Abstract
Introduction:
Psoriasis is a chronic skin ailment, which can be connected with other ailments including dyslipidemia.
Examinees and methods:
Research included 70 patients affected by psoriasis. Both genders, above 18 years of age. Average age of the respondents was 47.14 (SD= ±15.41), which consisted of 36 men (51.43%) and 34 women (48.57%). The average duration of psoriasis was 15.52 (SD= ±12.54) years.
Results:
Frequency of dyslipidemia on those affected by psoriasis was 62.85%. Most often it was hypertriglyceridemia (39%) and hypertriglyceridemia with a lowered value of HDL (36%), average age of those affected by psoriasis with dyslipidemia was 48.76 years (SD= ±14.72), and the average duration of the basic disease was 16.15 years (SD= ±12.63), the average values of the PASI score were 16.65. Increase in values of PASI score and dyslipidemia were statistically significantly connected (r=0.41; p=0.0001).
Conclusion:
Psoriasis is connected with dyslipidemia.
Keywords: psoriasis, dyslipidemia
1. INTRODUCTION
Psoriasis is a chronic ailment of unknown etiology. Different studies, conducted among different populations have investigated the relation between psoriasis and metabolism of fats, that is dyslipidemia. By reviewing 19 studies which investigated the relation between psoriasis and dyslipidemia, a meaningful connection between psoriasis and dyslipidemia has been discovered in 17 studies (1). Next to the frequency of appearance of dyslipidemia, a subject of interest were changes in the composition of lipids. In most studies, statistically, the amount of overall cholesterol has been increased, LDL cholesterol and/or triglycerides in those affected by psoriasis relating to the control groups, and a lowered HDL cholesterol (2).
Although the precise relation between psoriasis and dyslipidemia has never been established, those affected by psoriasis had their proinflammatory cytokines elevated: example. TNF IL-1 or IL-6, and they can besides all else also affect the metabolism of lipids (3). Appearance of dyslipidemia can also be attributed to the subject’s life style, such as physical inactivity, inadequate nutrition, stress.
Dyslipidemia as a comorbidity can also appear during the treatment of psoriasis with cyclosporine and acitretin (1). Appearance of dyslipidemia in those affected by psoriasis is meaningful considering that dyslipidemia can be a factor of risk for other ailemnts, mainly cardio-vascular ones.
2. THE AIM OF THE RESEARCH
To establish the frequency of dyslipidemia in those affected by psoriasis, and to establish the severity of psoriasis with the occurrence of dyslipidemia.
3. PARTICIPANTS AND METHODS
This perspective research has occurred in the period between November of 2011 and June of 2013, it consisted of 70 consecutively chosen patients affected by psoriasis, of both genders, older than 18 years of age. Average age of the respondents was 47.14 (SD= ±15.41), which consisted of 36 men (51.43%) and 34 women (48.57%). The average duration of Psoriasis was 15.52 (SD= ±12.54) years.
Research also included patients with documented cases of diagnosed psoriasis, ambulatory or hospital reports from dermatologist, and pathophysiological report, of those who were treated at the clinic for skin diseases of University clinical center Tuzla. Research did not include patients which besides psoriasis suffered from some other skin disease, and those which suffered from psoriasis for less than a year. Research has been approved from the side of ethics committee of University clinical center Tuzla.
Firstly, all examinees were explained the purpose of the research, asked for a written consent to participate in the research, taken anamnesis, got their skin and visible mucous membranes dermatologically tested and had their PASI score values determined, after which they were subjected to the research, and lastly, had the values of their complete cholesterol, HDL cholesterol and triglycerides tested.
Reference values are: Cholesterol ≤ 5.2 mmol/L, triglycerides ≤ 1.7mmol/L, HDL cholesterol (in men ≤ 1.03mmol/L) and in women <1.29mmol/L).
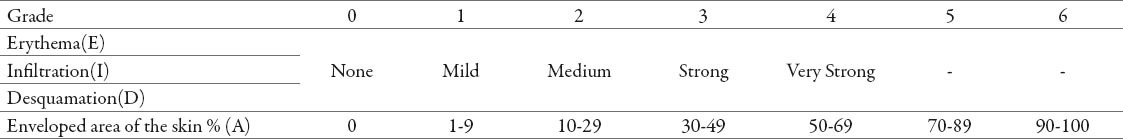
For determining the severity and outspread of psoriasis, Psoriasis Area and Severity Index (PASI) was used. In four regions body-head, torso, upper and lower extremities. In the four regions of the body-head, torso, upper and lower extremities evaluated the characteristics of the disease, severity of erythema, infiltration and desquamation with the score 1-4, and the affected area of skin psoriatic changes with the score 1-6 (Table 1). In assessing the severity of erythema scales may not be removed. Theoretically PASI can range from 0-72 (4).
