia:9/10, Anxiety:10/11. Regarding the results from the Greek version of SRSDA the cut-off point for the mania was not taken under consideration due to the statistical criteria.
Statistics
Descriptive statistics were initially generated for sample characteristics. Normality was checked by the Kolmogorov-Smirnov test. The results on the dimension of MBI and on the subscales of SRSDA were mixed. Some subscales exhibited marginally normal distributions (emotional exhaustion, personal accomplishment, asthenia, melancholia, anxiety) while others were clearly not normally distributed (depersonalization, Beck-21, Beck-13, mania). As there are articles in the literature arguing that parametric tests can successfully be applied to non-normally distributed data [30,31], data was processed with parametric tests. Chronbach’s α ranged between 0.81 and 0.90 for individual MBI and SRSDA scales. More specifically: emotional exhaustion: 0.87, personal accomplishment: 0.84, depersonalization: 0.81, BDI-21: 0.89, BDI-13: 0.90, melancholia: 0.89, asthenia: 0.87, anxiety: 0.88 and mania: 0.10. As the mania scale exhibited the lowest reliability, well below 0.60, it was excluded from the study. The classification of the Greek version of MBI was used for the burnout scores of the sample in order to find out if the levels of burnout are low, moderate or high. The cut-off points of the Greek version of SRSDA were used to determine the mental health status of the sample. General linear models with MBI dimensions as independent variables and SRSDA subscales as dependent variables were used to determine the relation between burnout and mental health status. Statistics were processed with SPSS v. 17.0 (SPSS, Chicago, IL, USA). Statistical significance was set at p=0.05.
4. RESULTS
Demographic Data
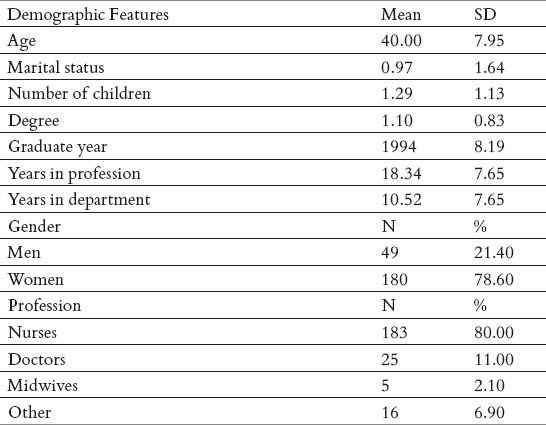
Demographic and job features are presented in Table 1. The average age of the sample is 40.00±7.95 years. Regarding gender the percentage of men is 21.40% (N=49) and of women is 78.60% (N=180). As for marital status, 64.40% declared married (mean score= 0.97, 0=single, 1=married, 2=divorced) and 33.80% of the married declared that they do not have children. The 74% of the sample members has graduated from higher education (universities and technological educational institutes) and as for the profession 80.00% are nurses 11.00% doctors 2.10% midwives and 6.90% other specialties. The mean score of years in profession for the sample is 18.34± 7.65 and for years in department is 10.52 ±7.65.
Table 1.
Descriptive Statistical Results for the Demographic Features of the Sample
Burnout Levels
The mean scores and the percentages of burnout levels are shown in Table 2 and are compared with the mean scores for each dimension that have been provided by the Greek version of MBI [28].
Table 2.
Mean Sample Scores and Percentages for Low, Moderate and High Levels of Burnout Dimensions
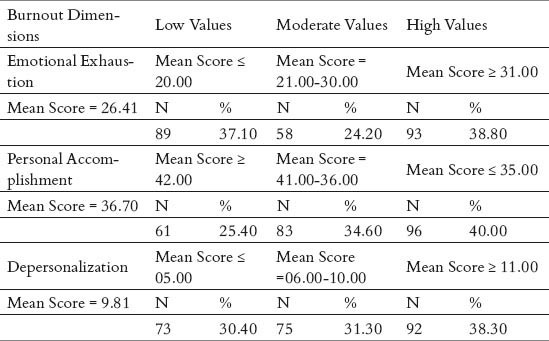
Overall the professional burnout of health care workers is moderate. The mean score for emotional exhaustion is 26.41 (moderate=21.00-30.00), for personal accomplishment 36.70 (moderate=41.00-36.00) and for depersonalization 9.81 (moderate=6.00-10.00). But the means for personal accomplishment and depersonalization are very close to high levels (high level of personal accomplishments ≤ 35.00, high levels of depersonalization ≥ 11.00).
