Abstract
Introduction:
Acetabular fractures treatment represents a great controversy, challenge and dilemma for an orthopedic surgeon.
Aim:
The aim of the paper was to present the results of treatment of 96 acetabular fractures in the Clinic of Traumatology Banja Luka, in the period from 2003 to 2013, as well as to raise awareness regarding the controversy in the methods of choice in treating acetabulum fractures.
Material and methods:
The series consists of 96 patients, 82 males and 14 females, average age 40.5 years. Traffic trauma was the cause of fractures in 79 patients (85%), and in 17 patients (15%) fractures occurred due to falls from height. Polytrauma was present in 31 patients (32%). According to the classification of Judet and Letournel, representation of acetabular fractures was as follows: posterior wall in 32 patients, posterior column in 28, anterior wall in 4, anterior column in 2, transverse fractures in 8, posterior wall and posterior column in 10, anterior and posterior wall in 6, both- column in 4 and transversal fracture and posterior wall in 2 patients. 14 patients were treated with traction, that is, 6 patients with femoral traction and 8 patients with both lateral and femoral traction. 82 patients (86.4%) were surgically treated. Kocher-Langenbeck approach was applied in the treatment of 78 patients. In two patients from the Kocher-Langenbeck’s approach, the Ollier’s approach had to be applied as well. Two acetabular were primarily treated with Ollier’s approach. Extended Smith- Peterson’s approach was applied 4 times, and Emile Letournel’s (ilioinguinal) approach 14 times.
Results:
Functional outcome (after follow-up of 18 months), according to the Harris hip score of surgical treatment in 82 patients, was as follows: good 46 (56%), satisfactory 32 (39%) and poor 4 (5%). Results of acetabulum fractures treated with traction were: good 8 (57%), satisfactory 4 (28%) and poor 2 (15%). According to the Brook’s classification of heterotopic ossification, periarticular hetero-tropic calcifications after surgical treatment were: 0° in 65 patients (79%), I-II° in 9 patients (11%) and III-IV ° in 8 patients (10%). Calcifications in 14 patients treated with traction of heterotopic ossification by Brook-s classification were as follows: 0° in 10 patients (72%), I-II ° in 3 patients (22%) and III-IV° in 1 patient (6%).
Conclusion:
At the occurrence of acetabular fracture, it is necessary to start the treatment immediately, with an obligatory application of thromboembolic and antibiotic prophylaxis. Conservative treatment is acceptable if the dislocation of fracture is less than 5 mm. Indications for surgical treatment are incongruent or unstable fractures with verified dislocation greater than 5 mm, as well as when the radiography measured by JM Matta shows incongruence of acetabular roof less than 40° in all planes. Kocher-Langenbeck approach is the choice of surgical approach for the management of posterior column / wall, and Letournel’s (ilioinguinal) approach is the choice for the management of anterior wall/column.
Keywords: Acetabulum, fracture, Harris hip score, therapy
1. INTRODUCTION
Due to their weight, as well as the consequences they leave, acetabular fractures occupy an important place in modern traumatology. Their treatment represents a major challenge and dilemma for orthopedic surgeon. Depending on the author, representation of acetabular fractures ranges from 0.5-8%. High-energy force causes a fracture in young patients (38.6 ± 4.6), more frequently in males- 69.4% (1). More frequently, low-energy force leads to acetabular fractures in elderly patients (1). Type of acetabular fracture is determined by the position of the femoral head at the time of injury. Most common causes of acetabular fracture are: traffic accidents in 80.5%, falls from height in 10.7% and other causes in 8.8% (1). Acetabular injuries are followed by polytrauma in 20% -50% of cases. In 36% of cases, acetabular fracture is accompanied with injury of the lower extremities (2). Classification of acetabular fractures by Judet and Letournel is used as a guide to treatment and as a comparison method regarding the results of other authors.
After diagnosis, the greatest controversy in the treatment of fractures represents the treatment choice: operational or non-operational. Common indication for operative treatment is a significant dislocation of fragments more than 5 mm, incongruence between the femoral head and acetabular roof-arc. Acetabular fractures are treated operatively in the case when the acetabular roof-arc by JM Matta is of 40° or less in all planes: an anterior roof-arc of 30° or less, a medial roof-arc of 40° and a posterior roof-arc of 50°(2). Nonoperative treatment of fractures of vision is conditioned by general health, age, occupation, displacement of fragments less than 2-5mm of roof-arc, low anterior column fractures, joint column fractures with a secondary congruence without a considerable anterior shift of the columns (3).
