Abstract
Introduction:
More than three decades after recognition of acquired immunodeficiency syndrome (AIDS) in the United States, the pandemic of human immunodeficiency virus (HIV) infection has dramatically changed the global burden of disease.
Aim:
The main goal of this research is retrospective analysis of epidemiological and clinical characteristics of 28 HIV infected patients, who were diagnosed and treated at the Clinic for Infectious Diseases in University Clinical Center Tuzla in the period from 1996 until the end of 2013.
Subjects and Methods:
Retrospective analysis was performed using the medical records of 28 HIV-infected persons. Two rapid tests were used for HIV testing: OraQuick Advance test, Vikia HIV1/2, Elisa combo test, HIV RNA test. AIDS disease was determined by using the criteria from WHO.
Results:
Among a total of 28 HIV-infected persons, 23 (82.14%) were males and 5 (17.86%) were females, with the male: female ratio of 4,6:1. In terms of the transmission route, a large proportion of cases were infected through heterosexual contact 19 (67.86%). At the time of the first visit, 16 (57.15%) patients showed asymptomatic HIV infection, 4 (14.28%) HIV infection with symptoms other than the AIDS defining diseases, and 8 (28.57) had AIDS. At the time of first hospital visit, the CD4 + cells count ranged from 40 to 1795/µl (conducted in 19 patients), and mean value of CD4 + cells was 365,31/µl, and mean HIV RNA titer was 287 118 copies/ml³. Of 28 HIV-infected persons 39 cases of opportunistic diseases developed in 12 patients (42.9%). In terms of the frequency of opportunistic diseases, tuberculosis (12 cases, 42.9%). Among a total of 28 HIV-infected patients, 6 (21.4%) of them died.
Conclusion:
This study characterizes the epidemiological and clinical patterns of HIV–infected patients in Tuzla region of Bosnia and Herzegovina to accurately understand HIV infection/AIDS in our region, in the hope to contribute in the establishment of effective HIV guidelines in the Tuzla region of B&H in the future.
Keywords: HIV, hospitalized patients, epidemiology, clinical characteristics
1. INTRODUCTION
More than three decades after recognition of acquired immunodeficiency syndrome (AIDS) in the United States, the pandemic of human immunodeficiency virus (HIV) infection has dramatically changed the global burden of disease, and its effects will continue well into the next decades (1, 2).
According to estimates done by the World Health Organization (WHO) and the Joint United Nations Programme on HIV/AIDS (UNAIDS) at the end of 2011, there were 34 million people around the world who were infected with HIV, which accounted for an increase of about 20% in comparison with 2001. In 2001, 2.5 million people around the world were infected with HIV, and 1.7 million died of AIDS. It is, at the global level, reduction for 20% of new HIV infections compared with 2001, and 24% fewer deaths from AIDS than there were in 2005. These estimates of reduction in the number of new infections and deaths from HIV/AIDS at the global level, show significant progress in preventing the spread of infection and increase in the number of people who have access to treatment and drugs (3). The number of those infected with HIV has now reached 35 million (4).
Since 1986, when the first HIV infected patient was registered in Bosnia and Herzegovina (B&H), until November 2003, totally 250 HIV infected persons were registered, of which 127 (50,8%) developed AIDS. HIV is mostly transmitted by sexual contact, and in B&H 127 (50,8%) persons are infected through heterosexual contact, 78 (31,2%) by homosexual contact, 22 (8,8%) by intravenous drug use, 3 (1,2%) by blood products, vertical transmission in 2 (0,8%) cases, and for 18 (7,2%) persons there are no data of transmission route. In Federation of Bosnia and Herzegovina (FB&H) since 1986, with exception of 10 cases who were registered before war, 151 persons are HIV positive, of which 78 (51,65%) developed AIDS. Eighty percent from that number are males and 20% are females. Depending of the route of transmission, 76 (50,35%) are infected by heterosexual contact, 53 (35,10%) by bisexual contact, 15 (9,94%) by intravenous drug use, 1 (0,66%) by vertical transmission, and for 5 (3,31%) there are no data of transmission route (5,6).