Regarding the percentages of the sample, the 38.80% (N=93) is presenting high levels of emotional exhaustion, 40.00% (N=96) is presenting high levels of personal accomplishment and 38.30% (N=92) is presenting high levels of depersonalization.
Mental Health Status Results
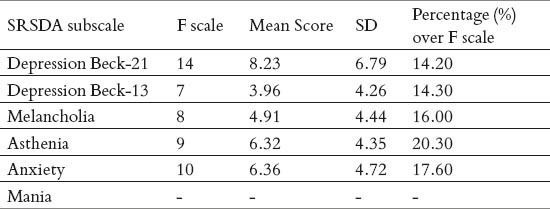
The descriptive statistical results for SRSDA are presented in Tables 3 and 4. In Table 3 are presented the results for each question of SRSDA and in Table 4 the results for each subscale of SRSDA. The mean for each subscale of SRSDA is 8.23±6.79 for Depression Beck-21, 3.96±4.26 for Depression Beck-13, 4.91±4.44 for Melancholia, 6.32±4.35 for Asthenia and 6.36±4.72 for Anxiety. The cutoff points of the Greek version of SRSDA are presented as an F scale in Table 4. According to the mean scores of the subscales and the F scale, most of the health care workers do not appear mental health disorders. The percentages of sample members with a possible psychiatric disorder (scores over cutoff points) are 20.30% for Asthenia, 17.60% for Anxiety, 16.00% for Melancholia, 14.30% for Depression Beck-13 and 14.20% for Depression Beck-21.
Table 3.
Descriptive Statistical Results for each question of SRSDA
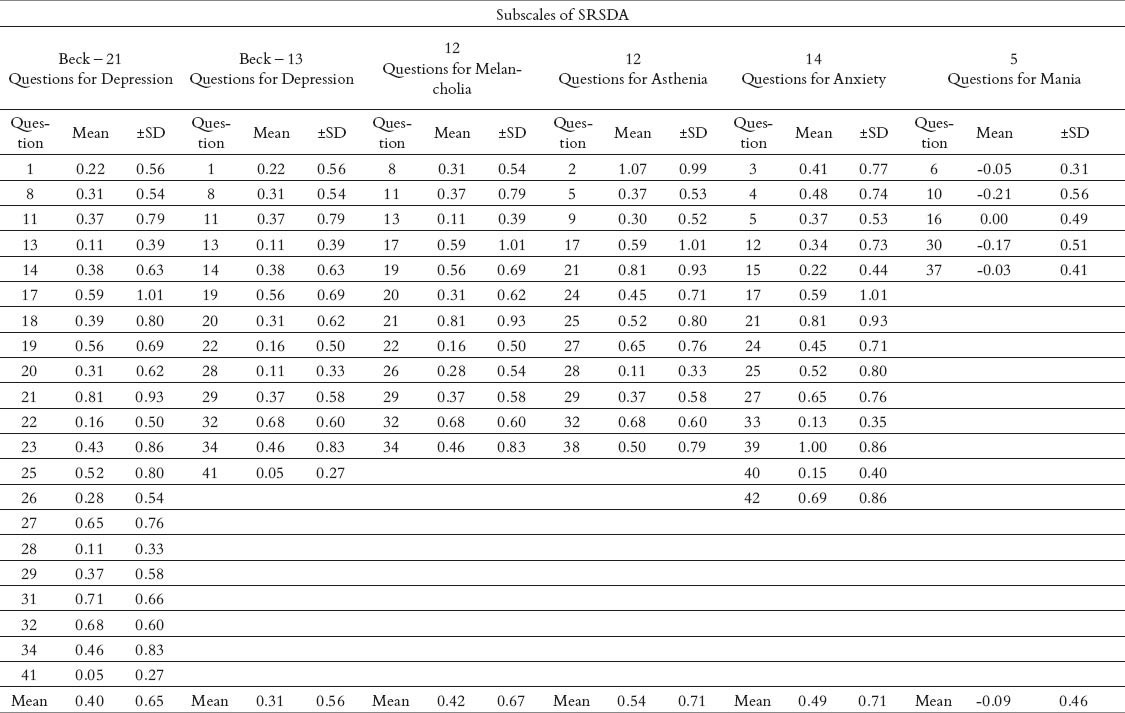
Table 4.