Objective
The aim of this study was to show the results of treatment of 96 acetabular fractures at the Clinic of Traumatology Banja Luka, in the period from 2003 to 2013, as well as to raise awareness regarding the controversy in the methods of choice in treating acetabulum fractures, and finally, to choose an adequate approach in fractures treatment in order to preserve functional, mobile, painless hip for the rest of the patient’s life.
2. PATIENTS AND METHODS
In the present study, we present a series of patients with acetabular fractures who were treated from 2003 to 2013 at the Clinic of Traumatology in University hospital Clinical Centre Banja Luka. The series consisted of 96 patients, 82 males and 14 females, average age 40.5 years. Traffic trauma was the cause of fractures in 79 patients (85%), fall from height in 12 patients (11%) and other causes in 5 patients (4%). Upon arrival at the hospital, the clinical and radiographic diagnosis of fractures was performed. Radiographic examinations are: standard AP view of the pelvis with both hips and a scan in the inner and outer rotation of 45° (obturator oblique view and iliac oblique view) which gives an insight into the acetabular fracture. Diagnosis: Computed tomography (CT), that is, 3D computed tomography (3D), gives an overview of the fracture and the acetabular interior. This type of diagnosis has been used since 2007. Polytrauma was present in 31 patients (32%): broken ribs and chest injuries in 12 patients, pelvis in 4, abdominal visceral injuries in 7, n. ischiadicus in 3, fracture of the femur in 4, tibia fracture in 6 and craniocerebral injury in 1 patient. Chi-square test confirmed that polytrauma was not statistically dominant in acetabular fractures (p <0.01). According to the Judet and Letournel classification, prevalence of acetabular fractures was as follows: posterior wall in 32 patients, posterior column in 28, anterior wall in 4, anterior column in 2, transverse fractures in 8, posterior wall and posterior column in 10, anterior and posterior wall in 6, both columns in 4, transverse fracture and posterior wall in 2 patients. After the radiography diagnosis had been performed, all luxation acetabular fractures (12 posterior and 2 anterior) were immediately repositioned under general anesthesia. While the patient was still under anesthesia, and reluxation of femoral head occurred, a supracondylar extension, used for detaining the head in acetabular, was placed. Transacetabular, supra articular acetabular fractures, together with vertical fracture of the iliac bone, lead to horizontal instability of the pelvic ring. These fractures are associated with bleeding from the bone and retroperitoneal hematoma. Initially, the hematoma is asymptomatic and hardly realizable for the diagnosis. It is not clinically seen, and due to hemoconcentration, an organism may compensate a blood test and hemoglobin reduction. A few hours after the injury, the patient can go into serious hemorrhagic shock. In transacetabular, supra articular acetabular fractures, controversy are raised by a dilemma whether to put the side traction or not.
Nowadays, when these fractures occur, we place side and supracondylar extensions, mainly to tampon the fracture and prevent bleeding from broken bones. The extension serves as a temporary reduction and immobilization of transacetabular fractures and it maintains muscle elongation until the conditions for operative treatment are achieved. If comorbidity of patients does not allow surgical treatment, temporary repositioning remains the definitive form of treatment. 14 patients were treated with traction, that is, 6 patients with femoral traction, and 8 patients with femoral and lateral traction simultaneously. “T” fractures combined with a vertical fraction line that stretches back, down-forward or ahead, were treated with femoral and lateral traction until 2007. Depending on the type of fracture, the weight up to 20% of body weight was set on the femoral supracondylar traction, while on the side; the weight was up to 10% of body weight. The resultant vector force goes in the direction of the femoral neck and “pulls” the head of the femur from the acetabulum by the technique of ligamentotaxis (Figure 1).
Figure 1.
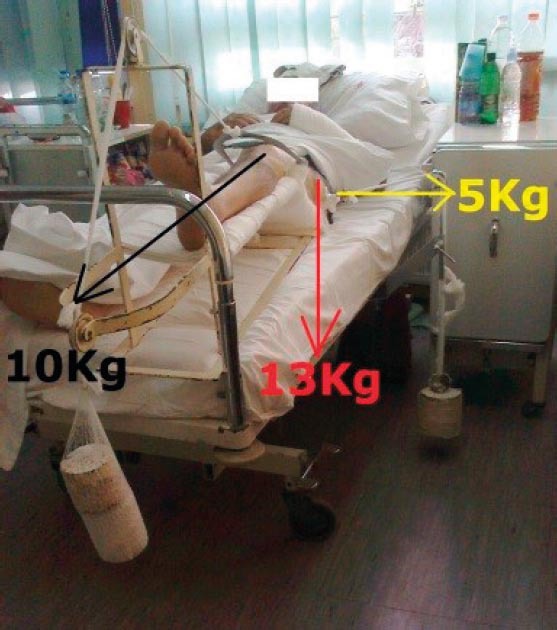
Side extension of 5 Kg and 10 Kg of supracondylar give the resultant vector force of 13 Kg which “pulls” the head of the femur from the acetabulum by the technique of ligamentotaxis
24 hours afterwards, the first radiographic control with an existing traction and weight was performed in bed. Control radiography in bed, with existing loads, was performed every second or third day, until a satisfactory reposition of acetabulum was reached.