In the Register for HIV infected in Croatia, from 1985, when the first HIV infected patient was registered, by the end of 2012, 1017 HIV infected persons were registered, of which 371 with AIDS. In the same period 187 persons died of AIDS (7).
HIV clinical presentation is known to be complex since AIDS was described in 1981 (8). HIV can manifest in a variety of ways depending on the organs affected and concurrent infections prevalent in the area. The initial clinical presentation may mimic symptoms of common endemic diseases in the particular region (9-12). However, the severity of manifestation depends on the infected individuals baseline health status. The most significant early manifestation of HIV infection in Africa were marked by slim disease (diarrhea and wasting), tuberculosis, variety of Opportunistic Infections (OI), weight loss, fever, and dermatological symptoms (11,13).
WHO has established a four stage classification system determined by the presence of Opportunistic Infections and other HIV related conditions (14).
The main goal of this research is retrospective analysis of epidemiological and clinical characteristics of 28 HIV infected patients, who were diagnosed and treated at the Clinic for Infectious Diseases in University Clinical Center Tuzla in the period from 1996 until the end of 2013.
2. MATERIALS AND METHODS
2.1. Subjects
The subjects were patients who were treated at the Clinic for Infections Disease of the University Clinical Centre Tuzla, from 1996, when the first case of HIV infection was registered in Tuzla, until end of 2013. Retrospective analysis was performed using the medical records of 28 HIV-infected persons.
2.2. Methods
Medical records provided information on sex, age, transmission route, reasons for testing, history of earlier diseases, state of diseases, the presence or absence of opportunistic infections, the outcome of the infection, and immunologic and virologic status.
Two rapid tests were used for HIV testing: OraQuick Advance test is a test for quick qualitative detection of antibodies for HIV 1/2 virus. The test strip contains synthetic peptides representing the procedural control of the region of HIV envelope, and sheep anti-human IgG antibodies which are immobilized on the nitrocellulose membrane in the test (T) and control (C) range (Qarad, Geel, Belgium) and Vikia HIV 1/2 test which is based on immunochromatografic technique for qualitative detection of serum antibodies to HIV-1 and HIV-2 in human serum, plasma or whole blood (BioMerieux, Lyon, France). CD4 + cell count are obtained by adding into a sample of blood of HIV-infected person a suitable reagent (monoclonal antibody specific for CD4, conjugated with a fluorochrome), and analyzed by flow cytometer (FC 500 Beckman Coulter Flow Cytometer, Nyon, Switzerland). p24 Ag is measured based on the ELISA method (Abott, Illinois, USA). HIV RNA was measured using RT-PCR Cobas Amplicor HIV1 Monitor test (Mannhein, Germany). AIDS was defined in those cases that were positive by Western blot and with an AIDS defining disease. AIDS disease was determined by using the criteria from WHO (14).
3. RESULTS
3.1. Epidemiological characteristics
Among a total of 28 HIV-infected persons, 23 (82.14%) were males and 5 (17.86%) were females, with the male: female ratio of 4,6:1. (Table 1).
Table 1.
