Abstract
Background
In Uganda and elsewhere, the private sector provides an increasing and significant proportion of maternal and child health services. However, little is known whether private care results in better quality services and improved outcomes compared to the public sector, especially regarding care at the time of birth.
Objective
To describe the characteristics of care-seekers and assess newborn care practices and services received at public and private facilities in rural eastern Uganda.
Design
Within a community-based maternal and newborn care intervention with health systems strengthening, we collected data from mothers with infants at baseline and endline using a structured questionnaire. Descriptive, bivariate, and multivariate data analysis comparing nine newborn care practices and three composite newborn care indicators among private and public health facilities was conducted.
Results
The proportion of women giving birth at private facilities decreased from 25% at baseline to 17% at endline, whereas overall facility births increased. Private health facilities did not perform significantly better than public health facilities in terms of coverage of any essential newborn care interventions, and babies were more likely to receive thermal care practices in public facilities compared to private (68% compared to 60%, p=0.007). Babies born at public health facilities received an average of 7.0 essential newborn care interventions compared to 6.2 at private facilities (p<0.001). Women delivering in private facilities were more likely to have higher parity, lower socio-economic status, less education, to seek antenatal care later in pregnancy, and to have a normal delivery compared to women delivering in public facilities.
Conclusions
In this setting, private health facilities serve a vulnerable population and provide access to service for those who might not otherwise have it. However, provision of essential newborn care practices was slightly lower in private compared to public facilities, calling for quality improvement in both private and public sector facilities, and a greater emphasis on tracking access to and quality of care in private sector facilities.
Keywords: newborn health, private health care, public health care, essential newborn care, Uganda
Newborn mortality (deaths within the first 28 days of life) remains unacceptably high in sub-Saharan Africa and in Uganda. Every year 2.9 million babies die during the neonatal period (1), with the majority of these deaths occurring in the first week of life. This is also the time of greatest risk for stillbirths and maternal deaths (2). In Uganda, out of 1.5 million births in 2012, 82,000 resulted in a mother or baby dying (3). There are many missed opportunities to improve care and increase the potential to save lives at and immediately after birth. Saving mothers and babies is rarely the result of a single, simple intervention, but a complex and comprehensive set of interlinked services and practices supported by health workers.
Skilled attendance at birth is considered a critically important platform to reduce the burden of maternal and newborn mortality worldwide (4, 5). If backed by a referral level providing comprehensive emergency obstetric care, uptake of skilled attendance will prevent by far the largest part of maternal and newborn mortality as well as many stillbirths (2). However, skilled attendance will only have the promised effect if the different components of it are implemented, and thus quality of care is assured (6). Although quality of care is a complex and multidimensional concept including safety, effectiveness, timeliness, efficiency, equity, and patient-centredness (7), measuring signal indicators may provide some insight into the coverage and quality of care overall (8).
Private for-profit providers, typically small privately owned clinics with a single proprietor, play a significant role in provision of outpatient health care and reproductive health, but involvement in maternity care is a relatively recent phenomenon in sub-Saharan Africa, where most women still deliver at home or choose the public health system (9). Still, in some countries such as Nigeria or Kenya, a larger proportion of deliveries are now taking place in private clinics and hospitals (10–13). One of the milestones of the newly launched Every Newborn Action Plan is coordinated support and effort amongst private sector providers of delivery services and newborn care (14).
Engagement of the private sector to increase accessibility to reproductive and child health care is much debated (15). Some studies have reported that greater participation of the private sector improved access to and equity in care (16, 17), whereas others indicated the opposite (18). Criticisms in regard to private maternity care include late referral to public health facilities in the case of obstetric emergencies, as private maternity facilities are not always equipped to provide 24-h emergency obstetric care services (19, 20). Where operative services are available, the fees charged for a caesarean section delivery might increase caesarean section rates, particularly where third-party fee-for-service reimbursement gives health providers an income from their services.
Families often seek out private health facilities as they perceive the quality of care as better overall (21–28), although a recent systematic review suggests that quality in both public and private provider groups is poor, with the private sector being better in terms of drug availability and aspects of responsiveness to client expectations (29). Results from an investigation into the use of private maternity services from a Nairobi informal settlement indicated that private care was less costly, closer to the home, and providers were more empathic (30, 31). In Nigeria, private maternity care was the preferred place of delivery because of the low quality of government facilities, particularly with respect to absence of staff, poor perceived quality, waiting times, and high costs (11).
Despite increasing prominence of the private sector as a provider of delivery and newborn care, there is a dearth of data on newborn care practices in these facilities. To the best of our knowledge, no information on the quality of delivery care of private providers is available from Uganda. As part of the Uganda Newborn Study (UNEST) (32), we engaged public as well as private for-profit and not-for-profit providers through sensitisation, training, and supervision around childbirth and newborn care. UNEST aimed at improving newborn survival through a community-based intervention using home visits by volunteers linked to health facilities. The intervention included a health system strengthening component and improving linkages between the community-based intervention and the health facilities. Here we present the determinants of use and the quality of public and private maternity care. Furthermore, we assessed the impact of facility strengthening on implementation of essential newborn care interventions among births that occurred in private and public health facilities in rural eastern Uganda. This is the sixth paper in a series on the UNEST results.