Table 1.
Measurement of PASI
By this method we calculate :
Buttocks as a part of lower extremities, that is, region of the leg (l)
Armpits and shoulders as a part of upper extremities, that is, region of the arm (a)
The neck is calculated as a part of the head (h)
Torso (t)
For calculating the PASI, the summation of erythema, infiltrations and desquamation of single region is multiplied with the numerical value of the region of the body and with the percentage by which the lesions have spread at a single region. Results obtained for each single region are calculated in PASI.
Form for calculating PASI:
PASI=0.1×(Eh+Ih+Dh)×Ah+0.3×(Et+It+Dt)×At+0.2×(Ea+Ia+Da)×Aa+0,4×(El+Il+Dl)×Al
Legend :
E–Erythema
I–Infiltration
D – Desquamation
A – Area
h–head
t–torso
a–arm
l–leg
Statistical analysis
For data processing and hypothesis testing was used statistical package Arcus Quickstat Biomedical Version 1.0. Statistical series are described measures of central tendency and variability measures. The relationship between variables was estimated correlation test. As the minimum value of the level of significance was taken as p <0,05.
4. RESULTS
The frequency of dyslipidemia in those affected by psoriasis was 62.85%. Mostly it was hypertriglyceridemia (39%) and hypertriglyceridemia with a lowered value of HDL (36%). The average age of those affected by dyslipidemia was 48.76 years (SD= ±14.72), and the average duration of the basic disease was 16.15 years (SD= ±12.63).
Clinical characteristics of the patients were estimated based on the index of severity of psoriasis on the affected area, (PASI). The average PASI score values were 16.65. The increase in values of PASI score and dyslipidemia were statistically highly connected. (Figure 1).
Figure 1.
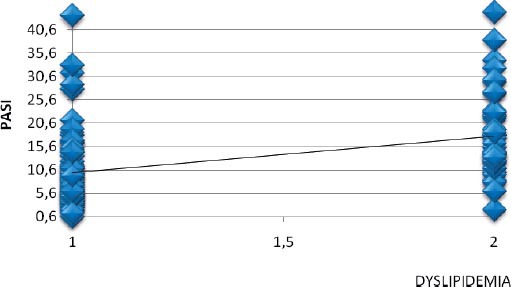
Relation between values of PASI score and dyslipidemia (r=0,41; p=0,0001).
5. DISCUSSION
In this research, the frequency of dyslipidemia in those affected by psoriasis was 62.85%. Other studies have also shown an increased frequency of dyslipidemia by reviewing literature, which were analyzed by 25 studies, 20 studies showed that psoriasis is connected with dyslipidemia (5). In Brazil around 67% of those affected by psoriasis also had dyslipidemia (6). Study in Japan also showed that dyslipidemia is closely connected with psoriasis, respectively, dyslipidemia occurs in those affected by psoriasis at around 34.3% and in the control group, 16.2% (P <0.01),(7). In the research in Israel, the frequency of dyslipidemia was statistically higher in those affected by psoriasis (56.9%), compared to the control group (47.3%) (P<0.001) (8).
Hypertriglyceridemia was present in 39% of examinees, and hypercholesterolemia was present in 36% of examinees. Other studies also discovered an increased frequency of hypertriglyceridemia and hypercholesterolemia in those affected by psoriasis. In Denmark, prevalence of hypercholesterolemia was higher in those affected by psoriasis, compared to the control group (9), and in Great Britain, an increased number of triglycerides was discovered in those affected by psoriasis compared to the control group (36% vs 28%) (10).