Characteristics of 28 HIV-infected patients
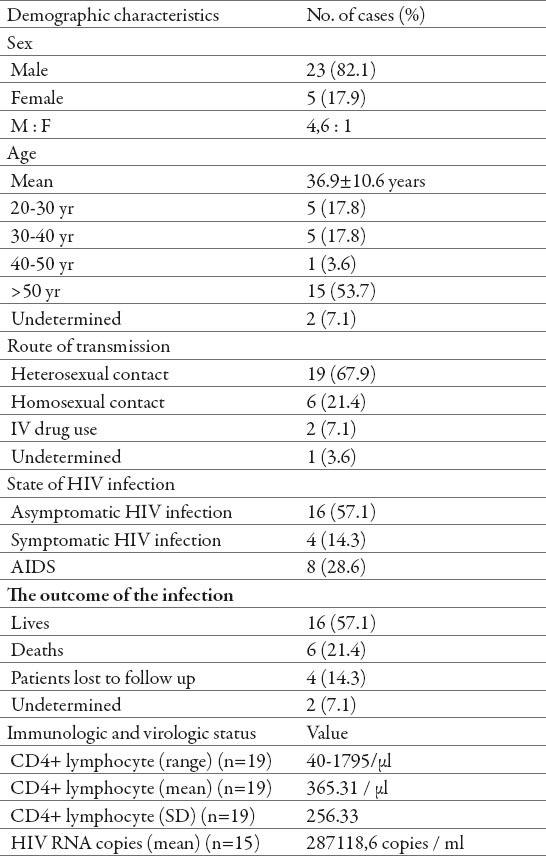
As for age distribution at the time of the initial diagnosis of HIV infection, 5 (17.86%) were diagnosed in the age from 20 to 30 years, 5 (17.86%) in the age from 30 to 40 years, 1 (03.57%) in the age from 40 to 50 years, 15 (53.57%) in the age > 50 years. The age of patients ranged from 20-57 years. The average age at the time of first hospital visit of those patients was 36.9 ± 10.6 years. In terms of the transmission route, a large proportion of cases were infected through heterosexual contact 19 (67.86%), followed by homosexual contact 6 (21.43%), intravenous drug use 2 (07.14%), and other routes 1 (03.57%). At the time of the first visit, 16 (57.15%) patients showed asymptomatic HIV infection, 4 (14.28%) HIV infection with symptoms other than the AIDS defining diseases, and 8 (28.57) had AIDS.
3.2. Clinical characteristics
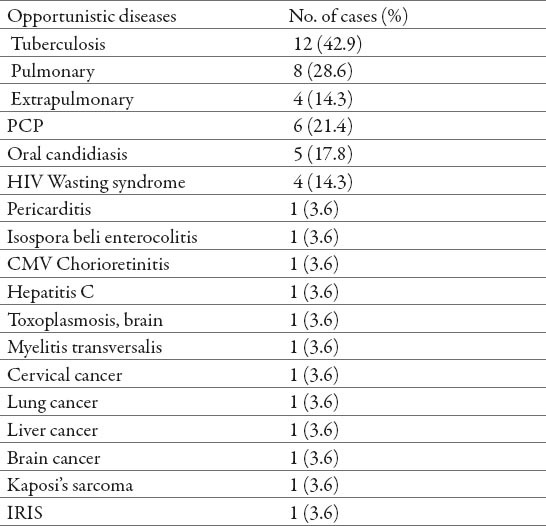
At the time of first hospital visit, the CD4 + cells count ranged from 40 to 1795/µl (conducted in 19 patients), and mean value of CD4 + cells was 365,31/µl, and mean HIV RNA titer was 287 118 copies/ml³ (conducted in 15 patients). Of 28 HIV-infected persons 39 cases of opportunistic diseases developed in 12 patients (42.9%). In terms of the frequency of opportunistic diseases, tuberculosis (12 cases, 42.9%) was the most prevalent followed by Pneumocystis carinii pneumonia (6 cases, 21.4%), oral candidiasis (5 cases, 17.8%), HIV Wasting syndrome (4 cases, 14.3%). It was registered 1 (3.6%) case of each of the following opportunistic diseases: pericarditis, Isospora beli enterocolitis, CMV chorioretinitis, hepatitis C, toxoplasmosis of the brain, myelitis transversalis, IRIS. Malignant diseases were registered in 5 (17.8%) patients, 1 (3.6%) case of each of the following malignant diseases: cervical cancer, lung cancer, brain cancer, liver cancer and Kaposi’s sarcoma (Table 2).
Table 2.