Methods
Study design and setting
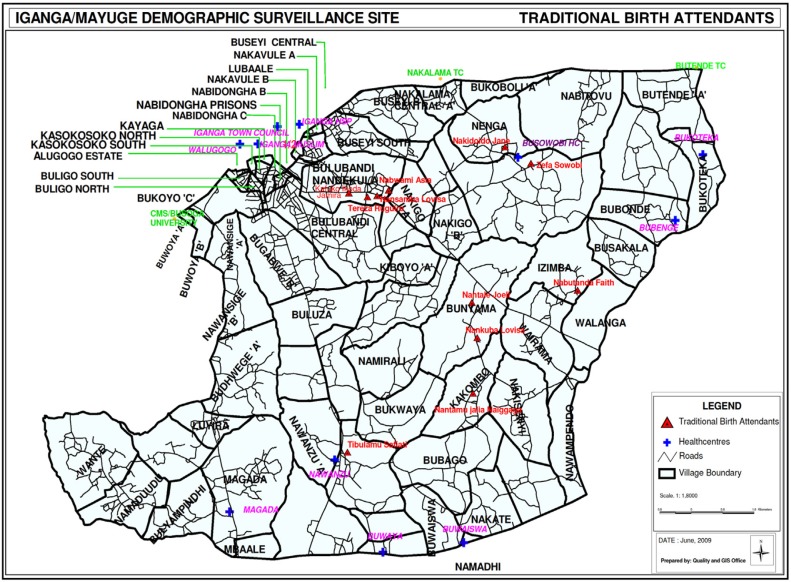
The UNEST design and package has been described elsewhere (32–34). In brief, the study took place in the Iganga-Mayuge Health and Demographic Surveillance Site (HDSS) located in Iganga and Mayuge districts in the eastern region of Uganda, about 120 km east of the capital city of Kampala. The HDSS serves a population size of 70,000 people, at the time of the study, living in 65 villages, with women of reproductive age comprising 23%. The total fertility rate of the HDSS is 4.3. The population is served by 20 facilities including six private facilities (Fig. 1). The public hospital in Iganga is the only comprehensive emergency obstetric care facility. The public facilities charge no fees for services, although there are often informal costs requested of families. Typically, private facilities consisted of a small clinic with less than five staff who could provide essential care for common conditions. Private facilities are more accessible to the population and sometimes to rural areas than public facilities.
Fig. 1.
Map of the UNEST study area.
Villages were randomised to intervention or control arms. Intervention villages had a community health worker who was trained to provide home visits during pregnancy and the first week after delivery, whereas comparison villages received the standard care as delivered by the facilities in the area. Health facility strengthening including training of health workers on essential maternal-newborn care skills and provision of medicine, basic equipment, and supplies was done in all health facilities with a reasonable client load (more than 15–20 per month) for delivery care, independent of ownership and management or whether the facility was located in the intervention or comparison area. Both public and private health facilities were supported by quarterly supervision as part of the health system strengthening. In addition, linkages between community and health facilities were strengthened.
Data collection
A standardised tool was adapted and pretested for data collection. Data collectors were experienced HDSS field staff. The baseline census was done between March and August 2007. Women with infants aged 1–4 months (n=395) in the HDSS were interviewed through visits to all households (35). At endline census, done between August and November 2011, we interviewed all women of childbearing age who had had a live birth in the previous 12 months (n=1,761) (17, 36–38).
Data analysis
All analyses used Stata software version 12.1. Univariate and bivariate analyses were used to describe background characteristics of women who delivered in a health facility. The chi-square test was used to compare the difference between the private and public facilities as place of delivery. A multiple logistical regression model was constructed to identify determinants of private facility births using all of the explanatory variables which were significant at bivariate analysis. We checked for multicollinearity between the independent variables, and only included non-collinear variables in the analysis. For this study the effect of treatment – overall and within subgroups – and covariates were reported using odds ratios (ORs).
Data on nine essential newborn care practices were collected. These interventions included wrapping the baby immediately after birth using a dry cloth, early skin-to-skin placement, delayed bath at least 6 h after delivery, clean instrument used to cut the umbilical cord, clean device used to tie or clamp the cord, placing nothing on the cord stump, breastfeeding within the first hour after birth; not giving the baby a bottle, and not giving any food or drink other than breast milk. Interventions were combined into composite indicators for thermal care, hygienic cord care, and optimal feeding practices. In addition we assessed how many women received more than one to all nine essential newborn care interventions.