Descriptive Statistical Results for each Subscale of SRSDA
Implications of Burnout on Mental Health Status
The results of general linear models with the MBI dimensions as independent variables and the SRSDA subscales as dependent variables are shown in Table 5. Emotional exhaustion and personal accomplishment are statistically correlated with all subscales of SRSDA, while depersonalization is not correlated with any SRSDA subscale.
Table 5.
General linear regression with Burnout Dimensions as independent variables and SRSDA Subscales as dependent variables
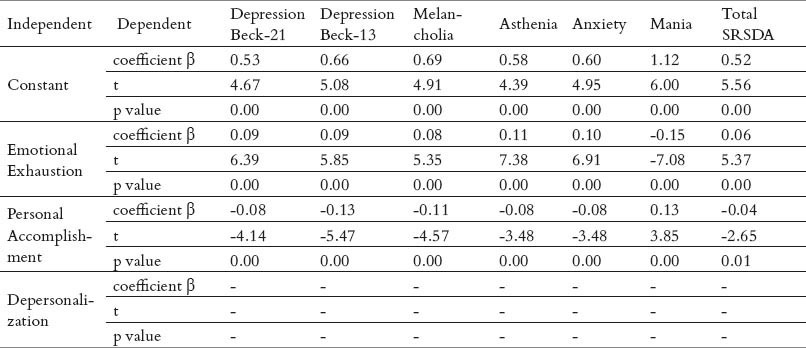
The positive scores of coefficient β for emotional exhaustion show that, higher levels of emotional exhaustion implicate higher levels of depression (β=0.09, p=0.00), melancholia (β=0.08, p=0.00), asthenia (β=0.11, p=0.00) and anxiety (β=0.10, p=0.00). The negative score of coefficient β in linear regression model between emotional exhaustion and mania (β= -0.15, p=0.00), means that higher levels of emotional exhaustion implicate lower levels of mania. The interpretation of this result can be done according to psychiatric symptomatology of mania, which includes increased and irritable mood and exuberant self esteem, totally different from exhaustion.
The results are totally the opposites for personal accomplishment. Personal accomplishment are negatively correlated with depression (β= -0.08, p=0.00), melancholia (β= -0.11, p=0.00), asthenia (β= -0.08, p=0.00), and anxiety (β= -0.08, p=0.00) and positively correlated with mania (β=0.13, p=0.00).
According to the values of coefficient β and the p-values, emotional exhaustion is correlated the most with the total SRSDA (β=0.06, p=0.00), meaning that it has more implications in mental health status of health care providers.
5. DISCUSSION
This study aims to analyze the relation between burnout and mental health status among health care providers. At the begging levels of burnout and mental health status were investigated. The results about burnout showed that the levels of the three burnout dimensions are moderate. But, the 38.80% of the sample is experiencing high levels of emotional exhaustion, 40.00% is experiencing high levels of personal accomplishment and 38.30% is experiencing high levels of depersonalization.
According to mental health status the levels are also moderate; but the 20.30% of the sample is experiencing high levels of asthenia, 17.60% is experiencing high levels of anxiety, 16.00% is experiencing high levels of melancholia and 14.30% is experiencing high levels of depression.
