To the Editor
Improvements in prevention have led to declines in rates of myocardial infarction (MI). 1 Simultaneously, evidence from randomized trials has confirmed the role of medical therapy as a first-line treatment for stable coronary disease.2 Together, these forces could lead to significant declines in population-wide rates of coronary revascularization. We examined recent temporal trends in population rates of coronary revascularization utilizing comprehensive clinical data collected in Massachusetts.
Methods
We included all Massachusetts residents undergoing coronary revascularization at non-federal hospitals from April 2003 through September 2012. These included patients undergoing inpatient or outpatient PCI, and CABGs with and without concomitant valve or aortic surgery. We counted only the first procedure per year per patient. Procedures were classified as “urgent” if done in the setting of (PCI) or within 21 days of (CABG) myocardial infarction, and otherwise classified as “elective”. Population denominators were obtained from the U.S. Census, stratified by sex and age.3 Direct methods for adjustment were used using the 2012 population as standard.1 Cochran-Armitage testing was used to assess linear trend.
Results
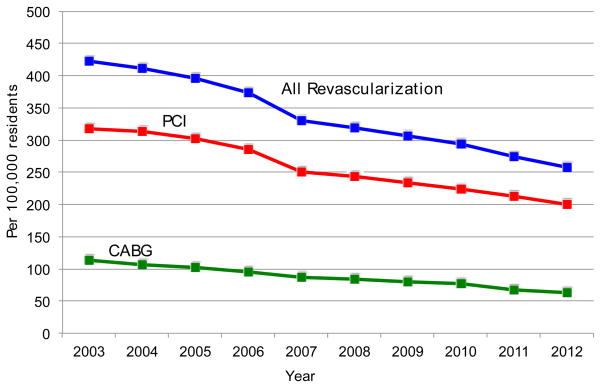
From April 2003 through September 2012, 171,702 coronary revascularization procedures (76.9% PCI, 23.1% CABG) were included. The mean adult Massachusetts population was 5.2 million. The age-sex-adjusted rate of coronary revascularization declined from 423 per 100,000 to 258 (P < 0.001, Figure 1), a 39.0% decline during the study period. Rates of PCI declined from 318 to 200 per 100,000 while rates of CABG declined from 113 to 63 per 100,000 (p < 0.001 for both).
Figure 1.
Temporal trends in population-wide rates of coronary revascularization in Massachusetts, 2003 – 2011.
Rates reflect the number of unique individuals undergoing revascularization in a given year, per 100,000 residents, and are adjusted for age and sex. PCI, percutaneous coronary intervention. CABG, coronary artery bypass graft surgery.
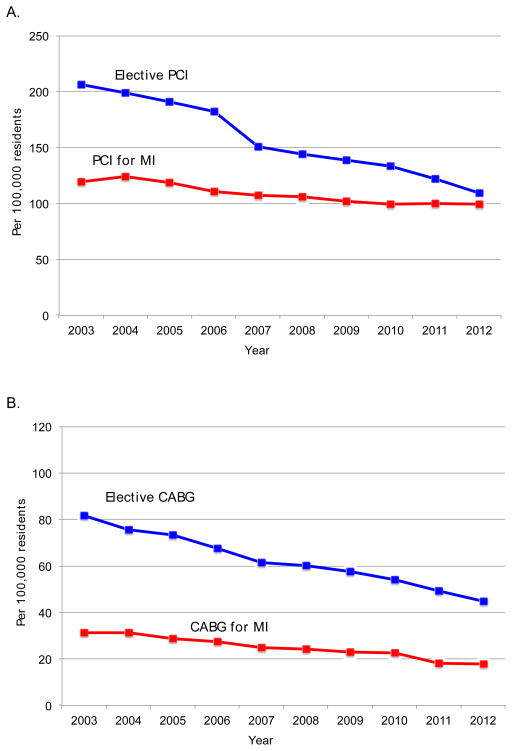
Among PCIs, elective PCIs declined from 206 to 109 per 100,000 (P < 0.001), while urgent procedures declined from 119 to 100 per 100,000 (P < 0.001, Figure 2). Elective CABG declined from 82 to 45 per 100,000 while urgent CABG declined from 31 to 18 per 100,000 (P < 0.001). Isolated CABG rates fell from 90 to 45 per 100,000 (P < 0.001), while combined isolated CABG and aortic or mitral valve surgery did not change (10 per 100,000 in 2003 vs. 10 in 2012).
Figure 2.
Temporal trends in rates of A) percutaneous coronary intervention and B) coronary artery bypass graft surgery, stratified by presentation with or without myocardial infarction, 2003 – 2012.