Control radiography gave us information regarding the type of traction that needed to be corrected (supracondylar or lateral), that is, whether to increase or decrease the weight. Acquired satisfactory reposition was maintained by traction for 6 to 8 weeks, to the emergence of callus.
After removing the brake, verticalization was performed, patients were walking with the aid of armpit crutches until the emergence of mature callus. Full support was achieved 12-16 weeks after the fracture. In cases when, after 5 days of traction, an adequate reposition was not achieved, the fracture was fixed operationally. Of 96 treated acetabular fractures 14 (13.6%) were treated non operatively, and 82 (86.4%) operatively. In surgical treatment, the Kocher-Langenbeck approach was used in 78 patients. Hi-square test confirmed a statistically significant difference between methods of treatment in favor of surgical treatment (p <0.01). The controversy of using this approach raises a dilemma whether to lay the patient on his stomach or semi laterally.
We position the patient semi laterally and use posterior posterolateral (Kocher-Langenbeck) approach. With this approach, we get a full insight into the posterior acetabular wall or column but satisfying visualization of the entire acetabular roof is absent. The lateral position of the patient enables Kocher- Langenbeck approach to be “transformed” in Ollier’s approach without moving the patient. Ollier’s approach gives a good overview of the posterior wall and column as well as the roof of acetabulum. The force of gravity “pulls” muscles down so that it takes less force of Homan’s hooks which are positioned on the posterior acetabular column in order for it to be completely displayed. This reduces the possibility of compression on n. ischiadicus. In the case of lesion of gluteus superior and its “escape” into the pelvis, the lateral position of the patient allows access to the anterolateral aspects of the anterior abdominal wall and retroperitoneal space where a.ilaica internal is identified and its terminal branch, that is, a. glutea superior, is ligated. At this unexpected surgical problem, the approach can be applied without moving the patient. The usage of Kocher-Langenbeck approach when the patient is laid on his stomach makes the force of gravity “pulls” muscles into the operative field. This produces the need for greater uncontrolled force on Homan’s hooks to move a muscle mass and enable good visibility of the posterior pillar or acetabulum wall. With a desire to display the operative field, an assistant may oversee that the pressure of Homan’s hook may lesion n. ischiadicus and et n. gluteus superior, despite the fact that the operated leg is bent in a knee. This position allows easier reposition of the bone fragments and to maintain the reposition. The need for Ollier’s approach or retroperitoneal approach requires displacement of the patient in the lateral position.
In the case of 2 patients, due to poor assessment and previously applied Kocher-Langenbeck approach, the same needed to be transformed into the Ollier’s approach. Acetabulum fracture was primarily treated surgically using the Ollier’s approach. Controversy is also raised when it comes to the choice of approach in the management of anterior acetabular wall / column. Some authors prefer Emil Letournel’s approach and others Keel’s or Smith- Peterson’s approach.
Extended Smith- Peterson’s approach has been used 4 times, and Emile Letournel’s approach 14 times. Chi-square test confirmed a statistically significant difference in the management of the anterior wall/column in favor of Smith-Peterson’s approach in relation to Emile Letournal approach (p <0.01). Since 2007, according to the classification of Judet and Letournel, the complex types of fractures (usually joint fractures of the anterior and posterior column), have been handled in two acts. Usually the fourth day after the admission, the anterior column was handled surgically using the Emile Letournel’s approach. In order to stabilize the fracture, original AO plates and screws were used. It was technically easier to manage the anterior wall / column first, whiles the posterior wall / column was unstable and mobile. Upon the stabilization of the general condition averagely eight days later, posterior column was managed using the Kocher-Langenbeck approach. 14 patients, aged 36.2 years, were treated in such manner. Traffic trauma was present in 12 patients (85%) and all of them were polytraumatized.