Finally the results from regression analysis, showed that two of the burnout dimensions, emotional exhaustion and personal accomplishment, are statistically correlated – positively or negatively- with levels of depression, melancholia, asthenia, anxiety and mania across health care employees in Greek working settings.
Anxiety and depression are referred in the literature as indicators of mental health status (32-34). Maslach is mentioned that researches have shown that burnout is related with neuroticism, which includes the trait of anxiety and depression (35). Turnipseed, by using measurement scales for anxiety as a state and as a trait condition, in order to predict the dimensions of MBI, concluded that anxiety levels contribute significantly to burnout and emotional exhaustion in particular (36). This research is shown that the opposite is also occurs.
The influence of mental health factors in the presence of people at their work and in their absenteeism, the conduct addressing of labor conditions, the psychosomatic illnesses and the job performance, are also important components burnout (37-41). Recent published research studies are focused on depression in working environments (42-46). Depression was defined as a set of negative feelings, suicidal thoughts, emotional fatigue and social withdrawal (18). The work considered depression has been investigated under occupational burnout (47, 48). The studies about depression in the employment context, were guided by theories for stress and burnout (33, 49, 50). Although it is difficult to draw firm conclusions from the rather limited evidence of research, it appears that the examination of depression in the context of labor enriches the understanding of the relationship between work and mental health.
For the measurement of depression, studies were mostly based on using the Beck depression scale, which demonstrates good psychometric properties for a wide range of population (51-54). Other measurements have included the depression subscale of GHQ- 12 (55-58).
Although today the concept of burnout is determined in a sufficiently clear manner, there seems to be some kind of confusion about the difference between burnout and depression. The reason for this confusion lies in the fact that depression and burnout are having common features (35). There are theoretical arguments that have been supported by empirical studies, which suggest that, the concepts of depression and burnout are substantially similar (59). As conditions, burnout and depressive symptoms usually refer to mood states. The symptoms of depression include feelings of sadness, mental vacuum, hopelessness, feelings of distress, poor physical and mental energy, that respectively leading to mental and physical exhaustion. That last element of depressive symptomatology, the exhaustion, was the main point for assessing burnout and depression as overlapping states (60, 61).
Some researchers promoted the concept of “professional depression” as a more comprehensive concept, which includes common elements of depression and burnout (60). Recognizing the similarities between the two concepts, Leiter and Durup highlighted the fundamental differences between them (18). They maintained that while burnout is a social construct, depression has a clinical nature that reflects personal thoughts and feelings. In this context, they presented empirical evidence demonstrating the validity of the distinction between burnout and depression (18).
In many studies, as in this study, their levels are highly related (62, 63). Burnout can be used as a predictor to depressive symptoms in work life (20, 59, 64). Glass and McKnight researched the relation and distinction between burnout and depression by conducting a systematic literature review of 18 studies (17). The total number of participants in these studies exceeded 4800. In most studies, burnout was measured with the MBI scale, while various scales were used to measure depression. The conclusion of the review was that depression and burnout are not the same, and emotional exhaustion is presented to correlate positively with depression (17). In addition, depressive symptomatology is regarded as one of the components of the five major factors that shape the neurotic personality, which has been shown to be closely related to burnout (65).
Iacovides et al, in an attempt to approach the relation between the concepts of burnout, depression and work stress, are giving a host of empirical studies whose findings show that burnout and depression are two different disease entities (24). High levels of psychological demands, low levels of participation in decision making, low levels of social support and high psychological stress due to improper working conditions are important predictors of depression (24).
Remarkable is the study of Glass and McNight, which propose that burnout and depressive effects may have common ground and that the difference between them may be due to the simultaneous evolution (17).
The direction of the relation that may exist between depression and other mental disorders with burnout is a point that has preoccupied many researchers and deserves further study. There is a belief that in the future these issues will be at the focus of many empirical studies (17, 25, 35).