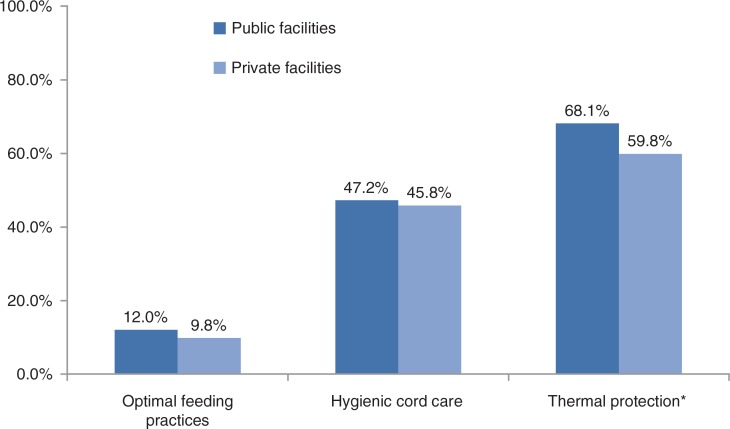
Fig. 2.
Coverage of babies receiving essential newborn care interventions. * χ2prob=0.007
Wealth quintiles were constructed using the Principal Component Analysis based on household assets as used by the Ugandan Bureau of Statistics, including number of sleeping rooms, type of floor material, type of roof material, wall material, type of bed, fuel used for cooking, source of light; and possession of a radio, a sewing machine, an electric flat iron, charcoal flat iron, a bed net, kerosene lamp, kerosene stove, car, tea table, refrigerator, television set, sound stereo, telephone, mattress, wheelbarrow, cell phone, and camera. These gave a Cronbach's alpha of 0.848. Principal component analysis was performed and the first principal component was scored to create an asset index that was used to group all households in the HDSS into wealth quintiles (35). Schooling was assessed using categories of completed education level.
Results
Background characteristics
The average age of the women who delivered in a health facility was 26 years, with no significant difference between private and public sector (Table 1). Nine of 10 mothers were married. Slightly more than half of all women had primary education as the highest level attained, and 9% had no education at all. More than one-third of women (38%) had given birth four or more times. Almost all women (99%) attended at least one antenatal care (ANC) visit and 49% attended four or more times. Less than one-fourth (23.6%) of women attended ANC in their first trimester. The rate of caesarean section was 4.4% overall.
Table 1.
Background characteristics of respondents for endline census
| Total (all facility deliveries) | Private facilities | Public facilities | ||
|---|---|---|---|---|
| Characteristics | N (%) | N (%) | N (%) | p |
| Maternal age (yrs) | n=1,358 | n=299 | n=1,059 | |
| <19 | 96 (7.07) | 16 (5.35) | 80 (7.55) | 0.1797 |
| 19–25 | 564 (41.53) | 120 (40.13) | 444 (41.93) | 0.5770 |
| 26–30 | 357 (26.29) | 79 (26.42) | 278 (26.25) | 0.9530 |
| >30 | 341 (25.11) | 84 (28.09) | 257 (24.27) | 0.1786 |
| Marital status | n=1,369 | n=306 | n=1,063 | |
| Not married | 116 (8.47) | 22 (7.19) | 94 (8.84) | 0.3610 |
| Married | 1,253 (91.53) | 284 (92.81) | 969 (91.16) | 0.3610 |
| Education | n=1,369 | n=306 | n=1,063 | |
| No education | 127 (9.28) | 33 (10.78) | 94 (8.84) | 0.3026 |
| Primary | 783 (57.20) | 198 (64.71) | 585 (55.03) | 0.0026* |
| Secondary | 407 (29.73) | 68 (22.22) | 339 (31.89) | 0.0011* |
| University | 52 (3.80) | 7 (2.29) | 45 (4.23) | 0.1176 |
| Wealth quintile | n=1,036 | n=240 | n=796 | |
| 1 (Poorest) | 154 (14.86) | 46 (19.17) | 108 (13.57) | 0.0326* |
| 2 (Poor) | 219 (21.14) | 52 (21.67) | 167 (20.98) | 0.8185 |
| 3 (Average) | 258 (24.90) | 63 (26.25) | 195 (24.50) | 0.5827 |
| 4 (Rich) | 207 (19.98) | 48 (20.00) | 159 (19.97) | 0.9919 |
| 5 (Richest) | 198 (19.11) | 31 (12.92) | 167 (20.98) | 0.0054* |
| Parity | n=1,369 | n=306 | n=1,063 | |
| 1 | 262 (19.14) | 37 (12.09) | 225 (21.17) | <0.001 |
| 2–4 | 585 (42.73) | 129 (42.16) | 456 (42.90) | 0.8176 |
| >4 | 522 (38.13) | 140 (45.75) | 382 (35.94) | 0.0019* |
| Number of ANC visits | n=1,351 | n=300 | n=1,051 | |
| 1 | 46 (3.40) | 15 (5.00) | 31 (2.95) | 0.0842 |
| 2–3 | 646 (47.82) | 142 (47.33) | 504 (47.95) | 0.8496 |
| >3 | 659 (48.78) | 143 (47.67) | 516 (49.10) | 0.6621 |
| Trimester of first ANC visit | n=1,363 | n=303 | n=1,060 | |
| 1 | 322 (23.62) | 59 (19.47) | 263 (24.81) | 0.0536* |
| 2 | 875 (64.20) | 198 (65.35) | 677 (63.87) | 0.6356 |
| 3 | 166 (12.18) | 46 (15.18) | 120 (11.32) | 0.0700 |
| Mode of delivery | n=1,369 | n=306 | n=1,063 | |
| Spontaneous | 1,307 (95.47) | 303 (99.02) | 1,004 (94.45) | <0.001* |
| Caesarean | 60 (4.38) | 3 (0.98) | 57 (5.36) | 0.001* |
| Other | 2 (0.15) | 0 (0.00) | 2 (0.19) | 0.4454 |
Determinants of births in private facilities
Although there was an overall increase in health facility births, from 69.6% at baseline to 77.8% at endline, there was a decrease in private sector deliveries, from 25.1 to 17.3% overall (Table 2). Of the 1,369 women who delivered in a health facility, 22% gave birth in the private sector. Compared to their counterparts who delivered in public health facilities, women delivering in private facilities were significantly more likely to have higher parity, lower socio-economic status, and less education, and were more likely to seek ANC later in pregnancy. They were also more likely to have a normal delivery, associated with the lack of operative capacity in the majority of the private facilities. There was no significant association between the time when women went into labour and the place that they delivered (results not shown).