Upon the admission to the clinic it is obligatory to ordinate medicamental thromboembolic prophylaxis. Mechanical thromboembolic prophylaxis, elastic bandages, breathing exercises and physical therapy procedures were used since the first postoperative day. Graduated compression stockings were not used. Antiplatelet therapy Andol 100 as well as Indametacin was used in home treatment for about a month.
3. RESULTS
Patients underwent anamnestic, clinical and radiographic analysis. Average duration of the follow-up was 18 months (9 to 35). Harris Hip Score was used for the assessment of the condition of the hip, while standard radiographic images, CT and 3D reconstruction were used for the assessment of post-traumatic arthrosis and the occurrence of avascular necrosis. During the treatment of patients who were treated with traction, 3 patients suffered from the emergence of decubitus and skin dehiscence over the gluteal region, while the heel was affected in 7 patients. Transient infections around the pins occurred in 4 patients, and respiratory complications in 2 patients. For the prevention of skin decubitus, we used static exercise during bed rest and we placed ring shaped cotton under the heel. Iatrogenic complication of Kocher-Langebeck approach was on lesion of circumflexae superior when a. iliaca interna needed to be accessed in order for it to be liasoned. Postoperatively, tansitoral paresis of n. ischiadicus occurred in 4 patients. The most severe complications of Kocher- Langebeck approach occurred in one patient as a result of Homan’s hooks’ pressure on peritoneum, whereupon a rectal contusion, that is, rectal dehiscence occurred. Due to insufficient diagnosis, anus praeter needed to be done 10 days afterwards. One patient had a retroperitoneal hematoma, which was solved by making an incision and drainage. Incongruent and unstable reposition of the posterior acetabular column occurred in 3 patients, which led to subluxation of the hip joint, accompanied by pain and avascular necrosis of the femoral head. Averagely, 2.5 months after the surgical treatment of acetabular, the complication was eliminated with cementless total hip prosthesis. Pulmonary embolism was identified and diagnosed on the third postoperative day, on average–clinically and radiographically in 5 patients, and clinically and PE scintigraphy (perfusion and inhalation) in 2 patients. Functional outcome (after 18 months of follow-up) according to the Harris hip score of surgical treatment of 82 patients was as follows: good in 36 patients (43.90%), satisfactory in 32 (39.03%) and poor in 14 patients (17.07%). Results of acetabulum fractures treated with traction were as follows: good, in 8 patients (57%), satisfactory in 4 (28%), poor in 2 patients (15%) (Figure 2). Chi-square test showed that there was no statistically significant difference between patients treated surgically or conservatively (p = 0.659).
Figure 2.
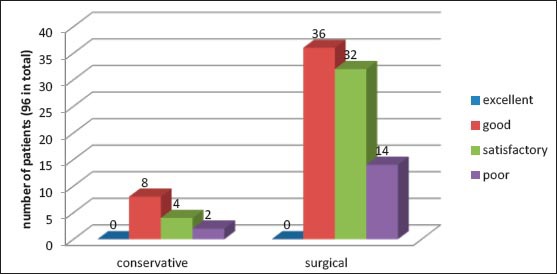
Results of conservative and surgical treatment of acetabulum fractures by Harris hip score after 18 months of follow-up
Periarticular heterotrophic calcifications according to the Brook’s classification of heterotopic ossification after surgically treated patients were as follows: 0° in 65 patients (79%); I-II° in 9 (11%), III-IV° in 8 patients (10%). In 14 patients treated with traction of heterotopic ossifications according to the Brook’s classification, periarticular heterotrophic calcifications were as follows: 0° in 10 patients (72%), I-II° in 3 patients (22%) and III- IV° in 1 patient (6%). Chi-square test showed that there was no statistically significant difference in heterotopic ossification in patients treated operatively or non-operatively (p = 0.346).
4. DISCUSSION
From 1980 to 2007, Ferguson presented radiological and epidemiological studies on acetabular fractures in patients aged over 60 years. The series included 1309 patients. Fractures were reported more frequently in poor people exposed to physical effort (3). The study showed that the fracture was characterized by a shift of the anterior column, more frequently in the elderly when compared to younger patients. Impacted fracture of the acetabular roof was present in 40% of cases, and impacted anterior wall / column was represented in 38% (3). When compared to younger patients, the percentage of elderly patients with acetabular fractures increased during the 27-year-old researches with different distributions of fractures (3). In a study by 1152 patients, during the treatment of traumatic arthritis with arthroplasty and anterior approach, the authors came to the following conclusion: the low percentage of dislocation, earlier return of functions and reduced intra- and postoperative complications (4).