Much attention has been given to improving work environments for health care providers (5). Pressure of overload working, demanding patients, life-long learning for knowledge and risk of treatments is related with mental problems (4). Studies have shown that the increase prevalence of mental health problems among health providers is most likely caused by occupational stress, burnout and individual factors. The results of this study highlight the implications of burnout in mental health status of healthcare providers in work context.
In terms of the prevention of mental and psychological disorders, interventions for straiten stress and burnout in the workplace, have been focused on changing job conditions (2). Reforms in health care systems are expected to inevitably deteriorate the mental health problems of health professionals.
6. CONCLUSION
Burnout appears to implicate mental health status of healthcare providers in work index. Emotional exhaustion is the burnout dimension that is correlated the most with employees’ mental health. Further studies about factors that are affecting burnout levels and mental health status would be very helpful and a starting point for changes in health care setting in Greece.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Maslach C, Jackson SE. The measurement of experienced burnout. Journal of Occupational Behavior. 1981;2:99–113. [Google Scholar]
- 2.Fradelos E, Mpelegrinos S, Mparo S, Vassilopoulou Ch, Argyriou P, Tsironi M, Zyga S, Theofilou P. Burnout syndrome impacts on quality of life in nursing professionals: The contribution of perceived social support. Prog Health Sci. 2014;4(1):102–109. doi: 10.4081/hpr.2014.984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Byrne BM. The Maslach Burnout Inventory: Testing for factorial validity and invariance across elementary, intermediate and secondary teachers. Journal of Occupational and organizational Psychology. 1993;66:197–212. [Google Scholar]
- 4.Cordes CL, Dougherty TW. A review and integration of research on job burnout. Academy of Management Review. 1993;18:621–656. [Google Scholar]
- 5.Bakker AB, Schaufeli WB. Burnout contagion processes among teachers. Journal of Applied Social Psychology. 2000;30:2289–2308. [Google Scholar]
- 6.Schaufeli WB, Buunk BP. Burnout: An overview of 25 years of research and theorizing. In: Schabracq MJ, Winnubst JAM, Cooper CC, editors. Handbook of work and health psychology. 2nd ed. West Sussex, U.K: Wiley; 2003. pp. 383–429. [Google Scholar]
- 7.Kulkarni GK. Burnout. Indian Journal of Occupational & Enviromental Medicine. 2006;10:3–4. [Google Scholar]
- 8.Mor ME, Nissly JA, Levin A. Antecedents to Retention and turnover among child welfare, social work, and other human service employees: What can we learn from past research? A review and metanalysis. Social Service Review. 2001;75(4):625–661. [Google Scholar]
- 9.Kee AJ, Don Johnson, Portia H. Burnout and Social Support in Rural Mental Health Counselors. Journal of Rural Community Psychology. 2002;E5:1. www.marshall.edu./jrcp/sp2002Contents.htm . [Google Scholar]
- 10.Buchan J. What difference does (“good”) HRM make? Human Resources for Health. 2004:2–6. doi: 10.1186/1478-4491-2-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Burke RJ, Greenglass ER. A longitudinal study of progressive phases of psychological burnout. Journal of Health and Human Resources Administration. 1991;13:390–408. [Google Scholar]
- 12.Jones-Schenk J. How magnets attract nurses. Nurs Manage. 2001;32(1):40–42. doi: 10.1097/00006247-200101000-00017. [DOI] [PubMed] [Google Scholar]