Table 2.
Place of delivery
| Baseline | Endline | |||
|---|---|---|---|---|
| n=395 | % | n=1,761 | % | |
| Facility delivery | 275 | 69.6 | 1,369 | 77.7 |
| Public facility | 176 | 44.6 | 1,062 | 60.3 |
| Private facility | 99 | 25.1 | 306 | 17.4 |
| Delivered by traditional birth attendant | 44 | 11.1 | 147 | 8.3 |
| Delivered at home or elsewhere | 110 | 27.8 | 245 | 13.9 |
| Missing | 10 | 2.5 | 0 | 0.0 |
According to the logistical regression analysis (Table 3) women who had two to four previous births compared to those with only one birth were almost twice as likely to deliver in a private health facility (OR 1.86, 95% CI 1.05–3.30). Women with more than four previous births were two times more likely to deliver in a private facility (OR 2.36; 95% confidence interval (CI) 1.34–4.16). In addition, delivery in private health facilities was less likely (although non-significantly so) for mothers of higher wealth quintiles (OR 0.58, CI 0.33–1.02). The odds of women who delivered in private facilities having a caesarean section was 80% lower than in those who delivered in public facilities (OR 0.20, 95% CI 0.48–0.86).
Table 3.
Determinants of births in private health facilities
| Variable | Univariate unadjusted | Multivariate unadjusted | ||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Parity | ||||
| 1 | 1 | 1 | ||
| 2–4 | 1.72 | 1.15–2.56 | 1.72 | 1.06–2.81 |
| >4 | 2.22 | 1.50–3.32 | 2.01 | 1.22–3.31 |
| Wealth quintile | ||||
| 1 (Poorest) | 1 | |||
| 2 (Poor) | 0.73 | 0.46–1.16 | 0.75 | 0.46–1.21 |
| 3 (Average) | 0.76 | 0.49–1.19 | 0.75 | 0.48–1.19 |
| 4 (Rich) | 0.71 | 0.44–1.14 | 0.75 | 0.46–1.22 |
| 5 (Richest) | 0.44 | 0.26–0.73 | 0.52 | 0.30–0.90 |
| Education level | ||||
| No education | 1 | |||
| Primary | 0.96 | 0.63–1.48 | 1.08 | 0.67–1.76 |
| Secondary or higher | 0.56 | 0.35–0.89 | 0.93 | 0.53–1.66 |
| Trimester of first ANC visit | ||||
| 1 | 1 | |||
| 2 | 1.30 | 0.94–1.80 | 1.31 | 0.89–1.92 |
| 3 | 1.71 | 1.10–2.66 | 1.77 | 1.07–2.95 |
| Mode of delivery | ||||
| Normal | 1 | |||
| Caesarean | 0.17 | 0.05–0.56 | 0.20 | 0.48–0.84 |
Coverage of essential newborn care practices by place of birth
Amongst all facility births, coverage of essential newborn care practices varied from a low of 58.6% of women practicing dry cord care to 94.8% use of a clean instrument to clamp or tie the umbilical cord. However, the composite indicators of babies receiving all basic essential interventions were much lower, range being 11.5% optimal feeding practices, 46.9% hygienic cord care, and 66.3% receiving thermal protection overall. With the exception of immediate breastfeeding, the coverage of individual essential newborn care practices was higher but not significantly different in public sector facilities compared to private facilities (Table 4). Similarly, the composite essential newborn care indicators of optimal feeding practices, hygienic cord care, and thermal protection were all higher in public facilities, with thermal care practices significantly higher at 68.1% coverage in public sector facilities compared to 59.8% in private facilities (Fig. 2).
Table 4.