In treatment of acetabular fracture, the following controversy is raised: whether to primarily perform the hip arthrodesis due to fractures? In my series, I have always strive to do a restitution of the acetabulum. Acetabulum repaired, even incongruent one, provides good support and stability to hip arthroplasty. It is still a great controversy in orthopedic surgery to do a hip replacement after arthrodesis is done. In a series by 151 patients who had hemodynamic instability, an unstable pelvic fracture was accompanied by acetabular fractures. The pelvis was primarily treated with external fixation (2). Dynamic stability was clinically achieved by placing an external fixator. Radiographically, despite the improvement of arcus pubis (symphysis pubis), 64% of patients had an aggravation of posterior diastase (sacroiliac joint) (5). Finding of “external fixator deformity” in 73% of cases, which is diagnosed with an emergence of increasing flexion or internal rotation of the hemipelvis (5), is characteristic. During his 10-year-old experience, JM Matta has stated that surgical treatment of acetabulum fracture through ilioinguinal approach provides excellent results obtained with surgical treatment in 119 (33%) out of the 373 acetabular fractures. The following fractures were managed with the ilioinguinal approach: anterior wall or column, the anterior column associated with transverse fractures as well as columns with transverse fractures (6). Matta also indicates some complications: wound infection 3%, iatrogenic nerve injury 2%, death from pulmonary embolism 1%. After one year, clinical postoperative results were as follows: excellent in 37% of patients, good in 47%, satisfactory in 14% and poor in 2% of patients. Two patients underwent arthroplasty due to post-traumatic arthritis (6). From March, 1991 to December, 1992, Cole JD and Bolhofner BR surgically treated 55 acetabular fractures using the ilioinguinal approach (8). The approach provides an excellent visualization of the pelvic ring. Patients were followed for 17.7 months on average (8). The fracture was repaired 6-12 weeks after surgery. Radiographic marks were as follows: excellent in 64% of patients, good in 25%, satisfactory in 7% and poor in 4% of patients. The following complications were stated: transient failure of n. femoral vein in 2 patients, one infection, and one inguinal hernia (8). The established reposition was lost in one patient. In the first year of life, six patients reported post-traumatic arthritis. Heterotopic ossification was not statistically significant (4). Clinical results for this sample were as follows: excellent in 47% of patients, good in 42%, satisfactory in 9%, and poor in 2% of patients. In acetabular fractures controversy is raised by a dilemma whether to primary solve the fracture with endoprosthesis. In the study, the authors stated that he primarily used osteosynthesis when treating acetabular fractures in patients aged over 70 years, and simultaneously, he embedded total cement prosthesis. They had 8% of revisions. Averagely one year later, 21 % of the patients who were primarily treated only with acetabular osteosynthesis needed endoprothesis as well (7).
Letournel et al. presented their experiences in the treatment of 195 acetabular fractures using the ilioinguinal approach in 178 cases (90%), and in 17 cases (10%), using a combination of Kocher- Langenbeck approach, as a double cut. 39 simple and 156 complex cases of acetabular fractures were surgically treated. In 39 cases of complex fractures, the fracture of anterior column and transversum occurred, while in 98 patients, the fracture of anterior and posterior wall occurred (9). Incongruence of acetabular fractures through the ilioinguinal approach was perfect in 85% of cases. The complication rate was extremely low, with no evidence of external iliac heterotrophic ossification (9).
In the study from 1990 to 2006, Saveski J. (11) treated 236 patients with acetabular fractures (10). According to the Letournel’s classification, in 86 patients (36, 4%), simple acetabular fractures were represented, and 150 patients (63.6%) had a complex fracture (10). Clinical results according to d’Aubigné were as follows: excellent in 90 patients (38%), good in 80 (34%), satisfactory in 38 (16%) and poor in 28 (12%) patients (7). Heterotopic ossification according to the Brook’s classification occurred in 21 patients (9%) (10).
Starcevic et al. presented a series of 39 patients with an average follow-up of 28 months. Six months after the surgery, Harris Hip Score was 82, and after 12 months, it was 91 (11). In another study, Mladenovic et al.(12) presented a treatment of 29 patients with acetabular fractures, of which 17 patients had an elementary fracture, and 12 of them, a complex one (12). Excellent result was achieved in 9 patients, good in 11 (37%), satisfactory in 4 (14%) and poor in 5 patients (17 %).