Temporal trends in rates of percutaneous coronary intervention (Panel A) and coronary artery bypass graft surgery (Panel B), stratified by presentation with or without myocardial infarction. Rates reflect the number of unique individuals with and without myocardial infarction undergoing percutaneous coronary intervention in a given year, per 100,000 residents, and are adjusted for age and sex. PCI, percutaneous coronary intervention. MI, myocardial infarction.
Discussion
We observed steep declines in population-wide rates of coronary revascularization in Massachusetts over the previous decade. For PCI, reductions in the rates were greater in magnitude for elective procedures than for procedures done for myocardial infarction, declining by nearly 50% between 2003 and 2012 for elective PCI compared with a 16.4% decline in rates of urgent PCI over the same time period.
The etiologies of the observed trends are likely multifactorial. Significant reductions in rates of myocardial infarction have been observed in multiple populations, likely attributable to improved primary and secondary prevention. 4,5 The publication of the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial2 comparing PCI to initial medical therapy for stable angina was temporally associated with the steepest 1 year decline in elective PCI rates. Explicit attention to the appropriate use of PCI may also have contributed to more recent declines in PCI. 6
The study has several limitations. We cannot know with certainty what has led to the observed trends, and our results may not generalize to other geographic locations. Also, we did not capture outcomes of patients who may have been considered for, but did not undergo coronary revascularization, and do not know if overall cardiovascular outcomes in these patients has changed.
In summary, we found that rates of coronary revascularization have declined by nearly 40% in Massachusetts since 2003, with the most rapid declines in elective PCI procedures and isolated CABG surgeries. These data have broad implications for regional health policy, training and provider accreditation, hospital resource allocation, and patient outcomes.
Acknowledgments
Dr. Robert Yeh had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The authors acknowledge the work of Treacy Silbaugh, Katya Zelevinksy, Matthew Cioffi and Cashel O’Brien in the preparation of this manuscript. The work was supported, in part, by the Hassenfeld Scholars Program. The authors report the following disclosures: Dr. Yeh receives funding from the National Heart, Lung, and Blood Institute (1K23HL118138), the Hassenfeld Scholars Program, and the Harvard Clinical Research Institute. Dr. Mauri receives institutional research support from Abbott, Boston Scientific, Cordis, Medtronic, Eli Lilly, Daiichi Sankyo, Bristol Myers Squibb, Sanofi-Aventis; and has consulted for Cordis, Medtronic, Boston Scientific and Biotronik.
Footnotes
Disclosures: Dr. Yeh receives funding from the National Heart, Lung, and Blood Institute (1K23HL118138), the Hassenfeld Scholars Program, and the Harvard Clinical Research Institute. Dr. Mauri receives institutional research support from Abbott, Boston Scientific, Cordis, Medtronic, Eli Lilly, Daiichi Sankyo, Bristol Myers Squibb, Sanofi-Aventis; and has consulted for Cordis, Medtronic, Boston Scientific and Biotronik. The remaining authors report no disclosures.
References
- 1.Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010 Jun 10;362(23):2155–2165. doi: 10.1056/NEJMoa0908610. [DOI] [PubMed] [Google Scholar]
- 2.Boden WE, O’Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007 Apr 12;356(15):1503–1516. doi: 10.1056/NEJMoa070829. [DOI] [PubMed] [Google Scholar]
- 3.Annual Estimates of the Resident Population by Single Year of Age and Sex for the United States, States, and Puerto Rico Commonwealth: April 1, 2010 to July 1, 2012. U.S. Census Bureau, Population Division; Jun, 2013. [Google Scholar]
- 4.Roger VL, Weston SA, Gerber Y, et al. Trends in incidence, severity, and outcome of hospitalized myocardial infarction. Circulation. 2010 Feb 23;121(7):863–869. doi: 10.1161/CIRCULATIONAHA.109.897249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yeh RW, Normand SL, Wang Y, Barr CD, Dominici F. Geographic disparities in the incidence and outcomes of hospitalized myocardial infarction: does a rising tide lift all boats? Circ Cardiovasc Qual Outcomes. 2012 Mar 1;5(2):197–204. doi: 10.1161/CIRCOUTCOMES.111.962456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patel MR, Dehmer GJ, Hirshfeld JW, Smith PK, Spertus JA. ACCF/SCAI/STS/AATS/AHA/ASNC 2009 Appropriateness Criteria for Coronary Revascularization: a report by the American College of Cardiology Foundation Appropriateness Criteria Task Force, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons, American Association for Thoracic Surgery, American Heart Association, and the American Society of Nuclear Cardiology Endorsed by the American Society of Echocardiography, the Heart Failure Society of America, and the Society of Cardiovascular Computed Tomography. J Am Coll Cardiol. 2009 Feb 10;53(6):530–553. doi: 10.1016/j.jacc.2008.10.005. [DOI] [PubMed] [Google Scholar]