Reported neonatal care practices by place of delivery
| Public health facilities | Private health facilities | ||
|---|---|---|---|
| Practices | N (%) | N (%) | p |
| Clean instrument used to cut the cord | n=1,063 | n=306 | |
| 883 (83.07) | 252 (82.35) | 0.7681 | |
| Clean instrument used to tie or clamp the cord | n=1,063 | n=306 | |
| 1,014 (95.39) | 285 (93.14) | 0.1153 | |
| Dry cord care | n=1,062 | n=304 | |
| 631 (59.42) | 170 (55.92) | 0.2733 | |
| Breastfed within first hour | n=1,063 | n=306 | |
| 734 (69.05) | 218 (71.24) | 0.4633 | |
| Baby fed by breast only (no bottle) | n=1,063 | n=306 | |
| 1,026 (96.52) | 300 (98.04) | 0.1791 | |
| Exclusive breastfeeding in the first month | n=1,063 | n=305 | |
| 862 (81.09) | 247 (80.98) | 0.9655 | |
| Baby wrapped after delivery with dry cloth | n=1,063 | n=306 | |
| 1,060 (99.72) | 304 (99.35) | 0.3428 | |
| Baby placed skin-to-skin | n=1,063 | n=306 | |
| 821 (77.23) | 218 (71.24) | 0.0309* | |
| First bath delayed >6 h | n=1,055 | n=302 | |
| 920 (87.20) | 255 (84.44) | 0.2146 | |
| Hygienic cord care | n=1,063 | n=306 | |
| Clean instrument used to cut cord; clean instrument used to tie cord; nothing placed on cord | 502(47.22) | 140(45.75) | 0.6498 |
| Thermal protection | n=1,063 | n=306 | |
| Baby wrapped after delivery with dry cloth; placed skin-to-skin; bath delayed >6 h | 724 (68.11) | 183 (59.80) | 0.0067* |
| Optimal feeding practices | n=1,063 | n=306 | |
| Baby breastfed within first hour; no bottle used; exclusive breastfeeding for the first month | 128 (12.04) | 30 (9.80) | 0.2798 |
Babies born in public health facilities were more likely to receive more individual newborn care practices compared to their private health facility counterparts. Whereas 42.8% of babies born in public facilities received at least eight essential newborn care practices, only 27.5% in private facilities received the same number. Nearly all (98%) babies born in public health facilities received at least three practices, compared to 95% amongst those in private health facilities (Table 5).
Table 5.
Number and distribution of essential newborn care interventions by place of delivery (%)
| Number of newborn care interventions received | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 0 | Mean (SD) | |
| Private facility | 8.5 | 27.4 | 46.8 | 68.8 | 81.0 | 89.5 | 95.1 | 98.2 | 99.5 | 100.0 | 6.16 (1.92) |
| Public facility | 16.4 | 42.8 | 67.8 | 82.9 | 92.4 | 96.6 | 98.4 | 99.5 | 99.8 | 100.0 | 7.04 (1.59) |
| p | <0.001* | ||||||||||
Interventions include: Wrapping the baby using a dry cloth; early skin-to-skin placement; delayed bath at least 6 h after delivery; clean instrument used to cut the umbilical cord; clean device used to tie or clamp the cord; placing nothing on the cord stump; breastfeeding within the first hour after birth; no use of bottle; not giving any food or drink other than breast milk for the first month.
Discussion
To our knowledge this is the first study to compare the difference in newborn care practices between private and public health facilities in Uganda. We found that there is little difference in newborn care practices in private and public facilities. Private facilities are more likely to be accessed by the poorest families and at-risk women. After health system strengthening, including health worker training, provision of essential supplies, and supervision in both public and private sectors, there was an overall increase in health facility births. During the same period we observed a decline in private sector deliveries.
The increase in facility deliveries in public facilities suggests that the health system strengthening activities had a positive impact on utilisation. Although we cannot make a causal interference as the study is based on two subsequent cross-sectional surveys without any comparison area, the temporal relationship gives some indication that such an association might exist. No other intervention which might confound the association was ongoing in the study area. As the place of delivery is likely to be an indicator which is easily remembered, we do not think that the difference in recall period (4 months at baseline and 12 months at endline) may bias the results; in most surveys recall periods of one year or more are used (39).
Thus, we think that it is likely that the combined supply- and demand-side interventions in UNEST resulted in perceived or real improvements in care, including public sector health workers being more receptive and responsive to clients. Possibly the intervention could have influenced perceived quality of and access to public sector services.
These findings have public health implications for Uganda, and also for other low- and middle-income countries looking to strengthen care at the time of birth.
In this setting, women who delivered at private health facilities had a higher-risk birth profile compared to women who sought care at public facilities. Women who gave birth in private facilities were associated with lower socio-economic status, higher parity, lower education, and were more likely to attend ANC later in pregnancy. Private facility-based delivery care in sub-Saharan Africa is typically associated with the urban rich and more educated segment of the population. However, in our experience, this is only true for the more advanced private health units, not for the majority of private units in rural areas, that are often small and designed to serve the poor.
The use of a private health facility, however, bears the risks of potentially catastrophic costs associated with obstetric care (40, 41), making the pattern of private sector care seeking amongst poorer families potentially harmful. However, a similar pattern as observed in our study in rural Uganda has also been described in Nairobi's informal settlements (31). A plausible explanation could lie in the fact that public health facilities are more distant whereas private care providers are strategically placed to maximise access and to fill a demand gap, especially in more rural areas. In addition, informal payments – which are common in the public sector in Uganda – might have led families to make a rational choice to save on transport costs but pay more for the delivery care (42, 43).