5. CONCLUSION
Acetabulum fractures carry a high degree of risk for the occurrence of: venous thromboembolism and fat embolism, and therefore it are necessary to begin treatment immediately, as well as to include thromboembolic prophylaxis. Patient’s age and possible existing chronic diseases hold a great significance in the choice of treatment.
Conservative treatment is acceptable when the dislocation of fragments is less than 5 mm. The indications for surgical treatment are incongruent or unstable fractures with a dislocation verified to be greater than 5 mm, as well as radiography, performed and measured by JM Matta, that shows incongruence between the femoral head and the supporting columns, where the acetabular roof is less than 40° in all planes. The method of surgical approach for the management of posterior pillar or wall is the Kocher-Langenbeck approach. However, when it comes to the management of the anterior wall or pillar, E. Letournel’s approach is used. Smith-Peterson’s approach may be used if the front pillar does not exceed Pectineal line. Stable internal fixation is achieved by the original plates and 3.5 mm cortical screws. Stable osteosynthesis does not require postoperative traction and allows earlier physical rehabilitation. As a prevention of heterotopic ossification, indomethacin therapy is given for a month. The experience of the surgical team is a crucial factor in the treatment of acetabular injuries.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Giannoudis PV, Grotz MRW, Papakostidis C, Dinopoulos H. Operative treatment of displaced fractures of the acetabulum. Ameta-analysis. J Bone Joint Surg Br. 2005;87:2–9. [PubMed] [Google Scholar]
- 2.Kakar R, Sharma H, Al Lcock P, Sharma P. Occult acetabular fractures in elderly patients: a report of three cases. Jurnal of Othopedic Surgery. 2007;15(2):242–244. doi: 10.1177/230949900701500225. [DOI] [PubMed] [Google Scholar]
- 3.Ferguson TA, Patel R, Bhandari M, Matta JM. Fractures of the acetabulum in patients aged 60 years and older: An Epidemiological and Radiological Study. Bone Joint Surgery Br. 2010 Feb;92(2):250–257. doi: 10.1302/0301-620X.92B2.22488. [DOI] [PubMed] [Google Scholar]
- 4.Kaempffe FA, Bone LB, Border JR. Open reduction and internal fixation of acetabular fractures: heterotopic ossification and other complications of treatment. J Orthop Trauma. 1991;5:439–445. doi: 10.1097/00005131-199112000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Sprague S, Matta JM, Bhandari M. Anterior Total Hip Arthroplasty Collaborative (ATHAC) Investigators, Dodgin D, Clark CR, Kregor P, Bradley G, Little L. Multicenter collaboration in observational research: improving generalizability and efficiency. J Bone Join Surgery Am. 2009 May;91(Suppl 3):80–86. doi: 10.2106/JBJS.H.01623. [DOI] [PubMed] [Google Scholar]
- 6.Matta JM. Operative treatment of acetabular fractures through the ilioinguinal approach: a 10-year perspective. J. Bone Join Surgery Am. 2009 Jun;129(6):719–727. [Google Scholar]
- 7.Borrelli J, Jr, Goldfarb C, Ricci W, Wagner JM, Engsberg JR. Functional outcome after isolated acetabular fractures. J Orthop Trauma. 2002;16(2):73–81. doi: 10.1097/00005131-200202000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Cole JD, Bolhofner BR. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach. Description of operative technique and preliminary treatment results. J Orthoped. Trama. 2007 Oct;21(9):647–656. [PubMed] [Google Scholar]
- 9.Letournel E, Robert J, Reginald AE. Springer T; 1997. Fractures Of The Acetabulum. [Google Scholar]
- 10.Saveski J. The first congress of orthopaedic surgeons and traumatologists of Serbia with international participation, Belgrade 25-26 September, Collection of papers; 2008. Surgical treatment of acetabular fractures; p. 120. [Google Scholar]
- 11.Starčević B, Lešić A, Damjanović G, Milošević I, Milemković M, Ilić M, et al. The first congress of orthopaedic surgeons and traumatologists of Serbia with international participation, Belgrade 25-26 September, Collection of papers; 2008. Prelomi acetabuluma- preliminarni rezultati operativnog liječenja; p. 120. [Google Scholar]
- 12.Mladenović D, Mitković M, Micić I, Milenković S, Karalejić S, Stojiljković P, et al. The first congressoforthopaedicsurgeonsandtraumatologists of Serbia with international participation, Belgrade 25-26 September, Collection of paper; 2008. Prelomi acetabuluma i hirurško liječenje; p. 12. [Google Scholar]