- 13.Hochwälder J, Brucefors AB. Psychological empowerment at the workplace as a predictor of ill health. Personality and Individual Differences. 2005;39(7):1237–1248. [Google Scholar]
- 14.Jeanneau M, Armelius K. Self-Image and burnout in psychiatric staff. Journal of Psychiatric and Mental Health Nursing. 2000;7:399–406. doi: 10.1046/j.1365-2850.2000.00321.x. [DOI] [PubMed] [Google Scholar]
- 15.Cherniss C. New York: Praeger; 1980. Professional Burnout in Human Service Organizations. [Google Scholar]
- 16.Kristoff AL. Person-Organization Fit: An Integrative Review of its Conceptualizations. Measurement and Implications, Personnel. 1996;49:1–49. [Google Scholar]
- 17.Glass DC, Mc Knight JD. Perceived control, depressive symptomatology, and professional burnout: A review of the evidence. Psychology and Health. 1996;11:23–48. [Google Scholar]
- 18.Leiter MP, Durum J. The discriminant validity of burnout and depression: A confirmatory factor analytic study. Anxiety, Stress, and Coping. 1994;7:357–373. [Google Scholar]
- 19.Bluen SD, Barling J, Burns W. Predicting sales performance, job satisfaction, and depression by using the achievement strivings and impatience-irritability dimensions of Type-A Behavior. Journal of Applied Psychology. 1990;75(2):212–216. [Google Scholar]
- 20.Firth H, Mc Keown P, Mc Intee J, et al. Professional depression, “burnout” and personality in longstay nursing. International Journal of Nursing Studies. 1987;24:227–237. doi: 10.1016/0020-7489(87)90005-8. [DOI] [PubMed] [Google Scholar]
- 21.Golembiewski RT, Boss W. Phases of burnout in diagnosis and intervention. Research in Organizational Change and Development. 1992;6:115–152. [Google Scholar]
- 22.Brenninkmeyer V, Van Yperen NW, Buunk BP. Burnout and depression are not identical twins: is decline of superiority a distinguishing feature? Personality and Individual Differences. 2001;30(5):873–880. [Google Scholar]
- 23.Ganster DC, Schaubroeck J. Work stress and employee health. Journal of Management. 1991;17(2):235–271. [Google Scholar]
- 24.Iacovides A, Fountoulakis KN, Kaprinis St, et al. The relationship between job stress, burnout and clinical depression. Journal of Affective Disorders. 2003;75:209–221. doi: 10.1016/s0165-0327(02)00101-5. [DOI] [PubMed] [Google Scholar]
- 25.Glass DC, Mc Knight JD, Valdimarsdottir H. Depression, burnout, and perceptions of control in hospital nurses. Journal of Consulting and Clinical Psychology. 1993;61(1):147–155. doi: 10.1037//0022-006x.61.1.147. [DOI] [PubMed] [Google Scholar]
- 26.Demerouti E, Bakker AB, Nachreiner F, Schaufeli WB. The job demands-resources model of burnout. Journal of Applied psychology. 2001;86(3):499. [PubMed] [Google Scholar]
- 27.Iacovides A, Fountoulakis KN, Moysidou C, et al. Burnout in nursing Staff: Is there a relationship between depression and burnout? INTL. Journal of Psychiatry in Medicine. 1999;29:421–433. doi: 10.2190/5YHH-4CVF-99M4-MJ28. [DOI] [PubMed] [Google Scholar]
- 28.Anagnostopoulos F, Papadatou D. Reliability and validity of the Maslach burnout inventory to a population of nurses. Journal of Psychological Issues. 1992;5:183–202. Published in Greek. [Google Scholar]
- 29.Fountoulakis KN, Iacovides A, Kleanthous S, Samolis S, Gougoulias K, Kaprinis G, Bech P. The Greek translation of the symptoms rating scale for depression and anxiety: preliminary results of the validation study. BMC Psychiatry. 2003;10:21. doi: 10.1186/1471-244X-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vickers AJ. Parametric versus non-parametric statistics in the analysis of randomized trials with non-normally distributed data. BMC Med Res Methodol. 2005;5:35. doi: 10.1186/1471-2288-5-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zimmerman DW. Statistical significance levels of nonparametric tests biased by heterogeneous variances of treatment groups. J Gen Psychol. 2000;127:354–364. doi: 10.1080/00221300009598589. [DOI] [PubMed] [Google Scholar]