Opportunistic diseases of 12 HIV-infected patients (n=28 cases) (PCP, Pneumocystis carinii pneumonia; CMV, cytomegalovirus; IRIS, immune reconstitution inflammatory syndrome.)
Among a total of 28 HIV-infected patients, 6 (21.4%) of them died. Three patients died shortly after detection of infection, because the infection was detected 5 days before death. Second comatose patient with the symptoms of multiorganic tuberculosis died 3 days after admission. His wife after the positive HIV test, refused further examination and treatment. She admitted 7 months later with the symptoms of lung tuberculosis, exudative pleuritis and specific lymphadenitis. She died shortly after the admission. Fifth patient died because of toxoplasmosis infection of the brain, one female patient died after double operation of brain tumor, sixth patient died in 1996, because of the lack of the ART. Seventeen (60,7%), of the 28 HIV infected patients, were treated with ART.
4. DISCUSSION
The main transmission routes of HIV infection are through sexual contact, syringes, blood products, and vertical transmission. In the Korea, the main transmission route is heterosexual contact (52.3%), followed by homosexual contact (23.9%), transfusion/blood products (2.3%) intravenous drug use (1.1%) and other routes (20.5%) (12). In Germany, the main transmission is also through homosexual contact (64.6%), followed by intravenous drug use (14.9%), and heterosexual contact (8.8%) (15). In Sub-Saharan Africa, the transmission of HIV is mostly through heterosexual contact (11). In Croatia, HIV/AIDS is registered almost exclusively among high risk population, with homosexual route being the most dominant route of transmission (7). Intravenous drug use is the main transmission route in Eastern Europe (16).
In Africa, the percentage of pregnant women who are HIV positive has reached up to 40% in certain regions, which is a high risk for vertical transmission (1). We determined that in our patients, heterosexual contact was the most frequent route of HIV transmission (67.9%), and the homosexual contact was also a major contributor accounting 21.4%. Since 1986, when the first HIV positive patient was registered in B&H, most HIV positive persons were infected by heterosexual contact 127 (50,8%), by homosexual contact 78 (31,2%), by intravenous drug use 22 (8,8%), and for 18 (7,32%) persons there are no data of transmission route (5,6).
At the time of first hospital visit 57.1% of the patients were diagnosed as asymptomatic HIV infection, 14.3% as symptomatic HIV infection and 28.6% as AIDS, and their immunity was with an average CD4 cell count of 365.31/µl. In this period we detected 24 HIV infected persons, and 4 persons came to our clinic with already known HIV positive status. Four of them were infected in B&H, 8 were infected in other European countries, and 1 was infected in Africa. Two persons after getting their HIV positive status left B&H, they went back to their origin countries, Moldova respectively Germany, so we had 26 HIV positive patients who had regular checkups and treatment in our clinic. Because of the stigma and discrimination, the number of tested persons in Centers for voluntary confidential counseling and testing (VCCT centers) is still small, while the number of persons with risky behavior is in rise.