The average age of those affected by psoriasis with dyslipidemia was 48.76 years (SD = ±14.72) and was similar to the average age of all examinees which was 47.14 years (SD =±15.41). And the average duration of psoriasis in those affected by dyslipidemia was 16.15 years (SD= ±12.63) and was similar to the average duration of psoriasis on all examinees, which was 15.52 years (SD =± 12.54). This research contained a positive correlation between PASI values and dyslipidemia (r=0.41 p=0.001), that is, the severity of psoriasis and frequency of dyslipidemia, which is confirmed by tests of other research, so in a research conducted in Middle East, prevalence of dyslipidemia in those affected by psoriasis is 14.1% for mild to medium psoriasis, (PASI<10), 22.48% for severe psoriasis (PASI>10), and in the control group 4,96% (11). The correct mechanism of connections between psoriasis and dyslipidemia is not known. It is considered that proinflammatory cytokines in those affected by psoriasis can also affect the metabolism of lipids, but diet and medicines used for treatment of psoriasis are also important. Connection between psoriasis and dyslipidemia has been confirmed, and the effect of severity of psoriasis on the frequency of dyslipidemia, but further research is required to determine the precise mechanisms of that connection. Further research will illuminate the connection between psoriasis and metabolism of fats. Based on the current findings, it is necessary to follow lipid status in those affected by psoriasis, in a goal to prevent lipid disorders, diagnostics and treatment of already existing disorders of fats, considering it contains risk factors and can lead to development of other ailments, especially cardiovascular ones.
6. CONCLUSION
Psoriasis is connected with dyslipidemia, but it is necessary to further research the precise mechanism of that connection.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Daudén E, Castañeda S, Suárez C, García-Campayo J, Blasco AJ, Aguilar MD, et al. Integrated approach to comorbidity in patients with psoriasis. Working Group on Psoriasis-associated Comorbidities. Actas Dermosifiliogr. 2012;103(1):1–64. doi: 10.1016/S0001-7310(12)70001-7. [DOI] [PubMed] [Google Scholar]
- 2.Pietrzak AT, Zalewska A, Chodorowska G, Krasowska D, Michalak-Stoma A, Nockowski P, et al. Cytokines and anticytokines in psoriasis. Clin Chim Acta. 2008;394(1-2):7–21. doi: 10.1016/j.cca.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 3.Azfar R, Gelfand J. Psoriasis and metabolic disease: epidemiology and pathophysiology. Curr Opin Rheumatol. 2008;20(4):416–422. doi: 10.1097/BOR.0b013e3283031c99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fredriksson T, Pettersson U. Severe psoriasis - oral therapy with new retinoid. Dermatologica. 178(157):238–244. doi: 10.1159/000250839. [DOI] [PubMed] [Google Scholar]
- 5.Ma C, Harskamp CT, Armstrong EJ, Armstrong AW. The association between psoriasis and dyslipidaemia: a systematic review. Br J Dermatol. 2013;168(3):486–495. doi: 10.1111/bjd.12101. [DOI] [PubMed] [Google Scholar]
- 6.Rosa DJ, Machado RF, Matias FA, Cedrim SD, Noronha FL, Gaburri D, et al. Influence of severity of the cutaneous manifestations and age on the prevalence of several cardiovascular risk factors in patients with psoriasis. Eur Acad Dermatol Venereol. 2012;26(3):348–353. doi: 10.1111/j.1468-3083.2011.04076.x. [DOI] [PubMed] [Google Scholar]
- 7.Takahashi H, Iizuka H. Psoriasis and metabolic syndrome. J Dermatol. 2012;39(3):212–218. doi: 10.1111/j.1346-8138.2011.01408.x. [DOI] [PubMed] [Google Scholar]
- 8.Dreicher J, Weitzman D, Davidovici B, Shapiro J, Cohen AD. Psoriasis and dyslipidaemia: a population-based study. Acta Derm Venereol. 2008;88(6):561–565. doi: 10.2340/00015555-0510. [DOI] [PubMed] [Google Scholar]
- 9.Gyldenløve M, Jensen P, Linneberg A, Thyssen JP, Zachariae C, Hansen PR, et al. Psoriasis and the Framingham risk score in a Danish hospital cohort. Int J Dermatol. 2013 doi: 10.1111/ijd.12196. doi: 10.1111/ijd.12196. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 10.Langan SM, Seminara NM, Shin DB, Troxel AB, Kimmel SE, Mehta NN, et al. Prevalence of metabolic syndrome in patients with psoriasis: a population-based study in the United Kingdom. J Invest Dermatol. 2012;132(3 Pt 1):556–562. doi: 10.1038/jid.2011.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al-Mutairi N, Al-Farag S, Al-Mutairi A, Al-Shiltawy M. Comorbidities associated with psoriasis: an experience from the Middle East. J Dermatol. 2010;37(2):146–155. doi: 10.1111/j.1346-8138.2009.00777.x. [DOI] [PubMed] [Google Scholar]