Private health care was not found to be synonymous with better capacity and quality. The private health facilities in the study setting had less capacity in terms of infrastructure, staffing, equipment, and medicines (32). The lack of emergency obstetric services at private health facilities and referral delays pose a real risk to the survival and health of mothers and babies. Through UNEST, private as well as government health facilities were targeted for health system strengthening, with the knowledge that the private ones are often overlooked by development partners and districts in capacity-building efforts such as dissemination of service guidelines; in-service training; provision of equipment, drugs, and supplies; and supervision and mentorship. Although public health facilities performed on par with private health facilities across almost all newborn care practices, coverage overall was not optimal, especially in the case of early and exclusive breastfeeding. These essential newborn care practices are inexpensive and require little if any technology and commodities. The low coverage represents a missed opportunity for all births, regardless of place of delivery.
More information is needed to understand the patterns of care seeking in the public and private sector. There are few disaggregated data available in terms of utilisation as the main source of population-based data, the Demographic and Health Surveys, combines private for-profit and private not-for-profit facilities together, obscuring this potentially important distinction in healthcare provision (9).
This study has some limitations. Newborn care practices were assessed by asking the mother about the care she had received or provided to her newborn. Such responses are subject to recall bias, as some women might not remember interventions implemented during or immediately after birth, particularly for complicated deliveries. However, it can be assumed that such recall bias is similar in women receiving care from a public or private provider. Restricting survey respondents to women who had live births may limit understanding of the potentially different profile of care received by women who experienced stillbirths or early pregnancy loss. However, it was not considered appropriate or feasible to interview such women due to the sensitive nature of their experience. The study did not assess the capacity of private or government health facilities to provide essential newborn care, such as the availability of staff, training received on newborn care, or availability of equipment and supplies. Observation studies would have provided more accurate data, but they consume much time and resources.
Conclusion
As countries increase attention on improving coverage and quality of maternal and newborn care, and in the context of the post-Millennium Development Goal agenda focusing on universal health care, it is important to also consider the role of private sector providers, especially those in rural and urban poor areas which serve under-reached, vulnerable populations. Financial, geographic, and sociocultural barriers to accessing public sector care should be further explored. As for the public facilities, the private sector also requires accountability mechanisms and capacity-building activities, including training and supervision support and guidance on evidence-based best practices for newborn care.
Acknowledgements
We thank all participants, data collectors, data enterers, and researchers involved in the Uganda Newborn Study (UNEST).
This paper is part of the Special Issue: Newborn health in Uganda. More papers from this issue can be found at http://www.globalhealthaction.net
Disclaimer
The contents of the publication are solely the responsibility of the authors and do not necessarily reflect the views of Sida/SAREC, Save the Children, the Bill & Melinda Gates Foundation, or any of the authors’ institutions of affiliation.
Conflict of interest and funding
This study was supported by the Sida/SAREC-Makerere University-Karolinska Institutet Research collaboration as well as by funds provided by Save the Children through a grant from the Bill & Melinda Gates Foundation. This supplement was funded by Save the Children's Saving Newborn Lives programme through a grant from the Bill & Melinda Gates Foundation.
References
- 1.UN Inter-agency Group for Child Mortality Estimations. Estimates developed by the UN Inter-agency Group for Child Mortality Estimation. New York: UN IGME; 2013. Levels and trends in child mortality. [Google Scholar]
- 2.Pattinson R, Kerber K, Buchmann E, Friberg IK, Belizan M, Lansky S, et al. Stillbirths: how can health systems deliver for mothers and babies? Lancet. 2011;377:1610–23. doi: 10.1016/S0140-6736(10)62306-9. [DOI] [PubMed] [Google Scholar]
- 3.Mbonye AK, Sentongo M, Mukasa GK, Byaruhanga R, Sentumbwe-Mugisa O, Waiswa P, et al. Newborn survival in Uganda: a decade of change and future implications. Health Policy Plan. 2012;27:iii104–17. doi: 10.1093/heapol/czs045. [DOI] [PubMed] [Google Scholar]
- 4.Campbell O, Graham W. The Lancet Maternal Survival Series steering group. Strategies for reducing maternal mortality: getting on with what works. Lancet. 2006;368:1284–99. doi: 10.1016/S0140-6736(06)69381-1. [DOI] [PubMed] [Google Scholar]