Most of the known common HIV related opportunistic infections were less frequent than expected in this population despite many patients having CD4 cell counts less than 200 cell per µl (1). It is well established that patients at this level of CD4 + cell counts have high risk of AIDS opportunistic infections and AIDS related cancers (14.17). A study in the US in 1999 reported that most prevalent opportunistic disease was P. Carinii pneumonia (53.0%) and this was followed by atypical mycobacterium infection (30.0%), esophageal candidiasis (24.4%), Kaposis sarcoma (22.6%), HIV wasting syndrome (20.8%) and CMV retinitis (20.6%) (18). In study in the Nepal in 2009 high prevalence high prevalence of opportunistic infections as pneumonia (52.8%), oral thrush (33.9%) and esophageal candidiasis (24.5%) (19). In the northern European countries, the major opportunistic diseases are P. Carinii pneumonia, and in southwestern European countries, extra pulmonary tuberculosis (20). In our patients tuberculosis was the leading opportunistic disease (42.9%). Tuberculosis (31-61%) is the most frequent opportunistic disease in many reports around the world: Thailand, India, Zaire and other Southeast Asian countries (18, 21, 22, 23). Tuberculosis and HIV co-infection still presents a significant cause of mortality, especially in Africa, although their incidence has been declining since 2005. Tuberculosis can occur at any stage of HIV-infection, and the risk of developing the disease as well as its atypical forms is higher as cell immunity is impaired. P. Carinii pneumonia is the second most common opportunistic disease in our patients (21,4%), which is similar to many reports from around the world (1, 12). Oral candidiasis is registered in 17.8% of our patients. Candidiasis is often registered in HIV infected patients as shown in numerous of reports from many other countries (1, 11, 12). Opportunistic diseases, which are not AIDS-defining diseases, also differ according to the region, country, and race (1,14). Our study found that 21.4% of those infected with HIV died, and the main causes were tuberculosis, toxoplasmosis, brain cancer, and lack of antiretroviral therapy (ART).
5. CONCLUSION
A small number of HIV infected persons in B&H, as well as in the Tuzla region puts us among countries with low prevalence. This information should not deceive us, on the contrary it should warn us that it does not represent the true situation. Early detection of HIV infection provides good chances for the infected to begin with the ART in time, and with that to have a longer and better quality life. Because of the stigma and discrimination, the number of tested persons in VCCT centers is still small, while the number of persons with risky behavior is increasing. This study characterizes the epidemiological and clinical patterns of HIV–infected patients in Tuzla region of Bosnia and Herzegovina to accurately understand HIV infection/AIDS in our region, in the hope to contribute in the establishment of effective HIV guidelines in the Tuzla region of B&H in the future.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Piot P, Carael M. Global Perspectives on Human Immunodeficiency Virus Infection and Acqired Immunodeficiency Syndrome. In: Mandel GL, Benet JE, Dolin R, editors. Principles and practice of Infectious Diseases. Philadelphia: Churchill Livingstone, Elsevier; 2010. pp. 1619–1633. [Google Scholar]
- 2.Ezzati M, Lopez AD, Rodgers A, et al. Selected major risk factors and global and regional burden of disease. Lancet. 2002;360:1347–1360. doi: 10.1016/S0140-6736(02)11403-6. [DOI] [PubMed] [Google Scholar]
- 3.Geneve Switzerland: 2011. UNAIDS. GLOBAL HIV/AIDS RESPONSE. Epidemic update and health sector progress towards Universal Access Progress Report 2011. [Google Scholar]
- 4.Geneve, Switzerland: 2014. UNAIDS. The Gap Report. [Google Scholar]
- 5.Zavod za javno zdravstvo Federacije Bosne i Hercegovine. http://www.zzjzfbih.ba .
- 6.Republika Srpska Javna zdravstvena ustanova Institut za javno zdravstvo. http://www.phi.rs.ba/index_lat.html .