- 32.Zohar D. The justice perspective of job stress. Journal of Organizational Behavior. 1995;16:487–495. [Google Scholar]
- 33.Roskies E, Louis-Guerin C, Fournier C. Coping with job insecurity: How does personality make a difference? Journal of Organizational Behavior. 1993;14:617–630. [Google Scholar]
- 34.Greenglass ER. Esther R, editor. The contribution of social support to coping strategies. In Special Issue on Women and Management, Guest. Greenglass and Judi Marshall, Applied Psychology: An International Review. 1993;42(4):323–340. [Google Scholar]
- 35.Maslach C, Schaufeli W, Leiter MP. Job burnout. Annual Review of Psychology. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 36.Turnipseed DL. Anxiety and burnout in the health care work environment. Psychological Reports. 1998;82(2):627–642. doi: 10.2466/pr0.1998.82.2.627. [DOI] [PubMed] [Google Scholar]
- 37.Derogatis LR, Lipman RS, Rickels K, et al. The Hopkins Symptom Checklist (HSCL): A self-report symptom inventory. Behavioral Science. 1997;19:1–15. doi: 10.1002/bs.3830190102. [DOI] [PubMed] [Google Scholar]
- 38.Baba VV, Harris MJ. Stress and absence: A cross-cultural perspective. Research in Personnel and Human Resources Management. 1989;1:317–337. [Google Scholar]
- 39.Lee RT, Ashforth BE. A meta-analytic examination of the correlates of the three dimensions of job burnout. Journal of Applied Psychology. 1996;81(2):123–133. doi: 10.1037/0021-9010.81.2.123. [DOI] [PubMed] [Google Scholar]
- 40.Leiter MP. The impact of family resources, control coping, and skill utilization on the development of burnout: A longitudinal study. Human Relations. 1990;11:1067–1083. [Google Scholar]
- 41.Stewart W, Barling J. Daily work stress, mood and interpersonal job performance: A mediational model. Work & Stress. 1996;10(4):336–351. [Google Scholar]
- 42.Abd El-aal NH, Ibrahim Hassan N. Relationship between staff nurses’ satisfaction with quality of work and their levels of depression, anxiety and stress in critical care units. Journal of American Science. 2014;10:1s. [Google Scholar]
- 43.Gökçen C, Zengin S, Oktay MM, Alpak G, Al B, Yıldırım C. Burnout, job satisfaction and depression in the healthcare personnel who work in the emergency department. Anadolu Psikiyatri Derg. 2013;14(2):122–128. [Google Scholar]
- 44.Carod-Artal FJ, Vazquez-Cabrera C. Burnout for experts. US: Springer; 2013. Burnout syndrome is an International setting; pp. 15–35. [Google Scholar]
- 45.Gito M, Ihra H, Ogata H. The relationship of resilience, hardiness, depression and burnout among Japanese psychiatric hospital nurses. Journal of Nursing Education and Practice. 2013;3(11):12–18. [Google Scholar]
- 46.Bakker AB, Costa PL. Chronic job burnout and daily functioning: A theoretical analysis. Burnout Research. 2014;1(3):112–119. [Google Scholar]
- 47.Burke RJ, Greenglass ER. A longitudinal study of psychological burnout in teachers. Human Relations. 1995;48(2):187–202. [Google Scholar]
- 48.Chopra SS, Sotile WM, Sotile MO. Physician burnout. JAMA. 2004;291(5):633. doi: 10.1001/jama.291.5.633. [DOI] [PubMed] [Google Scholar]
- 49.Arsenault A, Dolan SL, Van Ameringen MR. Stress and mental strain in hospital work: Exploring the relationship beyond personality. Journal of Organizational Behavior. 1991;12:483–493. [Google Scholar]
- 50.Bluen SD, Barling J, Burns W. Predicting sales performance, job satisfaction, and depression by using the achievement strivings and impatience-irritability dimensions of Type-A Behavior. Journal of Applied Psychology. 1990;75(2):212–216. [Google Scholar]