- 5.WHO. A joint WHO/UNFPA/UNICEF/World Bank statement. Geneva: WHO; 1999. Reduction of maternal mortality. [Google Scholar]
- 6.Graham WJ, Varghese B. Quality, quality. quality: gaps in the continuum of care. Lancet. 2011;379:e5–6. doi: 10.1016/S0140-6736(10)62267-2. [DOI] [PubMed] [Google Scholar]
- 7.Institute of Medicine. Crossing the chasm: the IOM Health Care Quality Initiative. Available from: http://www.iom.edu/Global/News Announcements/Crossing-the-Quality-Chasm-The-IOM-Health-Care-Quality-Initiative.aspx [cited 12 January 2015]. [Google Scholar]
- 8.Gabrysch S, Civitelli G, Edmond KM, Mathai M, Ali M, Bhutta ZA, et al. New signal functions to measure the ability of health facilities to provide routine and emergency newborn care. PLoS Med. 2012;9:e1001340. doi: 10.1371/journal.pmed.1001340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nguyen H, Snider J, Ravishankar N, Magvanjav O. Assessing public and private sector contributions in reproductive health financing and utilization for six sub-Saharan African countries. Reprod Health Matters. 2011;19:62–74. doi: 10.1016/S0968-8080(11)37561-1. [DOI] [PubMed] [Google Scholar]
- 10.Okonkwo J, Ibeh C. The contribution of privately owned hospitals in the provision of essential obstetric care in Nigeria. Niger J Clin Pract. 2006;9:159–63. [PubMed] [Google Scholar]
- 11.Osubor K, Fatusi A, Chiwuzie J. Maternal health-seeking behavior and associated factors in a rural Nigerian community. Matern Child Health J. 2006;10:159–69. doi: 10.1007/s10995-005-0037-z. [DOI] [PubMed] [Google Scholar]
- 12.Limwattananon S, Tangcharoensathien V, Sirilak S. Trends and inequities in where women delivered their babies in 25 low-income countries: evidence from demographic and health surveys. Reprod Health Matters. 2011;19:75–85. doi: 10.1016/S0968-8080(11)37564-7. [DOI] [PubMed] [Google Scholar]
- 13.Peters DH, Mirchandani GG, Hansen PM. Strategies for engaging the private sector in sexual and reproductive health: how effective are they? Health Policy Plann. 2004;19:i5–21. doi: 10.1093/heapol/czh041. [DOI] [PubMed] [Google Scholar]
- 14.Mason E, McDougall L, Lawn JE, Gupta A, Claeson M, Pillay Y, et al. From evidence to action to deliver a healthy start for the next generation. Lancet. 2014;384:455–67. doi: 10.1016/S0140-6736(14)60750-9. [DOI] [PubMed] [Google Scholar]
- 15.Berer M. Privatisation in health systems in developing countries: what's in a name? Reprod Health Matters. 2011;19:4–9. doi: 10.1016/S0968-8080(11)37565-9. [DOI] [PubMed] [Google Scholar]
- 16.Yoong J, Burger N, Spreng C, Sood N. Private sector participation and health system performance in sub-Saharan Africa. PLoS One. 2010;5:e13243. doi: 10.1371/journal.pone.0013243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brugha R, Pritze-Aliassime S. Promoting safe motherhood through the private sector in low- and middle-income countries. Bull World Health Organ. 2003;81:616–23. [PMC free article] [PubMed] [Google Scholar]
- 18.Hotchkiss D, Godha D, Do M. Effect of an expansion in private sector provision of contraceptive supplies on horizontal inequity in modern contraceptive use: evidence from Africa and Asia. Int J Equity Health. 2011;1:33. doi: 10.1186/1475-9276-10-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Almerie Y, Almerie M, Matar H, Shahrour Y, Al Chamat A, Abdulsalam A. Obstetric near-miss and maternal mortality in maternity university hospital, Damascus, Syria: a retrospective study. BMC Pregnancy Childbirth. 2010;10:65. doi: 10.1186/1471-2393-10-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Adisasmita A, Deviany P, Nandiaty F, Stanton C, Ronsmans C. Obstetric near miss and deaths in public and private hospitals in Indonesia. BMC Pregnancy Childbirth. 2008;8:10. doi: 10.1186/1471-2393-8-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kallander K, Kadobera D, Williams TN, Nielsen RT, Yevoo L, Mutebi A, et al. Social autopsy: INDEPTH network experiences of utility, process, practices, and challenges in investigating causes and contributors to mortality. Popul Health Metr. 2011;9:44. doi: 10.1186/1478-7954-9-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Waiswa P, Kallander K, Peterson S, Tomson G, Pariyo GW. Using the three delays model to understand why newborn babies die in eastern Uganda. Trop Med Int Health. 2010;15:964–72. doi: 10.1111/j.1365-3156.2010.02557.x. [DOI] [PubMed] [Google Scholar]