- 7.Blažić Nemeth T, Pavlić J. Epidemiologija HIV/AIDS-a u Hrvatskoj i rad centara za besplatno i anonimno savjetovanje i testiranje na HIV. Infektološki glasnik. 2013;33(1):27–33. [Google Scholar]
- 8.Piot P, Colebunders R. Clinical manifestations and natural history of HIV infection in adults. Western J Med. 1987;147:709–712. [PMC free article] [PubMed] [Google Scholar]
- 9.Begovac J. Infekcija virusom humane imunodeficijencije. In: Begovac J, Božinović D, Lisić M, Baršić B, Schönwald S, editors. Definicije, uzročnik i dijagnostika zaraze virusom humane imunodeficijencije. Zagreb: Infektologija; 2006. pp. 338–378. [Google Scholar]
- 10.Strecker W, Gurtler L, Schilling M, Binibangili M, Strecker K. Epidemiology and clinical manifestation of HIV infection in northern Zaire. Eur J Epidemiol. 1994;10(1):95–98. doi: 10.1007/BF01717460. [DOI] [PubMed] [Google Scholar]
- 11.Idindili B, Minzi O, Rumisha SF, Mugusi F, Tanner M. HIV/AIDS Clinical Manifestations and their Implication for Patient Clinical Staging in Resource Limited Settings in Tanzania. The Open AIDS Journal. 2011;5:9–16. doi: 10.2174/1874613601105010009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.June MK, Goon JC, Sung KH, Kyung HC, Joo SC, Young HC, Young GS, Aejung H, Joon SY, Kkot SL, Jun YC. Epidemiology and Clinical Features of HIV Infection/AIDS in Korea. Yonsei Med J. 2003;44(3):363–370. doi: 10.3349/ymj.2003.44.3.363. [DOI] [PubMed] [Google Scholar]
- 13.Grant A. Clinical features of HIV disease in developing countries. Leprosy Rev. 2002;73(2):197–205. [PubMed] [Google Scholar]
- 14.World Health Organization. Antiretroviral therapy for HIV infection in adults and adolescents in resource-limited settings: towards universal access recommendation for public health approach 2006 revision [Google Scholar]
- 15.UNAIDS/World Health Organization. Epidemiological fact sheet on HIV/AIDS and sexually transmitted infections-2000 update, Germany. 2000 [Google Scholar]
- 16.UNAIDS/World Health Organization. AIDS epidemic update-December. 2000:1–25. [Google Scholar]
- 17.Deuffic-Burban S, Losina E, Wang B, et al. Estimates of opportunistic infection incidence or death within specific CD4 strata in HIV-infected patients in Abidjan, Cote d’ lvoire: impact of alternative methods of CD4 count modelling. Eur J Epidemiol. 2007;22(10):737–744. doi: 10.1007/s10654-007-9175-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.CDC. Surveillance for AIDS-defining opportunistic illnesses 1992-1997. MMWR. 1999;48:1–22. [PubMed] [Google Scholar]
- 19.Shama S, Dhungana GP, Pokherel BM, Rijal BP. Clinical features of HIV/AIDS and various opportunistic infections in relation to antiretroviral status among HIV seropositive individuals from Central Nepal. Kathmandu University Medical Journal. 2009;7(4):355–359. doi: 10.3126/kumj.v7i4.2754. [DOI] [PubMed] [Google Scholar]
- 20.Blaxhult A, Kirk O, Pedersen C, Dietrich M, Barton SE, Gatell JM, et al. Regional differences in presentation of AIDS in Europe. Epidemiol Infect. 2000;125:143–51. doi: 10.1017/s0950268899004185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grant AD, Alison D, De Cock KM. The growing challenge of HIV/AIDS in developing countries. Br Med Bull. 1998;54:369–381. doi: 10.1093/oxfordjournals.bmb.a011694. [DOI] [PubMed] [Google Scholar]
- 22.Transuphasawadikul S, Amornkul PN, Tanchanpong C, Limpakarnjanarat K, Kaewkungwal J, Likanonsakul S, et al. Clinical presentation of hospitalized adult patients with HIV infection and AIDS in Bangkok, Thailand. J Acquir Immune Defic Syndr Hum Retrovirol. 1999;21:326–332. doi: 10.1097/00126334-199908010-00011. [DOI] [PubMed] [Google Scholar]
- 23.Perović-Mihanović M, Begovac J, Višković K, Puljiz I. Tuberkuloza u osoba zaraženih HIV-om. Infektološki glasnik. 2013;33(2):79–89. [Google Scholar]
- 24.Piot P, Legido-Quigley H. Global Perspectives on Human Immunodeficiency Virus Infection and Acquired Immunodeficiency Syndrome. Mandell, Douglas, and Bennet's Principles and Practice of Infectious Diseases: 2-Volume Set, 8e Hardcover-September 11. 2014:1469–1495. [Google Scholar]