- 51.Soares JF, Jablonska B. Psychosocial experiences among primary care patients with and without musculoskeletal pain. European Journal of Pain. 2004;3:79–89. doi: 10.1016/S1090-3801(03)00083-1. [DOI] [PubMed] [Google Scholar]
- 52.Beck J, Gerber M, Brand S, Puhse U, Holsboer-Trachsler E. Executive function performance is reduced during occupational burnout but can recover to the level of healthy controls. Journal of Psychiatric Research. 2013;47(1):1824–1830. doi: 10.1016/j.jpsychires.2013.08.009. [DOI] [PubMed] [Google Scholar]
- 53.Rossouw L, Seedat S, Emsley RA, Suliman S, Hagemeister D. The prevalence of burnout and depression in medical doctors working in the Cape Town Metropolitan Municipality community healthcare clinics and district hospitals of the Provincial Government of the Western Cape: a cross-sectional study. South African Family Practice. 2013;55(6):567–573. [Google Scholar]
- 54.Bianchi R, Boffy C, Hingray C, Truchot D, Laurent E. mparative symptomatology of burnout and depression. Journal of health psychology. 2013;18(6):782–787. doi: 10.1177/1359105313481079. [DOI] [PubMed] [Google Scholar]
- 55.Marchand A, Durand P, Juster RP, Lupien SJ. Workers’ psychological distress, depression, and burnout symptoms: associations with diurnal cortisol profiles. Scandinavian journal of work, environment & health. 2014;40(3):305. doi: 10.5271/sjweh.3417. [DOI] [PubMed] [Google Scholar]
- 56.Machado T, Sathyanarayanan V, Bhola P, Kamath K. Psychological vulnerability, burnout, and coping among employees of a business process outsourcing organization. Industrial psychiatry journal. 2013;22(1):26. doi: 10.4103/0972-6748.123609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Adebowale TO, Adelufosi AO. Stress and minor psychiatric morbidity among Nigerian executives: Some socio-demographic and biological correlates. Annals of medical and health sciences research. 2013;3(3):412–416. doi: 10.4103/2141-9248.117946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chen X, Tan X, Li L. Health problem and occupational stress among Chinese doctors. Chinese Medicine. 2013;4:1. [Google Scholar]
- 59.Tanaka JS, Huba GJ. Confirmatory hierarchical factor analysis of psychological distress measures. Journal of Personality and Social Psychology. 1984;46:621–635. [Google Scholar]
- 60.Firth H, Mc Keown P, Mc Intee J, et al. Professional depression, “burnout” and personality in longstay nursing. International Journal of Nursing Studies. 1987;24:227–237. doi: 10.1016/0020-7489(87)90005-8. [DOI] [PubMed] [Google Scholar]
- 61.Toker S, Shirom A, Shapira I, et al. The Association between Burnout, Depression, Anxiety, and Inflammation Biomarkers: C-Reactive Protein and Fibrinogen in Men and Women. Journal of Occupational Health Psychology. 2005;10(4):344–362. doi: 10.1037/1076-8998.10.4.344. [DOI] [PubMed] [Google Scholar]
- 62.Corrigan PW, Holmes EP, Luchins D, et al. Staff burnout in a psychiatric hospital: A cross-lagged panel design. Journal of Organizational Behavior. 1994;15:65–74. [Google Scholar]
- 63.Meier ST. The construct validity of burnout. Journal of Occupational Psychology. 1984;57:211–219. [Google Scholar]
- 64.Duquette A, Sandhu BK, Beauter L. Factors relating to nursing burnout: a review of empirical knowledge. Issues in Mental Health Nursing. 1994;15:337–358. doi: 10.3109/01612849409006913. [DOI] [PubMed] [Google Scholar]
- 65.Zellars KL, Perrewé PL. Affective personality and the content of emotional social support: coping in organizations. J Appl Psychol. 2001;86(3):459–467. doi: 10.1037/0021-9010.86.3.459. [DOI] [PubMed] [Google Scholar]