- 23.Kallander K, Hildenwall H, Waiswa P, Galiwango E, Peterson S, Pariyo G. Delayed care seeking for fatal pneumonia in children aged under five years in Uganda: a case-series study. Bull World Health Organ. 2008;86:332–8. doi: 10.2471/BLT.07.049353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kalyango JN, Alfven T, Peterson S, Mugenyi K, Karamagi C, Rutebemberwa E. Integrated community case management of malaria and pneumonia increases prompt and appropriate treatment for pneumonia symptoms in children under five years in eastern Uganda. Malar J. 2013;12:340. doi: 10.1186/1475-2875-12-340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kalyango JN, Rutebemberwa E, Karamagi C, Mworozi E, Ssali S, Alfven T, et al. High adherence to antimalarials and antibiotics under integrated community case management of illness in children less than five years in eastern Uganda. PLoS One. 2013;8:e60481. doi: 10.1371/journal.pone.0060481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rutebemberwa E, Nsabagasani X, Pariyo G, Tomson G, Peterson S, Kallander K. Use of drugs, perceived drug efficacy and preferred providers for febrile children: implications for home management of fever. Malar J. 2009;8:131. doi: 10.1186/1475-2875-8-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rutebemberwa E, Pariyo G, Peterson S, Tomson G, Kallander K. Utilization of public or private health care providers by febrile children after user fee removal in Uganda. Malar J. 2009;8:45. doi: 10.1186/1475-2875-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rutebemberwa E, Kallander K, Tomson G, Peterson S, Pariyo G. Determinants of delay in care-seeking for febrile children in eastern Uganda. Trop Med Int Health. 2009;14:472–9. doi: 10.1111/j.1365-3156.2009.02237.x. [DOI] [PubMed] [Google Scholar]
- 29.Berendes S, Heywood P, Oliver S, Garner P. Quality of private and public ambulatory health care in low and middle income countries: systematic review of comparative studies. PLoS Med. 2011;8:e1000433. doi: 10.1371/journal.pmed.1000433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bazant ES, Koenig MA. Women's satisfaction with delivery care in Nairobi's informal settlements. Int J Qual Health Care. 2009;21:79–86. doi: 10.1093/intqhc/mzn058. [DOI] [PubMed] [Google Scholar]
- 31.Bazant ES, Koenig MA, Fotso J-C, Mills S. Women's use of private and government health facilities for childbirth in Nairobi's informal settlements. Stud Fam Plann. 2009;40:39–50. doi: 10.1111/j.1728-4465.2009.00185.x. [DOI] [PubMed] [Google Scholar]
- 32.Waiswa P, Pariyo G, Kallander K, Akuze J, Namazzi G, Ekirapa-Kiracho E, et al. Effect of the Uganda Newborn Study on care-seeking and care practices: a cluster-randomised controlled trial. Glob Health Action. 2014;7 doi: 10.3402/gha.v8.24584. 24584, doi: http://dx.doi.org/10.3402/gha.v7.24584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Waiswa P, Peterson SS, Namazzi G, Ekirapa EK, Naikoba S, Byaruhanga R, et al. The Uganda Newborn Study (UNEST): an effectiveness study on improving newborn health and survival in rural Uganda through a community-based intervention linked to health facilities – study protocol for a cluster randomized controlled trial. Trials. 2012;13:213. doi: 10.1186/1745-6215-13-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Waiswa P, Namazzi G, Kerber K, Peterson S. Designing for action: adapting and implementing a community-based newborn care package to affect national change in Uganda. Glob Health Action. 2014;7 doi: 10.3402/gha.v8.24250. 24250, doi: http://dx.doi.org/10.3402/gha.v7.24250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Waiswa P, Peterson S, Tomson G, Pariyo GW. Poor newborn care practices – a population based survey in eastern Uganda. BMC Pregnancy Childbirth. 2010;10:9. doi: 10.1186/1471-2393-10-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chanrachakul B, Herabutya Y, Udomsubpayakul U. Epidemic of cesarean section at the general, private and university hospitals in Thailand. J Obstet Gynaecol Res. 2000;26:357–61. doi: 10.1111/j.1447-0756.2000.tb01339.x. [DOI] [PubMed] [Google Scholar]
- 37.Barros FC, Victora CE, Vaughan JP, Huttly SRA. Epidemic of caesarean sections in Brazil. Lancet. 1991;338:167–9. doi: 10.1016/0140-6736(91)90149-j. [DOI] [PubMed] [Google Scholar]
- 38.Price M, Broomberg J. The impact of the fee-for-service reimbursement system on the utilisation of health services. Part III. A comparison of caesarean section rates in white nulliparous women in the private and public sectors. S Afr Med J. 1990;78:136–8. [PubMed] [Google Scholar]
- 39.Uganda Bureau of Statistics, MEASURE, ICF International. Kampala, Uganda: Uganda Bureau of Statistics; 2012. Uganda demographic and health survey 2011. [Google Scholar]
- 40.Arsenault C, Fournier P, Philibert A, Sissoko K, Coulibaly A, Tourigny C, et al. Emergency obstetric care in Mali: catastrophic spending and its impoverishing effects on households. Bull World Health Organ. 2013;91:207–16. doi: 10.2471/BLT.12.108969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Su TT, Kouyate B, Flessa S. Catastrophic household expenditure for health care in a low-income society: a study from Nouna district, Burkina Faso. Bull World Health Organ. 2006;84:21–7. doi: 10.2471/blt.05.023739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Xu K, Evans DB, Kadama P, Nabyonga J, Ogwal PO, Nabukhonzo P, et al. Understanding the impact of eliminating user fees: utilization and catastrophic health expenditures in Uganda. Soc Sci Med. 2006;62:866–76. doi: 10.1016/j.socscimed.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 43.McPake B, Asiimwe D, Mwesigye F, Ofumbi M, Ortenblad L, Streefland P, et al. Informal economic activities of public health workers in Uganda: implications for quality and accessibility of care. Soc Sci Med. 1999;49:849–65. doi: 10.1016/s0277-9536(99)00144-6. [DOI] [PubMed] [Google Scholar]